Abstract
This study examines the impact of county- and state-level policies on the spread and severity of COVID-19 in communities in the USA during the first wave of the COVID-19 pandemic. We use county-level COVID-19 death and case data to examine the impact of county- and state-level mandates and non-pharmaceutical interventions (NPIs) on the spread and severity of COVID-19. Following previous work by Amuendo-Dorantes et al. (2020), we utilize a strategy that incorporates the duration of NPI implementation within a county. Specifically, we examine aggregated measures of mask mandates, daycare closures, stay-at-home orders, and restaurant and bar closures. In addition to the implementation and duration of NPI policy, we examine the role of pre-existing factors that contribute to social determinants of health in a locality. We incorporate information on the incidence of prior health conditions, socio-economic factors, and demographics including racial and ethnic composition, share of immigrant population of counties, and state governance in our estimations. To alleviate the possible endogeneity of COVID-19 outcomes and NPIs, we use instrumental variable estimation and our results show that collectively NPIs decreased the intensity of the pandemic by decreasing the total deaths and cases. Furthermore, we find the magnitude of the impact of NPIs increases the longer they are implemented. We also estimate a specification that allows for heterogeneity of NPI impact based on the racial and ethnic composition of counties. Our results suggest that NPIs have a non-uniform impact in counties with different racial and ethnic compositions.
Similar content being viewed by others
Introduction
The Coronavirus Disease 2019 (COVID-19) was first identified in Wuhan, China, in December 2019, and has since ravaged the world. This paper focuses on COVID-19 in the USA from the first reported case to September 7th, 2020. During this period, COVID-19 resulted in more than 970,000 deaths and over 29 million reported cases worldwide.Footnote 1 Within the USA over the same time period, there were approximately 113,700 deaths and 4.885 million cases (authors’ calculation from data). The actual number of deaths and cases may be even larger, as it is suspected that many countries are under-reporting COVID-19 deaths and cases due to a lack of testing to identify COVID-19 and the overwhelming pressure on healthcare systems across the globe (Felter 2021).
During the early stages of the pandemic, from December 2019 to September 7, 2020, there were not many tools available to combat the spread of COVID-19, as no vaccinations were developed and there was limited understanding of which pharmaceutical interventions and medical treatments might mitigate the severity of COVID-19. Understanding of the virus and how it spread was minimal at best. At one point, the public was told that transmission occurred on surfaces and that the COVID-19 virus did not spread through the air. Then, following more research into the new pathogen, scientists determined that COVID-19 is spread via aerosols and began recommending social distancing and masking in public to prevent spread (Center for Disease Control (CDC) 2021a). Because the pathogen was never before seen, the best policies to mitigate the impact of the virus and minimize deaths and cases were not clear.
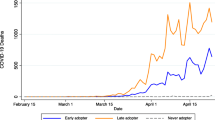
This paper focuses on the overall impact of state and local government response to the initial stages of the COVID-19 pandemic in the USA through the end of Labor Day weekend 2020 (September 7, 2020). In response to the uncertainty and ever-changing understanding of the COVID-19 pandemic in this time frame, many localities chose to enact non-pharmaceutical interventions (NPIs). The timing of the implementation of these NPIs was heterogeneous. Some counties and states decided to implement NPIs before others, yet others implemented these NPIs for a longer duration. Additionally, the spread of COVID-19 was not uniform across states and counties within states. Some areas had more deaths and cases early on in the first wave, while others had more deaths and cases later in the first wave. It should be noted that some counties did not have a single death from COVID-19 in this time period. While other studies focus on daily data and were intended to provide rapid estimates, we rather focus on the impact of policy interventions throughout the first wave with the intention of examining what NPIs were most effective retrospectively using a cross section of counties in the USA.
We know that COVID-19 impacted areas with large minority populations disproportionately, both in terms of the number of cases and the number of severe cases leading to hospitalization, ICU use, and death (Benitiz et al., 2020; Hill and Artiga 2022; CDC 2021b). There are many possible reasons for this phenomenon that have been examined in the literature such as previous lack of healthcare access and healthcare utilization, poverty, age, demographics, or other pre-existing socioeconomic conditions in these areas. Given the fact that racial and ethnic minorities have not fared well during the pandemic, we will also estimate a specification that allows for the differential impact of NPIs on COVID-19 outcomes depending on the share of minority populations (Hispanics and blacks) within a county. This will allow us to see if NPI policies have a differential effect on COVID-19 outcomes depending on racial and ethnic composition.
We focus on two measures of NPIs that aggregate mask mandates, daycare and school closures, restaurant and bar closures, and stay-at-home orders at the county and state levels. We will estimate the impact of these NPIs on the following COVID-19 outcomes: total number of deaths and cases (normalized by the population), and cumulative deaths and cases from the first reported death/case to the peak, and time from first case/death to peak case/death. Understanding how NPIs influence the spread of the virus remains a key question in public health and for combatting the pandemic and future potential outbreaks. Though COVID-19 is trending towards an endemic disease, understanding what policies best ameliorate COVID-19 spread, cases, and deaths will be important for localities. In this research, we examine the impact of NPIs and their duration while controlling for prior health status and healthcare infrastructure, demographic factors, socioeconomic factors, geographic factors, and the political party of the state governor on the spread of COVID-19 in a county using cross-sectional county-level data with approximately three thousand observations.
Due to a concentrated worldwide effort, the COVID-19 vaccine was approved for emergency use by the FDA in under a year. Additionally, treatments such as antiviral medications are now approved. With vaccines and pharmaceutical responses to COVID-19 available, localities within the USA have cautiously reopened their economies starting late 2021. This paper will look back and focus on the effectiveness and associated results of the initial NPI decisions made by governments in the first nine months of 2020 as the COVID-19 pandemic was heading to its first peak, prior to the availability of pharmaceutical intervention.
In “Background,” we provide further background information on the COVID-19 pandemic and various NPIs as well as our aggregate measures. In “Data,” we discuss the data. In “Descriptive Statistics, Methodology, and Results,” we share our summary statistics, methodology, and results. These results include alternative specifications, robustness checks, and results related to the racial and ethnic composition of counties. “Conclusion” will conclude.
Background
This section provides further background information about the COVID-19 pandemic and the NPIs that we focus on in this paper.
COVID-19
Across the USA, there were differences in when the virus first emerged, when deaths/cases peaked, and the number of deaths and cases. The first reported cases of COVID-19 in the USA occurred early in 2020. The first death attributed to COVID-19 was in Santa Clara County, California, on February 6, 2020 (Soucheray 2020). On March 11th, 2020, the World Health Organization (WHO) officially declared COVID-19 a pandemic, and 2 days later, the USA declared a national emergency (AJMC Staff 2021). Much of the initial spread of the virus within the USA occurred on the west coast and in the state of New York with other areas seeing deaths and cases increase in the summer of 2020.
Over this time, there was variation both between states and between counties within states in COVID-19 spread and severity as seen in Figs. 1 and 2. Figure 1 shows cases per 100,000 by county for our time period. Cases were concentrated in the southeast United States, California, and Washington state. Figure 2 shows deaths per 100,000 by county over our time period. Deaths occur frequently in the counties where we see a high number of cases, but also appear to occur more often in the Midwest and along the eastern seaboard. It is still an open question in the literature why these differences exist both between and within states. Due to the novelty of the virus, a vaccine would not be available for public use until December of 2020, after the time period we discuss in this paper (FDA 2020). To curb the speed of the spread of the virus, state and local governments turned to NPIs. These intervention strategies include mask mandates, daycare and school closures, restaurant and bar closures, and stay-at-home orders. We discuss NPIs in more detail in the section that follows.
Non-pharmaceutical intervention (NPI) is a blanket term for a wide variety of strategies used in an attempt to stall the spread of COVID-19 that do not involve the use of pharmaceutical technology. Many NPIs focus on reducing social interaction between infected and healthy individuals and slowing the spread of the virus to a more manageable rate. The virus is spread through exposure to respiratory fluids that are often released in the process of speaking, coughing, or breathing. The CDC recommendation based on this understanding is to maintain a distance of 6 ft between oneself and others (social distancing). The chances of exposure and infection can be further reduced by wearing a well-fitting mask over one’s mouth and nose (CDC 2020).
In addition to recommendations about social distancing and masking, further government policies were implemented at the state and county level to try to slow the spread of COVID-19. On March 13, 2020, the USA declared a national state of emergency, and 6 days later California became the first state to issue a stay-at-home order, mandating all residents to stay at home unless performing essential jobs or shopping for essential needs (AJMC Staff 2021). These stay-at-home orders were closely followed by mask mandates, the closure of businesses, and the closure of schools. Essential business closures and school closures reduce the number of in-person contacts that could increase the risk of spreading the virus among individuals. As an airborne infectious disease, it is likely that mask mandates, business and school closures, stay-at-home orders, and social distancing precautions may all be able to slow the spread of COVID-19 and could have played a critical role in easing pressures off of healthcare systems, slowing the spread, and saving lives as researchers worked to develop vaccines and other pharmaceutical treatments for COVID-19. Indeed, Grage et. al (2020) summarized the research published during 2020 and report more than 15 papers showing the effectiveness of NPIs in reducing the spread of COVID-19.
Putting restrictions on people and businesses has its own associated costs to individuals and the economy. There was much criticism of these policies due to both the economic toll and the mental health cost resulting from these isolating policies. Others were concerned about government overreach and infringements on liberty. Some states and counties began to lift their NPI orders within the time frame of our study. When policies are lifted, their benefits may linger for several days or weeks, as mobility from outside travelers is still reduced, and those within a region may continue to hold some hesitations about going out and putting themselves in harm’s way. However, after this initial lag, if policies are lifted prematurely, regions may see increases in COVID-19 spread that could negate the initial benefits seen by ever enacting the policy, effectively offsetting any benefits found in the first place (Singh et al. 2021). It should be the goal of policymakers to find the least costly intervention strategies that balance the adverse health effects of the pandemic and the economic and health costs of NPIs.
In this work, we focus on a measure of NPIs that aggregates mask mandates in public areas, daycare closures, school closures, bar and restaurant closures, and stay-at-home orders. Each of these NPIs is briefly described in the sections that follow.
Mask Mandates
Between April 8th and May 15th, 2020, fifteen governors and the mayor of Washington D.C. implemented mandatory mask mandates in public places such as grocery stores and public transportation. Mask mandates are used to prevent the spread of infectious particles while still allowing people to gather in public. Mask mandates allow people to continue to work, shop, gather, and travel. Masks should block some of the aerosolized virus and decrease the COVID-19 risk associated with participating in everyday activities.Footnote 2 In one of the first studies to look at the impact of mask mandates in real-time, Lyu & Weby (2020) found that early mask mandates led to a decrease in the growth rate in daily COVID-19 cases early in the pandemic. Guy et al. (2021) and Guzman-Cotrill et al. (2021) showed that mask mandates reduced county-level COVID-19 deaths and cases within 20 days of implementation.
Childcare/Daycare Closures, K-12 School Closures
Other efforts to stop the spread of COVID-19 included the closure of schools, child services, and daycare centers. Although at the time it was believed that children were not at high risk of severe complications from COVID-19, the concern was that children (particularly younger children) would struggle to follow social distancing and mask protocols and would spread the infection among themselves and then take COVID-19 home to their respective family members. Two-thirds of daycare centers were closed in April 2020, though government-mandated daycare closures were not as common as K-12 school closures (Lee & Parolin 2021). These closures create challenges for parents, employees, and the children themselves. Without adequate care options, many parents were left to juggle their own childcare on top of at-home work. Daycare employees faced loss of pay or their jobs. Without daycare and the opportunity to interact with peers, children missed out on valuable social interaction and learning opportunities.
Restaurant and Bar Closures
Restaurant and bar closures effectively limited adult social interaction within establishments that serve food and beverages. Additionally, many states put restrictions on in-establishment service for restaurants and bars. Some restaurants were forced to close altogether. Others pivoted toward take-out business with restricted hours. The CDC recommended that dining could be done safely through drive-throughs, take-out, outdoor seating, or masked and distanced dine-in measures (CDC 2021c). Over the time frame in question, in addition to mandated closures and restrictions on dine-in in restaurants, many restaurants permanently closed their doors due to the economic hardships faced within the industry. More than 110,000 restaurants and bars closed, leading to 2.5 million lost jobs (King 2021).
Stay-at-Home Orders
From March 1st to May 31st, 2020, 42 states and territories issued mandatory stay-at-home orders affecting 73% of all counties in the USA (Moreland et al. 2020). While more intrusive than other NPIs, stay-at-home orders make disease transmission much less likely and reduce in-person contact between individuals in different households. For instance, Dave et al. (2021) showed that stay-at-home orders reduced cumulative COVID-19 cases by 53.3% three weeks after implementation. A large reduction in travel between regions also reduces the spread of the disease. While stay-at-home orders have been found effective in preventing and mitigating the spread of COVID-19, this NPI has high costs (Fowler et al. 2021; Bongaerts et al. 2021). Stay-at-home orders stifle the economy and have been shown to have an adverse impact on mental health due to the isolation they impose. The associated financial struggles as well as an overall increase in stress and uncertainty contributed to the negative toll on individuals’ mental health. In January 2019, 1 in 10 Americans reported having feelings of anxiety and depression. This number increased to 4 in 10 adults during the pandemic. Amid job loss and social isolation, 36% of adults reported difficulty sleeping, and 12% claimed increases in alcohol consumption or substance use (Panchal et al. 2021). Furthermore, stay-at-home orders also changed consumer behaviors (Alexander and Karger 2020). Finally, Baek et al. (2021) showed the negative unemployment effects of stay-at-home orders.
Data
The sections that follow describe the data sources and transformations used to generate key variables utilized in the “Descriptive Statistics, Methodology, and Results” section.
Data Sources
This paper combines data from four main sources: (1) Covid Act Now, (2) the COVID-19 US State Policy Database, (3) the COVID-19 State and County Policy Order, and (4) County Health Rankings & Roadmaps. A description of each data source is below:
Covid Act Now
Covid Act Now is a volunteer-driven non-profit organization whose aim is to provide the best-available local-level disease intelligence and data analysis. Their model’s first version was published in March 2020 and has since provided information to individuals and governments. Covid Act Now collects daily data at the county level for all 50 states and over 3000 counties. The organization pulls data on deaths and cases from a wide range of sources including The New York Times, Covid County Data, and the COVID Tracking Project. These sources obtain their data from a combination of journalists, official state- and county-level dashboards, and state/district/territory public health authorities. For this paper, we utilize daily county-level time series data from January 21, 2020, to September 7, 2020, to examine COVID-19-related deaths and cases at the county level.
COVID-19 US State Policy Database
The COVID-19 US State Policy Database is developed and maintained by researchers at the Boston University School of Public Health. It tracks the dates of state-level NPI policy changes. They also maintain data on existing health and social policies and information on state-level population characteristics. The policy database is sourced from individual state government websites and reports (Raifman et al. 2020). Variables from this source are listed in Appendix Table 6.
COVID-19 State and County Policy Order
The COVID-19 State and County Policy Order database was provided by the US Department of Health and Human Services. Data are compiled and maintained from several sources and updated daily for public download. Variables of interest include the level at which an NPI is enacted or retracted, the date of action, and the state or county in which it took place (US Department of Health and Human Services, 2022). Variables from this data source are listed in Appendix Table 6.
County Health Rankings & Roadmaps
Country Health Rankings & Roadmaps (CHR&R) is a collaboration between the Robert Wood Johnson Foundation and the University of Wisconsin Population Health Institute. We use the “2020 County Health Rankings National Data” file. These data include measures of health for nearly every county in the nation by Federal Information Processing Standard (FIPS) code. Values are gathered from a variety of national and state-level data sources (Remington et al 2015). The variables we use from CHR&R and their original sources are listed in Appendix Table 7.
Data Transformation and Key Variables
We combine the data from Covid Act Now, CHR&R, and the two NPI databases discussed above into a cross-sectional dataset by county. Many of the county-level variables from CHR&R are used as is. However, we transform the Covid Act Now data and the NPI data. We discuss these transformations below.
Covid Act Now Data
To examine the COVID-19 data for the totality of the first wave we collapsed time series data into a cross-section. We do this because many of the right-hand side variables we use in this analysis are not time varying. The variables that we use or create from the Covid Act Now dataset include the following calculated over the time frame January 21, 2020, to September 7, 2020 (Labor Day): Total deaths, Total cases, Date of first death, Date of first case, Date of peak death, Date of peak case, and Cumulative deaths between first death and peak death, Cumulative cases between first case and peak case, time from first case to peak case, time from first death to peak death, and time from first case to peak death. From this time series of COVID data, we first look at the total deaths and total cases recorded within a county during our time frame. We normalize case and death data to be per 100,000 population to account for different counties having different population sizes. Next, we record the date of first death and date of first case for each county. We then construct a seven-day moving average of deaths and a seven-day moving average of cases. From here, we look at the peak 7-day moving average deaths and moving average cases before September 7, 2020.Footnote 3 We also record the date of peak death and date of peak case for each county. In counties where there are no deaths (586 counties) or no cases (17 counties) the date of peak death or case is coded as missing.Footnote 4 We then use these variables to construct two more variables of interest: cumulative deaths from first death to peak death which is the sum of all deaths from the beginning of our time frame up until the peak, and cumulative cases from first case to peak case, which is the sum of all cases from the beginning of our time frame up until the peak. These cumulative measures are also per 100,000 population. Finally, to analyze the distributional characteristics of cases and deaths, we constructed three variables that show the number of days from first case/death to peak case/death.
NPI data
The individual NPIs we focus on are mask mandates, daycare closures, restaurant and bar closures, and stay-at-home orders. For the intensity measures, we will also include school closures. For school closures, we do not have a reopening date given that we truncated the data at Labor Day. While many NPIs were implemented at the state level, some were implemented by counties. We have aggregated the state and county-level NPIs together and coded the county as having a particular NPI on the first date that it was implemented whether that was a county order or a state-level order.
65% of counties had a mask mandate. The average length of mask mandates within our time frame studied was 51.4 days. Twenty-three percent of counties had government-mandated daycare closures. The average length of these closures is 23 days. 98% of counties had a government-mandated restaurant or bar closure during the time period. The average length of these closures was 55 days. Seventy-one percent of counties implemented a stay-at-home order with an average length of around 38 days.
The variables created from the NPI data are as follows:
Length of NPI (lNPI) is the number of days between the implementation of the first NPI in a county and the removal of the first NPI in that same county, where the NPIs considered are mask mandates, restaurant and bar closures, stay-at-home orders, and daycare closures. We omit school closures here due to the complications introduced by the summer break.
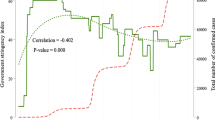
We then construct a measure of how intensively state and local governments implemented NPIs, NPI intensity in duration (NPI Days), is the sum of the number of days any NPI was implemented. For instance, a county that implemented a mask mandate for 37 days and bar closures for 52 and no other NPIs would have an intensity in duration measure of 89. The geographic distribution of variation of intensity in duration is in Fig. 3. Figure 3 shows the Midwest, northeast, and west coast states implemented NPIs for more NPI days. It should be noted that counties that implemented more NPIs for longer periods were also early epicenters of the pandemic and are generally the metropolitan areas.
Intensity of NPI total days (NPI days). Data source: Authors’ calculations from Boston University’s School of Public Health COVID-19 US State Policy Database and the US Department of Health and Human Services COVID-19 State and County Policy Order. Category bins are broken up into quartiles. 176–250 days of NPI intensity is the bottom 25%. 405–587 days of NPI intensity is the top 25%. Alaska (not pictured) has 26 counties at 268 intensity days, 2 counties at 271 intensity days, and 1 county at 274 intensity days. Hawaii (not pictured) has 4 counties at 468 intensity days and 1 county at 470 intensity days. Category bins are broken up into quartiles. 176–250 days of NPI intensity is the bottom 25%. 405–587 days of NPI intensity is the top 25%. Alaska (not pictured) has 26 counties at 268 intensity days, 2 counties at 271 intensity days, and 1 county at 274 intensity days. Hawaii (not pictured) has 4 counties at 468 intensity days and 1 county at 470 intensity days
Descriptive Statistics, Methodology, and Results
This section will discuss descriptive statistics for the data described in the previous section, provide a discussion of our methodology, and provide results.
Descriptive Statistics
Summary statistics for COVID-19-related outcomes are presented in the top panel of Table 1. The average number of deaths per 100,000 population in all counties over this time frame is around 36 whereas the cumulative deaths at peak is on average 21.24 per 100,000. The average number of cases per 100,000 population in all counties over this time frame is around 1557 while the cumulative cases at peak in these counties on average is almost 979 per 100,000. The average number of days to reach from the first case to peak cases was 110 days, while first death to peak death was only 46 days. We also examined the time from first case to peak death which was 77 days.
In the middle panel of Table 1, we present the descriptive statistics for NPIs. Our general measure of NPI (lNPI) has an average of 98 days of implementation. The duration of these NPIs (NPI Days) is 332 NPI days of implementation on average. To control for county- and state-level heterogeneity, we consider a host of county- and state-level characteristics including share of population that has fair/poor health, aged above 65, blacks, Hispanics, immigrants, females, population living in rural areas, children receiving free and reduced-price lunch as well as the number of physicians, median income, and the governing party of the state that the county is in. Few of those controls are particularly important to us. The share of blacks and Hispanics were important controls as these minority groups were impacted more adversely during the pandemic.
Methodology and Results
In this study, we answer a commonly voiced question of the public during the pandemic. Did longer mask mandates, daycare closures, restaurant and bar closures, and stay-at-home orders decrease the deaths and/or cases during the first phase of the pandemic? We use the model in Eq. 1 to estimate the impact of NPIs on the COVID-19-related outcomes discussed in the previous section.
Yc is one of the COVID-19 outcomes which are total deaths, total cases, and cumulative deaths and cases at peak. lNPI (length of NPI) is the number of days from the earliest intervention put in place until the first lifting of an NPI intervention.Footnote 5 Our estimation also includes controls for county- and state-level characteristics, i.e., prior health and health infrastructure at the county level, county demographics (share of people aged 65 or above, blacks and Hispanics, immigrants, and female), socioeconomic factors (median income and share of free or reduced-price lunch) at the county level, and the governor’s political affiliation. Additionally, we include the share of population within the county living in rural areas. To capture the time-invariant differences across regions, we also include Census region fixed effects.
One possible concern about the relationship between the COVID-19 outcomes and interventions is related to the potential endogeneity between these variables. It is conceivable that the implementation of the NPIs might be non-random. Aksoy et al. (2020) show that the implementation and timing of the NPIs are closely connected to public attention. States and counties in which the public is more informed are more likely to implement NPIs. Counties and states facing heightened levels of deaths and cases might be more willing to pass a mandate or policy to reduce the severity of the pandemic. To alleviate these endogeneity concerns, we implement an instrumental variable/two-stage least squares (2SLS) strategy, instrumenting for the NPI variable in Eq. 1. We identified a possible exogenous variable that is related to NPI implementation but not related to COVID-19 outcomes: religiosity of the states.Footnote 6 The religiosity variable shows the percentage of adults who say that religion is very important in their lives. In order for the instrument to be theoretically valid and appropriate we would want them to impact the implementation and duration of NPIs without impacting COVID-19 deaths or cases. One might think that counties with a higher level of religiosity may have different preferences in implementing government policies. At the same time, we would not expect religiosity to directly impact the spread of COVID-19. Indeed, first-stage estimations from this model (shown in Eq. 2) suggest that the religiosity instrument is statistically significant, confirming that the variable is a strong instrument. Diagnostic tests indicate that all COVID-19 outcomes are indeed endogenous and 2SLS is warranted.Footnote 7
Table 2 shows the second-stage estimates from the two-stage least squares estimations for our general NPI measure (length of NPI) that combines all mask mandates, daycare closures, restaurant and bar closures, and stay-at-home orders at the county and state levels. The variable measures the duration of the earliest interventions put in place until the first removal of an NPI. During the time period analyzed, all 3137 counties plus Washington D.C. had at least one of these interventions or closed schools. We present the results for the following four COVID-19-related outcomes: Total Deaths, Total Cases, Cumulative Deaths at Peak, and Cumulative Cases at Peak starting from a baseline estimation in column 1 of Table 2, which includes only a constant and the length of NPI (lNPI) measure as the regressors. We add county-level control variables in subsequent columns. In column 2, we add the prior health and health infrastructure measured by the share of population with poor/fair health prior to the pandemic as well as the number of primary care physicians per population in these counties. In column 3, we add demographic controls which include the share of the population that is over age 65, percent female, percent black, percent Hispanic, and percent immigrant at the county level. Socioeconomic controls including median income and the share of students that receive free or reduced-price lunch at school in these counties and are added in column 4. Finally, column 5, our full specification, includes a variable for rural share of the county and an indicator for the state-level governing party (political affiliation of the governor). Although data allow us to use state-level fixed effects, we opt for regional fixed effects as most of these NPI policies were implemented at the state level.
The results in Table 2 clearly indicate that these NPIs collectively reduced both the total and cumulative deaths and cases with the coefficients being statistically significant at conventional levels. The coefficients for “Total Deaths” and “Total Cases” in the last column (our preferred specification) are − 1.02 and − 15.28 respectively, suggesting that an additional day of NPI implementation before removing the first NPI decreased the deaths and cases by more than one per one hundred thousand (2.81%) and fifteen per one hundred thousand (1.28%) respectively. Our results are in line with the findings of Amuedo-Dorantes et al. (2020) who found that an additional day of NPI adoption lowers the COVID-19 death rate by 2.4 percent. The NPIs also successfully decreased the “Cumulative Deaths at peak” by approximately 0.58 per 100,000 for each additional day of implementation, suggesting that state and county-level mandates collectively helped relieve some of the pressure on the healthcare system during the initial stages of the pandemic in each county. Length of NPI (lNPI) does not have a statistically significant impact on “Cumulative Cases at Peak”. For brevity, we do not report the coefficients and their statistical significance of the control variables, but it is important to note that deaths and cases (both total and cumulative at peak) are higher in counties that did not fare well health-wise prior to the pandemic. In addition, COVID-19 outcomes (deaths and cases) are worse in counties with larger shares of blacks, Hispanics, and immigrants and in counties in states with Republican governors. Results related to blacks and Hispanics are especially relevant as literature frequently showed that these minority groups did not fare well during the pandemic, even after controlling for socio-economic factors.
One strength of our data is that we are able to examine if these policies were effective at “flattening the curve.” We can combine the information in Table 2 regarding total deaths and cases at peak and cumulative deaths and cases at peak with information regarding how long it took (number of days) for each county to get from its first case/death to the peak case/death. We will look at these alternative measures of the distribution of cases and deaths in Table 3. A positive coefficient is expected if these policies do in fact flatten the curve.
We estimate our full specification with prior health, demographics, socioeconomic, and location-specific controls, similar to the last column of Table 2; however, this time, our COVID-related outcomes are (1) time from first case to peak case in column one, (2) time from first death to peak death in column 2, and (3) time from first case to peak death in column 3. These variables are expected to capture the distributional characteristics of the spread of COVID-19. They look beyond the pure case and death numbers related to COVID; and they are more informative in terms of capturing the rush for the healthcare services, especially during the initial stages of the pandemic when hospital beds were scarce. Again, these variables allow us to test whether non-pharmaceutical interventions indeed flattened the curve, and prevented early rushes to the hospitals, which was one of the main expected benefits of early NPI interventions. Our results suggest that, although NPIs decreased the deaths and cases, the NPIs did not “flatten the curve,” i.e., did not decrease the rush to the hospitals. In fact, we found negative and statistically significant coefficients on NPIs for time from first death to peak death and first case to peak death as shown in columns 2 and 3 of Table 3.
Those counties that implemented NPIs longer have faster times to reach their peak deaths. This can be explained by two possible factors. One might be related to health professionals’ ability to combat the pandemic in counties that reached peak deaths at the early stages of the pandemic. In the early months of the pandemic, health professionals had limited tools and knowledge to contain the virus where the death toll was significantly higher. It is possible that some of the counties who reached peaks early might be those who implemented NPIs longer. The second possible explanation is non-uniform implementation of NPIs. Our data shows that some counties implemented NPIs early, while others implemented later; yet some never. It is conceivable that counties that implemented NPIs proactively might be those that are more likely to be hit hard by COVID, either because of the socioeconomic composition or racial/ethnic composition of the county.
Next, we turn our attention to an alternative definition of NPI. As mentioned in the previous section, different counties implemented NPIs with different levels of intensities. We use an alternative measure of NPI intensity (NPI Days) that adds together the number of days that each county had each specific NPI in place. For example, a county that implemented a mask mandate for 37 days and bar and restaurant closures for 52 days would have an intensity in duration measure of 89 NPI Days.
In Table 4, we present the results for the NPI intensity (NPI Days). While our first measure examines the length of time from the first policy implementation to the first removal of an NPI policy, this measure relies on the total duration of each NPI intervention and as such, provides a measure of policy intensity within a county over the time frame. We call this measure of NPI days. As shown in Table 1, the mean value of this intensity measure, which is the sum of the number of days each of the five interventions is in place, is 332.6 with a minimum of 176 and a maximum of 587. It is clear that there is a great level of variation in the intensity of NPI policy used by states and counties. We expect the higher the number of NPI Days, the more intense the government intervention; therefore, more reductions in deaths and cases during the first wave of the pandemic. The results suggest that one day longer implementation of a single NPI reduced the total and cumulative deaths at peak by 0.12 per 100,000 and 0.07 per 100,000 while it decreased the total and cumulative cases at peak by 5.8 per 100,000 and 3.3 per 100,000, respectively. This confirms our hypothesis that these interventions were effective and the intensity of implementation had an impact on deaths and cases during the first phases of the pandemic when pharmaceutical intervention for COVID-19 was not readily available. Our results have important policy implications. Not only implementing an NPI reduces the adverse health effects of the pandemic, but also the intensity of those NPIs matters according to our estimations. Policymakers can benefit from early intervention, longer implementation of NPIs, and instituting a variety of NPIs in response to a pandemic.
Finally, we focus on minority racial and ethnic groups. Previous literature including Yancy (2020) and Lee (2021) shows that minority racial and ethnic groups in the USA are impacted more adversely by the pandemic. Indeed, if one important contribution of this work is examining the effectiveness of NPIs, the second important aspect of our work is how these policies interact with the racial and ethnic composition of localities. The fundamental and natural question, then, would be whether these NPIs were effective in counties where these racial and ethnic populations are more concentrated. For this purpose, we revise Eq. 1 by interacting the non-pharmaceutical intervention variables with the share of blacks or Hispanics as shown below:
Because we are using the 2SLS estimation method, in addition to our original instrument of religiosity, we include the interaction of the instrument with the share of population in the county that is black or Hispanic in the first-stage estimations. We repeat this exercise for both NPI measures: length of NPI and the NPI Days. Table 5 has 8 columns (the first four columns are for length of NPI while the last four are for NPI Days) that show the four COVID-19 outcomes, namely total deaths, total cases, cumulative deaths at peak, and cumulative cases at peak. The results for blacks are presented on the top panel of Table 5 while the results for Hispanics can be found in the bottom panel.
The top panel of Table 5 shows the results for the 2SLS estimation as shown in Eq. 3 for blacks. Along with the coefficient on the length of NPI, we present the coefficient on the interaction between the length of NPI and race/ethnicity. The results are similar to those presented in Table 4 for the length of the NPI coefficient, negative and statistically significant suggesting that the implementation of NPIs curbs the impact of the pandemic, with the exception of cumulative cases. The interaction variable between NPI and race/ethnicity is statistically insignificant for deaths (column 1), suggesting that there is no statistically significant differential impact of the length of NPIs on deaths in counties with a higher share of blacks. The same can be said for cumulative deaths at peak (column 3). However, we do see a statistically significant and negative result for cases and cumulative cases at peak (columns 2 and 4). This suggests that implementing NPIs for a longer duration in counties with a larger share of blacks led to a decrease in overall cases. The same general pattern holds when we examine the impact of NPI days with some mixed results for deaths. In terms of deaths, there is a statistically significant difference in the impact of NPI days on deaths or cumulative deaths at peak for blacks (columns 5 and 7) and it is contrary to our a priori expectations with a positive coefficient. These results suggest that counties with stricter non-pharmaceutical interventions where NPI days are longer with a higher share of blacks experienced higher deaths and cumulative deaths. However, the impact of NPI days interacted with the share of black population on cases shows a statistically insignificant result in column 6. However, there is a statistically significant negative result on cumulative cases (columns 8), implying that in counties with a larger share of black population, that had more intense implementation of NPIs helped to mitigate the number of cumulative cases at peak, but policy intensity did not have any impact on total cases.
The bottom panel of Table 5 shows the results for the 2SLS estimation as shown in Eq. 3 for Hispanics. These results are also very similar to Table 4, particularly in terms of the coefficients of NPI-related measures. However, unlike the blacks, the effectiveness of these interventions is more moderate in counties with larger shares of Hispanics. The coefficients on the interaction terms are positive and statistically significant, implying that, while there is an initial negative impact of the length of NPI and intensity of NPI (NPI Days), this impact is weaker in counties with higher proportions of the Hispanic population.
It is important to discuss why counties with larger shares of blacks have higher effectiveness of NPIs while these policies are less effective in counties with a larger share of Hispanics even after controlling for socio-economic, demographic, and geographic factors. One possible explanation is labor market sorting of these racial ethnic groups. If in fact these racial and ethnic groups sort themselves into jobs that require more interaction between employees and customers with less ability to work from home, or jobs that are more likely to be deemed “essential” and continue going to work during a stay-at-home order or implementation of our other NPIs, this would lead to higher risk for these populations and potentially a higher rate of transmission. Selden and Berdahl (2020) showed that 64.5% of Hispanics with a high risk of severe illness lived in households with at least one worker who is unable to work from home. Furthermore, they found that more Hispanics compared to whites work in food-related jobs. In this case, we would expect to see differential impacts in counties with different racial/ethnic makeups.
Conclusion
COVID-19 has been one of the deadliest and most disruptive pandemics of the modern day. The impact and spread of the virus and the impact of interventions to control the virus have been examined thoroughly by the researchers for the last 2 years. This paper looks at the early stages of the pandemic, from the first case through the end of the summer of 2020, examining the non-pharmaceutical interventions that states and counties implemented to reduce the spread of the virus in the absence of pharmaceutical interventions. The period in question has been an interesting, yet very uncertain one, as policymakers scrambled to identify and implement mandates with the intention of protecting the public, delaying the patient surges in the healthcare system, and reducing the flow of cases into hospitals when hospital beds and ventilators were scarce. These state and county-imposed interventions and policies varied but the most common ones were mask mandates, school/daycare closures, restaurant and bar closures, and stay-at-home orders. At the time of the implementation of these NPIs, the public was unsure of the effectiveness of these interventions. Many questioned the necessity of these policies and whether the costs outweigh the benefits. Some parts of the country showed strong opposition to the implementation of these policies. This paper aims to examine the effectiveness of these policies at reducing COVID-19-related deaths and cases.
We use publicly available county-level COVID-19 outcome data, namely total deaths and cases per 100,000 as well as cumulative total deaths and cases at peak per 100,000 to analyze the impact of the most commonly used NPIs. We were also able to analyze distributional characteristics of the cases and deaths analyzing the time to first case/death to peak case/death; effectively testing the “flattening the curve” argument of the policymakers at the early stages of the pandemic. The NPIs included in this study are mask mandates, school/daycare closures, restaurant and bar closures, and stay-at-home orders. We examine the duration of NPI from the first implementation to the lifting of the first NPI. We also analyze the impact of the intensity of duration of NPIs (NPI Days). We estimate a two-stage least squares regression model using cross-sectional county-level data on these outcomes and interventions for more than three thousand counties. Our results suggest that longer NPI duration reduced deaths and cases. More intense policy responses from local governments are associated with fewer deaths and cases, as well as lower peaks for deaths and cases. We also find that these policies were not successful in lengthening the time to the peak or redistributing the timing of cases and deaths within a county or “flattening the curve,” This study also extends to the analysis of differential impacts based on the county proportion of racial and ethnic minorities. It is important to examine how the racial and ethnic composition of a county may have led to differential impacts of NPIs as minority racial and ethnic groups were found to be more adversely impacted by the pandemic. Our results suggest that in counties where Hispanics and blacks are more concentrated, NPIs continued to be effective. However, these impacts are moderated in counties with large numbers of Hispanics.
One of the important aspects of our study is that we focus on the first wave of the pandemic. Since September 2020, there have been multiple other waves. Caution should be used when extrapolating these results to other time periods and settings. Additionally, we do not speak to the impact of vaccines, as these were approved after the conclusion of our time period. However, our goal is to examine the efficacy of these early policy responses by state and local governments when NPIs were the only policy option. This is a unique time period to study because we know that vaccines are not confounding our results.
One weakness of this study is that we are using the data as a cross-section instead of as a time series. This is because we seek to examine the impact over the time period of the first wave and to examine whether or not these policies succeeded in flattening the curve. Additionally, many of our control variables are not time varying. It is true that we are losing a lot of information about the progression of COVID-19 within the individual counties during the first wave by treating the data as a cross-section. Furthermore, our cross-section approach prevents us to analyze the steep learning curve of healthcare professionals who quickly identified and implemented lifesaving treatment approaches especially during the summer months of 2020. This time series analysis aspect of the pandemic is left to future work.
Our paper shows that NPIs, early intervention, longer implementation of NPIs, and instituting a variety of NPIs, were effective in reducing deaths and cases during the first wave of the COVID-19 pandemic. In case of another pandemic that spreads via aerosols, these policies should be considered options to help mitigate the spread of disease. That said, all policy options also have costs and policymakers should consider both the benefits (reduced deaths and cases) and costs of any future NPI policy. Our results also suggest that the effectiveness of policies may depend on the racial and ethnic composition of a county. Given our argument about labor market sorting, policymakers should think about both racial composition and employment mix within their county. Will many of their citizens actually be able to stay home if a stay-at-home order is issued? If not, they may want to focus on other NPIs such as mask mandates or other novel NPI strategies.
Data Availability
Data are publicly available at the sources described in the text.
Notes
For the most recent COVID-19 deaths and cases, “WHO Coronavirus (COVID-19) Dashboard.” World Health Organization, World Health Organization, https://covid19.who.int/.
For complete list of these mask mandates, see: https://ballotpedia.org/State-level_mask_requirements_in_response_to_the_coronavirus_(COVID-19)_pandemic,_2020-2021#Mask_requirements_over_time
We use the 7-day moving average to account for differences in testing intensity and reporting on the weekends.
If more than one date has the same moving average within a county, we pick the earliest date.
One limitation of the estimation model is the assumption of the linear impact of duration of an intervention. It is possible to estimate this model with a duration squared to account for non-linear response of outcomes.
Religiosity data are from https://www.pewresearch.org/fact-tank/2016/02/29/how-religious-is-your-state/ accessed 05–15-22.
First-stage estimation results can be found in the Appendix Table 8.
References
AJMC Staff. A timeline of COVID-19 developments in 2020. 1 Jan. 2021, https://www.ajmc.com/view/a-timeline-of-covid19-developments-in-2020. Accessed 5 Sept 2021.
Aksoy CG, Ganslmeier M, Poutvaara P. Public attention and policy responses to COVID-19 pandemic. Working Paper. 2020. Retrieved from https://ideas.repec.org/p/ces/ceswps/_8409.html. Accessed 14 Nov 2021.
Alexander D, Karger E. Do stay-at-home orders cause people to stay at home? Effects of stay-at-home orders on consumer behavior (Revised May 2020). Working Paper. 2020. Retrieved from https://doi.org/10.21033/wp-2020-12.
Amuedo-Dorantes C, Kaushal N, Muchow AN. Is the cure worse than the disease? County-level evidence from the COVID-19 pandemic in the united states. Working Paper. 2020. Retrieved from. https://www.econstor.eu/handle/10419/227222. Accessed 14 Nov 2021.
Baek CW, McCrory PB, Messer T, Mui P. Unemployment effects of stay-at-home orders: evidence from high frequency claims data. Rev Econ Stat. 2021;5:979–93. https://doi.org/10.1162/rest_a_00996.
Benitez J, Courtemanche C, Yelowitz A. Racial and ethnic disparities in COVID-19: evidence from six large cities. J Econ Race Policy. 2020;3:243–61. https://doi.org/10.1007/s41996-020-00068-9.
Bongaerts D, Mazzola F, Wagner W. Closed for business: the mortality impact of business closures during the COVID-19 pandemic. PLOS ONE. 2021. https://doi.org/10.1371/journal.pone.0251373.
CDC calls on Americans to wear masks to prevent COVID-19 spread. Cent Dis Control Prev. 2020. https://www.cdc.gov/media/releases/2020/p0714-americans-to-wear-masks.html. Accessed 1 Nov 2021.
Considerations for restaurant and bar operators. Cent Dis Control Prev. 2021c. https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/business-employers/bars-restaurants.html. Accessed 14 Nov 2021
Dave D, Friedson A, Matsuzawa K, Sabia JJ. When do shelter-in-place orders fight COVID-19 best? Policy heterogeneity across states and adoption time. Econ Inq. 2021;59(1):29–52. https://doi.org/10.1111/ecin.12944.
FDA takes key action in fight against COVID-19 by issuing emergency use authorization for first COVID-19 vaccine. U.S. Food Drug Adm. FDA. 2020. https://www.fda.gov/news-events/press-announcements/fda-takes-key-action-fight-against-covid-19-issuing-emergency-use-authorization-first-covid-19. Accessed 5 Sept 2021.
Felter C. By how much are countries underreporting COVID-19 cases and deaths? Counc Foreign Relat. 2021. https://www.cfr.org/in-brief/how-much-are-countries-underreporting-covid-19-cases-and-deaths. Accessed 1 Nov 2021.
Fowler JH, Hill SJ, Levin R, Obradovich N. Stay-at-home orders associate with subsequent decreases in COVID-19 cases and fatalities in the United States. PLOS ONE. 2021. https://doi.org/10.1371/journal.pone.0248849.
Grage L, Hennessy T, Bulkow L. Review of non-pharmaceutical interventions on transmission reduction for COVID-19. 2020. Retrieved from https://www.muni.org/Covid-19/Documents/20200814_UAA%20White%20paper%20on%20Transmission%20reduction%20of%20NPI%20Aug%2014.pdf. Accessed 14 Nov 2021.
Guy Jr. GP, Lee FC, Sunshine G, McCord R, Howard-Williams M, Kompaniyets L, Dunphy C, Gakh M, Weber R, Sauber-Schatz E, Omura JD, Massetti GM. Association of state-issued mask mandates and allowing on-premises restaurant dining with county-level COVID-19 case and death growth rates — United States, March 1–December 31, 2020. MMWR. Morb and Mortal Wkly Rep 70. 2021. https://doi.org/10.15585/mmwr.mm7010e3.
Guzman-Cottrill JA, Malani AN, Weber DJ, Babcock H, Haessler SD, Hayden MK, Henderson DK, et al. Local, state and federal face mask mandates during the COVID-19 pandemic. Infect Control Hosp Epidemiol, 2021;1–2. https://doi.org/10.1017/ice.2020.1403.
Hill L, Artiga S. COVID-19 cases and deaths by race/ethnicity: current data and changes over time. Kaiser Fam Found. 2022. https://www.kff.org/coronavirus-covid-19/issue-brief/covid-19-cases-and-deaths-by-race-ethnicity-current-data-and-changes-over-time/. Accessed 24 Nov 2022.
King R. More than 110,000 eating and drinking establishments closed in 2020. Fortune. 2021. https://fortune.com/2021/01/26/restaurants-bars-closed-2020-jobs-lost-how-many-have-closed-us-covid-pandemic-stimulus-unemployment/. Accessed 25 Nov 2022.
Lee EK, Parolin Z. The care burden during COVID-19: a national database of child care closures in the United States. Socius. 2021. https://doi.org/10.1177/23780231211032028.
Lee FC. Counties with high COVID-19 incidence and relatively large racial and ethnic minority populations — United States. April 1–December 22, 2020. MMWR. Morb Mortal Wkly Rep 70. 2021. https://doi.org/10.15585/mmwr.mm7013e1.
Lyu W, Wehby GL. Community use of face masks and COVID-19: evidence from a natural experiment of state mandates in the US. Health Aff. 2020;39(8). https://doi.org/10.1377/hlthaff.2020.00818.
Moreland A, Herlihy C, Tynan MA, et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement - United States, March 1–May 31, 2020. Cent Dis Control Prev. 2020. https://doi.org/10.15585/mmwr.mm6935a2.
Panchal N, Kamal R, Cox C, Garfield R. The implications of COVID-19 for mental health and substance use. Kaiser Family Foundation Issue Brief. 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/. Accessed 5 Sept 2021.
Raifman J, Nocka K, Jones D, Bor J, Lipson S, Jay J, Chan P. COVID-19 US state policy database. 2020 Available at: www.tinyurl.com/statepolicies. Accessed 30 Sept 2021.
Remington PL, Catlin BB, Gennuso KP. The county health rankings: rationale and methods. Popul Health Metrics. 2015;13:11. https://doi.org/10.1186/s12963-015-0044-2.
Risk for COVID-19 infection, hospitalization, and death by race/ethnicity. Cent Dis Control Prev. 2021b, https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Accessed 1 Nov 2021.
Selden TM, Berdahl T. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Aff. 2020;39:9. https://doi.org/10.1377/hlthaff.2020.00897.
Scientific brief: SARS-CoV-2 transmission. Center for Disease Control and Prevention. Updated 7 May 2021a. https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html. Accessed 14 Nov 2021.
Singh S, Shaikh M, Hauck K, Miraldo M. Impacts of introducing and lifting nonpharmaceutical interventions on COVID-19 daily growth rate and compliance in the United States. PNAS. 2021;118 (12). https://doi.org/10.1073/pnas.2021359118.
Soucheray S. Coroner: first US COVID-19 death occurred in early February. CIDRAP News, University of Minnesota Center for Infectious Disease Research and Policy. 2020. https://www.cidrap.umn.edu/news-perspective/2020/04/coroner-first-us-covid-19-death-occurred-early-february. Accessed 1 Nov 2021.
The University of Wisconsin Population Health Institute. County Health Rankings & Roadmaps 2020. www.countyhealthrankings.org.
U.S. Department of Health and Human Services. COVID-19 State and Country Policy Orders 2022. https://healthdata.gov/dataset/COVID-19-State-and-Country_Policy-Orders/gyqz-9u7n
Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19):1891. https://doi.org/10.1001/jama.2020.6548.
Acknowledgements
The authors would like to acknowledge two anonymous referees and the editor for their thoughtful comments as well as participants at the 2021 Southern Economic Association Meeting.
Author information
Authors and Affiliations
Contributions
AS, MY, and JO wrote the main manuscript text. AS, MY, and JO handled data cleaning. AS and MY handled data modeling and execution. JO prepared Figs. 1 − 4. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical Approval and Consent to Participate
Not applicable.
Human and Animal Ethics
Not applicable.
Consent for Publication
All authors consent to publication at JERP.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stype, A.C., Yaya, M.E. & Osika, J. Non-pharmaceutical Interventions and COVID-19: Do County- and State-Level Policies Predict the Spread of COVID-19?. J Econ Race Policy 6, 126–142 (2023). https://doi.org/10.1007/s41996-022-00112-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41996-022-00112-w