Abstract
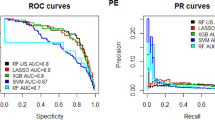
Venous thromboembolism (VTE) is a well-recognized complication that is prevalent in patients undergoing major orthopedic surgery (e.g., total hip arthroplasty and total knee arthroplasty). For years, to identify patients at high risk of developing VTE, physicians have relied on traditional risk scoring systems, which are too simplistic to capture the risk level accurately. In this paper, we propose a data-driven machine learning framework to identify such high-risk patients before they undergo a major hip or knee surgery. Using electronic health records of more than 392,000 patients who undergone a major orthopedic surgery, and following a guided feature selection using the genetic algorithm, we trained a fully connected deep neural network model to predict high-risk patients for developing VTE. We identified several risk factors for VTE that were not previously recognized. The best FCDNN model trained using the selected features yielded an area under the ROC curve (AUC) of 0.873, which was remarkably higher than the best AUC obtained by including only risk factors previously known in the medical literature. Our findings suggest several interesting and important insights. The traditional risk scoring tables that are being widely used by physicians to identify high-risk patients are not considering a comprehensive set of risk factors, nor are they as powerful as cutting-edge machine learning methods in distinguishing low- from high-risk patients.





Similar content being viewed by others
Notes
It should be noted that the Cerner Corporation had not migrated from ICD-9 to ICD-10 yet by October 2015. Hence, all the records used for this study captured diagnoses, medications, and operations using ICD-9. In addition, while some EHR systems use both ICD and CPT coding systems to record procedures, Cerner used solely ICD-9 for procedures.
The standard thresholds categorize each patient as low, moderate, high, and very high risk. To make a one-to-one match to the binary classification ML models, we merged the first two and the last two categories and labeled them as “low risk” and “high risk,” respectively.
We tested 50, 100, and 150 as the feature set sizes in separate runs of the GA algorithm. No remarkable improvement in the model's performance was made beyond 100 added features, so we decided to use 100 as the feature set size.
We also pursued a similar grid search approach for all other ML algorithms mentioned in Table 5 to ensure that their best possible results are used for model comparison.
References
Chong J et al (2021) Development and implementation of venous thromboembolism stewardship across a hospital network. Int J Med Inform 104575
CDC (2021) Data and Statistics on Venous Thromboembolism | CDC.
Cohen AT et al (2007) Venous thromboembolism (VTE) in Europe. Thromb Haemost 98(10):756–764
Anderson FA, Spencer FA (2003) Risk Factors for Venous Thromboembolism. Circulation 107(SUPPL):23. https://doi.org/10.1161/01.CIR.0000078469.07362.E6
Haas S, Encke A, Kopp I (2016) S3-Leitlinie zur Prophylaxe der venösen Thromboembolie. DMW-Deutsche Medizinische Wochenschrift 141(07):453–456
Geerts WH et al (2004) Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 126(3):338S-400S
Geerts WH et al (2008) Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 133(6):381S-453S
Arcelus JI, Kudrna JC, Caprini JA (2006) Venous thromboembolism following major orthopedic surgery: what is the risk after discharge? Orthopedics 29(6):506–516
Holmes M, Nieto MP, Song H, Tonkin E, Grant S, Flach P (2020) Modelling patient behaviour using IoT sensor data: a case study to evaluate techniques for modelling domestic behaviour in recovery from total hip replacement surgery. J Healthc Informatics Res 4(3):238–260. https://doi.org/10.1007/s41666-020-00072-6
Raffini L, Trimarchi T, Beliveau J, Davis D (2011) Thromboprophylaxis in a pediatric hospital: a patient-safety and quality-improvement initiative. Pediatrics 127(5):e1326–e1332
Male C et al (2020) Rivaroxaban compared with standard anticoagulants for the treatment of acute venous thromboembolism in children: a randomised, controlled, phase 3 trial. Lancet Haematol 7(1):e18–e27
Morgan J et al (2018) Prevention of perioperative venous thromboembolism in pediatric patients: Guidelines from the Association of Paediatric Anaesthetists of Great Britain and Ireland (APAGBI). Pediatr Anesth 28(5):382–391
Karnuta JM, Navarro SM, Haeberle HS, Billow DG, Krebs VE, Ramkumar PN (2019) Bundled care for hip fractures: a machine-learning approach to an untenable patient-specific payment model. J Orthop Trauma 33(7):324–330
Ramkumar PN et al (2019) Preoperative prediction of value metrics and a patient-specific payment model for primary total hip arthroplasty: development and validation of a deep learning model. J Arthroplasty 34(10):2228–2234
Ramkumar PN et al (2019) Development and validation of a machine learning algorithm after primary total hip arthroplasty: applications to length of stay and payment models. J Arthroplasty 34(4):632–637
Navarro SM et al (2018) Machine learning and primary total knee arthroplasty: patient forecasting for a patient-specific payment model. J Arthroplasty 33(12):3617–3623
Cabitza F, Locoro A, Banfi G (2018) Machine learning in orthopedics: a literature review. Front Bioeng Biotechnol 6:75
Urish K, Reznik AM (2018) How would a computer diagnose arthritis on a radiograph. AAOS Now 2018:32–33
Kozic N et al (2010) Optimisation of orthopaedic implant design using statistical shape space analysis based on level sets. Med Image Anal 14(3):265–275
Kotti M, Duffell LD, Faisal AA, McGregor AH (2017) Detecting knee osteoarthritis and its discriminating parameters using random forests. Med Eng Phys 43:19–29
Haeberle HS et al (2019) Artificial intelligence and machine learning in lower extremity arthroplasty: a review. J Arthroplasty 34(10):2201–2203
Liu S et al (2019) Machine learning approaches for risk assessment of peripherally inserted Central catheter-related vein thrombosis in hospitalized patients with cancer. Int J Med Inform 129:175–183
Martins TD, Annichino-Bizzacchi JM, Romano AVC, Maciel Filho R (2020) Artificial neural networks for prediction of recurrent venous thromboembolism. Int J Med Inform 141:104221
Caprini JA (2005) Thrombosis risk assessment as a guide to quality patient care. Dis Mon 51(2–3):70–78
Turpie AGG, Bauer KA, Eriksson BI, Lassen MR, of the POP Studies SC (2002) Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery: a meta-analysis of 4 randomized double-blind studies. Arch Intern Med 162(16):1833–1840
Zolbanin HM, Davazdahemami B, Delen D, Zadeh AH (2020) Data analytics for the sustainable use of resources in hospitals: predicting the length of stay for patients with chronic diseases. Inf Manag 103282 https://doi.org/10.1016/j.im.2020.103282
Guan WJ et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382(18) https://doi.org/10.1056/NEJMoa2002032
Davazdahemami B, Zolbanin HM, Delen D (2022) An explanatory analytics framework for early detection of chronic risk factors in pandemics. Healthc Anal 100020 https://doi.org/10.1016/j.health.2022.100020
Nogas J, Khan SS, Mihailidis A (2020) DeepFall: non-invasive fall detection with deep spatio-temporal convolutional autoencoders. J Healthc Informatics Res 4(1):50–70. https://doi.org/10.1007/s41666-019-00061-4
Zhao H (2008) Instance weighting versus threshold adjusting for cost-sensitive classification. Knowl Inf Syst 15(3):321–334
Alexe G, Alexe S, Hammer PL, Vizvari B (2006) Pattern-based feature selection in genomics and proteomics. Ann Oper Res 148(1):189–201. https://doi.org/10.1007/s10479-006-0084-x
Fan Y-J, Chaovalitwongse WA (2010) Optimizing feature selection to improve medical diagnosis. Ann Oper Res 174(1):169–183. https://doi.org/10.1007/s10479-008-0506-z
Mehmanchi E, Gómez A, Prokopyev OA (2021) Solving a class of feature selection problems via fractional 0–1 programming. Ann Oper Res 303(1):265–295. https://doi.org/10.1007/s10479-020-03917-w
Şeref O, Fan Y-J, Borenstein E, Chaovalitwongse WA (2018) Information-theoretic feature selection with discrete $$k$$-median clustering. Ann Oper Res 263(1):93–118. https://doi.org/10.1007/s10479-014-1589-3
Hastie T, Tibshirani R, Friedman J (2009) The elements of statistical learning: data mining, inference, and prediction. Springer Sci Bus Media
Delen D, Eryarsoy E, Davazdahemami B (2020) No place like home: a cross-national assessment of the efficacy of social distancing during the COVID-19 pandemic (Preprint). JMIR Public Heal Surveill. https://doi.org/10.2196/19862
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143(1):29–36
Davazdahemami B, Delen D (2018) A chronological pharmacovigilance network analytics approach for predicting adverse drug events. J Am Med Informatics Assoc. https://doi.org/10.1093/jamia/ocy097
Delen D, Davazdahemami B, Eryarsoy E, Tomak L, Valluru A (2019) Using predictive analytics to identify drug-resistant epilepsy patients. Health Informa J 146045821983312 https://doi.org/10.1177/1460458219833120
Rajpurohit V, Tejvir P, Meena N, Mittal K (2017) Metatarsal fracture leading to massive pulmonary embolism. Indian J Crit Care Med 21(6):401–403. https://doi.org/10.4103/ijccm.IJCCM_125_17
Ho E, Omari A (2017) Prevalence of acute deep vein thrombosis in patients with ankle and foot fractures treated with nonoperative management-a pilot study. Int J Angiol 26(1):53–59. https://doi.org/10.1055/s-0035-1556054
Sağlam Aykut D, Karabulut Gül H (2017) Pulmonary thromboembolism associated with quetiapine: a case report. Psychiatry Clin Psychopharmacol 27(4):427–428
Jönsson AK, Schill J, Olsson H, Spigset O, Hägg S (2018) Venous thromboembolism during treatment with antipsychotics: a review of current evidence. CNS Drugs 32(1):47–64. https://doi.org/10.1007/s40263-018-0495-7
Wijarnpreecha K, Thongprayoon C, Panjawatanan P, Ungprasert P (2017) Hepatitis C virus infection and risk of venous thromboembolism: a systematic review and meta-analysis. Ann Hepatol 16(4):514–520. https://doi.org/10.5604/01.3001.0010.0279
Galli L, Gerdes VEA, Guasti L, Squizzato A (2014) Thrombosis associated with viral hepatitis. J Clin Transl Hepatol 2(4):234
González-Reimers E, Quintero-Platt G, Martín-González C, Pérez-Hernández O, Romero-Acevedo L, Santolaria-Fernández F (2016) Thrombin activation and liver inflammation in advanced hepatitis C virus infection. World J Gastroenterol 22(18):4427–4437. https://doi.org/10.3748/wjg.v22.i18.4427
Zhu T et al (2008) Influenza vaccination reduces the risk of venous thromboembolism. Am Heart Assoc
Vickers ER et al (2017) Risk of venous thromboembolism following influenza vaccination in adults aged 50years and older in the Vaccine Safety Datalink. Vaccine 35(43):5872–5877. https://doi.org/10.1016/j.vaccine.2017.08.086
George JN et al (1998) Drug-induced thrombocytopenia: a systematic review of published case reports. Ann Intern Med 129(11_Part_1):886–890
Acknowledgements
This work was conducted with data obtained from the Cerner Health Facts data warehouse of EHRs, provided by Oklahoma State University (OSU), Center for Health Systems Innovation (CHSI). Any opinions, findings, conclusions, or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the Cerner Corporation, OSU, or CHSI. The authors would also like to thank Ms. Elvena Fong, health data analytics program manager at CHSI, for her support in extracting and understanding the healthcare data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rasouli Dezfouli, E., Delen, D., Zhao, H. et al. A Machine Learning Framework for Assessing the Risk of Venous Thromboembolism in Patients Undergoing Hip or Knee Replacement. J Healthc Inform Res 6, 423–441 (2022). https://doi.org/10.1007/s41666-022-00121-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41666-022-00121-2