Key summary points
To identify what evidence exists regarding how geriatricians feel about managing older people living with HIV.
AbstractSection FindingsCurrently whilst geriatricians are willing to contribute to the care of older people living with HIV, they lack the experience and training to take a prominent role.
AbstractSection MessageIncorporating education about HIV care into geriatric medicine curricula and the formation of quality clinical practice guidelines is required to prepare geriatricians to help participate in the care of older people living with HIV.
Abstract
Purpose
The proportion of people living with HIV being older adults is increasing and due to high rates of multimorbidity and frailty within this group geriatricians are well placed to contribute to their care. However, little is known about how geriatricians feel about this new opportunity.
Methods
A scoping review was performed following the Arksey & O’Malley’s methodological framework with nine databases searched in December 2021 for studies reporting the experiences or views of geriatricians on caring for people living with HIV. Study inclusion was not limited by language or year of publication. Narrative reviews were excluded. Two reviewers independently performed the extraction using predetermined criteria. A descriptive analysis of extracted information was performed.
Results
Six publications reporting four studies, all conducted in the USA, were identified. The current barriers to geriatricians being involved in the care of older people living with HIV are: their current experience in managing people living with HIV, their knowledge of HIV, specific issues related to older people living with HIV and screening for HIV in older people as well as their attitudes to people living with HIV and experience of managing older LGBTQ + people.
Conclusion
Prior to geriatricians being routinely involved in the care of older people living with HIV further research outside of the USA is required. Geriatricians will also require specific training which should be incorporated into geriatric medicine training curricula as well as the creation of learning tools and quality clinical practice guidelines ideally created in collaboration with HIV organisations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Across Europe approximately half of the people accessing HIV services are over the age of 50 and by 2030 this will rise to 70% with almost 40% being over 65 [1,2,3,4,5]. The reasons for this rise include the availability of effective antiretroviral therapy (ART) and improved management of opportunistic infections and comorbidities [6, 7]. However, another factor is that the number of new diagnoses in older people is increasing, with one in six new cases of HIV diagnosed in Europe being in someone aged 50 or older, representing 14% of new diagnoses with this increasing by 2% annually [1, 8].
HIV is associated with high rates of multimorbidity and frailty making geriatricians well positioned to contribute to the care of people living with HIV which is presently done within HIV services by clinicians less familiar with the concept of ‘Comprehensive Geriatric Assessment’ (CGA) as evidenced by of 23 out of 98 HIV services in the United Kingdom (UK) surveyed in 2016 reporting a need for a dedicated ageing service and approximately half of clinics indicating they would refer complex older adults to a geriatrician [9,10,11,12,13,14]. The most recent European guidelines produced by the European AIDS Clinical Society (EACS) emphasises the importance of frailty screening and CGA whilst those produced by the British HIV Association (BHIVA) promote incorporating geriatricians into the care of complex older people living with HIV [15, 16].
Currently in some European countries geriatricians are already involved in the delivery of specialist clinics for older people living with HIV and report positive outcomes suggesting a multidisciplinary model could prevent older people living with HIV falling between the cracks in existing services [17, 18]. However, this will require more geriatricians to become familiar with HIV and how it affects people in later life. Whilst numerous papers highlight the importance of CGA and the engagement of geriatricians in the care of older people living with HIV little is known about how geriatricians themselves feel about this new opportunity [3, 6, 14, 19,20,21,22].
Methods
A scoping review was performed according to the methodological framework developed by Arksey and O’Malley with reporting following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Review checklist [23, 24].
Search strategy
A comprehensive search of published research was conducted in December 2021 with nine computerised databases (AMED, BNI, CINAHL, EMBASE, EMCARE, HMIC, Medline, PsychINFO and PubMed) accessed using synonyms of the keywords ‘HIV’ and ‘geriatrician’ or ‘geriatric medicine’. The grey literature was also searched. The full search strategy is outlined in Appendix 1.
Identifying the research question
The research question was ‘what evidence exists regarding how geriatricians feel about managing older people living with HIV?’.
Study selection
The search was performed using the Healthcare Databases Advanced Search (HDAS) and after duplicates were removed the two reviewers (HTJ and TJB) independently assessed the titles and abstracts for eligibility. Further review of potentially eligible full texts was then done against the eligibility criteria by both reviewers. There was a strategy in place to engage a third reviewer should differences in opinion during the selection process have arisen.
Eligibility criteria
Population
Any studies exploring the views of doctors working in the field of geriatric medicine on managing people living with HIV were included regardless of their stage of training. No other limitations based on population characteristics were applied.
Concept
Any publications reporting the desired outcome measure were included regardless of their primary aims.
Context
All sources of evidence pertaining to any country or contextual setting were eligible for inclusion.
Type of evidence sources
The initial search was limited to primary research articles or systematic reviews from peer reviewed sources as despite scoping reviews not requiring appraisal of methodological quality, the peer review process ensures the research question is answered through robust data. Due to the limited number of relevant articles, a decision was made to include peer reviewed conference abstracts and search the grey literature for additional studies with the intent to consolidate all existing data. Narrative reviews were excluded as they do not report original results but their reference lists were reviewed to identify additional eligible studies. There was no limitation on the year or language of publication to allow worldwide studies to be included as well as information from both the pre-ART and post-ART eras.
Data charting
The reviewers determined what data was to be extracted prior to data charting to maintain consistency. Extracted data included: title, authors, publication type, journal, publication year, location and country of study, study aims, sample size and demographics, study design, analysis methodology as well as key findings. Extracted data were examined by both reviewers for clarity and reliability.
Quality appraisal
As this was a scoping review which aims to identify gaps in existing evidence, methodological quality was not assessed.
Data analysis
Extracted information was tabulated according to the categories outlined above, with a descriptive analysis of extracted information performed and presented narratively.
Results
Selection of studies
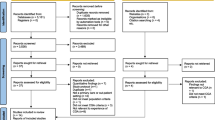
The initial database search yielded 802 results which was reduced to 467 after duplicate removal, with an additional 15 articles identified through hand searching. Screening records by title and abstract resulted in 40 full-text articles being retrieved with six proving eligible for analysis. No further studies were identified from the reference lists of included studies or from the grey literature. The full PRISMA flow diagram is displayed in Fig. 1.
PRISMA Diagram. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. https://doi.org/10.1371/journal.pmed1000097. For more information, visit www.prisma-statement.org
Study characteristics
The identified studies were published between October 2008 and April 2021 with three (50%) being published in the last 5 years (Table 1) [25,26,27,28,29,30]. All studies were conducted within the Unites States of America (USA) [25,26,27,28,29,30]. Five publications (83%) were conference abstracts with the remaining being a primary research article [25,26,27,28,29,30]. Three publications presented the results of the same study (two conference abstracts and one article) [27, 28, 30]. Five (83%) utilised a cross-sectional methodology involving surveys, whilst the remaining study was a pilot of an elective within HIV medicine for geriatric medicine trainees [25,26,27,28,29,30]. The participants of the studies were broad with three (the aforementioned same study) involving geriatricians, as well as nurses and social workers [27, 28, 30]. One study included staff at both a family medicine and geriatric medicine practice whilst the last presented the views of geriatric medicine providers only [26, 29]. Most studies did not report full participant demographic data but in those that did geriatricians were predominately White (62–66%) females (57–64%) who were heterosexual (93.7%) and who had been working in geriatric medicine for an average of 10 years [27, 28].
Findings
Six main themes were identified from the literature (Fig. 2):
Current experience in managing people living with HIV
In a cohort of 94 geriatricians 46% reported they were ‘not comfortable at all’ in providing care to people living with HIV, with 44.7% having seen none in the last year and the remaining 46.8% seeing between one and five, which explains the predominant finding from all studies being that currently geriatricians have a knowledge gap related to the management of people living with HIV [25,26,27,28,29,30].
Knowledge of HIV
Hughes utilised the original ‘HIV Knowledge Questionnaire-45’ (HIV-K-Q-45) which is a self-administered 45 part true or false questionnaire developed to assess respondents knowledge of HIV [31]. They compared the results of geriatricians (n = 111), to nurses (n = 190) and social workers (n = 173) and found that geriatricians scored statistically significantly higher (p < 0.0005) with a mean score of 39.94 (total sample 38.08) [28, 30].
Knowledge of specific issues related to older people living with HIV
Hughes also asked participants what percentage people over 50 contributed to the total number of AIDS cases in the USA from the start of the epidemic to 2006 with scores calculated as the absolute difference from the correct value (13%) with geriatricians scoring 11.2 points from this (total sample: 13.64 points, SD: 12.43, range 0–69) but no statistically significant differences was found between the groups of professionals (p = 0.061) [28]. Only 47% of geriatricians were able to correctly rank the four most common risk factors for HIV infection in older people (correct ranking at the time: 1. sex between men, 2. injection drug use 3. sex between men and women 4. blood transfusion) [28, 30]. It must be noted that sex between men and women is now the second most common mode of transmission and injection drug use third [32]. Similarly, only a minority (31%) knew that dementia related to HIV is reversible [27, 28, 30]. Conversely, 75% of geriatricians recognised that cases of HIV amongst heterosexual people over 50 are increasing compared to only 66% of nurses and social workers though again this was not statistically significant (p = 0.105) [27, 28, 30]. Finally, a geriatric medicine trainee working with people living with HIV identified that geriatric syndromes were common and presented earlier [25].
Knowledge of screening for HIV in older adults
With regards to screening for HIV in a study of 14 geriatric medicine providers 71% reported good knowledge of the United States Preventive Services Task Force (USPSTF) HIV screening guidelines and ordered tests if they identified risk factors [29]. However of the 1259 patients seen in the geriatric medicine clinic in a 3-month period only 31 (2.5%) were tested, with 26 (84%) being tested based on a known risk factor [29]. The mean age of the 31 tested was 81.64, and 14 (45%) of the patients were male with only 7 (22.5%) having documentation of their sexual activity [29]. Respondents reported that annual HIV screening was often not done due to there “not being enough time to discuss” (21%) or because “patients refused to discuss” (21%) [29]. Overall, geriatricians were likely to enquire about older people’s sexual practices less than once a year but when it was done discussion of condom use was common (79%) [29].
Attitudes to older people living with HIV
Overall, the geriatricians surveyed had positive attitudes towards older people living with HIV and were attitudinally prepared to provide care to them [26, 28, 30]. Hughes assessed this in their study using a modified version of the ‘AIDS Attitude Scale (AAS)’ which has been shown to be a valid and reliable measure of attitudes, and consists of two subscales: a 14-item avoidance scale and a 7-item empathy scale with each of the 21 items rated on a 6-point Likert scale from 1 (strongly disagree) to 6 (strongly agree) [28, 30, 33, 34]. Mean scores for the AAS subscales range from 1 to 6, with a score of 6 on empathy representing high levels of empathy, while a 6 on the avoidance subscale represents a high level of avoidance [33, 34]. The attitudes of geriatricians were found to be positive with high mean score on the empathy subscale of 5.46 (SD 0.69) and a low mean score on the avoidance subscale of 1.72 (SD 0.69) [28, 30]. However, significant differences were not found for either subscale when comparing the geriatricians to nurses or social workers [28, 30].
Experience of managing older LGBTQ + people
Finally, the geriatricians surveyed identified an overlap between people living with HIV and those identifying as lesbian, gay, bisexual, transgender, queer or questioning (LGBTQ +) and had positive attitudes towards caring for them though reported less comfort around trans patients due to concerns about ensuring they used the appropriate pronouns and their lack of experience of gender-affirming hormone therapy [26]. Lastly, of the 57 geriatricians surveyed 39% reported witnessing discrimination towards LGBTQ + patients, families, or staff in the workplace [26].
Discussion
The recommendations from the six publications were homogenous highlighting that whilst geriatricians have positive attitudes towards people living with HIV and have some understanding of the condition, they currently require further training before they can play a prominent role in the care of older people living with HIV [25,26,27,28,29,30]. Education should focus on the history of the HIV epidemic and training on HIV as a condition but more specifically how it affects people in older age [25,26,27,28,29,30].
The richest data came from the 2011 study by Hughes which whilst informative is now over a decade old [28]. Due to ongoing advancements in HIV care, evolving attitudes towards people living with HIV and changes to the demographics of new cases this data is not directly applicable today. The HIV-K-Q-45 is now over 20 years old and therefore contains outdated questions and concepts, for example asking if ‘a person can get HIV from a toilet seat’ [31, 35]. Similarly, the AAS was only validated in groups of nurses, health education students and lay people but never doctors, or specifically geriatricians, meaning the results from Hughes’ study are less reliable as one would expect geriatricians to have a higher level of knowledge of HIV compared to nurses and social workers that could directly impact attitudes [33, 34, 36, 37]. The questions in the AAS are also outdated with several only exploring attitudes towards gay men or people who inject drugs and equating that with being synonymous with living with HIV [33, 34, 36, 37]. These flaws restrict the clinical use of the AAS as they limit its ability to measure one attitude construct at a time, specifically attitudes towards people living with HIV, when the items bring in attitudes about differing constructs such as homosexuality [33, 34, 36, 37]. Attitudes towards LGBTQ + people have progressed since the validation studies for the AAS and Hughes’ study meaning their results have less pertinence today [28, 33, 34, 36, 37]. It must also be noted that Hughes chose to compare knowledge of and attitudes towards people living with HIV between geriatricians, nurses and social workers which are discrete professions [27, 28, 30]. This is important as there are external societal factors that impact the profession a person may pursue. Across all three professions being White was the predominant ethnicity though the geriatrician group had the most diversity with 40.5% being non-White compared to only 11.9% of nurses and 12.9% of social workers [28]. Other differences include more gender variation amongst geriatricians with 57.1% being female versus 96.9% of nurses and 84.2% of social workers and whilst all the nurses recruited identified as heterosexual 6.3% of geriatricians and 7.4% of social workers identified as LGBTQ + [28]. Finally, as expected the geriatrician group had the highest level of postgraduate education, followed by social workers then nurses [28]. Each of these characteristics may impact a person’s knowledge or attitude to a subject matter meaning the groups are not the most optimal comparators. Therefore, it may have been preferable to compare different medical professionals for example geriatricians to infectious diseases or internal medicine specialists. In a 2016 study of infectious disease fellows from across the USA 51% reported little experience in initiating and monitoring patients on ART and only 22% felt this was adequality taught during their fellowship programme [38]. Meanwhile, a 2010 study utilising a cross-sectional survey of 223 s and third year internal medicine residents from four programs in Baltimore, Boston, Detroit, and New York City USA between March and June 2006 identified that 51% had contributed to the inpatient care of at least 30 people living with HIV in the past year whilst the majority (63%) and only cared for up to five outpatients [39]. The majority (89%) of residents viewed managing people living with HIV as an excellent educational opportunity but felt less prepared to do so in an outpatient setting which is important as HIV continues to transition to a chronic illness model [39]. Therefore, the potential hardships geriatricians may face are not specific to this discipline and extend to other non-HIV specialists managing people living with HIV [38, 39]. However, despite its weaknesses Hughes’ work does provide the most robust answer to the research question currently available supporting the need for further studies [28]. Rather than replicating Hughes’ study in Europe what is required is the development of a validated tool to assess clinicians’ knowledge of managing older people living with HIV focussing on current common clinical scenarios such as comorbidities, geriatric syndromes, polypharmacy and drug-drug interactions [28, 31, 35].
Due to a rising number of new HIV diagnoses in older age education and guidance for geriatricians on when to screen patients for HIV is paramount [7, 29, 40]. Many older people will have grown up during the HIV epidemic and will recall the advertising campaigns many of which focussed on specific groups such as gay men or Black people from Africa indirectly contributing to the idea that White heterosexual people are at negligible risk of acquiring HIV, potentially explaining the rising rates within this group [6, 7, 40]. Advancements in HIV care has resulted in less public health campaigns resulting in low levels of knowledge about HIV amongst the general public but specifically amongst older heterosexual people [40, 41]. Stigma remains a large problem not only around HIV but also LGBTQ + relationships, sex outside of a long-term relationship or sex in later life resulting in healthcare professionals’ fear of offending older people by offering a test consequentially leading to a barrier to testing as well as older peoples’ potential embarrassment with them being less used to discussing sex and relationships with healthcare professionals [40, 42,43,44]. Meanwhile, whilst many younger patients may utilise sexual health services to undergo HIV testing the majority of testing in older people across Europe is performed within Primary Care [42,43,44,45,46]. This is important as many older people may not feel confident in attending sexual health services and therefore borrowing strategies from Primary Care such as offering routine HIV testing for all new patients or as part of a standard annual health check regardless of risk could be applied to all people attending geriatric medicine services helping to reduce stigma as well as identifying those undiagnosed particularly older women [29, 40, 42,43,44, 47].
When to refer an older person living with HIV to a geriatrician is also not well defined which is not unsurprising as the criteria for referring to a geriatrician generally varies not only across Europe but also within individual countries [48, 49]. Some centres may use chronological age whilst others favour alternate measures looking at indicators of biological age such as frailty scores [48, 49]. Interestingly whilst typical ageing research arbitrarily regards older people as being over 65 the literature on ageing HIV populations typically uses 50 based on the original age stratification of HIV set by the US Centers for Disease Control (CDC) [1, 50]. This age continues to be used today not only for this reason, but also as studies have demonstrated that people over 50 living with HIV are less likely to achieve a complete immunological response despite concordance to treatment when compared to younger people as well as 50 being shown to be the age when the main causes of mortality change to causes unrelated to HIV [1]. Given this is an evolving field this age cut-off should persist for now though referral processes should also follow EACS recommendations and calculate a frailty score, with the Fried frailty phenotype (FFP) being the most validated amongst people living with HIV [11, 15, 17, 51]. However, it must be noted that the FFP does not consider the broader elements of frailty such as psychosocial functioning or cognition and whilst other frailty scores do consider these they are not as well validated in people living HIV or in people under 65 [11, 51, 52]. Therefore, at present whilst further research is conducted referrals to geriatricians should be done based on local agreement with referral processes incorporating information on age, frailty score, presence of geriatric syndromes and any other concerns of the person living with HIV, their family and friends or the referrer themselves.
How best to deliver the care to older people living with HIV is also unclear as there is no agreed standardised model [17]. A survey of 27 HIV clinicians in the USA described them wanting assistance with managing multimorbidity (median: 85, range 65–100), polypharmacy (83, 51–100), cognitive impairment (80, 68.5–96), and mood disorders (80, 67–92) which are often common conditions identified in older people living with HIV and which geriatricians are well versed in [17, 18, 53]. They also reported a desire for the development of specific guidelines for older people living with HIV (68%) and access to more training on managing older people (60%) [53]. Similar findings have also been reported in Europe with HIV clinicians recognising the importance of geriatricians in managing frailty and multimorbidity [12, 54]. At present it is clear that no group of health professionals can manage the care of older people living with HIV independently so a collaborative service model remains the most appropriate due to the low levels of confidence, knowledge and experience amongst geriatricians and the lack of experience of HIV clinicians in managing frail older people. Several joint HIV and geriatric medicine clinics exist already internationally such as the ‘Sage Clinic’ at the Royal Free Hospital in London, UK, the ‘Silver Clinic’ in Brighton, UK and the ‘Golden Compass Programme’ in San Francisco, USA demonstrating positive outcomes from collaborative working [17, 18, 55]. However, this model may not be feasible everywhere due to issues of either supply or demand, with alternatives including incorporating geriatricians into multidisciplinary meetings about complex patients or having clear referral pathways into existing services for HIV clinicians to follow.
Increasing education on how to manage people living with HIV is fundamental to try and ensure geriatricians are comfortable due to the low levels reported with the creation of learning tools highlighted as important due to many currently lacking exposure in their current practice [25,26,27,28,29,30]. Another option would be for interested geriatric medicine trainees to spend time working in HIV medicine to gain experience, similar to an Orthogeriatrics or Oncogeriatrics model, with the elective depicted in this review being positively received by both the trainee and the supervising HIV clinicians [25, 56]. Education is important to reduce stigma, improve healthcare professionals’ attitudes towards people living with HIV and to provide better care, for example increasing awareness of drug-drug interactions [3, 6, 17, 21, 28, 57]. Basic education about HIV with specific focus on older people should be incorporated into geriatric medicine curricula to ensure all geriatricians gain some exposure [58]. Finally, it may be beneficial for HIV organisations such as EACS to come together with geriatric medicine bodies like the European Geriatric Medicine Society (EuGMS) to author joint standards and guidelines, promoting interspeciality working and holistic care [15, 16].
Finally, this review has also highlighted that geriatricians require more cultural competency training on managing LGBTQ + people regardless of HIV status [26]. Currently, gay and bisexual men make up a large number of older men living with HIV with sex between men still contributing to a significant proportion of new cases [32]. A 2010 study found that more than half of lesbian, gay, and bisexual respondents and 70% of transgender respondents had experienced discrimination by healthcare providers ranging from biases, incorrect assumptions, derogatory statements to refusal of care [59]. LGBTQ + older adults may delay or avoid health care because of fear of or previous experiences of discrimination while others may hide their identity when using healthcare services [60]. Given that the number of older LGBTQ + people in Europe is expected to double by 2030 geriatricians not only have a responsibility to educate themselves about the health conditions common amongst older LGBTQ + people, but also their lived experiences and be actively involved in ensuring accessible culturally sensitive services through public policy and societal guidelines with specific focus made to ensure trans people are well represented [26, 60,61,62,63].
As a scoping review the absence of methodological quality appraisal limits its ability to provide validated recommendations, however given the aim was to consolidate the views of geriatricians the impact of this should be minimal. All studies were conducted in the USA where cultural, political and healthcare model factors may impact the views of respondents and limit its generalisability [64,65,66]. However, given the knowledge gap it still has the potential to inform providers in Europe. There were only six publications, providing data from four separate studies with only one of the four having the primary aim being to ascertain the views of geriatricians on caring for people living with HIV [27, 28, 30]. Another limitation is that five of the six publications consist of conference abstracts [25,26,27, 29, 30]. Whilst conference abstracts may not contain detailed information, and determining the dependability of the results is challenging their inclusion was important due to the paucity of data available resulting in an increased in comprehensiveness and decreasing the impact of publication bias [67]. Half of the included publications were published within the last 5 years but as mentioned previously despite one having rich data the remaining three publications all by Hughes have less relevance due to their age [25,26,27,28,29,30]. The review was strengthened by not limiting studies by language meaning the chances of omitting those from lower and lower-middle income countries was reduced [68]. Therefore, this review provides an encompassing review of the literature on the views and experiences of geriatricians on managing people living with HIV and clearly demonstrates a scarcity of high-level evidence providing grounds for future high-quality research.
There is a lack of knowledge on this topic outside of the USA and more international studies are required due to differing healthcare systems and HIV prevalence between countries [64,65,66]. Health care systems will impact both how people living with HIV experience care as well as how geriatricians experience working within it [64,65,66]. Geriatric medicine training also varies between countries with some having more formal structured training programmes than others prompting the recent creation of a standardised European postgraduate curriculum [48, 58, 69]. Exploring the views of geriatricians across Europe is crucial to see whether the experiences reported are generalisable and not specific to the USA. This does not however consider the situation in lower and lower-middle income countries with a high prevalence of HIV such as in Sub-Saharan Africa where despite the rising numbers of older people living with HIV there remains very few geriatricians which must also be explored [66, 70].
This article provides a comprehensive review of the existing literature regarding the views of geriatricians on managing older people living with HIV providing the groundwork for future high-quality research and intervention strategies on how best to support people living with HIV as they age. Future steps comprise gaining an international view, developing educational tools for geriatricians including creating clinical practice guidelines. These are required before we can support recommendations for geriatricians play a dominant role in the care of older people living with HIV and will inform decisions on how best to structure HIV services across Europe to manage this ageing cohort in the near future.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
References
Sánchez-Conde M, Díaz-Alvarez J, Dronda F, Brañas F (2019) Why are people with HIV considered “older adults” in their fifties? Eur Geriatr Med 10:183–188
Smit M, Brinkman K, Geerlings S et al (2015) Future challenges for clinical care of an ageing population infected with HIV: a modelling study. Lancet Infect Dis 15:810–818
Brañas F, Ryan P, Troya J, Sánchez-Conde M (2019) Geriatric-HIV medicine: the geriatrician’s role. Eur Geriatr Med 10:259–265
Brañas F, Guaraldi G, Sánchez-Conde M (2019) HIV and aging: time to bridge the gap between clinical research and clinical care. Eur Geriatr Med 10:165–167
Wing EJ (2017) The aging population with HIV infection. Trans Am Clin Climatol Assoc 128:131–144
Kearney F, Moore AR, Donegan CF, Lambert J (2010) The ageing of HIV: implications for geriatric medicine. Age Ageing 39:536–541
Guaraldi G, Zona S, Brothers TD et al (2015) Aging with HIV vs. HIV seroconversion at older age: a diverse population with distinct comorbidity profiles. PLoS One 10:e0118531
Tavoschi L, Gomes Dias J, Pharris A (2017) New HIV diagnoses among adults aged 50 years or older in 31 European countries, 2004–15: an analysis of surveillance data. Lancet HIV 4:e514–e521
De Francesco D, Sabin CA, Reiss P (2020) Multimorbidity patterns in people with HIV. Curr Opin HIV AIDS 15:110–117
Welsh TJ, Gordon AL, Gladman JR (2014) Comprehensive geriatric assessment—a guide for the non-specialist. Int J Clin Pract 68:290–293
Jones HT, Levett T, Barber TJ (2022) Frailty in people living with HIV: an update. Curr Opin Infect Dis 35:21–30
Cresswell F, Levett T (2017) Specialist care of older adults with HIV infection in the UK: a service evaluation. HIV Med 18:519–524
Montejano R, de Miguel R, Bernardino JI (2019) Older HIV-infected adults: complex patients—comorbidity (I). Eur Geriatr Med 10:189–197
Bertagnoli L, Iannuzzi P, Ciccone S et al (2019) Older HIV-infected adults: complex patients—geriatric syndromes (II). Eur Geriatr Med 10:213–218
European AIDS Clinical Society (2021) EACS guidelines 2021. In: EACS
British HIV Association (2018) British HIV association standards of care for people living with HIV 2018. In: BHIVA
Jones HT, Samji A, Cope N et al (2022) What problems associated with ageing are seen in a specialist service for older people living with HIV? HIV Med 23:259–267
Levett T, Alford K, Roberts J et al (2020) Evaluation of a combined HIV and geriatrics clinic for older people living with HIV: the Silver Clinic in Brighton, UK. Geriatrics 5:81
Sangarlangkarn A, Yamada Y, Ko FC (2021) HIV and aging: Overcoming challenges in existing hiv guidelines to provide patient-centered care for older people with HIV. Pathogens 10.
Bhatta M, Nandi S, Dutta N et al (2020) HIV care among elderly population: systematic review and meta-analysis. AIDS Res Hum Retroviruses 36:475–489
Del Carmen T, Johnston C, Burchett C, Siegler EL (2019) Special topics in the care of older people with HIV. Curr Treat Options Infect Dis 11:388–400
Guaraldi G, Marcotullio S, Maserati R et al (2019) The management of geriatric and frail HIV patients. A 2017 update from the Italian guidelines for the use of antiretroviral agents and the diagnostic clinical management of HIV-1 infected persons. J Frailty Aging 8:10–16
Arksey H, O’Malley L (2005) Scoping studies: towards a methodological framework. Int J Soc Res Methodol 8:19–32
Tricco AC, Lillie E, Zarin W et al (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169:467–473
Walker J, Thompson K (2020) Creation and pilot implementation of a geriatrics fellows' elective in HIV medicine for older adults. J Am Geriatr Soc 68
Spina E, Salzman B, Liantonio J, Danielewicz M (2021) Enhancing cultural and medical competency for lgbt older adults. J Am Geriatr Soc 69
Hughes AK (2008) Geriatricians and HIV: Comfort level and knowledge. Gerontologist 48:107–108
Hughes AK (2011) HIV knowledge and attitudes among providers in aging: results from a national survey. AIDS Patient Care STDS 25:539–545
Kim H, Blachman N, Han BH, Pitts R (2020) HIV screening in an urban geriatrics ambulatory clinic. J Am Geriatr Soc 68:S120–S121
Hughes AK (2010) Learning what we don't know: attitudes and knowledge of gerontological health providers toward HIV/AIDS. J Am Geriatr Soc 58:S94
Carey MP, Morrison-Beedy D, Johnson BT (1997) The HIV-knowledge questionnaire: development and evaluation of a reliable, valid, and practical self-administered questionnaire. AIDS Behav 1:61–74
Centers for Disease Control and Prevention (2020) Diagnoses of HIV infection in the United States and dependent areas, 2018 (updated), volume 31. In: Atlanta, Georgia, USA: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention (CDC), U.S. Department of Health and Human Services
Froman RD, Owen SV (1997) Further validation of the AIDS attitude scale. Res Nurs Health 20:161–167
Froman RD, Owen SV, Daisy C (1992) Development of a measure of attitudes toward persons with AIDS. Image J Nurs Sch 24:149–152
Carey MP, Schroder KE (2002) Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Educ Prev 14:172–182
Froman RD, Owen SV (2001) Measuring attitudes toward persons with AIDS: the AAS-G as an alternate form of the AAS. Sch Inq Nurs Pract 15:161–174; discussion 175–177
Rose JS, Laux JM, Fox CM et al (2020) Development and validation of the mental health professionals’ attitude towards people living with HIV/AIDS scale (MHP-PLHIV-AS). AIDS Care 32:10–18
Hicks C, Johnson SC, Daar E et al (2017) HIV/AIDS training and skills of infectious disease fellows among 33 US academic institutions. Open Forum Infect Dis 4:S448–S448
Phillips KA, Cofrancesco J Jr, Sisson S et al (2010) A multicenter study of internal medicine residents’ perceptions of training, competence, and performance in outpatient HIV care. AIDS Patient Care STDS 24:159–164
Youssef E, Wright J, Delpech V et al (2018) Factors associated with testing for HIV in people aged ≥50 years: a qualitative study. BMC Public Health 18:1204
Anokye R, Acheampong E, Budu-Ainooson A et al (2019) Knowledge of HIV/AIDS among older adults (50 years and above) in a peri-urban setting: a descriptive cross-sectional study. BMC Geriatr 19:304
Bauer M, Haesler E, Fetherstonhaugh D (2016) Let’s talk about sex: older people’s views on the recognition of sexuality and sexual health in the health-care setting. Health Expect 19:1237–1250
Bourne C, Minichiello V (2009) Sexual behaviour and diagnosis of people over the age of 50 attending a sexual health clinic. Australas J Ageing 28:32–36
Gott M, Hinchliff S, Galena E (2004) General practitioner attitudes to discussing sexual health issues with older people. Soc Sci Med 58:2093–2103
Desai S, Tavoschi L, Sullivan AK et al (2020) HIV testing strategies employed in health care settings in the European Union/European Economic Area (EU/EEA): evidence from a systematic review. HIV Med 21:163–179
Davis T (2015) Perspectives from older adults: HIV knowledge, attitudes, and HIV prevention. Gerontologist 55:682–683
Durvasula R (2014) HIV/AIDS in older women: unique challenges, unmet needs. Behav Med 40:85–98
Soulis G, Kotovskaya Y, Bahat G et al (2021) Geriatric care in European countries where geriatric medicine is still emerging. Eur Geriatr Med 12:205–211
Deschodt M, Boland B, Lund CM et al (2018) Implementation of geriatric care models in Europe (imAGE.eu): a cross-sectional survey in eight countries. Eur Geriatr Med 9:771–782
Poindexter C, Emlet C (2006) HIV-infected and HIV-affected older adults. In: Berkman B (ed) Handbook of social work in health and aging. Oxford University Press, New York, pp 91–99
Fried LP, Tangen CM, Walston J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146-156
Falutz J, Brañas F, Erlandson KM (2021) Frailty: the current challenge for aging people with HIV. Curr Opin HIV AIDS 16:133–140
Perfect C, Okeke NL, Sangarlangkarn A et al (2019) Infectious diseases provider opinions on care models for older adults living with HIV. J Am Geriatr Soc 67:S286
Cresswell F, Churchill D, Levett T (2016) A survey to evaluate the provision of specialist services for older adults with HIV in the UK. HIV Med 17:66
Greene ML, Meissner L, Tan JY et al (2018) Patient and provider perceptions of a comprehensive care program for HIV-positive adults over 50 years of age: the formation of the Golden Compass HIV and aging care program in San Francisco. PLoS One 13:e0208486
Gladman JR (2016) Delivering comprehensive geriatric assessment in new settings: advice for frontline clinicians. J R Coll Physicians Edinb 46:174–179
Back D, Marzolini C (2020) The challenge of HIV treatment in an era of polypharmacy. J Int AIDS Soc 23:e25449
Roller-Wirnsberger R, Masud T, Vassallo M et al (2018) European postgraduate curriculum in geriatric medicine developed using an international modified Delphi technique. Age Ageing 48:291–299
Legal L (2010) When health care isn’t caring: Lambda Legal’s survey of discrimination against LGBT people and people with HIV. Lambda Legal, New York, pp 1–26
Committee AGSE (2015) American Geriatrics Society care of lesbian, gay, bisexual, and transgender older adults: position statement. Br J Healthcare Assist 9:344–349
Caceres BA (2019) Care of LGBTQ older adults: What geriatric nurses must know. Geriatr Nurs 40:342–343
Hardacker CT, Rubinstein B, Hotton A, Houlberg M (2014) Adding silver to the rainbow: the development of the nurses’ health education about LGBT elders (HEALE) cultural competency curriculum. J Nurs Manage 22:257–266
Ettner R (2013) Care of the elderly transgender patient. Curr Opin Endocrinol Diabetes Obes 20:580–584
Cancarevic I, Plichtová L, Malik BH (2021) Healthcare systems around the world. In: Tohid H, Maibach H (eds) International medical graduates in the United States: a complete guide to challenges and solutions. Springer International Publishing, Cham, pp 45–79
Pandey A, Galvani AP (2019) The global burden of HIV and prospects for control. Lancet HIV 6:e809–e811
Frank TD, Carter A, Jahagirdar D et al (2019) Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the global burden of diseases, injuries, and risk factors study 2017. The Lancet HIV 6:e831–e859
Scherer RW, Saldanha IJ (2019) How should systematic reviewers handle conference abstracts? A view from the trenches. Syst Rev 8:264
Shenderovich Y, Eisner M, Mikton C et al (2016) Methods for conducting systematic reviews of risk factors in low- and middle-income countries. BMC Med Res Methodol 16:32–32
Petrovic M (2011) Geriatric medicine in Europe: towards professional and training paradigm. Adv Gerontol 24:126–129
Dotchin CL, Akinyemi RO, Gray WK, Walker RW (2012) Geriatric medicine: services and training in Africa. Age Ageing 42:124–128
Funding
This research has received no external funding.
Author information
Authors and Affiliations
Contributions
HTJ was responsible for synthesis of the research question and was the major contributor in drafting and writing the manuscript. Both HTJ and TJB contributed significantly to the design, interpretation of data and substantive revision of all drafts.
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Financial disclosure
TJB has received speaker fees, conference support and advisory board honoraria from Gilead Sciences LTD., ViiV, Roche, MSD and Thera. HTJ has nothing to disclose.
Patient consent for publication
Not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jones, H.T., Barber, T.J. How do geriatricians feel about managing older people living with HIV? A scoping review. Eur Geriatr Med 13, 987–997 (2022). https://doi.org/10.1007/s41999-022-00642-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-022-00642-4