Abstract
Background
Photobiomodulation (PBM) therapy has attracted major interest in the field of tissue engineering as it can enhance stem cell differentiation. It has been shown that PBM therapy can stimulate differentiation of cells in culture by exerting biomodulatory effect. Recent evidences show that PBM therapy can positively modulate dental pulp stem cell (DPSC) properties. Combination of PBM therapy with growth factors and biomaterials can possibly accelerate osteogenic differentiation of dental pulp stem cells.
Aims
To evaluate the biomodulatory effect of low-level laser dose on dental pulp stem cells in the presence of hydroxyapatite-based scaffold particle for osteogenic differentiation.
Materials and methods
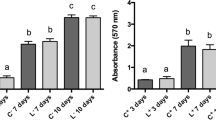
DPSCs were harvested from human premolar teeth and expanded using mesenchymal stem cell medium. Characterization of DPSCs was done using fluorescence-activated cell sorting with CD105, CD44, CD34, and CD45 markers. Cultured DPSCs along with the N-acetylcysteine-labeled hydroxyapatite (NAC-HA) particles and osteogenic differentiation media were exposed to gallium-aluminum-arsenide (Ga-Al-As) diode laser at 810 nm. Cells were divided into 3 groups: L1 (single exposure), L2 (double exposure), and control (no exposure). Osteodifferentiation after PBM therapy was assessed using Alizarin red S staining, Alkaline phosphatase activity (ALP), and by osteopontin expression. Differences between groups at each time point were analyzed using the Mann–Whitney U test. A level of significance of 5% was adopted (p < 0.05).
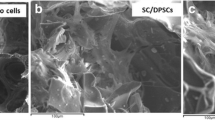
Results
DPSCs grown on NAC-HA polymers show increased cell adhesion and proliferation. Double irradiated groups were consistent with increased calcium (71%) and alkaline phosphatase activity (75%) when compared with single-irradiated groups. mRNA expression of osteopontin was relatively increased in a significant (p < 0.001) manner in L2 when compared with L1 group. Alizarin red S and ALP positive staining confirmed the presence of calcium deposition in the test samples. The osteopontin expression of L2 (216.681) as compared with L1 (123.276) group prove the efficacy of double exposures over a single dose of PBM therapy.
Conclusion
The result envisages the enhanced osteogenic potential of PBM therapy on the differentiation of DPSCs in NAC-HA scaffolds. Double exposure of PBM therapy expresses better biomodulatory effect on DPSCs as compared with the single dose.





Similar content being viewed by others
References
Ma L, Makino Y, Yamaza H, Akiyama K, Hoshino Y, Song G, Kukita T, Nonaka K, Shi S, Yamaza T (2012) Cryopreserved dental pulp tissues of exfoliated deciduous teeth is a feasible stem cell resource for regenerative medicine. PLoS One 7(12):e51777
Shi S, Gronthos S (2003) Perivascular niche of postnatal mesenchymal stem cells in human bone marrow and dental pulp. J Bone Miner Res 18:696–704
Gronthos S, Brahim J, Li W, Fisher LW, Cherman N, Boyde A, DenBesten P, Robey PG, Shi S (2002) Stem cell properties of human dental pulp stem cells. J Dent Res 81:531–535
Kerkis I, CaplanAI ( 2012) Stem cells in dental pulp of deciduous teeth. Tissue Eng Part B Rev 18:129–138
Arthur A, Rychkov G, Shi S, Koblar SA, Gronthos S (2008) Adult human dental pulp stem cells differentiate toward functionally active neurons under appropriate environmental cues. Stem Cells 26:1787–1795
Gronthos S, Mankani M, Brahim J, Robey PG, Shi S (2000) Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci U S A 97:13625–13630
Miura M, Gronthos S, Zhao M, Lu B, Fisher LW, Robey PG, Shi S (2003) SHED: stem cells from human exfoliated deciduous teeth. Proc Natl Acad Sci U S A 100:5807–5812
Nosrat IV, Smith CA, Mullally P, Olson L, Nosrat CA (2004) Dental pulp cells provide neurotrophic support for dopaminergic neurons and differentiate into neurons in vitro; implications for tissue engineering and repair in the nervous system. Eur J Neurosci 19:2388–2398
Nosrat IV, Widenfalk J, Olson L, Nosrat CA (2001) Dental pulp cells produce neurotrophic factors, interact with trigeminal neurons in vitro, and rescue motoneurons after spinal cord injury. Dev Biol 238:120–132
Laino G, D’Aquino R, Graziano A, Lanza V, Carinci F, Naro F, Pirozzi G, Papaccio G (2005) A new population of human adult dental pulp stem cells: a useful source of living autologous fibrous bone tissue (LAB). J Bone Miner Res 20:1394–1402
Khanna-Jain R, Mannerström B, Vuorinen A, Sándor GK, Suuronen R, Miettinen S (2012) Osteogenic differentiation of human dental pulp stem cells on β-tricalcium phosphate/poly (l-lactic acid/caprolactone) three-dimensional scaffolds. J Tissue Eng 3:2041731412467998
WaelAtt, Masahiro Yamada, Norinaga Kojima, Takahiro Ogawa (2009) N-Acetyl cysteine prevents suppression of oral fibroblast function on poly(methylmethacrylate) resin. Acta Biomater 5: 391–398
Lean JM, Davies JT, Fuller K, Jagger CJ, Kirstein B, Partington GA, Urry ZL, Chambers TJ (2003) A crucial role for thiol antioxidants in estrogen-deficiency bone loss. J Clin Invest 112:915–923
Meister A, Anderson ME (1983) Glutathione. Annu Rev Biochem 52:711–760
Stanislawski L, Lefeuvre M, Bourd K, Soheili-Majd E, Goldberg M, Perianin A (2003) TEGDMA-induced toxicity in human fibroblasts is associated with early and drastic glutathione depletion with subsequent production of oxygen reactive species. J Biomed Mater Res A 66:476–482
Gillissen A, Scharling B, Jaworska M, Bartling A, Rasche K, Schultze-Werninghaus G (1997) Oxidant scavenger function of ambroxol in vitro: a comparison with N-acetyl cysteine. Res Exp Med (Berl) 196:389–398
Incerti Parenti S, Panseri S, Gracco A, Sandri M, Tampieri A, Alessandri Bonetti G (2013) Effect of low-level laser irradiation on osteoblast-like cells cultured on porous hydroxyapatite scaffolds. Ann 1st Super Sanita 49:255–260
Brosseau L, Robinson V, Wells G, Debie R, Gam A, Harman K, Morin M, Shea B, Tugwell P (2005) Low-level laser therapy (classes I, II and III) for treating rheumatoid arthritis. Cochrane Database Syst Rev CD002049
Pogrel MA, Chen JW, Zhang K (1997) Effects of low-energy gallium-aluminum-arsenide laser irradiation on cultured fibroblasts and keratinocytes. Lasers Surg Med 20:426–432
AlGhamdi KM, Kumar A, Moussa NA (2012) Low-level laser therapy: a useful technique for enhancing the proliferation of various cultured cells. Lasers Med Sci 27:237–249
Lopes LA, Rigau J, ZaÃngaro RA, Neto JG, Marques Jaeger MM (2001) Comparison of the low level laser therapy effects on cultured human gingival fibroblasts proliferation using different irradiance and same fluence. Lasers Surg Med 29:179–184
Hamblin MR (2016) Photobiomodulation or low-level laser therapy. J Biophotonics 9:1122–1124
Anders JJ, Lanzafame RJ, Arany PR (2015) Low-level light/laser therapy versus photobiomodulation therapy. Photomed Laser Surg 33:183–184
Weng W, Shen G, Han G (2000) Low temperature preparation of hydroxyapatite coatings on titanium alloy by a sol-gel route. J Mater Sci Lett 19:2187–2188
Levi S, Rac V, Manojlovi V, VesnaRaki BBT, Katarzyna F et al (2011) Limonene encapsulation in alginate/poly (vinyl alcohol). Procedia Food Science 1:1816–1820
Sugden B, DeTroy B, Roberts RJ, Sambrook J (1975) Agarose slab-gel electrophoresis equipment. Anal Biochem 68:36–46
Evans DH, Abrahamse H (2008) Efficacy of three different laser wavelengths for in vitro wound healing. Photodermatol Photoimmunol Photomed 24:199–210
Hawkins D, Abrahamse H (2005) Biological effects of helium-neon laser irradiation on normal and wounded human skin fibroblasts. Photomed Laser Surg 23:251–259
Matsui S, Takeuchi H, Tsujimoto Y, Matsushima K (2008) Effects of Smads and BMPs induced by Ga-Al-As laser irradiation on calcification ability of human dental pulp cells. J Oral Sci 50:75–81
Chen AC, Arany PR, Huang YY et al (2011) Low-level laser therapy activates NF-kB via generation of reactive oxygen species in mouse embryonic fibroblasts. PLoS One 6:e22453
Renno AC, McDonnell PA, Parizotto NA, Laakso EL (2007) The effects of laser irradiation on osteoblast and osteosarcoma cell proliferation and differentiation in vitro. Photomed Laser Surg 25:275–280
Martinasso G, Mozzati M, Pol R, Canuto RA, Muzio G (2007) Effect of superpulsed laser irradiation on bone formation in a human osteoblast-like cell line. Minerva Stomatol 56:27–30
Renno AC, McDonnell PA, Crovace MC, Zanotto ED, Laakso L (2010) Effect of 830 nm laser phototherapy on osteoblasts grown in vitro on biosilicate scaffolds. Photomed Laser Surg 28:131–133
Bouvet-Gerbettaz S, Merigo E, Rocca JP, Carle GF, Rochet N (2009) Effects of low-level laser therapy on proliferation and differentiation of murine bone marrow cells into osteoblasts and osteoclasts. Lasers Surg Med 41:291–297
Soleimani M, Abbasnia E, Fathi M, Sahraei H, Fathi Y, Kaka G (2012) The effects of low-level laser irradiation on differentiation and proliferation of human bone marrow mesenchymal stem cells into neurons and osteoblasts—an in vitro study. Lasers Med Sci 27:423–430
Borzabadi-Farahani A (2016) Effect of low-level laser irradiation on proliferation of human dental mesenchymal stem cells; a systemic review. J Photochem Photobiol B 162:577–582
Ginani F, Soares DM, Barreto MP, Barboza CA (2015) Effect of low-level laser therapy on mesenchymal stem cell proliferation: a systematic review. Lasers Med Sci 30:2189–2194
Cruz LB, Ribeiro AS, Rech A, Rosa LG, Castro CG Jr, Brunetto AL (2007) Influence of low-energy laser in the prevention of oral mucositis in children with cancer receiving chemotherapy. Pediatr Blood Cancer 48:435–440
Kuhn A, Porto FA, Miraglia P, Brunetto AL (2009) Low-level infrared laser therapy in chemotherapy-induced oral mucositis: a randomized placebo-controlled trial in children. J Pediatr Hematol Oncol 31:33–37
Acknowledgments
The authors acknowledge PMS College of Dental Science and Research for facilitating the infrastructure. The authors would like to profoundly thank Dr. KiranNayak for providing the laser device.
Funding
Partly funded by Department of Biotechnology, Government of India, New Delhi.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical clearance was obtained from the institutional ethical committee with IEC number: PMS/IEC/2012/25.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sivakumar, T.T., Muruppel, A.M., Joseph, A.P. et al. Photobiomodulatory effect delivered by low-level laser on dental pulp stem cell differentiation for osteogenic lineage. Laser Dent Sci 3, 175–181 (2019). https://doi.org/10.1007/s41547-019-00066-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41547-019-00066-7