Abstract
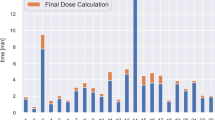
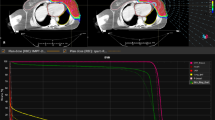
Intensity-modulated proton therapy (IMPT) is becoming essential for proton therapy and is under rapid development. However, for IMPT, the lateral penumbra of the spot-scanning proton beam is still an urgent issue to be solved. Patient-specific block collimators (PSBCs), which can block unnecessary doses, play a crucial role in passive scattering delivery technology but are rarely used in spot scanning. One objective of this study is to investigate the lateral penumbra variations of intensity-modulated spot scanning with and without a PSBC. For fields with varying degrees of sharpness and at varying depths in a water phantom, the lateral penumbral widths were calculated using a Monte Carlo-based dose engine from RayStation 6. The results suggest that the lateral penumbral widths can be reduced by more than 30% for uniform target volumes, regardless of whether a range-shifter is used, and that the maximum dose beyond the field edges can be reduced significantly. The results of patient cases show that the doses in organs-at-risk near the edge of the target volume decrease if a PSBC is implemented. This study demonstrates that intensity-modulated spot scanning with a PSBC can effectively reduce the lateral penumbra and block unnecessary doses and is therefore promising for clinical applications in spot-scanning proton therapy.





Similar content being viewed by others
References
S.W. Wu, C.J. Tung, C.C. Lee et al., Impact of the material composition on proton range variation—a Monte Carlo study. Radiat. Phys. Chem. 116, 199–202 (2015). https://doi.org/10.1016/j.radphyschem.2015.01.017
B. Clasie, N. Depauw, M. Fransen et al., Golden beam data for proton pencil-beam scanning. Phys. Med. Biol. 57, 1147–1158 (2012). https://doi.org/10.1088/0031-9155/57/5/1147
H. Paganetti, Proton Therapy Physics (CRC Press, Boca Raton, 2012), p. 61
A. Mirandola, S. Molinelli, F.G. Vilches et al., Dosimetric commissioning and quality assurance of scanned ion beams at the Italian National Center for Oncological Hadrontherapy. Med. Phys. 42, 5287–5300 (2015). https://doi.org/10.1118/1.4928397
H. Li, L. Zhang, L. Dong et al., A CT-based software tool for evaluating compensator quality in passively scattered proton therapy. Phys. Med. Biol. 55, 6759–6771 (2010). https://doi.org/10.1088/0031-9155/55/22/010
J.R. Mendez, J. Perl, J. Schumann et al., Improved efficiency in Monte Carlo simulation for passive-scattering proton therapy. Phys. Med. Biol. 60, 5019–5035 (2015). https://doi.org/10.1088/0031-9155/60/13/5019
Y. Zheng, J. Fontenot, P. Taddei et al., Monte Carlo simulations of neutron spectral fluence, radiation weighting factor and ambient dose equivalent for a passively scattered proton therapy unit. Phys. Med. Biol. 53, 187–201 (2008). https://doi.org/10.1088/0031-9155/53/1/013
J.C. Polf, W.D. Newhauser, Calculations of neutron dose equivalent exposures from range-modulated proton therapy beams. Phys. Med. Biol. 50, 3859–3873 (2005). https://doi.org/10.1088/0031-9155/50/16/014
J.C. Polf, W.D. Newhauser, U. Titt, Patient neutron dose equivalent exposures outside of the proton therapy treatment field. Radiat. Prot. Dosim. 115, 154–158 (2005). https://doi.org/10.1093/rpd/nci264
D.E. Hyer, P.M. Hill, D. Wang et al., A dynamic collimation system for penumbra reduction in spot-scanning proton therapy: proof of concept. Med. Phys. 41, 91701 (2014). https://doi.org/10.1118/1.4837155
M. Prusator, S. Ahmad, Y. Chen, TOPAS Simulation of the Mevion S250 compact proton therapy unit. J. Appl. Clin. Med. Phys. 18, 88–95 (2017). https://doi.org/10.1002/acm2.12077
S. Safai, T. Bortfeld, M. Engelsman, Comparison between the lateral penumbra of a collimated double-scattered beam and uncollimated scanning beam in proton radiotherapy. Phys. Med. Biol. 53, 1729–1750 (2008). https://doi.org/10.1088/0031-9155/53/6/016
C. Winterhalter, A. Lomax, D. Oxley et al., A study of lateral fall-off (penumbra) optimisation for pencil beam scanning (PBS) proton therapy. Phys. Med. Biol. 63, 25022 (2018). https://doi.org/10.1088/1361-6560/aaa2ad
G. Karamysheva, S. Gurskiy, O. Karamyshev, et al., Compact superconduction cyclotron SC200 for proton therapy. in Proceedings of the 21st international conference on cyclotrons and their applications (CYC’16). 2016. pp. 208–211
K. Yasui, T. Toshito, C. Omachi et al., Evaluation of dosimetric advantages of using patient-specific aperture system with intensity-modulated proton therapy for the shallow depth tumor. J. Appl. Clin. Med. Phys. 19, 132–137 (2018). https://doi.org/10.1002/acm2.12231
C. Bäumer, M. Janson, B. Timmermann, J. Wulff, Collimated proton pencil-beam scanning for superficial targets: impact of the order of range shifter and aperture. Phys. Med. Biol. 63, 85020 (2018). https://doi.org/10.1088/1361-6560/aab79c
U.W. Langner, J.G. Eley, L. Dong et al., Comparison of multi-institutional Varian ProBeam pencil beam scanning proton beam commissioning data. J. Appl. Clin. Med. Phys. 18, 96–107 (2017). https://doi.org/10.1002/acm2.12078
J. Shirey, H.T. Wu, Quantifying the effect of air gap, depth, and range shifter thickness on TPS dosimetric accuracy in superficial PBS proton therapy. J. Appl. Clin. Med. Phys. 19, 164–173 (2018). https://doi.org/10.1002/acm2.12241
M.J. Berger, J.S. Coursey, M.A. Zucker et al., Stopping-Power & Range Tables for Electrons, Protons, and Helium Ions. NIST Standard Reference Database 124 (2017). https://dx.doi.org/10.18434/T4NC7P
RaySearch Laboratories, RayStation 6 Reference Manual (Stockholm, RaySearch, 2016), pp. 155–158
J. Saini, D. Maes, A. Egan, S.R. Bowen, S. St James, M. Janson et al., Dosimetric evaluation of a commercial proton spot scanning Monte-Carlo dose algorithm: comparisons against measurements and simulations. Phys. Med. Biol. 62, 7659–7681 (2017). https://doi.org/10.1088/1361-6560/aa82a5
F.C. Charlwood, A.H. Aitkenhead, R.I. Mackay, A Monte Carlo study on the collimation of pencil beam scanning proton therapy beams. Med. Phys. 43, 1462–1472 (2016). https://doi.org/10.1118/1.4941957
B.R. Smith, D.E. Hyer, P.M. Hill, W.S. Culberson, Secondary neutron dose from a dynamic collimation system during intracranial pencil beam scanning proton therapy: a Monte Carlo investigation. Int. J. Radiat. Oncol. Biol. Phys. 103, 241–250 (2019). https://doi.org/10.1016/j.ijrobp.2018.08.012
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by the Key Program of the 13th Five-Year Plan, the Hefei Institutes of Physical Science of the Chinese Academy of Sciences (No. KP-2017-24).
Rights and permissions
About this article
Cite this article
Liu, CB., Song, YT., Liu, HD. et al. Quantifying lateral penumbra advantages of collimated spot-scanning beam for intensity-modulated proton therapy. NUCL SCI TECH 30, 168 (2019). https://doi.org/10.1007/s41365-019-0687-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41365-019-0687-y