Abstract
Background
Since there is no diet that is perfect for everyone, personalized nutrition approaches are gaining popularity to achieve goals such as the prevention of obesity-related diseases. However, appropriate choices about funding and encouraging personalized nutrition approaches should be based on sufficient evidence of their effectiveness and cost-effectiveness. In this study, we assessed whether a newly developed personalized plan (PP) could be cost-effective relative to a non-personalized plan in Denmark.
Methods
Results of a 10-week randomized controlled trial were combined with a validated obesity economic model to estimate lifetime cost-effectiveness. In the trial, the intervention group (PP) received personalized home-delivered meals based on metabolic biomarkers and personalized behavioral change messages. In the control group these meals and messages were not personalized. Effects were measured in body mass index (BMI) and quality of life (EQ-5D-5L). Costs [euros (€), 2020] were considered from a societal perspective. Lifetime cost-effectiveness was assessed using a multi-state Markov model. Univariate, probabilistic sensitivity, and scenario analyses were performed.
Results
In the trial, no significant differences were found in the effectiveness of PP compared with control, but wide confidence intervals (CIs) were seen [e.g., BMI (−0.07, 95% CI −0.51, 0.38)]. Lifetime estimates showed that PP increased costs (€520,102 versus €518,366, difference: €1736) and quality-adjusted life years (QALYs) (15.117 versus 15.106, difference: 0.011); the incremental cost-utility ratio (ICUR) was therefore high (€158,798 to gain one QALY). However, a 20% decrease in intervention costs would reduce the ICUR (€23,668 per QALY gained) below an unofficial gross domestic product (GDP)-based willingness-to-pay threshold (€47,817 per QALY gained).
Conclusion
On the basis of the willingness-to-pay threshold and the non-significant differences in short-term effectiveness, PP may not be cost-effective. However, scaling up the intervention would reduce the intervention costs. Future studies should be larger and/or longer to reduce uncertainty about short-term effectiveness.
Trial Registration Number
ClinicalTrials.gov registry (NCT04590989).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We found that the short-term effectiveness of a personalized nutrition plan compared with a non-personalized plan was limited. However, we saw that there was large uncertainty regarding effectiveness, which could be reduced by making trials longer or larger. |
The combination of modest short-term effectiveness and the extra costs of personalization resulted in unfavorable cost-effectiveness estimates over a lifetime. Scaling up personalized nutrition interventions would reduce per-patient costs and thereby make them more cost-effective. |
1 Introduction
Overweight [body mass index (BMI) ≥ 25 kg/m2] and obesity (BMI ≥ 30 kg/m2) are growing public health problems [1]. Globally, the prevalence of obesity has nearly tripled between 1975 and 2016 [1]. Moreover, research from the Organization for Economic Cooperation and Development (OECD) shows that the average rates of adult obesity in OECD countries has risen from 21.3% in 2010 to 24.0% in 2016; this corresponds to an additional 50 million people with obesity [2]. Additionally, in 34 out of 36 OECD member countries, more than half of the population is now overweight [2]. A higher BMI is in turn a major risk factor for non-communicable diseases, such as cardiovascular diseases (the leading cause of death in 2012), diabetes, musculoskeletal disorders, and some cancers [1]. These diseases and obesity itself will reduce the average life expectancy by 2.7 years across OECD countries over the period 2020–2050 [2]. Because of these related diseases and the direct negative effect of overweight and obesity on physical ability and mental health (e.g., stress, depression, and anxiety) [3,4,5], people may be hampered in their capacity to perform their daily activities. Altogether, these negative physical and mental conditions reduce health-related quality of life (HRQoL) [6, 7]. Fortunately, studies have shown that weight loss is associated with improved HRQoL [7,8,9].
In addition to the huge global health problems caused by overweight and obesity, these conditions also pose a serious threat to the economy [2]. On average, 8.4% of the health budget of OECD countries is spent on treating the consequences of obesity [2, 10]. In the USA this number is even higher, at 14% of the health budget [2]. Besides healthcare costs, obesity has a rising impact on other social costs as well, such as patient and family costs and productivity losses [11, 12]. Lifetime productivity losses are almost twice as high in the obesity population compared with normal weight populations [11].
A well-balanced healthy diet is one of the key factors to prevent overweight, obesity, and related diseases [2]. Several studies showed relationships between dietary patterns and significant changes in BMI over time [13,14,15]. Countries have therefore implemented different policies to tackle overweight and obesity, including those targeting diets [2]. However, obesity is a complex multifactorial disorder, which makes its management a challenging task [16]. One single ‘perfect’ diet suitable for everyone may not exist because of the interindividual variation in a dietary treatment response (i.e., how the body utilizes and metabolizes nutrients), due to multiple phenotypic factors and genetic variants [17,18,19]. Therefore, there is an increasing demand for studies investigating personalized nutrition approaches, rather than approaches on a population level [20]. Personalized nutrition could be defined as “an approach that uses information on individual characteristics to develop targeted nutritional advice, products or services” [20]. Several studies have already proven the effectiveness of personalized nutrition, but they have not yielded consistent findings [21, 22]. For example, the Food4Me study did not find significant gene–diet interaction effects on body weight but did find more appropriate changes in dietary behavior in a personalized nutrition group versus a control group (a non-personalized intervention) [23]. Moreover, Zeevi et al. [24] showed that personalized diets created with an accurate predictor of blood glucose response, considering dietary habits, physical activity, and gut microbiota, may successfully modify elevated postprandial blood glucose and its metabolic consequences.
Although there is a growing interest in advanced omics technologies to facilitate holistic approaches to biological problems (e.g., metabolomics, transcriptomics, and genomics), there is a need for a simple, effective, and affordable personalized nutrition tool that integrates these technologies with other nutritional and psychological aspects [25]. To address this need, the PREVENTOMICS project (Horizon 2020: no. 818318) took an innovative approach by integrating genetic, nutritional, and psychological sciences with state-of-the-art metabolomics technologies and computational modeling. The outcome of this project was a comprehensive platform that includes a decision support system (DSS) [25, 26]. This platform effectively combines genetic, nutritional, biochemical, physiological, and behavioral factors and utilizes machine learning techniques to provide personalized dietary recommendations [24, 25]. This study reports the results of the Danish intervention, in which the platform is integrated in an e-commerce digital tool created for delivering personalized meals plus a behavioral change program (i.e., personalized plan, PP) to sustainably improve the health status of people with overweight or obesity and thereby prevent obesity-related diseases [26]. Effectiveness results showed that the PP intervention did not significantly improve health measures beyond those produced by the control (non-personalized) intervention [27]. However, the wide confidence intervals (CIs) around the effectiveness estimates (e.g., effect in BMI of PP versus control: −0.07, CI 95% −0.51, 0.38) shows that the PP nutrition may still be more effective than a non-personalized intervention.
In addition to activities to assess the evidence regarding the effectiveness of personalized nutrition interventions, it is important to assess the cost-effectiveness of these interventions, since policymakers expect evidence of cost-effectiveness when making reimbursement decisions. There is still a lack of cost-effectiveness literature relating to newly developed personalized nutrition interventions that specifically focus on omics-based personalized nutrition [28]. This is, however, especially crucial to evaluate, given the potentially higher estimated costs of using omics technologies to personalize interventions [29]. An economic evaluation can help to shed light on whether this intervention might potentially be cost-effective. Such information is especially important at this stage of first integration of the intervention, as it can help to inform developers of personalized nutrition interventions, as well as possible payers of the interventions. The aim of this study is therefore to evaluate the potential cost effectiveness of the PP intervention versus a control intervention (non-personalized) in adults with overweight and obesity in Denmark.
2 Methodology
2.1 Overall Study Design
Results regarding clinical and health outcomes from a clinical trial in Denmark (i.e., short-term results) (registered at clinicaltrial.gov (NCT04590989) were analyzed and then used to estimate the long-term effects, costs, and cost-effectiveness of the PP intervention versus control, using a validated obesity cost-effectiveness model [30]. The Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement was followed [31].
2.2 Study Population
The study population included in these analyses was based on the population included in the Danish trial within the PREVENTOMICS project. Participants in this intervention were women and men aged 18–65 years with overweight or obesity (BMI of 27 kg/m2 but < 40 kg/m2) and had no chronic diseases (e.g., diabetes and cancer) [26, 27].
2.3 Trial Description
The Danish trial was a 10-week randomized, single-center, parallel-group, double-blinded intervention study [26, 27]. The study had two intervention arms: PP and control. Participants were allocated in a 1:1 ratio, that was stratified by five ‘clusters’ to either PP or control. The clusters involved were oxidative stress, inflammation, carbohydrate metabolism, lipid metabolism, and microbiota-generated metabolites [25]. Information into which cluster to classify the participant was gathered from a metabolome analysis of 51 biomarkers quantified from urine, plasma, and serum samples taken during the pre-baseline visit. Moreover, saliva analysis of 35 different single nucleotide polymorphisms was used, since they could affect the biomarker levels associated with the five clusters [26, 27]. Together, the biomarkers and saliva analysis provided a score for each cluster. This was done by using proprietary algorithms for any participant where both the absolute value of the biomarker in the biofluid and the biological relevance of the biomarker in the metabolic cluster were considered.
The PP group and the control group received easy-to-prepare boxed meals twice a week (12 meals/week) from Simple Feast (Copenhagen, Denmark); all meals were plant-based [26, 27]. Both groups received meals that were isocaloric and complied with the national dietary guidelines on macronutrient distribution [32]. Moreover, the food items included in the boxes for the PP group were based on a list created as part of the project, which differed between clusters. One meal box included both breakfast and dinner for 3 days, delivered twice a week, meaning that for the days for which meals were not provided (Saturdays) as well as for lunches, participants were referred to the Simple Feast Recipe App. The number of meals provided to the participants was determined using a combination of factors, including budgetary limitations, practical reasons, and behavioral factors. In this app they were shown a set of recommended recipes so they could prepare meals as similar as possible to the group and cluster to which they were assigned. Meals in the PP group also included some bioactive compounds (i.e., functional ingredients); the compounds were especially (or exclusively) beneficial for the metabolic function of individuals corresponding to a cluster. Additionally, both groups (PP and control) received a behavioral program delivered through Onmi’s app, which is a behavior change technology aimed to increase behavioral flexibility and to facilitate adoption of healthier habits [33]. During this program, participants received 2–3 electronic push notifications per week. In the PP group, participants received active “do’s” (behavioral prompts) from the predefined Onmi’s evidence-based behavioral change program. The do’s were based on participants’ individual behavior, assessed by questionnaire, and inputs from Eurecat’s Nutrition team via the PREVENTOMICS platform. For example, suppose a participant received a recommendation to include kale and Brussels sprouts in their diet. In that case, they might receive a message such as: ‘Our analysis shows kale and Brussels sprouts are good for you and should be part of your diet. Find out how much you should be consuming. Do it now’ [26]. The control group received general messages, which were not given to prompt participants to take a specific action, but mostly informational in nature (i.e., messages based on general guidelines from the National Health Service and the World Health Organization) [26]. See Supplement 1 for more details about the different behavioral messages for the PP and the control group. More details about the trial protocol can be found elsewhere [26].
2.4 Short-Term Costs and Effects
2.4.1 Effects
Different health outcomes were derived from measurements at baseline and follow-up, of which BMI was one [27]. Information about quality of life was also measured by the EuroQol five-dimension questionnaire with five levels (EQ-5D-5L) [34]. The questionnaire was completed online in Danish. The EQ-5D-5L consists of five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression, with five response levels per dimension; an EQ-5D index score (0 can be considered equal to death and 1 full health) was calculated by using a country specific value set [35, 36]. The EQ-5D-5L also includes a Visual Analogue Scale (EQ VAS), by which respondents report their perceived health status [35].
Statistical analyses were performed using STATA 17 software [37]. Participants’ baseline characteristics were described using descriptive statistical analyses. Possible differences between the PP and control groups were also assessed. In case of normal distributed data, an independent t-test was used to test for differences between groups, while the Mann–Whitney U test was used in case of non-normality data. The chi-squared test was used to test for differences regarding categorical variables. Linear mixed models (LMMs) were used to quantify the differences in BMI effects between the PP and control group (i.e., difference in outcome measures between baseline and follow-up) [38]. The participant’s identification was included as random intercept, while all other covariates were included as fixed effects [(i.e., time of measurement (visit), intervention group (PP versus control), interaction between time and intervention]. Sex and age were included as fixed covariates as well. The two-tailed significance level was set at α = 0.05. Restricted maximum likelihood (REML) was used to fit LMMS to accommodate missing values at random within a single response variable among the participants’ data [39]. For analyzing EQ-5D-5L data, a simple linear transformation was done to obtain right-skewed data for the utilities (utility decrements) and generalized estimation equations (GEE) were used to analyze the HRQoL parameters (i.e., EQ-VAS and EQ-5D-5L utilities), using link function, exchangeable correlation structure, and robust standard error estimator [40,41,42]. Sex, age, baseline HRQoL, time of measurement (visit) and intervention group (PP versus control), as well as the interaction between time and intervention, were included as fixed covariates.
2.4.2 Costs
Costs were considered from a societal perspective, as proposed in the Danish standards for economic evaluations [43, 44], but only intervention costs were assumed relevant societal costs over the trial period [45]. Intervention costs were gathered via interviews and by provided information from partners involved in the PREVENTOMICS project. Development costs during the project were not considered, but intervention costs were based upon a hypothetical scenario in which the intervention would enter the market. The costs for the two groups included (1) costs for meals [i.e., food, packaging, production, delivery, indirect costs (see Table 1)], (2) behavioral messages, (3) access to the Simple Feast app, and (4) costs for the PREVENTOMICS platform (i.e., storage of data, maintenance questionnaires). In addition, the PP group had costs for (1) the functional ingredients that were added to the meals and for (5) collecting personal data (i.e., blood, urine, and saliva testing/analyses). Which functional ingredient, in what amount, and for which price was added to the meals, varied per cluster. The amount is shown in the paper by Aldubayan et al.[27], and the prices per kilogram were 3.84€, 9.85€, 3.73€, 2.30€ for inulin, fructooligosaccharides, sunflower, and turmeric powder, respectively. With the number of participants per cluster, the weighted average price for functional ingredients was calculated.
The costs for the PREVENTOMICS platform were determined as a fixed price. Given that the Danish trial was just one of the clinical trials utilizing the platform (with three other trials conducted as part of the PREVENTOMICS project [25]), the total fixed price was divided by the total number of participants in all trials of the project (N = 400). This calculation allowed us to calculate the per-participant costs for utilizing the platform (4). Additionally, the costs for collecting personal data (5) and some cost components of the meals (1) (i.e., the production costs of the meals, indirect costs of the meals) were given per participant but may potentially decrease as the total number of participants increases. However, the exact extent of cost reduction with an increasing number of participants remains uncertain. Costs were given per participant and expressed in 2020 euros as well as in 2020 Danish krone (DKK).
2.5 Long-Term Cost-Effectiveness
2.5.1 Method to Estimate Long-Term Outcomes
Since the trial duration was too short to capture all relevant costs and effects, a Markov model for obesity with obesity-related diseases was used to estimate lifetime costs and health outcomes [30]. The model was developed as part of a European Union (EU)-funded project (COMPAR-EU) [46]. Figure 1 provides an overview of the model’s structure [30]. Each rectangle shows a different health state. The model starts with a cohort of people with overweight or obesity and a certain distribution in men/women, a mean age, and a mean BMI (based on the population in the Danish trial) in the state titled ‘no diabetes/no ischemic heart disease (IHD)/no stroke.’ The model then simulates what can happen over time in this cohort regarding the occurrence of diabetes, IHD, stroke, and death; these diseases were included in the model since their prevalence and costs are the highest amongst obesity-related diseases [47, 48]. A cycle length of 1 year was used to model over a lifetime horizon.
Structure of the Markov model for obesity as described by Hoogendoorn et al.[30]. BMI body mass index, IHD Ischemic heart disease
Disease incidence and mortality are dependent on sex, age, BMI, and health state. Incidence of IHD is, for example, higher for patients in the diabetes state than patients in the ‘no diabetes/no IHD/no stroke’ state [30]. Mortality in the diabetes state encompasses both diabetes-related mortality and mortality due to other causes. IHD, including myocardial infarction (MI), and stroke are events associated with a significant risk of mortality when they occur. As a result, mortality for these disease states has been subdivided into case fatality, IHD- or stroke-related mortality, and mortality due to other causes [30].
BMI is included as a continuous variable in this model. All analyses were performed in R using RStudio (version Ri386 3.6.1/ Rx64 3.6.1). Details of the model can be found elsewhere [30].
2.5.2 Model Inputs
For the analysis, we used data from the Danish intervention study in the PREVENTOMICS project. Other sources were used to derive the demographic and epidemiological distributions of the Danish population for estimating the transition probabilities, as well as to describe the associated HRQoL and costs in each health state. Model inputs are described in the following sections and presented in Table 2; details are described elsewhere [30].
2.5.2.1 Demographic and epidemiological input for transition probabilities
The model included mean BMI by sex and age of the Danish population, and this was obtained from the Global Burden of Disease study [49]. The sex-specific relative risks for the association between BMI and all-cause mortality were obtained from a meta-analysis of 230 cohort studies [50]. The Global Burden of Disease study was used for the relative risks by age for the association between BMI and diabetes, IHD, and stroke [49]. Additionally, the relative risks for the co-occurrence of diabetes and stroke and diabetes and IHD were considered; risks for co-occurrence of IHD and stroke were assumed equal to the risks for diabetes and IHD [51,52,53]. Data on the prevalence and incidence for diabetes, IHD, and stroke, specified by sex and age, were obtained from the DYNAMO-HIA study; mortality data were also obtained from this study [51, 52]. Moreover, three additional studies [54,55,56] and OECD data were used to calculate mortality [57, 58]. No fixed transition probabilities are given in Table 2 since they varied according to age, sex, and BMI [30].
2.5.2.2 Effectiveness
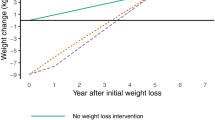
The mean change in BMI was used as one of the intervention effects and was obtained from the Danish trial [27]. Since this change was observed over the 10-week trial period, an assumption had to be made about changes in BMI beyond the trial’s follow-up period. On the basis of the study conducted by Knowler et al.[59], we assumed that the treatment effect in terms of BMI reduction would gradually decline in subsequent years. Specifically, the annual percentage of treatment effect loss in BMI was estimated to be 17.9% until the beginning of year 5, after which any remaining BMI reduction was assumed stable (see more explanation below Table 2) [59]. This assumption was deemed reasonable for two reasons: firstly, the behavioral prompts provided as part of the intervention were expected to lead to sustained treatment effects beyond the intervention period, as supported by previous research indicating the role of behavioral flexibility in maintaining long-term health behaviors [60, 61]. Secondly, participants in the intervention group were exposed to new, healthier, and more suitable ideas for cooking meals during the intervention, which they could continue to apply, and could therefore lead to a sustained intervention effect.
The other intervention effect used in the cost-effectiveness model was the change in utility (mean) obtained from the trial (see Sect. 2.4.1). The long-term health outcomes, as recommended in the guideline [43, 44], were expressed in life expectancy and quality-adjusted life years (QALYs), which were estimated using the model [30]. HRQoL in the model was based on general population sex- and age-specific utilities, based on EQ-5D values in Denmark [62]. These utilities were adjusted for the occurrence of diabetes, IHD, and stroke using prevalence data and previously published utility decrements for the different diseases [63]. All utilities were discounted at 4% per year [43, 44, 64].
2.5.2.3 Costs
Total costs of the intervention (see section 2.4.2) were applied only during the first cycle (i.e., costs were applied during the intervention period and assumed to be zero afterwards). Direct medical costs for treating diabetes, IHD, and stroke were obtained from different studies [64,65,66,67].
Costs of productivity loss were estimated using SHARE data [68] on the basis of values for central European countries since the employment status in Denmark is comparable with those in central European countries [69, 70]. The costs for long-term work loss were calculated using SHARE data [68] on the percentage of people with a paid job, the mean number of working hours per week, and the probability of unemployment using the friction cost method (friction period of 3 months [71]). Production costs per hour were also obtained from the Eurostat website [72]. See Supplement 2 for more details. Costs for informal care were based on SHARE data [68] and calculated using information on the percentage of people receiving informal care and the number of hours per day on the basis of regression equations for northern European countries.
Unrelated medical costs (i.e., costs for other diseases than obesity-related diseases) were calculated by subtracting the related costs per capita for diabetes, IHD, and stroke from the annual healthcare spending by capita by sex and age. More information about this calculation is shown in Supplement 3. Non-medical costs were age specific and estimated from national household consumption/expenditure surveys in each country [Household Budget Surveys (HBS) from Eurostat]. The non-medical costs were based on mean consumption expenditure [73] by taking into account household size [74] and by correcting for the probability of having more than one adult per household [75]. See Supplement 4 for more details.
All costs were converted to 2020 currency using the consumer price index for Denmark [76]. Thereafter, as recommended by the ISPOR’s guideline on good research practices [77], the costs were converted to DKK using purchasing power parity (PPP) [78] and exchange rates [79], depending on the source. All costs were then converted from 2020 DKK to 2020 € using exchange rates (1 DKK = 0.134€) [79]. Costs were discounted at 4% annually [43, 44, 64].
2.5.3 Base-Case Analysis
Model outcomes consisted of total costs (including a breakdown by cost component), life years, life years with diabetes, cumulative incident cases of IHD and stroke, and QALYs of the PP and control interventions. The incremental cost-utility ratio (ICUR) was calculated by dividing the incremental costs by the incremental QALYs (PP versus control). The gross domestic product (GDP) per capita in Denmark in 2020 (47,817€, or 357,100 DKK) was used as the willingness-to-pay threshold (WTP) to gain one QALY, as done in earlier studies [64, 80], since no specific threshold value was recommended in the guideline [43, 44].
2.5.4 Sensitivity Analyses
2.5.4.1 Univariate Sensitivity Analyses and Scenario Analysis
Several sensitivity analyses were conducted to examine the robustness of the results. Univariate sensitivity analyses were performed to estimate the impact of individual key model parameters or assumptions on the outcomes. Input parameters were varied individually according to the lower and upper limits of the 95% CI, while all other parameter values were kept constant. If the CI was unavailable, which was the case for the proportion of effect loss per year and different cost components, a variation of 20% was used. The uncertainty in intervention costs (+/− 20%) reflects, among other things, the uncertainty in the assumption in the number of people receiving the intervention. The results were presented in three tornado diagrams: one for incremental effectiveness (QALYs), one for incremental costs, and one for the ICUR. Moreover, a scenario analysis was performed in which non-medical and unrelated costs were excluded, since some have argued for their exclusion in cost-effectiveness analyses [84]. We did not include subgroup analyses since heterogeneity was not studied in the trial analyses, mainly because of sample size limitations [27, 85].
2.5.4.2 Probabilistic Sensitivity Analysis
Probabilistic sensitivity analysis (PSA) was performed with enough iterations (5000) to obtain stable estimates of relevant parameters. Uncertainty around the relative risks for the association of BMI with all-cause mortality and the relative risks for BMI and obesity-related diseases were incorporated in the PSA. Moreover, uncertainty around costs was included and all other parameters were kept fixed (e.g., utility decrements) (see Table 2). See Supplement 5 for more information on the PSA inputs. Results were presented in a cost-effectiveness plane and a cost-effectiveness acceptability curve (CEAC) [86].
3 Results
3.1 Short-Term Costs and Effects
In the actual trial, a total of 100 Danish participants started the intervention period at baseline. The results of the baseline characteristics can be found in Table 3. As expected, given the randomized allocation of participants, no significant differences in age, gender, BMI, and EQ-5D-5L utility were observed. However, there were significant differences in baseline EQ-5D VAS. Details about other parameters can be found elsewhere [27].
In total, 82 respondents finished the study (38 in the PP group and 44 in the control group). In both groups a significant decrease in BMI was observed compared with baseline measures (Table 4). Moreover, the PP group showed a slightly greater but nonsignificant decrease in BMI compared with the control group. A significant difference in EQ-5D-5L utility of 0.04 was found. Additionally, the PP group reported greater increases in EQ-5D VAS than the control group; however, these results were not statistically significant.
When costs of the two interventions were analyzed, a difference in total costs of 1749€ was found (Table 1). This mainly arose from the costs of preparing and providing the meals. Personalized meals were more labor intensive and therefore more costly, since more unique boxes needed to be prepared. Moreover, functional ingredients were incorporated into the personalized meals. Table 1 presents weighted average costs for these ingredients. The costs for the tests represented a one-time expenditure.
3.2 Base-case estimates of lifetime costs and effects
Table 5 provides the base-case results for various outcomes over a lifetime. Regarding discounted health outcomes, PP increased health by 0.011 QALYs (PP: 15.117 versus control: 15.106). Regarding discounted costs, PP increased total lifetime societal costs by 1736€ (12,963 DKK) (PP: 520,102€ versus control: 518,366€). The most important factor in this increase was intervention costs. Increases were found in unrelated costs and non-medical costs. On the contrary, there was a decrease in the costs of different obesity-related diseases and productivity costs. When the differences in QALYs and costs were combined, the additional cost for PP to gain one QALY was 158,798€ (1,185,909 DKK). This is much higher than the WTP threshold of 47,817€ per QALY gained (357,100 DKK), meaning that PP is not cost-effective given that threshold. The undiscounted results show higher effects and higher costs than the discounted results, resulting in a lower ICUR [99,575€ (743,632 DKK)] compared with the discounted ICUR.
3.3 Univariate Sensitivity Analyses and Scenario Analysis
Results from the univariate sensitivity analyses of different parameters are shown in Fig. 2A–C. The change in intervention costs had the most impact on the incremental costs, followed by the intervention’s effect on BMI (see Fig. 2A). The most impactful parameter for the incremental QALYs was the duration of the QoL effect (see Fig. 2B); an increase in duration of 0.19 years (trial period) to 10 years increased the incremental QALYs from 0.011 to 0.324. The second most influential parameter was the intervention’s effect on BMI.
Tornado diagrams for change in incremental costs in € (DKK) (A), incremental QALYs (B), and ICUR (C) using lower and upper bounds of parameters. BMI body mass index, DKK Danish krone, ICUR incremental cost-utility ratio, IHD ischemic heart disease, QALYs quality-adjusted life years, QoL quality of life. *No fixed number, since costs differ by sex and age. ^Parameters for both lower and upper bounds lead to results in the same direction (the control intervention dominates when the upper bound was used as input)
When the impact of varying individual parameters on the ICUR was explored (Fig. 2C), it was found that the effect in HRQoL (short-term trial effect) had the most impact. When the upper limit of the 95% CI for the treatment’s effect on utility was used (i.e., 0.07 as presented in Table 4), the ICUR decreased from 158,798€ per QALY (1,185,909 DKK) to 105,823€ per QALY (790,293 DKK). When the lower limit of the 95% CI of the other effect measure (i.e., BMI) that was obtained from the trial was used (i.e., −0.51 kg/m2 as presented in Table 4) an ICUR of 49,626€ per QALY gained (370,610 DKK) was found. This change in parameter did not result in an ICUR below the WTP threshold of 47,817€ (357,100 DKK). When the upper limit was used (i.e., 0.38 kg/m2), the PP intervention was dominated by the control. A 20% reduction in intervention costs resulted in an ICUR of 23,668€ per QALY gained (174,534 DKK), which is cost-effective given a WTP of 47,817€ (357,100 DKK). Given the close relationship between intervention costs and the ICUR, we varied the reductions in intervention costs to explore their impact on the ICUR (see Fig. 3). We found that if intervention costs were reduced by 16%, the ICUR was equal to the WTP threshold of 47,817€ (357,100 DKK). This translates into a reduction of 1213€ (9060 DKK) per person. Cost savings were even observed when intervention costs were reduced by more than 23%.
One scenario analysis was carried out, in which the non-medical costs and unrelated medical costs were excluded from the calculations. This resulted in a slight decrease in the incremental costs [1658€ (12,385 DKK)], leading to an ICUR that was lower than the base-case estimate, though still not cost-effective [156,173€ per QALY (1,166,309 DKK)]. See Supplement 6 for detailed results of this scenario analysis.
3.4 Probabilistic Sensitivity Analysis (PSA)
Fig. 4 shows an incremental cost-effectiveness scatterplot with discounted costs and QALYs. Most values can be found in the northeast quadrant (80%), meaning that PP is more costly and more effective than the control intervention. Moreover, the results show that most ICURS are above the maximum WTP threshold, meaning that the probability of PP to be cost-effective is low; only 3% of the iterations were found to be cost-effective at a threshold of 47,817€ (357,100 DKK). This finding is supported by Fig. 5, in which the cost-effectiveness acceptability curve is shown. Fig. 5 shows that by a WTP threshold of 200,856€ (1,500,000 DKK) the probability of PP being cost-effective is 57%. On the basis of the PSA results, the mean QALY gain from PP is 0.011 (95% CI −0.015, 0.04) and mean cost increase is 1748€ (13,055 DKK) [95% CI 1592€ (11,892 DKK), 1907€ (14,239 DKK)].
4 Discussion and Conclusion
This economic evaluation was based on a randomized controlled trial comparing a personalized intervention using omics science (PP) with a control intervention (non-personalized). In both groups, participants received home-delivered meals and behavioral messages, but the PP group received meals and messages that were based on individual phenotypic characteristics at the metabolome level, genotype, lifestyle habits, and preferences. In our study, we examined both the short-term and long-term costs and health outcomes associated with PP compared with the control intervention. The trial showed statistically nonsignificant differences in clinical outcomes (i.e., BMI change of −0.07 kg/m2 (CI 95% −0.51, 0.38) between the PP and control groups. When the short-term differences in effectiveness were extrapolated into lifetime effectiveness in QALYs, we found a slight increase of 0.011 QALYs when the PP intervention was compared with control. The costs increased as well [1736€ (12,963 DKK)], resulting in base-case results that were not cost-effective (158,798€) at a given WTP threshold of 47,817€ per QALY gained (357,100 DKK).
However, the limited statistical power, reflected in wide 95% CIs surrounding the estimated short-term effects, makes it important to address the uncertainty in cost-effectiveness results with sensitivity analyses. Results from the PSA showed that there was only a small probability (3%) that PP was cost-effective. From the univariate analyses we found again that the results were quite robust; for most parameters, varying their values did not substantially affect the cost-effectiveness estimates. However, as expected, a 20% reduction in intervention costs reduced the ICUR to 23,668€ per QALY gained (174,534 DKK), which is cost-effective given a WTP of 47,817€ (357,100 DKK). This was even the case if intervention costs were reduced by 16%. Overall, there are only small increases in QALYs observed when PP was compared with control and the incremental costs were relatively high. This can mainly be explained because personalization of nutrition is labor intensive, which makes intervention costs high; data need to be collected, organized, and analyzed [19]. For some intervention costs (i.e., the production costs of the meals, indirect costs of the meals, costs for testing and costs for the DSS), the costs per participant, and thereby the total intervention costs, could be reduced by increasing the volume (i.e., number of users). In other words, PP might be cost-effective when compared with the control group if the intervention were to be scaled up. This is something which should be validated in future research.
The results from our study correspond with a recently conducted systematic literature review that investigated the cost-effectiveness of interventions with a personalized nutrition component in adults [28]. That review included 49 studies and found that personalized nutrition interventions often led to incremental QALYs between 0 and 0.1, which is comparable with our study findings. However, the review concluded that most personalized nutrition interventions were cost-effective, which is somewhat different from our CEA results. This could mainly be explained by the lower incremental costs found in the review [most costs between −2000 (−1886€) and +2000 dollars (+1886€)] compared with the incremental costs in our study (+1736€). The lack of studies exploring personalized nutrition interventions on the basis of omics science, which incurs higher costs [29], could account for this finding. Instead, the reviewed studies personalized interventions using psychological data, while some incorporated basic biological data such as plasma fatty acids [87, 88] and vitamin or protein intake [89, 90]. However, none of them employed advanced omics technologies as seen in the PREVENTOMICS project.
Different choices need to be made when analyzing the cost-effectiveness of nutrition interventions (e.g., how to deal with ‘weight loss’), and this results in heterogeneity in methods across CEAs [28, 91,92,93,94]. In our study, we used the clinical trial results regarding BMI as a proxy for ‘weight loss’ as model input. However, some authors believe that it might be better to use other outcome measures than BMI [95]. For example, body fat might be a better measure for ‘weight loss’ since it is the most metabolically harmful tissue type [1, 96]. We, however, decided to stick to BMI as our outcome measure for several reasons. First, a validated economic model has been used to explore the cost effectiveness of PP [30]. This model used BMI as a continuous parameter, unlike most previously published obesity models that include classes (e.g., normal weight, overweight, and obese) [97]. Modeling BMI as a continuous parameter gives the model more flexibility in simulating the impact of personalized nutrition on BMI. There were not enough data available in the literature to do this with similar other outcome measures, such as body fat. Second, if we had used another outcome, we would have had to work with intermediate outcome measures; for example, body fat had to be transformed into BMI before calculating lifetime cost-effectiveness. This is not recommended in good research practice guidelines for cost-effectiveness analysis alongside clinical trials [98]. Third, studies have shown that there is a strong correlation between body fat and BMI [99], which was also found in the Danish trial results [27]; small (insignificant) decreases were found when PP was compared with control, so we would not expect different results if a different ‘weight loss’ measure was used as input for the model.
Additionally, the choice for a specific comparator also varied in economic evaluations of (personalized) nutrition interventions, and this might influence the cost-effectiveness results of personalized nutrition [28]. In our study, we used a control intervention that is already considered a ‘healthy’ option. It might therefore be the case that the benefits of additional personalization might not be worth the extra money, particularly given the high intervention costs that were observed for personalization. The question is then, will payers accept the necessary higher short-term costs (e.g., intervention costs) to achieve any long-term health benefits?
Another important question to consider is who the payers for personalized nutrition interventions will be. Nutrition interventions are typically paid out of pocket by the consumer and are thus not reimbursed by a third-party payer [92]. Higher social economic groups might therefore be more likely to use personalized nutrition, although literature showed that in high-income countries the obesity epidemic affects people with a lower socioeconomic status disproportionately [100]. Personalized nutrition might thereby ignore the underlying population causes of obesity (i.e., social, cultural, economic, and political contexts) and might increase social inequalities further. Some governments may therefore find it important to make personalized nutrition acceptable for everyone and could consider introducing reimbursement or subsidies for effective personalized nutrition interventions.
This study has several limitations that should be considered. First, the costs were presented in 2020 euros instead of a more current year closer to the time of publication. However, considering the inflation that has occurred since 2020, it is anticipated that the difference in costs between PP and control would only increase [76]. This, in turn, does not alter the ultimate conclusion that PP is not cost-effective since greater incremental costs would only increase the ICUR values. Second, although short-term effectiveness data were based on an appropriately designed and executed clinical trial, the trial population was relatively small, which resulted in limited statistical power and a rather wide 95% CI for BMI reduction. As a result, subgroup analyses were therefore not conducted. It would be desirable to perform a similar study with a larger population. Third, the trial’s follow-up might have been too short to capture the full effect of personalized nutrition. Given that personalized nutrition is an individual-tailored approach, it is likely that compliance with such interventions is higher, which could lead to sustained positive behavioral changes and greater long-term effectiveness regarding outcomes such as BMI [21]. However, this is likely not directly captured in our study due to the short follow-up. Our study findings, which mainly show insignificant short-term results, are in line with a previous study indicating that the most significant improvements by nutrition interventions occur after the first 6 months [101]. This highlights the need for properly funded long-term studies to effectively address the serious health consequences of obesity.
As with most clinical-trial-based evaluations, the short study follow-up necessitated modeling assumptions to estimate lifetime cost-effectiveness. For example, assumptions were made over the annual percentage of effect loss in BMI after the first year, on the basis of the literature [59], which is not as precise as if we had been able to measure this for a longer time. However, we found consistency in literature about this effect loss [102]. Moreover, we examined the impact of the uncertainty around the assumptions that we made in our sensitivity analyses. This study is therefore meant as a starting point for future studies of the cost-effectiveness of personalized nutrition interventions.
Although cost-effectiveness is an important factor in policymaking decisions about interventions, other factors are relevant as well. One approach to examine all relevant factors would be a comprehensive health technology assessment (HTA) [103,104,105], where interventions are systematically evaluated and assessed in the context of clinical, ethical, economic, social, legislative, organizational, and other domains. This HTA should include results from preference studies as well, since knowledge about people’s preferences regarding personalized nutrition interventions could lead to the development of more cost-effective interventions that people need and accept [106]. Moreover, this research could be extended to other countries as well to see if similar cost-effectiveness results are found [30].
We found that PP would not be considered cost-effective on the basis of the point estimate for BMI reduction seen in the clinical trial, but found that PP has the potential to yield health benefits when compared with a control. A larger and/or longer study would provide a more accurate estimate of effectiveness. Moreover, scaling up the intervention would reduce per-patient costs and thereby help to make the intervention cost-effective. In addition to the challenges in demonstrating the cost-effectiveness of personalized nutrition interventions, another challenge relates to how they will be financed; options to consider are needs-dependent reimbursements or subsidies.
References
World Health Organization. Obesity and overweight [Internet]. 2021 [cited 2022 Jul 13]. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
OECD. The heavy burden of obesity: the economics of prevention [Internet]. Paris; 2019. http://www.oecd.org/els/health-systems/facts and figures-high-res-social-media.pdf
Fisekovic S. Obesity biological and psychological aspect. Bosn J Basic Med Sci. 2005;5:30–4.
Luppino FS, De Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BWJH, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–9.
Simon GE, von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006;63:824–30.
Ul-Haq Z, MacKay DF, Fenwick E, Pell JP. Impact of metabolic comorbidity on the association between body mass index and health-related quality of life: a Scotland-wide cross-sectional study of 5,608 participants. BMC Public Health [Internet]. 2012;12:143. http://www.biomedcentral.com/1471-2458/12/143
Kroes M, Osei-Assibey G, Baker-Searle R, Huang J. Impact of weight change on quality of life in adults with overweight/obesity in the United States: a systematic review. Curr Med Res Opin. 2016;32:485–508.
Kolotkin RL, Andersen JR. A systematic review of reviews: exploring the relationship between obesity, weight loss and health-related quality of life. Clin Obes. 2017;7:273–89.
Hageman PA, Mroz JE, Yoerger MA, Pullen CH. Weight loss is associated with improved quality of life among rural women completers of a web-based lifestyle intervention. PLoS ONE. 2019;14:1–14.
Hecker J, Freijer K, Hiligsmann M, Evers SMAA. Burden of disease study of overweight and obesity; the societal impact in terms of cost-of-illness and health-related quality of life. BMC Public Health. 2022;22:1–13.
Neovius K, Rehnberg C, Rasmussen F, Neovius M. Lifetime productivity losses associated with obesity status in early adulthood: a population-based study of Swedish men. Appl Health Econ Health Policy. 2012;10:309–17.
Goettler A, Grosse A, Sonntag D. Productivity loss due to overweight and obesity: a systematic review of indirect costs. BMJ Open. 2017;7.
Poulimeneas D, Anastasiou CA, Santos I, Hill JO, Panagiotakos DB, Yannakoulia M. Exploring the relationship between the Mediterranean diet and weight loss maintenance: The MedWeight study. Br J Nutr. 2020;124:874–80.
Paradis AM, Godin G, Pérusse L, Vohl MC. Associations between dietary patterns and obesity phenotypes. Int J Obes. 2009;33:1419–26.
Mu M, Xu LF, Hu D, Wu J, Bai MJ. Dietary patterns and overweight/obesity: a review article. Iran J Public Health. 2017;46:869–76.
Chaudhary N, Kumar V, Sangwan P, Pant NC, Saxena A, Joshi S, et al. Personalized nutrition and -omics. Compr Foodomics. 2020;495–507.
Qi L. Personalized nutrition and obesity. Ann Med. 2014;46:247–52.
Stubbs J, Whybrow S, Teixeira P, Blundell J, Lawton C, Westenhoefer J, et al. Problems in identifying predictors and correlates of weight loss and maintenance: implications for weight control therapies based on behaviour change. Obes Rev. 2011;12:688–708.
Bush CL, Blumberg JB, El-Sohemy A, Minich DM, Ordovás JM, Reed DG, et al. Toward the definition of personalized nutrition: a proposal by The American Nutrition Association. J Am Coll Nutr. 2020;39:5–15.
Ordovas JM, Ferguson LR, Tai ES, Mathers JC. Personalised nutrition and health. BMJ (Online). 2018;361:1–7.
Shyam S, Lee KX, Tan ASW, Khoo TA, Harikrishnan S, Lalani SA, et al. Effect of personalized nutrition on dietary, physical activity, and health outcomes: a systematic review of randomized trials. Nutrients. 2022;14.
de Toro-Martín J, Arsenault BJ, Després JP, Vohl MC. Precision nutrition: a review of personalized nutritional approaches for the prevention and management of metabolic syndrome. Nutrients. 2017;9:1–28.
Celis-Morales C, Livingstone KM, Marsaux CFM, Macready AL, Fallaize R, O’Donovan CB, et al. Effect of personalized nutrition on health-related behaviour change: evidence from the Food4Me European randomized controlled trial. Int J Epidemiol. 2017;46:578–88.
Zeevi D, Korem T, Zmora N, Israeli D, Rothschild D, Weinberger A, et al. Personalized nutrition by prediction of glycemic responses. Cell. 2015;163:1079–94.
Keijer J, Escoté X, Galmés S, Palou-march A, Aldubayan MA, Pigsborg K, et al. Omics biomarkers and an approach for their practical implementation to delineate health status for personalized nutrition strategies. Crit Rev Food Sci Nutr. 2023;19:1–29.
Aldubayan MA, Pigsborg K, Gormsen SMO, Serra F, Palou M, Mena P, et al. Empowering consumers to PREVENT diet-related diseases through OMICS sciences (PREVENTOMICS): protocol for a parallel double-blinded randomised intervention trial to investigate biomarker-based nutrition plans for weight loss. BMJ Open. 2022;12: e051285.
Aldubayan MA, Pigsborg K, Gormsen SMO, Serra F, Palou-march A, Favari C, et al. Randomized control trials a double-blinded , randomized , parallel intervention to evaluate biomarker-based nutrition plans for weight loss : the PREVENTOMICS study. Clin Nutr. 2022;41.
Galekop MMJ, Uyl-de Groot CA, Redekop WK. A Systematic review of cost-effectiveness studies of interventions with a personalized nutrition component in adults. Value Health. 2021;24:325–35.
Wang DD, Hu FB. Precision nutrition for prevention and management of type 2 diabetes. Lancet Diabetes Endocrinol [Internet]. 2018;6:416–26. https://doi.org/10.1016/S2213-8587(18)30037-8
Hoogendoorn M, Galekop MMJ, van Baal P. The lifetime health and economic burden of obesity in five European countries: what is the potential impact of prevention? Diabetes Obes Metab. 2023;28.
Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Clin Ther. 2022;44:158–68.
Nordic Council of Ministers. Nordic nutrition recommendations 2012: Integrating nutrition and physical activity [Internet]. Nordisk Ministerråd. 2014. https://altomkost.dk/fileadmin/user_upload/altomkost.dk/Slet_ikke_filliste/Raad_og_anbefalinger/Nordic_Nutrition_Recommendations_2012.pdf
Habibovi M, Broers E, Piera-Jimenez J, Wetzels M, Ayoola I, Denollet J, et al. Enhancing lifestyle change in cardiac patients through the do CHANGE system (“Do cardiac health: Advanced new generation ecosystem”): randomized controlled trial protocol. JMIR Res Protoc. 2018;7:1–9.
EuroQol. No Title [Internet]. https://euroqol.org/
EuroQol Research Foundation. EQ-5D-5L User Guide [Internet]. 2019. https://euroqol.org/publications/user-guides
Jensen CE, Sørensen SS, Gudex C, Jensen MB, Pedersen KM, Ehlers LH. The Danish EQ-5D-5L value set: a hybrid model using cTTO and DCE data. Appl Health Econ Health Policy. 2021;19:579–91.
StataCorp. Stata statistical software: Relaease 17. College Station: TX:StataCorp LLC; 2021.
Singer JD, Willet JB. Applied longitudinal data analysis: modeling change and event occurrence. Oxford University Press; 2003.
Duricki DA, Soleman S, Moon LD. Analysis of longitudinal data from animals with missing values using SPSS. Nat Protoc. 2016;11:1112e29.
Wolowacz SE, Briggs A, Belozeroff V, Clarke P, Doward L, Goeree R, et al. Estimating health-state utility for economic models in clinical studies: an ISPOR good research practices task force report. Value Health. 2016;19:704–19.
Devlin N, Parkin D, Janssen B. Methods for analysing and reporting EQ-5D Data. Methods for analysing and reporting EQ-5D Data. 2020.
Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. New York: John Wiley & Sons; 2004.
Alban A, Gyldmark M, Pedersen AV, Sogaard J. The Danish approach to standards for economic evaluation methodologies. Pharmacoeconomics. 1997;12:627–36.
Sharma D, Aggarwal AK, Downey LE, Prinja S. National healthcare economic evaluation guidelines: a cross-country comparison. Pharmacoecon Open. 2021;5:349–64.
Swedisch council on Health Technology Assessment (SBU). Methods for health economic evaluations - A guideline based on current practices in Europe. 2015.
Ballester M, Orrego C, Heijmans M, Alonso-Coello P, Versteegh MM, Mavridis D, et al. Comparing the effectiveness and cost-effectiveness of self-management interventions in four high-priority chronic conditions in Europe (COMPAR-EU): a research protocol. BMJ Open. 2020;10:1–8.
Ara R, Blake L, Gray L, Hernandez M, Crowther M, Dunkley A, et al. What is the clinical effectiveness and cost-effectiveness of using drugs in treating obese patients in primary care? A systematic review. Health Technol Assess (Rockv) [Internet]. 2012;16:1–202. http://onlinelibrary.wiley.com/o/cochrane/cldare/articles/DARE-12012016429/frame.html
Allender S, Rayner M. The burden of overweight and obesity-related ill health in the UK. Obes Rev. 2007;8:467–73.
GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27.
Aune D, Sen A, Prasad M, Norat T, Janszky I, Tonstad S, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ (Online). 2016;353.
Boshuizen HC, Lhachimi SK, van Baal PHM, Hoogenveen RT, Smit HA, Mackenbach JP, et al. The DYNAMO-HIA model: an efficient implementation of a risk factor/chronic disease markov model for use in Health Impact Assessment (HIA). Demography. 2012;49:1259–83.
DYNAMO-HIA project. Workpackage 7: Overweight and obesity. Report on data collection for overweight and obesity prevalence and related relative risks. [Internet]. [cited 2020 Mar 12]. https://www.dynamo-hia.eu/sites/default/files/2018-04/BMI_WP7-datareport_20100317.pdf
van Baal PH, Engelfriet PM, Boshuizen HC, van de Kassteele J, Schellevis FG, Hoogenveen RT. Co-occurrence of diabetes, myocardial infarction, stroke, and cancer: quantifying age patterns in the Dutch population using health survey data. Popul Health Metr. 2011;9:1–9.
Hoogenveen RT, Boshuizen HC, Engelfriet PM, van Baal PHM. You only die once: accounting for multi-attributable mortality risks in multi-disease models for health-economic analyses. Med Decis Making. 2017;37:403–14.
Vaartjes I, van Dis I, Grobbee DE, Bots ML. The dynamics of mortality in follow-up time after an acute myocardial infarction, lower extremity arterial disease and ischemic stroke. BMC Cardiovasc Disord. 2010;10:57.
Vaartjes I, Reitsma JB, Berger-Van Sijl M, Bots ML. Gender differences in mortality after hospital admission for stroke. Cerebrovasc Dis. 2009;28:564–71.
OECD (2017). “Mortality following acute myocardial infarction (AMI).” in Health at a Glance 2017: OECD indicators, OECD Publishing, Paris [Internet]. https://doi.org/10.1787/health_glance-2017-34-en
OECD (2017). “Mortality following ischaemic stroke.” in Health at a Glance 2017: OECD indicators, OECD Publishing, Paris [Internet]. https://doi.org/10.1787/health_glance-2017-33-en
Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, Brenneman AT. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374:1677–86.
Habibović M, Piera-Jimenez J, Wetzels M, Widdershoven JWGM, Soedamah-Muthu SS. Associations between behavioral flexibility and health behavior in cardiac patients in the Do CHANGE trials. Health Psychol. 2022;41:710–8.
Fletcher BC, Hanson J, Page N, Pine K. FIT - do something different: a new behavioral programfor sustainedweight loss. Swiss J Psychol. 2011;70:25–34.
Sørensen J, Gudex C, Davidsen M, Brønnum-Hansen H, Pedersen KM. Danish EQ-5D population norms. Scand J Public Health. 2009;37:467–74.
Sullivan PW, Slejko JF, Sculpher MJ, Ghushchyan V. Catalogue of EQ-5D scores for the United Kingdom. Med Decis Making. 2011;31:800–4.
Ehlers LH, Lamotte M, Ramos MC, Sandgaard S, Holmgaard P, Frary EC, et al. The cost-effectiveness of oral semaglutide versus empagliflozin in Type 2 diabetes in Denmark. J Comp Eff Res. 2022;11:29–37.
Jennum P, Iversen HK, Ibsen R, Kjellberg J. Cost of stroke: a controlled national study evaluating societal effects on patients and their partners. BMC Health Serv Res. 2015;15:1–10.
Brorholt G, Jakobsen M, Hauge AM, Kjellberg Med Bidrag Fra J, Grønbaek M, Terkelsen CJ, et al. En helhjertet indsats – En artikelbaseret klinisk, patientnær og sundhedsøkonomisk kortlægning af hjerte-kar-området (VIVE report: A Whole-hearted Effort—a publication based clinical, patient centric and health economic mapping of the cardiovascular are [Internet]. 2018. https://www.kora.dk/media/8370396/11162-en-helhjertet-indsats_web.pdf
Sortsø C, Green A, Jensen PB, Emneus M. Societal costs of diabetes mellitus in Denmark. Diabet Med. 2016;33:877–85.
Börsch-Supan A, Brandt M, Hunkler C, Kneip T, Korbmacher J, Malter F, et al. Data resource profile: the survey of health, ageing and retirement in Europe (share). Int J Epidemiol. 2013;42:992–1001.
Eurostat. Employment and activity by sex and age - annual data: LFSI_EMP_A [Internet]. 2022 [cited 2022 Mar 10]. https://ec.europa.eu/eurostat/databrowser/view/LFSI_EMP_A__custom_2496824/bookmark/table?lang=en&bookmarkId=b483e86d-726d-4c8b-b813-38b05b3df447
Eurostat. Unemployment by sex and age—annual data: UNE_RT_A [Internet]. 2022 [cited 2022 Mar 10]. https://ec.europa.eu/eurostat/databrowser/view/UNE_RT_A__custom_2553687/bookmark/table?lang=en&bookmarkId=03a2bb70-40a8-4798-8682-d82d9c6701a0
Kigozi J, Jowett S, Lewis M, Barton P, Coast J. Estimating productivity costs using the friction cost approach in practice: a systematic review. Eur J Health Econ. 2016;17:31–44.
Eurostat. Labour cost levels by NACE Rev. 2 activity: LC_LCI_LEV [Internet]. 2022 [cited 2022 Mar 10]. https://ec.europa.eu/eurostat/databrowser/view/LC_LCI_LEV__custom_709491/bookmark/table?lang=en&bookmarkId=eb78a6c4-aa9b-4210-ad86-6f9d003e1952
Eurostat. Mean consumption expenditure by age of the reference person: [hbs_exp_t135] [Internet]. 2021 [cited 2022 Jul 1]. https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=hbs_exp_t135&lang=en
Eurostat. Household characteristics by age of the reference person: HBS_CAR_T314 [Internet]. 2021 [cited 2022 Jul 1]. https://ec.europa.eu/eurostat/databrowser/view/hbs_car_t314/default/table?lang=en
Mokri H, Kvamme I, de Vries L, Versteegh M, van Baal P. Future medical and non-medical costs and their impact on the cost-effectiveness of life-prolonging interventions: a comparison of five European countries. Eur J Health Econ [Internet]. 2022. https://doi.org/10.1007/s10198-022-01501-6.
OECD (2022). Inflation (CPI) (indicator) [Internet]. [cited 2022 Jul 19]. https://doi.org/10.1787/eee82e6e-en
Shi L, Hodges M, Drummond M, Ahn J, Li SC, Hu S, et al. Good research practices for measuring drug costs in cost-effectiveness analyses: an international perspective: the ISPOR drug cost task force report - Part VI. Value Health. 2010;13:28–33.
OECD (2022). Purchasing power parities (PPP) (indicator) [Internet]. [cited 2022 Jul 19]. https://doi.org/10.1787/1290ee5a-en
OECD (2022). Exchange rates (indicator) [Internet]. [cited 2022 Jul 19]. https://doi.org/10.1787/037ed317-en
Holm AL, Veerman L, Cobiac L, Ekholm O, Diderichsen F. Cost-effectiveness of preventive interventions to reduce alcohol consumption in Denmark. PLoS One. 2014;9.
Ecorys. Study on exploring the incidence and costs of informal long-term care in the EU [Internet]. 2021. https://op.europa.eu/en/publication-detail/-/publication/bafbb918-2197-11ec-bd8e-01aa75ed71a1
Kellerborg K, Perry-Duxbury M, de Vries L, van Baal P. Practical guidance for including future costs in economic evaluations in the Netherlands: introducing and applying PAID 3.0. Value Health. 2020;23:1453–61.
Carstensen B, Rønn PF, Jørgensen ME. Prevalence , incidence and mortality of type 1 and type 2 diabetes in Denmark 1996 – 2016. 2020;8:1–9.
Jiang S, Wang Y, Zhou J, Jiang Y, Liu GGE, Wu J. Incorporating future unrelated medical costs in cost-effectiveness analysis in China. BMJ Glob Health. 2021;6:1–11.
Shields GE, Wilberforce M, Clarkson P, Farragher T, Verma A, Davies LM. Factors limiting subgroup analysis in cost-effectiveness analysis and a call for transparency. Pharmacoeconomics. 2022;40:149–56.
Briggs A, Claxton K, Sculper M. Decision modelling for health economic evaluation. Oxford: Oxford University Press; 2006.
Dalziel K, Segal L. Time to give nutrition interventions a higher profile: cost-effectiveness of 10 nutrition interventions. Health Promot Int. 2007;22:271–83.
De Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: Final report of the Lyon Diet Heart Study. Circulation. 1999;99:779–85.
Sharma Y, Thompson C, Miller M, Shahi R, Hakendorf P, Horwood C, et al. Economic evaluation of an extended nutritional intervention in older Australian hospitalized patients: a randomized controlled trial. BMC Geriatr. 2018;18:1–13.
Ethgen O, Hiligsmann M, Burlet N, Reginster JY. Cost-effectiveness of personalized supplementation with vitamin D-rich dairy products in the prevention of osteoporotic fractures. Osteoporos Int. 2016;27:301–8.
Gentili A, Failla G, Melnyk A, Puleo V, Tanna GL Di, Ricciardi W, et al. The cost-effectiveness of digital health interventions: a systematic review of the literature. Front Public Health. 2022;10.
Poley MJ. Nutrition and health technology assessment: when two worlds meet. Front Pharmacol. 2015;6:1–6.
Dötsch-Klerk M, Bruins MJ, Detzel P, Martikainen J, Nergiz-Unal R, Roodenburg AJC, et al. Modelling health and economic impact of nutrition interventions: a systematic review. Eur J Clin Nutr. 2022;1–14.
Brown V, Tran H, Downing KL, Hesketh KD, Moodie M. A systematic review of economic evaluations of web-based or telephone-delivered interventions for preventing overweight and obesity and/or improving obesity-related behaviors. Obes Rev. 2021;22.
Burkhauser RV, Cawley J. Beyond BMI: the value of more accurate measures of fatness and obesity in social science research. J Health Econ. 2008;27:519–29.
Millstein RA. Measuring outcomes in adult weight loss studies that include diet and physical activity: a systematic review. J Nutr Metab. 2014;2014.
Griffiths UK, Anigbogu B, Nanchahal K. Economic evaluations of adult weight management interventions: a systematic literature review focusing on methods used for determining health impacts. Appl Health Econ Health Policy. 2012;10:145–62.
Ramsey SD, Willke RJ, Glick H, Reed SD, Augustovski F, Jonsson B, et al. Cost-effectiveness analysis alongside clinical trials II - An ISPOR good research practices task force report. Value Health. 2015;18:161–72.
Ilman M, Zuhairini Y, Siddiq A. Correlation between body mass index and body fat percentage. Althea Med J. 2015;2:575–8.
Chatelan A, Bochud M, Frohlich KL. Precision nutrition: hype or hope for public health interventions to reduce obesity? Int J Epidemiol. 2019;48:332–42.
Jancey J, Lee AH, James AP, Howat P, Hills AP, Anderson AS, et al. Long-term sustainability of a physical activity and nutrition intervention for rural adults with or at risk of metabolic syndrome. Aust N Z J Public Health. 2020;44:421–6.
Unick JL, Beavers D, Bond DS, Clark JM, Jakicic JM, Kitabchi AE, et al. The long-term effectiveness of a lifestyle intervention in severely obese individuals. Am J Med. 2013;126:236-242.e2.
Joore M, Grimm S, Boonen A, De Wit M, Guillemin F, Fautrel B. Health technology assessment: a framework. RMD Open. 2020;6:6–8.
Bilekova BK, Gavurova B, Rogalewicz V. Application of the HTA Core Model for complex evaluation of the effectiveness and quality of Radium-223 treatment in patients with metastatic castration resistant prostate cancer. Health Econ Rev. 2018;8.
EUnetHTA. Joint Action 2, Work Package 8. HTA Core Model ® version 3.0 (Pdf) [Internet]. The EUnetHTA JA. 2016. www.htacoremodel.info/BrowseModel.aspx.
van Overbeeke E, Forrester V, Simoens S, Huys I. Use of patient preferences in health technology assessment: perspectives of Canadian. Belgian and German HTA representatives Patient. 2021;14:119–28.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the European Union’s Horizon 2020 research and innovation program [Grant no. 818318].
Conflict of Interest
MMJG, CUG, and WKR declare that they have no conflict of interest.
Availability of Data and Material
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by MMJG and WKR. The first draft of the manuscript was written by MMJG and all authors (MMJG, WKR, and CUG) commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Code Availability (software application or custom code)
This code is available upon reasonable request.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Galekop, M.M.J., Uyl-de Groot, C. & Redekop, W.K. Economic Evaluation of a Personalized Nutrition Plan Based on Omic Sciences Versus a General Nutrition Plan in Adults with Overweight and Obesity: A Modeling Study Based on Trial Data in Denmark. PharmacoEconomics Open 8, 313–331 (2024). https://doi.org/10.1007/s41669-023-00461-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-023-00461-8