Abstract
Objectives
Sleep difficulties are highly prevalent among children with rare genetic neurodevelopmental conditions (RGNC) such as Angelman and Smith-Magenis syndromes. Behavioral interventions are commonly used in the treatment of sleep difficulties in children; however, research is limited in children with RGNC. This study evaluated the overall effectiveness and acceptability of function-based behavioral sleep interventions for children with RGNC.
Methods
Data was collated from a series of experimental single-case research studies with 26 children (18 months to 19 years of age) with a range of RGNC, who received a behavioral sleep intervention. Intervention strategies included circadian (e.g., sleep/wake rescheduling), antecedent (e.g., sleep hygiene), and/or consequence (e.g., positive reinforcement of sleep-conducive behavior and modified extinction) modifications implemented by parents. Clinicians provided support for parents mostly via telehealth methods. Overall outcomes were examined using modified Brinley plots and effect size estimates. The effect of age, gender, and a range of psychological variables on intervention response was also examined.
Results
Improvements in sleep problem severity were observed for 24/26 participants, and gains were maintained at long-term follow-up for 13/16. Interestingly, 50% of the children achieved clinically significant change with less restrictive strategies (e.g., circadian, antecedent and positive reinforcement strategies), suggesting extinction procedures may be used as the last option in a sequence of interventions. Parents generally perceived interventions to be acceptable. There was minimal evidence of any differential response to intervention as a function of age, gender, or psychological variables.
Conclusions
Results suggest function-based behavioral interventions offer an effective and socially valid method for treating sleep disturbance in children with RGNC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Rare genetic neurodevelopmental conditions (RGNC) are group of heterogeneous syndromes characterized by differences in the number and/or structure of chromosomes, which affect < 1:2000 of the general population (European Commission, 2021; Rare Diseases International, 2023). Phenotypic presentations often include physiological, intellectual, and developmental differences, typically manifested before 22 years of age. Examples of RGNC include Angelman, Prader-Willi, Fragile X, and Smith-Magenis syndromes (McLay et al., 2019; Neo et al., 2021).
Along with the phenotypic characteristics described, sleep difficulties are prevalent in children (encompassing children and adolescents) with RGNC compared to neurotypical children, with substantial variability depending on the type of sleep difficulty and RGNC (Agar et al., 2021; Annaz et al., 2011; Kronk et al., 2010; Veatch et al., 2021). Sleep difficulties experienced may include circadian rhythm disturbances, prolonged sleep onset latency (SOL), night wakings (NWs), unwanted bed-sharing, excessive daytime sleepiness, and early morning waking (EMW). These can have significant adverse short- and long-term effects on learning, behavior, and cognitive development (Kronk et al., 2010), as well as parent and family quality of life and physical and mental health (Annaz et al., 2011; Chu & Richdale, 2009; Kronk et al., 2010; Shochat et al., 2014; Mörelius & Hemmingsson, 2014). Thus, sleep disturbance may further compound the immense challenges already faced by children with RGNC and their families.
Research on the etiology of sleep difficulties associated with RGNC is scarce and mostly focused on biomedical causes (e.g., irregular melatonin production and/or co-occurring medical conditions; Agar et al., 2020; Stores, 2016; Woodford et al., 2021). Consequently, interventions are predominantly pharmacological, most commonly melatonin (e.g., Bailey et al., 2012; Braam et al., 2008). While melatonin is often effective (Bailey et al., 2012; Braam et al., 2008), it is not universally funded, many parents have general concerns about chronic use of medication, and problems that are not always associated with melatonin dysregulation (e.g., unwanted bed-sharing, NW and bedtime resistance) often persist (Blampied, 2013; McLay et al., 2022).
In children with neurodevelopmental conditions (e.g., autism, RGNC), sleep difficulties are generally understood to be the result of a complex interaction between biopsychosocial and behavioral variables (Richdale & Schreck, 2009; Veatch et al., 2021). Specifically, the behavioral model of sleep disturbance posits that sleep onset occurs at the end of a behavior chain, motivated by sleep pressure, that starts with a bedtime routine and ends with the behavioral quietude necessary for sleep to occur (Blampied, 2013; Blampied & van Deurs, 2022). Antecedent variables (i.e., variables that precede and/or regulate a behavior) can affect this behavior chain by altering motivation and cues for sleep (Loring & Malow, 2022). Homeostatic sleep pressure arising from sleep deprivation, delayed bedtime, or excessive daytime activity can increase an individual’s motivation to sleep and, thus, the reinforcing value of sleep (Borbély et al., 2016; Laraway et al., 2003). Further, each step in the behavior chain leading up to sleep onset is under stimulus control whereby each sequential step provides the discriminative stimulus for the step that follows (Blampied, 2013; Blampied & van Deurs, 2022). When discriminative stimuli are absent (e.g., because of a variable bedtime routine) or insufficiently salient, the behavior chain is disrupted. Moreover, when discriminative stimuli are consistently experienced at sleep onset, these cues may become required for sleep onset. Thus, some discriminative stimuli (e.g., a regularly available soft toy) can support, while others (e.g., the absence of parental presence following NWs when otherwise present at initial sleep onset) can interfere with sleep onset both at the start of the night and following NWs (Blampied & van Deurs, 2022). Furthermore, reinforcement contingencies also play a critical role in sleep. Consequences that occur immediately following a behavior may increase or decrease the future likelihood of that behavior (Cooper et al., 2020). If sleep-conducive (e.g., lying quietly in bed) or sleep-interfering (e.g., calling out) behaviors are reinforced (e.g., by some parental response), this is likely to result in continuation of that behavior (Blampied & van Deurs, 2022; McLay & Lang, 2022).
To effectively treat sleep difficulties that are underpinned by behavioral factors, it is essential to identify and address the contributing antecedent and consequence variables (Blampied & van Deurs, 2022; Jin et al., 2013; McLay et al., 2022). Functional Behavioral Assessment (FBA) guides the identification of relevant antecedents, contingencies of reinforcement, and other contextual factors to inform the development of individualized interventions for a range of behavioral difficulties including sleep disturbance (Blampied, 2013; Jin et al., 2013). Interventions may be based on the topography (i.e., presentation) or diagnostic classification of the behavior alone, but such an approach has many conceptual limitations (e.g., the lack of individualization and understanding of mechanisms; Ingram et al., 2005). Consequently, FBA-informed interventions are strongly recommended for children with neurodevelopmental conditions such as autism, attention-deficit hyperactivity disorder (ADHD), and intellectual disability (Soorya et al., 2018), with increased evidence to support their use in the treatment of sleep disturbance for these populations (e.g., Curfs et al., 1999; Didden et al., 1998; Jin et al., 2013; McLay et al., 2020; Weiskop et al., 2005).
Given the evidence supporting function-based interventions for children with higher incidence neurodevelopmental conditions such as autism, and the similarities in the type and topography of presenting sleep difficulties, such interventions merit investigation of their effectiveness for sleep difficulties in children with RGNC. Existing research is limited to individual case studies or small N projects (Curfs et al., 1999; Didden et al., 1998; Woodford et al., 2022) and has rarely included adolescents, and interventions have typically been generic rather than being individualized for each case (Allen et al., 2013; Weiskop et al., 2005). The current study is a retrospective review of 26 participants with RGNC who received function-based behavioral sleep interventions evaluated with experimental, single-case research designs (e.g., Woodford et al., 2022; 2024a). Overall outcomes, possible moderators of intervention response (demographic and child characteristics) and the social validity of the interventions were examined.
Method
The University of Canterbury research team has been investigating the effectiveness of behavioral sleep interventions for children with RGNC since 2018. For each participant, we used FBA to inform the design of individualized, parent-implemented interventions.
Participants and Recruitment
Participants were recruited from throughout New Zealand via service providers for children with RGNC. Between 2018 and 2022, approximately 50 families were screened for the sleep program. Of those screened, 26 families provided consent/assent and met criteria for inclusion in this study. Inclusion criteria were the child (a) was between 18 months and 21 years of age; (b) had or were likely to have a diagnosis of a RGNC, as defined above; (c) had parent-reported sleep difficulties (e.g., prolonged SOL, NWs, unwanted bed-sharing), verified during assessment using sleep diaries and/or video recordings; and (d) had at least commenced the intervention phase of the program and had provided at least one week of intervention data. If the child had a co-occurring condition not currently managed or that might interfere with the implementation of intervention (e.g., epilepsy, tube feeding), approval was obtained from the child’s primary physician; otherwise, they were excluded for safety reasons. Other reasons for exclusion included unstable medication use or withdrawal between the assessment phase and commencement of intervention.
Of the 26 participants (16 males; 10 females), 13 were aged ≤ 6 years, 9 were between 6 and 12 years, and 4 were > 12 years (M = 7.0, SD = 4.2). This included 13 participants from previously published studies (Woodford et al., 2022; 2024a) and 13 participants who did not meet the specific study criteria of these previous studies (N = 6) and/or who withdrew during intervention (N = 9). Inclusion of all participants regardless of whether they adhered to or completed intervention was important for determining the overall, relatively unbiased clinical effectiveness of behavioral sleep intervention (Lachin, 2000). Participant details are summarized in Table 1. In summary, children presented with a range of RGNC. Four cases did not have a confirmed RGNC: Two had a primary diagnosis of cerebral palsy, one had cerebral maldevelopment with cleft frontal lobe and ventriculomegaly and one had a diagnosis of autism and a suspected genetic condition. However, these four children were included due to similarities with those with RGNC (i.e., developmental delay, confirmed neurological alterations and/or were awaiting genetic testing results). All participants had at least one parent-reported co-occurring condition.
Study Design
This study is a retrospective analysis of case data collected within a series of single case experimental studies (e.g., Woodford et al., 2022; 2024a), similar to that conducted by McLay et al. (2020). Case data was gathered in the context of non-concurrent, multiple-baseline across participants experimental designs wherein all participants were randomly allocated pre-determined baseline lengths (namely, 7, 14, or 21 days). Such random allocation ensured that extraneous factors that may have affected response to intervention (e.g., researcher biases) were controlled for, while the assigned lengths were minimally sufficient to permit stability to be observed (Barlow et al., 2009; Christ, 2007; Cooper, et al., 2020; Kratochwill et al., 2010). Given the lack of prior research into the treatment of sleep disturbance with this population, constraints of time and financial support, the disruptions caused by COVID-19, and that by definition RGNC are rare, this N (26) is considered sufficient for research to be informative (Lakens, 2022).
Setting
All therapeutic support was provided remotely via email, phone, and video conferencing for all participants, except for seven who had in-person meetings in the family home or the university clinic. Sleep interventions were implemented by parents, in the family home, with the support of the research team through digital means.
Procedures
Each family progressed through the following phases (a) assessment including FBA; (b) baseline; (c) behavioral case formulation and intervention; and (d) maintenance, including short-term (STFU) and long-term (LTFU) follow-up.
Assessment
As part of the assessment, parents completed a clinical interview (conducted by the first author [EW] or a licensed psychologist or intern psychologist within the research team), at least three nights of parent-reported sleep diaries and/or video recording, and questionnaires (described under “Measures” section). The interview provided information about demographic characteristics, presenting sleep difficulties, goals for sleep, child developmental history, and parents’ motivation to engage in a sleep intervention. The Sleep Assessment Treatment Tool (SATT; Hanley, 2005), used extensively in prior research including neurodivergent children (e.g., Jin et al., 2013; McLay et al., 2020; Woodford et al., 2022), was used to guide interviewing around sleep.
FBAs for each participant considered data from the SATT (Hanley, 2005), sleep diaries, and video (for cases where data patterns were unclear), which were coded according to Antecedent, Behavior, Consequence event recording procedures (ABC recording; Cooper et al., 2020). Patterns that suggested potential behavioral (i.e., operant) functions, including (a) sleep/wake schedules that interfered with motivation for sleep; (b) other sleep-interfering antecedent variables (e.g., sleep hygiene, inappropriate discriminative stimuli for sleep, other environmental factors); and (c) reinforcement contingencies maintaining the sleep difficulties, were then identified by the research team.
Baseline
Baseline data were collected using sleep diaries and video for a randomly assigned baseline length of 7, 14, or 21 days. If visual analysis indicated baseline trends were unstable, or there were threats to internal validity (e.g., unforeseen circumstances such as illness), additional data were collected until baseline stability was achieved (Kazdin, 2011). During baseline, parents maintained typical routines throughout the night.
Behavioral Case Formulation and Intervention
Behavioral case formulation and intervention planning as outlined in Blampied (2013) was undertaken with parents within the framework of the guided participation model (Sanders & Burke, 2014). This was done to individualize intervention for each participant to suit the child’s FBA and accommodate factors such as the child’s developmental status, physical functioning, co-occurring conditions, and family preferences (e.g., the number of verbal prompts, steps taken in modified extinction, or rewards chosen differed depending on such factors). Intervention plans typically included three components: (1) circadian modifications (i.e., sleep/wake scheduling); (2) antecedent modifications; and/or (3) consequence-based modifications.
Circadian modifications were designed to increase motivation for sleep in consideration of the National Sleep Foundation Guidelines for age-appropriate sleep durations (Hirshowitz et al., 2015) and family routines and preferences. Procedures included restricting/eliminating daytime naps, faded bedtime (see Schreck, 2022 for a discussion of faded bedtime), and establishing consistent sleep/wake schedules.
Antecedent modifications included changes to the sleep environment to minimize precipitants of the sleep difficulties, for example, physical environmental (e.g., the addition of light switch coverings), discriminative stimuli (i.e., consistent sleep setting, visual supports, and use of discriminative stimuli for sleep/wake times), and sleep hygiene modifications (i.e., a consistent bedtime routine, sleep-conducive environment) (Loring & Malow, 2022). In addition, visual prompts (e.g., Gro-clocks™, Social Stories™; Gray, 2010) were used to facilitate sleep conducive behavior.
Consequence-based modifications included reinforcement of sleep-conducive behavior (i.e., by social and tangible rewards) and modification of contingencies of reinforcement maintaining sleep-interfering behavior (i.e., by extinction and modified extinction). Extinction procedures involved immediate withdrawal of reinforcement for sleep-incompatible behaviors (e.g., digital device use). Modified extinction procedures included faded parental presence and minimal check (see Carnett & McLay, 2022 for a discussion of extinction procedures).
All strategies were parent-implemented. Parent-clinician contact (mostly by digital means) was frequent (i.e., daily in the early stages of implementing strategies and at least once a week at other times), to obtain updated information and provide guidance. Parents were also able to contact the researchers for ad hoc advice as required. The principle of less restriction (Johnston & Sherman, 1993) was used to guide intervention planning in most cases, so that consequence modifications were the last option in the sequence of interventions given their complexity and difficulty (Woodford et al., 2022, 2024a). Parents were provided revised recommendations both verbally and in written format via email, with systematic formative evaluation of intervention progress. Intervention continued until the parent-clinician determined goals had been met, the family withdrew, or the research team determined that further support would not be beneficial. Intervention duration (including baseline) ranged from 21 to 250 nights (M = 112). See Table 2 for a summary of intervention procedures and the number of participants who received each intervention.
Maintenance and Follow-Up
On conclusion of intervention, parents moved to the maintenance phase where there was no more nightly sleep data recording or researcher-initiated contact, except for an interview with an independent interviewer to gather program feedback. Parents also completed post-intervention questionnaires before STFU. STFU and LTFU data (available for 17 and 16 families, respectively) were collected via seven nights of video and/or sleep diary recordings commencing at 4–6 and 10–14 weeks after the final day of intervention.
Measures
Primary sleep outcome measures included time-series parent-reported sleep diary data and Sleep Problem Severity (SPS) scoring of the diaries. Secondary sleep outcome measures included the Children’s Sleep Habits Questionnaire (Owens et al., 2000) global scores and video recording. The CSHQ was completed at pre-intervention (assessment phase) and post-intervention (maintenance phase, before STFU). Other measures included the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001), Strengths and Difficulties Questionnaire (SDQ; Goodman, 2001), and the Communication domain of the Vineland Adaptive Behavior Scale, Third Edition Parent/Caregiver comprehensive form (VABS-III; Sparrow et al., 2016). These were completed by parents’ pre-intervention to assess for potential moderators of intervention response.
Sleep Outcome Measures
Parent-Reported Sleep Diaries
Sleep diaries, in paper or digital format, were provided to parents via post or email and completed daily, across study phases (Horne & Biggs, 2013). Parents’ recorded information regarding their child’s (a) sleep setting; (b) frequency, duration (minutes), and timing of daytime naps and NW; (c) SOL (minutes); (d) frequency of curtain calls (CCs, i.e., bids for parent attention during sleep onset); (e) onset and offset times of bed-sharing with parent(s); (f) and morning wake time. Parents also described occurrences of sleep interfering behavior and their responses to these, as well as disruptions such as illness and family events.
Video Recording
Swann Advanced-Series DVR4-1200 night-time, infrared video cameras, D-Link HD Cloud cameras, or TP-Link Tapo C100 cameras and recording hardware were posted to parents to set up where the child slept (e.g., their bedroom). Video recordings were used to provide a direct measure of children’s sleep (i.e., from the child’s bedtime to morning waketime) where necessary (including providing data on nights in which sleep diaries were incomplete), as well as for interobserver agreement (IOA) calculations (described below). Videos were coded to align with sleep diary data (bedtime, sleep onset time, time and duration of NWs, etc.). Coding was completed by the lead author (EW), a research assistant or the primary clinician for at least 20% of nights across phases, for whom sufficient video was available. All who coded video footage were blinded to the sleep diaries.
Sleep Problem Severity
Sleep Problem Severity (SPS) composite scores were calculated using coded sleep diary data averaged across the final seven nights of each of baseline, intervention, and STFU and LTFU, as in previous studies conducted by the research team (e.g., McLay et al., 2020; Clarke et al., 2024; Woodford et al., 2022; 2024a). Missing sleep diary information was supplemented with video data, as required. Each child received a single (average) severity score per phase (range 0–22). Scoring code criteria were established based on previously published research defining adequate sleep quality and quantity for preschool (2–4 years 11 months), childhood (5–12 years 11 months), and adolescent (13–18 years) age groups (e.g., Crowley et al., 2014; Hirshkowitz et al., 2015; Mindell & Moore, 2014; Ohayon et al., 2017). An average score of > 2 indicates the presence of clinically significant sleep disturbance, i.e., severe disturbance in one sleep domain or moderate disturbance in two sleep domains (e.g., SOL, NWs) per night. SPS scoring criteria are outlined in Online Resource 1.
Children’s Sleep Habits Questionnaire
The CSHQ (Owens et al., 2000) is a 45-item parent-report measure of the frequency of specific sleep behaviors over the past seven nights in children 4–10 years of age. The CSHQ yields eight subscale scores and a total sleep disturbance score (range 33–99), with a clinical cutoff > 41 based on a neurotypical sample. This measure has acceptable sensitivity (0.80), specificity (0.72), internal consistency (α = 0.68–0.78) and test–retest reliability (r = 0.62–0.79) based on a neurotypical sample (Owens et al., 2000). Consequently, it has been rated by the American Psychological Association’s Evidence-based Assessment Task Force as “well-established” (Lewandowski et al., 2011). Although not validated for use with children with RGNC, it is widely used in research and practice as a measure of sleep disturbance among children both with and without neurodevelopmental conditions. The CSHQ was completed by parents of all children including those outside of the recommended age range (10/26 participants). This is not uncommon among children with neurodevelopmental conditions (Goodlin-Jones et al., 2008; Moss et al., 2014) and there was no alternative parent-report measure allowing for comparison across ages (Owens et al., 2000).
Treatment Acceptability
The Treatment Acceptability Rating Form-Revised (TARF-R; Reimers et al., 1992) is a 20-item parent-report measure given to parents to complete in the maintenance phase to evaluate their perceptions of the effectiveness and acceptability of intervention. Responses are provided on a 7-point Likert scale; 17 items rate treatment acceptability, and three items assess problem severity and parents’ understanding of the intervention process. Higher scores indicate greater acceptability.
Other Measures
Communication Domain of the VABS-III
The Communication domain of the VABS-III is a parent-report measure of children’s communication level used primarily to inform intervention planning. The Communication domain has three sub-domains, namely expressive, receptive, and written language. Item scores per sub-domain are summed and then converted to standardized age equivalence scores to determine the child’s communicative level relative to developmental norms (Pepperdine & McCrimmon, 2018; Sparrow et al., 2016). The VABS-III domains have good psychometric properties (e.g., internal consistency, α = 0.94–0.99, and test–retest reliability, r = 0.64–0.94; Pepperdine & McCrimmon, 2018) and have been frequently used to assess a range of adaptive behaviors in neurodivergent children (e.g., De Bildt et al., 2005).
Child Behavior Checklist
The CBCL (Achenbach & Rescorla, 2001) is a parent-report measure of internalizing and externalizing symptoms in children and adolescents between 1.5 and 18 years of age. Specific item ratings are summed to provide internalizing and externalizing problem scale scores and a total score, with higher scores indicating greater symptom severity. These are converted to t-scores to determine whether the child meets criteria for classifying symptom severity as “normal” (non-clinical; t-score < 65), “borderline” (at-risk: t-score 65–69), or “clinical” (t-score > 70). The CBCL has good psychometric properties based on a neurotypical sample (e.g., internal consistency, α = 0.63–0.90; Achenbach & Rescorla, 2001) and sample of pre-schoolers with RGNC (e.g., internal consistency, α = 0.82–0.94; Neo et al., 2021). Although not validated for use with children with RGNC > 5 years of age, Glasson et al. (2020) found it was the most used measure of internalizing and externalizing symptoms in this population.
Strengths and Difficulties Questionnaire
The SDQ is a 25-item parent-report measure of behavioral strengths and difficulties in young people 4–17 years of age (Goodman, 2001). It has five subscales: emotional symptoms, conduct problems, hyperactivity-inattention, peer problems, and prosocial behavior. Subscale scores (excluding prosocial behavior) are summed to give a total difficulties score, with higher scores indicating greater difficulty, and score ranges for classifying symptom severity as “normal” (0–13), “borderline” (14–16), and “abnormal” (i.e., clinical, 17–40). The SDQ has adequate psychometric properties based on a neurodiverse sample (e.g., internal consistency [α = 0.71]; Emerson, 2005).
Summary of Measures
The measures described contributed to varying components of data analysis for the 26 participants. In summary, data from sleep diaries and the derived SPS scores were used as the primary outcome measures, while CSHQ global scores were used as a secondary outcome measure in this study; data from sleep diaries and video recordings were the primary measures used for individual time-series analyses such as in (Woodford et al., 2022; 2024a) and interobserver agreement and treatment fidelity calculations; and data from the questionnaires assessing child psychological variables were used for analysis of potential moderators of intervention response in this study and for the analysis of collateral effects in a separate study (Woodford et al., 2024b).
Data Analysis
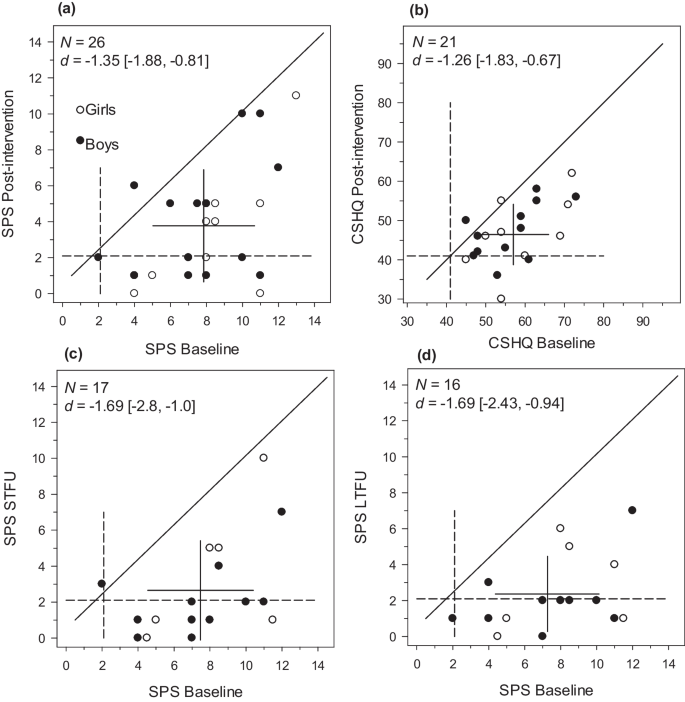
For the purposes of tracking outcome data for each case, individual time-series data was analyzed visually accompanied by percentage below the median (Parker et al., 2011) calculations as an individual effect size measure (see Woodford et al., 2022; 2024a). For this study, i.e., the purposes of the retrospective analysis of overall outcome, changes in participant SPS and CSHQ scores from pre-intervention to the end of intervention phases (i.e., the final week of intervention, STFU and LTFU for SPS; post-intervention for CSHQ) were examined via modified Brinley plots created using SigmaPlot 14 software (systatsoftware.com). These are a type of scatterplot that displays an individual’s response to intervention within the context of group data (Blampied, 2017). Data for each individual is represented as a coordinate pair, with baseline/pre-intervention data on the X axis and data from any subsequent time point on the Y axis. Individual data points that lie on or near the 45° diagonal line show minimal or no therapeutic benefit (Blampied, 2017), while points that fall below the diagonal line indicate a reduction in SPS and CSHQ scores (i.e., the direction of therapeutic change). A cross gives the coordinates of the X and Y means and the length of each arm reflects the standard deviation of the respective mean.
Cohen’s d (the standardized mean difference; dav = within-subjects and ds = between-subjects; Lakens, 2013) and the percent superiority effect size (PSES; the probability that a randomly selected participant has an improved score at time two relative to time one; McGraw & Wong, 1992) were both calculated using Lakens (2013) calculator. Negative d values indicate clinically desirable change (i.e., improvement on a measure). Interpretation of small (d ≤ 0.2), medium (d = ~ 0.5), and large (d ≥ 0.8) effect sizes were based tentatively on Cohen (1988) criteria. Confidence intervals (95% CI) about d were used to classify d as reliably different from zero (p < 0.05) and were calculated using the exploratory software for confidence intervals (ESCI) package by Cumming (2012).
A separate analysis was conducted to evaluate the possible impact of age, gender, and psychological variables on intervention outcome measured by the primary dependent variable (SPS scores) following the procedure of McLay et al. (2020). Psychological variables included VABS expressive and receptive language age equivalence scores, CBCL internalizing and externalizing symptom t-scores, and the SDQ total score. Gender was compared as natural groups, while the sample was split at the median score of the variables of interest to create groups (above or below the median) whose SPS scores could then be compared. First, Cohens ds was calculated to compare the groups’ SPS scores at baseline to see if the variable was associated with different SPS levels pre-intervention. Second, Cohens dav was calculated for each group to separately examine the response of the groups to intervention. A d value of at least medium size (≈0.5) on the SPS scores would indicate that the variable of interest either might be influencing baseline levels of severity and or response to intervention.
Interobserver Agreement and Treatment Fidelity
IOA and treatment fidelity were calculated for at least 20% and 30% of nights, respectively, across study phases for all participants for whom sufficient data were available, to determine the reliability of the parent-reported sleep diary data and parent adherence to intervention strategies, respectively. These percentage aims (≥ 20% and 30%) align with that of other sleep treatment evaluation studies (e.g., Kuhn et al., 2020; McLay et al., 2020) as well as research quality evaluation guidelines (e.g., Reichow et al., 2008).
To calculate IOA (%), participant data for all dependent variables (e.g., SOL, frequency and duration of NWs) from sleep diaries and video footage were compared (where variables were detectable by parents) and the formula (agreement/[agreement + disagreement]) × 100 was used. To calculate treatment fidelity (%), information regarding the intervention components implemented by parents as noted in sleep diaries, video coding and case notes were compared to the intervention protocol and the formula (number of intervention components implemented/total recommended components) × 100 was used.
Results
Results are presented in the following order. First, the outcomes of FBA across participants are described. Second, the intervention outcomes, i.e., changes in the sleep measures (SPS and CSHQ scores), are presented, comparing baseline/pre-intervention to post-intervention, STFU and LTFU. Third, possible moderating effects on intervention outcomes of (a) demographic variables and (b) selected psychological variables are presented. Fourth, a summary is provided regarding participant withdrawal. Fifth, data on IOA, treatment fidelity and acceptability are summarized.
FBA Outcomes
All participants had more than one type of parent-reported sleep difficulty (range = 2–6). Sleep difficulties included bedtime resistance, problematic sleep setting, prolonged SOL, CCs, frequent and prolonged NWs, EMW (i.e., time awake prior to goal waketime), unwanted bed-sharing, and/or parental involvement (i.e., the presence and/or support) during sleep onset and NWs. The most common sleep difficulties were prolonged SOL and NWs, present for 23/26 (88%) children. Interestingly, unwanted bed-sharing and parental involvement during sleep onset and NWs was also common, occurring for 14 (54%) and 6 (23%) participants, respectively. Difficulties related to bedtime resistance (6 participants; 23%), sleep setting (5 participants; 19%), CCs (6 participants; 23%) and EMW (9 participants; 35%) were less common.
There was a range of functions underpinning sleep difficulties. Insufficient sleep pressure related to inconsistent and/or developmentally inappropriate sleep/wake times was common (22 participants; 85%). Parent attention related to unwanted bed-sharing or parent involvement in the night was also common (20 participants; 77%). Other functions included escape from the bedroom (12 participants; 46%) and access to tangible items that competed with sleep, such as digital devices (12 participants; 46%), food/drink (8 participants; 31%), toys (7 participants; 27%), and earmuffs (1 participant; 4%). Automatic reinforcement of stereotypy (e.g., repeated vocalizations or physical movements) in the sleep context was identified for six participants (23%). Other factors that contributed to sleep difficulties included toileting issues (3 participants; 12%), caffeine consumption (1 participant; 4%), and co-occurring medical/physical issues (e.g., reflux, colds, allergies, headlice) that either were not known by the researcher pre-intervention or arose during intervention (11 participants; 42%).
Intervention Outcomes
Group pre- and post-intervention SPS and CSHQ data are summarized in Table 3 and displayed in Fig. 1. Mean SPS and CSHQ scores at baseline were 7.81 (SD = 2.83) and 57.29 (SD = 8.86), respectively, both above the respective clinical cut-offs. For SPS, all but three participants showed a reduction in scores from pre- to post-intervention. Of these three, one boy showed a slight deterioration, while the other two participant scores remained stable. The post-intervention scores of 13 participants fell on or below the clinical cut-off. Although nine participants dropped out in intervention or maintenance phases and do not have follow-up data, this pattern of improvement was maintained. For the CSHQ (N = 21), all but two participants showed a reduction in scores with intervention; however, the mean score remained above the cut-off (M = 47, SD = 7.92). Post-intervention scores fell on or below the clinical cut-off for five participants. Cohen’s dav values were − 1.26 (95%CI = − 1.83, − 0.67) and − 1.35 (95%CI = − 1.88, − 0.81) for the pre- to post-intervention CSHQ and SPS, respectively, indicating a large effect. The effect was also large for SPS from pre-intervention to STFU (dav = − 1.69; 95%CI = − 2.80, − 1.00; PSES = 93%) and LTFU (dav = − 1.69; 95%CI = − 2.43, − 0.94; PSES = 96%). All the 95% confidence intervals did not include zero, with the upper limits (the smallest probable effect given the negative range) consistently being either in the large or moderate effect range (− 0.67 to − 1.0).
Modified Brinley plots showing individual participants’ change for Sleep Problem Severity (SPS) scores from pre- to post-intervention and short-term (STFU) and long-term follow-up (LTFU) (a, c, and d) and for the Children’s Sleep Habits Questionnaire (CSHQ) total scores from pre- to post-intervention (b). Note. Filled and unfilled data points represent boys and girls, respectively. The 45° diagonal line (i.e., where X = Y) represents “no-change.” The dashed lines represent the measure’s clinical cut-off. The means and standard deviations are displayed as a cross, with the mean at the center and the cross arms = ± 1 SD
Analysis of Potential Moderator Variables
Summary data for the potential moderators of age, gender, and selected psychological variables are shown in Table 4. The outcomes of the analysis of the impact of these potential moderators on intervention outcome are shown in Table 5. Older children had somewhat lower SPS scores than younger children, suggesting older children had fewer sleep difficulties. Those above the median on the SDQ also had reduced SPS scores, suggesting those with greater social, behavioral, and emotional difficulties had fewer sleep difficulties. The associated effect size was large for both age and SDQ, but none of the other effect sizes were statistically significantly different from zero. All groups showed a consistently large response to intervention (range − 0.96 to − 2.15) with older age, being female, and having higher receptive and expressive language and lower CBCL internalizing symptoms associated with substantially better response to intervention than the respective comparison groups.
Participant Withdrawal
Of the 26 participants, nine (35%) withdrew at varying stages part way through intervention. Withdrawals included participant-initiated discontinuation of intervention prior to meeting parent-clinician determined goals. Reasons for withdrawal reported by parents included family stressors (N = 4), lack of parental readiness (N = 4), and/or child medical concerns (N = 6). The lack of parental readiness (i.e., ambivalence about the proposed intervention, or low motivation) was associated with concerns about the suitability of consequence modifications, which were recommended for some families as a last option in the sequence of interventions.
Data suggests that families who withdrew (i.e., non-completers), compared with those who completed intervention (i.e., completers), had a child younger in age (M = 3.8 versus 8.8 years) with greater sleep difficulties as measured by the baseline CSHQ (M = 60.2 versus 55) and SPS (M = 8.4 versus 7.5). Interestingly, these participants also had generally fewer reported co-occurring conditions (M = 2.9 versus 3.9) and took fewer medications (M = 1.2 versus 2.3). There were negligible differences between completers and non-completers in communication level and daytime functioning as measured by the VABS-III and CBCL, respectively.
Interobserver Agreement
IOA was calculated for 72% of cases. The remaining 28% did not have video recordings due to an equipment malfunction, or video was their primary data source (i.e., difficulties were undetectable to parents) meaning IOA was unable to be calculated. IOA was calculated for 15–34% of nights across all phases per participant. IOA was between 72 and 98% (M = 89%) for observed children, across all study phases and behaviors, suggesting parent-reported diary data were generally reliable.
Treatment Fidelity
Treatment fidelity was calculated over 32–66% of nights across intervention and follow-up phases, for 23 participants who had sufficient data available. Mean treatment fidelity overall was 78% (range 29–100%). Treatment fidelity declined across study phases with a mean of 80% (range 29–100%), 66% (range 43–100%), and 61% (29–100%) across intervention, STFU and LTFU, respectively.
Treatment Acceptability
The TARF-R was completed by 19 mothers and 9 fathers for 20/26 participants. The maximum possible total score and subscale scores differ; therefore, the percentage of the possible maximum score was calculated. Mean total TARF-R scores were 100.03 and 102.67 for mothers and fathers, respectively. There were negligible differences between mothers and fathers across subscales. Overall, taking 75% as the lower threshold of a highly acceptable rating, both mothers and fathers rated almost all aspects of intervention (except for disruptiveness) as highly acceptable. TARF-R results are detailed in Table 6.
Discussion
This study aimed to evaluate the overall effectiveness of parent-implemented, function-based sleep interventions for 26 children with RGNC. The results of the FBA across children identified a variety of co-occurring sleep difficulties, most commonly prolonged SOL and NWs, maintained by a combination of antecedent and consequence variables. At baseline, 77% of children required parental intervention (i.e., parental presence or bed-sharing) to manage prolonged SOL and NWs, suggesting social attention was a common function. However, sleep difficulties were often multi-functional; that is, they were maintained by social attention, insufficient sleep pressure, escape (i.e., avoidance of bed), automatic (i.e., sensory reinforcement), and/or tangible (e.g., access to devices, toys, and/or food and drink) functions. As a result, the function-based parent-implemented interventions consisted of a range of circadian, antecedent, and consequence modifications.
Results showed that behavioral sleep interventions were somewhat effective for 24/26 children, as reflected in reduced SPS scores and were maintained at follow-up (up to 14 weeks post-intervention). Interestingly, for approximately half, simple modifications to the sleep/wake schedule, sleep environment, and/or reinforcement of target behavior(s) were sufficient to reduce sleep disturbance. For one child, a faded bedtime procedure (Schreck, 2022) alone was sufficient to reduce NW and EMW to a clinically meaningful level. This suggests homeostatic sleep pressure may be used to promote sleep onset and maintenance as well as recalibrate the circadian rhythm (Deboer, 2018; Laraway et al., 2003; Woodford et al., 2022) even when behaviors are maintained by other functions (e.g., social, tangible, escape). For the remaining 13 participants, parents implemented an extinction or modified extinction procedure. For ten, addressing socially maintained difficulties, this involved faded parental presence or minimal check, with high rates of success.
Although highly effective for reducing sleep difficulties, particularly those maintained by parent attention, the finding that 50% of children did not require implementation of extinction-based procedures suggests that, for many, such procedures might not be needed. The principle of less restriction advises that practitioners should commence intervention using minimally sufficient and less intrusive strategies (Johnston & Sherman, 1993). In the sleep context, less restrictive strategies might comprise circadian and antecedent modifications, preliminary to consequence modifications involving extinction (Blampied & van Deurs, 2022; Woodford et al., 2022; 2024a). This study suggests staggering intervention components starting with those that are less restrictive (Johnston & Sherman, 1993) may facilitate change using less restrictive methods (Woodford et al., 2022; 2024a). Such an approach is particularly important for children with RGNC and their families, due to the high demands associated with the range and severity of co-occurring conditions or symptoms. In such cases, the need to minimize stress is important for the wellbeing of both the child and parents, as well as the child’s safety (Stores, 2016).
Given the range of needs with which children with RGNC present, it is also important that parents feel comfortable implementing behavioral sleep interventions. Only a few studies have evaluated the social validity of such interventions for parents of children with RGNC (Allen et al., 2013; McLay et al., 2020; Woodford et al., 2022), and our finding that these interventions were viewed as reasonable and effective is promising. Given the impact of child sleep disturbance on parents (Mörelius & Hemmingsson, 2014) and the acceptability of intervention being a moderator of intervention response (Miller & Rollnick, 2014), further research should continue to explore this area.
The influence of age, gender and child psychological variables on the response to behavioral intervention was also considered. Previous research has noted that a range of variables may influence children’s sleep and responses to intervention including behavioral difficulties and low communicative abilities and intellectual functioning (McLay et al., 2020; Stores, 2016). Interestingly, the present study found children who were younger in age, female and had fewer emotional and behavioral difficulties had slightly greater SPS at baseline. However, there was minimal evidence of any differential response to intervention as a function of those variables. While those with lower internalizing difficulties and greater communicative abilities responded better to intervention, the difference was small, and most children responded positively. Although these results are preliminary, they suggest sleep difficulties may be amenable to change, regardless of the presence and severity of co-occurring factors (France et al., 2022).
Furthermore, although physician approval and/or appropriate management of co-occurring medical and/or physical conditions were part of the inclusion criteria for this study, symptoms associated with these conditions likely still played a role in the presenting difficulties for some cases. In addition, alterations to biological sleep processes (e.g., altered melatonin regulation; Woodford et al., 2021) may have also played a role. The presence of such factors may explain why some children’s sleep difficulties did not fully resolve and provides context to working with children with RGNC in a clinical setting, i.e., behavioral sleep interventions must be applied in consideration of these (Hamilton et al., 2023).
Limitations and Future Research
There are several study limitations which should be considered. First, although the sample size was larger than most current studies that include children with RGNC (N = 1–66; M = 13.44; McLay et al., 2019), it is small relative to the population of children with RGNC, especially given the heterogeneity of that population. The small N reduces confidence in the reliability of the effect size estimates and in the generality of our findings to particular sub-samples of the RGNC population. However, given that RGNC are by definition rare, any evidence of therapeutic effects may be useful, and it should be noted that many of the effect sizes reported were clearly not zero (as shown by their 95%CI). Second, some participants (N = 9) withdrew during intervention and did not complete follow-up, and so results regarding treatment acceptability gathered post-intervention are limited. Interestingly, however, outcomes suggest positive changes are possible without fully completing intervention. Third, assessment of treatment acceptability was also relatively limited (TARF-R; Reimers et al., 1992). A more extensive investigation of parents’ expectations, experiences, resource-limitations, and stress would be desirable. Fourth, IOA could not be calculated for all participants due mostly to technical issues and thus the reliability of parent-report is not known for all participants. Given the measures were based primarily on parent-report, they are susceptible to bias (e.g., halo effect, social desirability bias). Fifth, most of the measures used have not yet been validated for use with children with RGNC. Consequently, there is potential for type one or two errors (Hamrick et al., 2020; Neo et al., 2021). However, these measures have been widely used in sleep research with neurodivergent children (e.g., Glasson et al., 2020; Goodlin-Jones et al., 2008; Moss et al., 2014). Therefore, they were used for consistency with extant research and because there was a lack of alternative measures. Sixth, although an analysis of potential moderators was completed one variable of interest at a time, information regarding parent variables and the cumulative impact of multiple child and parent variables as potential moderators is lacking. Future research should evaluate the complex interplay of a range of variables simultaneously. Finally, the effectiveness and acceptability of individual intervention components were not evaluated in this study. Future research should continue to implement behavioral strategies in a sequential fashion or evaluate individual strategies, to determine what is minimally sufficient for these children. This is particularly important, since multi-component interventions often require substantial clinical support, which is not always readily available in clinical settings.
Conclusion
In conclusion, this study shows that behavioral interventions are a feasible option for a wide variety of families and children affected by RGNC, the challenges posed by their co-occurring conditions notwithstanding. Although internalizing symptoms and communicative abilities might play a small role in determining intervention response, further research into factors that might moderate the response to intervention is needed. It emphasizes the importance of conducting a comprehensive functional assessment considering behavioral, environmental, developmental, and biological factors. Sound clinical judgment is then required to determine how a behavioral intervention is best implemented for each individual child. Within this, it is important to consider whether parents might or might not need to implement extinction procedures to resolve, or at the very least improve children’s sleep difficulties. Finally, and importantly, this study also provides preliminary evidence to suggest that telehealth individualized sleep support is feasible, having been delivered completely remotely for 22 participants during the peak of the COVID-19 pandemic.
Data Availability
The data that support the findings of this study are available on request from the corresponding author (EW).
References
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA school-age forms & profiles: Child behavior checklist for ages 6–18, teacher’s report form, youth self-report: An integrated system of multi-informant assessment. University of Vermont, Research Center for Children Youth & Families.
Agar, G., Brown, C., Sutherland, D., Coulborn, S., Oliver, C., & Richards, C. (2021). Sleep disorders in rare genetic syndromes: A meta-analysis of prevalence and profile. Molecular Autism, 12(1), 18–18. https://doi.org/10.1186/s13229-021-00426-w
Agar, G., Oliver, C., Trickett, J., Licence, L., & Richards, C. (2020). Sleep disorders in children with Angelman and Smith-Magenis syndromes: The assessment of potential causes of disrupted settling and night time waking. Research in Developmental Disabilities, 97, 103555. https://doi.org/10.1016/j.ridd.2019.103555
Allen, K. D., Kuhn, B. R., DeHaai, K. A., & Wallace, D. P. (2013). Evaluation of a behavioral treatment package to reduce sleep problems in children with Angelman syndrome. Research in Developmental Disabilities, 34(1), 676–686. https://doi.org/10.1016/j.ridd.2012.10.001
Annaz, D., Hill, C. M., Ashworth, A., Holley, S., & Karmiloff-Smith, A. (2011). Characterisation of sleep problems in children with Williams syndrome. Research in Developmental Disabilities, 32(1), 164–169. https://doi.org/10.1016/j.ridd.2010.09.008
Bailey, D. B., Raspa, M., Bishop, E., Olmsted, M., Mallya, U. G., & Berry-Kravis, E. (2012). Medication utilization for targeted symptoms in children and adults with Fragile X syndrome: US survey. Journal of Developmental and Behavioral Pediatrics, 33(1), 62–69. https://doi.org/10.1097/DBP.0b013e318236c0e1
Barlow, D. H., Nock, M., & Hersen, M. (2009). Single case experimental designs: Strategies for studying behavior for change (3rd ed.). Pearson Education.
Blampied, N. M. (2013). Functional behavioral analysis of sleep in infants and children. In A. R. Wolfson & H. E. Montgomery-Down (Eds.), The Oxford handbook of infant, child, and adolescent sleep and behavior. Oxford University Press. https://doi.org/10.1093/oxfordhb/9780199873630.013.0013
Blampied, N. M. (2017). Analyzing therapeutic change using modified Brinley plots: History, construction, and interpretation. Behavior Therapy, 48(1), 115–127. https://doi.org/10.1016/j.beth.2016.09.002
Blampied, N. M., & van Deurs, J. R. (2022). A conceptual framework for understanding and designing behavioral interventions for sleep problems in children on the autism spectrum. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 59–74). Springer International Publishing AG.
Borbély, A. A., Daan, S., Wirz-Justice, A., & Deboer, T. (2016). The two-process model of sleep regulation: A reappraisal. Journal of Sleep Research, 25(2), 131–143. https://doi.org/10.1111/jsr.12371
Braam, W. J., Didden, H. C. M., Smits, M. G., & Curfs, L. M. G. (2008). Melatonin for chronic insomnia in Angelman syndrome: A randomized placebo-controlled trial. Journal of Child Neurology, 23(6), 649–654. https://doi.org/10.1177/0883073808314153
Carnett, A., & McLay, L. K. (2022). Behavioral extinction as a treatment for sleep problems in children on the autism spectrum. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 177–191). Springer.
Christ, T. J. (2007). Experimental control and threats to internal validity of concurrent and nonconcurrent multiple baseline designs. Psychology in the Schools, 44(5), 451–459. https://doi.org/10.1002/pits.20237
Chu, J., & Richdale, A. L. (2009). Sleep quality and psychological wellbeing in mothers of children with developmental disabilities. Research in Developmental Disabilities, 30(6), 1512–1522. https://doi.org/10.1016/j.ridd.2009.07.007
Clarke, M. A. C., McLay, L. K., France, K. G., & Blampied, N. M. (2024). An evaluation of a stepped-care telehealth program for improving the sleep of autistic children. Research in Autism Spectrum Disorders, 112. https://doi.org/10.1016/j.rasd.2024.102356
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Erlbaum.
Cooper, J. O., Heron, T. E., & Heward, W. L. (2020). Applied behavior analysis (3rd ed.). Pearson.
Crowley, S. J., Tarokh, L., & Carskadon, M. A. (2014). Sleep during adolescence. In S. H. Sheldon, R. Ferber, M. H. Kryger, & D. Gozal (Eds.), Principles and practice of pediatric sleep medicine (2nd ed., pp. 45–5). W.B. Saunders. https://doi.org/10.1016/B978-1-4557-0318-0.00006-1
Cumming, G. (2012). Understanding the new statistics: Effect sizes, confidence intervals, and meta-analysis. Routledge. https://doi.org/10.4324/9780203807002
Curfs, L. M., Didden, R., Sikkema, S. P., & De Die-Smulders, C. E. (1999). Management of sleeping problems in Wolf-Hirschhorn syndrome: A case study. Genetic Counseling, 10(4), 345.
De Bildt, A., Sytema, S., Kraijer, D., Sparrow, S., & Minderaa, R. (2005). Adaptive functioning and behaviour problems in relation to level of education in children and adolescents with intellectual disability. Journal of Intellectual Disability Research, 49(9), 672–681. https://doi.org/10.1111/j.1365-2788.2005.00711.x
Deboer, T. (2018). Sleep homeostasis and the circadian clock: Do the circadian pacemaker and the sleep homeostat influence each other’s functioning? Neurobiology of Sleep and Circadian Rhythms, 5, 68–77. https://doi.org/10.1016/j.nbscr.2018.02.003
Didden, R., Curfs, L. M., Sikkema, S. P., & de Moor, J. (1998). Functional assessment and treatment of sleeping problems with developmentally disabled children: Six case studies. Journal of Behavior Therapy and Experimental Psychiatry, 29(1), 85–97.
Emerson, E. (2005). Use of the strengths and difficulties questionnaire to assess the mental health needs of children and adolescents with intellectual disabilities. Journal of Intellectual & Developmental Disability, 30(1), 14–23. https://doi.org/10.1080/13668250500033169
European Commission. (2021). Rare diseases: Commission activities in the area of rare diseases. European Commision. https://ec.europa.eu/info/research-and-innovation_en?pg=area&areaname=rare
France, K. G., McLay, L. K., Blampied, N. M., Chow, Y. W. Y., & Pin, N. I. (2022). Intervening in cases with clinical complexity. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 59–74). Springer International Publishing AG.
Glasson, E. J., Buckley, N., Chen, W., Leonard, H., Epstein, A., Skoss, R., Jacoby, P., Blackmore, A. M., Bourke, J., & Downs, J. (2020). Systematic review and meta-analysis: Mental health in children with neurogenetic disorders associated with intellectual disability. Journal of the American Academy of Child and Adolescent Psychiatry, 59(9), 1036–1048. https://doi.org/10.1016/j.jaac.2020.01.006
Goodlin-Jones, B. L., Sitnick, S. L., Tang, K., Liu, J., & Anders, T. F. (2008). The children’s sleep habits questionnaire in toddlers and preschool children. Journal of Developmental and Behavioral Pediatrics, 29(2), 82–88.
Goodman, R. (2001). Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry, 40(11), 1337–1345. https://doi.org/10.1097/00004583-200111000-00015
Gray, C. A. (2010). Social stories™10.1 definition, criteria, & sample stories. Retrieved from http://blogs.4j.lane.edu/communityaccess/files/2013/05/Social-Story-Criteria.pdf
Hamilton, A., Joyce, A., & Spiller, J. (2023). Recommendations for assessing and managing sleep problems in children with neurodevelopmental conditions. Current Developmental Disorders Reports, 10(4), 274–285. https://doi.org/10.1007/s40474-023-00283-7
Hamrick, L. R., Haney, A. M., Kelleher, B. L., & Lane, S. P. (2020). Using generalizability theory to evaluate the comparative reliability of developmental measures in neurogenetic syndrome and low–risk populations. Journal of Neurodevelopmental Disorders, 12(1), 16–16. https://doi.org/10.1186/s11689-020-09318-1
Hanley, G. P. (2005). Sleep assessment and treatment tool [Measurement instrument]. Retrieved May 26, 2017, from https://practicalfunctionalassessment.files.wordpress.com/2015/06/satt.pdf
Hirshkowitz, M., Whiton, K., Albert, S. M., Alessi, C., Bruni, O., DonCarlos, L., Hazen, N., Herman, J., Adams Hillard, P. J., Katz, E. S., Kheirandish-Gozal, L., Neubauer, D. N., O’Donnell, A. E., Ohayon, M., Peever, J., Rawding, R., Sachdeva, R. C., Setters, B., Vitiello, M. V., & Ware, J. C. (2015). National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Health, 1(4), 233–243. https://doi.org/10.1016/j.sleh.2015.10.004
Horne, S. C., & Biggs, S. N. (2013). Actigraphy and sleep/wake diaries. In A. R. Wolfson & H. E. Montgomery-Downs (Eds.), The Oxford handbook of infant, child, and adolescent sleep and behavior (pp. 189–203). Oxford University Press.
Ingram, K., Lewis-Palmer, T., & Sugai, G. (2005). Function-based intervention planning: Comparing the effectiveness of FBA function-based and non—function-based intervention plans. Journal of Positive Behavior Interventions, 7(4), 224–236. https://doi.org/10.1177/10983007050070040401
Jin, C. S., Hanley, G. P., & Beaulieu, L. (2013). An individualized and comprehensive approach to treating sleep problems in young children. Journal of Applied Behavior Analysis, 46(1), 161–180. https://doi.org/10.1002/jaba.16
Johnston, J. M., & Sherman, R. A. (1993). Applying the least restrictive alternative principle to treatment decisions: A legal and behavioral analysis. The Behavior Analyst, 16(1), 103–115. https://doi.org/10.1007/BF03392615
Kazdin, A. E. (2011). Single-case research designs: Methods for clinical and applied settings (2nd ed.). Oxford University Press. https://go.exlibris.link/WsvCgmqY.
Kratochwill, T. R., Hitchcock, J., Horner, R. H., Levin, J. R., Odom, S. L., Rindskopf, D. M. & Shadish, W. R. (2010). Single–case design technical documentation (Version 1.0 [Pilot]). What Works Clearinghouse. https://ies.ed.gov/ncee/wwc/Docs/ReferenceResources/wwc_scd.pdf
Kronk, R., Bishop, E. E., Raspa, M., Bickel, J. O., Mandel, D. A., & Bailey, D. B. (2010). Prevalence, nature, and correlates of sleep problems among children with Fragile X syndrome based on a large scale parent survey. Sleep: Journal of Sleep and Sleep Disorders Research, 33(5), 679–687. https://doi.org/10.1093/sleep/33.5.679
Kuhn, B. R., LaBrot, Z. C., Ford, R., & Roane, B. M. (2020). Promoting independent sleep onset in young children: Examination of the excuse me drill. Behavioral Sleep Medicine, 18(6), 730–745. https://doi.org/10.1080/15402002.2019.1674852
Lachin, J. M. (2000). Statistical considerations in the intent-to-treat principle. Controlled Clinical Trials, 21(3), 167–189. https://doi.org/10.1016/S0197-2456(00)00046-5
Lakens, D. (2022). Sample size justification. Collabra: Psychology, 8(1). https://doi.org/10.1525/collabra.33267
Lakens, D. (2013). Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Frontiers in Psychology, 4, 1–12. https://doi.org/10.3389/fpsyg.2013.00863
Laraway, S., Snycerski, S., Michael, J., & Poling, A. (2003). Motivating operations and terms to describe them: Some further refinements. Journal of Applied Behavior Analysis, 36(3), 407–414.
Lewandowski, A. S., Toliver-Sokol, M., & Palermo, T. M. (2011). Evidence-based review of subjective pediatric sleep measures. Journal of Pediatric Psychology, 36(7), 780–793.
Loring, W., & Malow, B. (2022). Sleep Hygiene and related interventions: Their impact on sleep. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 127–136). Springer International Publishing AG.
McGraw, K. O., & Wong, S. P. (1992). A common language effect size statistic. Psychological Bulletin, 111(2), 361–365. https://doi.org/10.1037/0033-2909.111.2.361
McLay, L. K., Carnett, A., & Sigafoos, J. (2022). Functional behavior assessment of sleep problems in children on the autism spectrum. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 77–91). Springer International Publishing AG.
McLay, L. K., France, K. G., Blampied, N. M., van Deurs, J. R., Hunter, J. E., Knight, J., Hastie, B., Carnett, A., Woodford, E., Gibbs, R., & Lang, R. (2020). Function-based behavioral interventions for sleep problems in children and adolescents with autism: Summary of 41 clinical cases. Journal of Autism and Developmental Disorders, 51(2), 418–432. https://doi.org/10.1007/s10803-020-04548-7
McLay, L. K., & Lang, R. (2022). The role of reinforcement in the treatment of sleep problems. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 161–177). Springer International Publishing AG.
McLay, L., Roche, L., France, K. G., Blampied, N. M., Lang, R., France, M., & Busch, C. (2019). Systematic review of the effectiveness of behaviorally-based interventions for sleep problems in people with rare genetic neurodevelopmental disorders. Sleep Medicine Reviews, 46, 54–63. https://doi.org/10.1016/j.smrv.2019.04.004
Miller, W. R., & Rollnick, S. (2014). The effectiveness and ineffectiveness of complex behavioral interventions: Impact of treatment fidelity. Contemporary Clinical Trials, 37(2), 234–241. https://doi.org/10.1016/j.cct.2014.01.005
Mindell, J. A., & Moore, M. (2014). Bedtime problems and night wakings. In S. H. Sheldon, R. Ferber, M. H. Kryger, & D. Gozal (Eds.), Principles and Practice of Pediatric Sleep Medicine (2nd ed., pp. 105–109). W.B. Saunders. https://doi.org/10.1016/B978-1-4557-0318-0.00014-0
Mörelius, E., & Hemmingsson, H. (2014). Parents of children with physical disabilities - perceived health in parents related to the child’s sleep problems and need for attention at night. Childcare, Health & Development, 40(3), 412–418. https://doi.org/10.1111/cch.12079
Moss, A. H. B., Gordon, J. E., & O’Connell, A. (2014). Impact of sleepwise: An intervention for youth with developmental disabilities and sleep disturbance. Journal of Autism and Developmental Disorders, 44(7), 1695–1707. https://doi.org/10.1007/s10803-014-2040-y
Neo, W. S., Suzuki, T., & Kelleher, B. L. (2021). Structural validity of the child behavior checklist (CBCL) for preschoolers with neurogenetic syndromes. Research in Developmental Disabilities, 109, 103834–103834. https://doi.org/10.1016/j.ridd.2020.103834
Ohayon, M., Wickwire, E., Hirshkowitz, M., Albert, S., Avidan, A., Daly, F., Dauvilliers, Y., Ferri, R., Fung, C., Gozal, D., Hazen, N., Krystal, A., Lichstein, K., Mallampalli, M., Plazzi, G., Rawding, R., Scheer, F., Somers, V., & Vitiello, M. (2017). National Sleep Foundation’s sleep quality recommendations: First report. Sleep Health, 3(1), 6–19. https://doi.org/10.1016/j.sleh.2016.11.006
Owens, J. A., Spirito, A., & McGuinn, M. (2000). The children’s sleep habits questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep, 23(8), 1043–1049. https://doi.org/10.1093/sleep/23.8.1d
Parker, R. I., Vannest, K. J., & Davis, J. L. (2011). Effect size in single-case research: A review of nine nonoverlap techniques. Behavior Modification, 35(4), 303–322. https://doi.org/10.1177/0145445511399147
Pepperdine, C. R., & McCrimmon, A. W. (2018). Test review: Sparrow, S. S., Cicchetti, D. V., & Saulnier, C. A. (2016), “Vineland adaptive behavior scales, third edition” ("vineland-3") San Antonio, TX: Pearson. Canadian Journal of School Psychology, 33(2), 157. https://doi.org/10.1177/0829573517733845
Rare Diseases International. (2023). Operational description of rare diseases. Rare Diseases International. https://www.rarediseasesinternational.org/description-for-rd/.
Reichow, B., Volkmar, F. R., & Cicchetti, D. V. (2008). Development of the evaluative method for evaluating and determining evidence-based practices in autism. Journal of Autism and Developmental Disorders, 38(7), 1311–1319. https://doi.org/10.1007/s10803-007-0517-7
Reimers, T. M., Wacker, D. P., Cooper, L. J., & Deraad, A. O. (1992). Clinical evaluation of the variables associated with treatment acceptability and their relation to compliance. Behavioral Disorders, 18(1), 67–76. https://doi.org/10.1177/019874299201800108
Richdale, A. L., & Schreck, K. A. (2009). Sleep problems in autism spectrum disorders: Prevalence, nature, & possible biopsychosocial aetiologies. Sleep Medicine Reviews, 13(6), 403–411.
Sanders, M. R., & Burke, K. (2014). The “Hidden” technology of effective parent consultation: A guided participation model for promoting change in families. Journal of Child and Family Studies, 23(7), 1289–1297. https://doi.org/10.1007/s10826-013-9827-x
Schreck, K. A. (2022). Bedtime fading and bedtime fading with response cost. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 137–150). Springer International Publishing AG.
Shochat, T., Cohen–Zion, M., & Tzischinsky, O. (2014). Functional consequences of inadequate sleep in adolescents: A systematic review. Sleep Medicine Reviews, 18(1), 75–87. https://doi.org/10.1016/j.smrv.2013.03.005
Soorya, L., Leon, J., Trelles, M. P., & Thurm, A. (2018). Framework for assessing individuals with rare genetic disorders associated with profound intellectual and multiple disabilities (PIMD): The example of Phelan McDermid syndrome. Clinical Neuropsychologist, 32(7), 1226–1255. https://doi.org/10.1080/13854046.2017.1413211
Sparrow, S. S., Cicchetti, D. V., & Saulnier, C. A. (2016). Vineland adaptive behavior scales, third edition (Vineland-3). Pearson.
Stores, G. (2016). Multifactorial influences, including comorbidities, contributing to sleep disturbance in children with a neurodevelopmental disorder. CNS Neuroscience & Therapeutics, 22(11), 875–879. https://doi.org/10.1111/cns.12574
Veatch, O. J., Malow, B. A., Lee, H., Knight, A., Barrish, J. O., Neul, J. L., Lane, J. B., Skinner, S. A., Kaufmann, W. E., Miller, J. L., Driscoll, D. J., Bird, L. M., Butler, M. G., Dykens, E. M., Gold, J., Kimonis, V., Bacino, C. A., Tan, W., Kothare, S. V., . . . Glaze, D. G. (2021). Evaluating sleep disturbances in children with rare genetic neurodevelopmental syndromes. Pediatric Neurology, 123, 30–37. https://doi.org/10.1016/j.pediatrneurol.2021.07.009
Weiskop, S., Richdale, A., & Matthews, J. (2005). Behavioral treatment to reduce sleep problems in children with autism or fragile X syndrome. Developmental Medicine and Child Neurology, 47(2), 94–104. https://doi.org/10.1017/S0012162205000186
Woodford, E. C., McLay, L., France, K. G., Blampied, N. M., Gibbs, R., Swan, C. E., & Eggleston, M. (2021). Endogenous melatonin and sleep in individuals with rare genetic neurodevelopmental disorders (RGNC): A systematic review. Sleep Medicine Reviews, 57, 101433–101433. https://doi.org/10.1016/j.smrv.2021.1014
Woodford, E. C., McLay, L., Blampied, N. M., France, K. G., Gibbs, R., Whitaker, C., & McCaughan, E. (2022). Less restrictive behavioral interventions for sleep problems in children with neurodevelopmental disorders: A single case feasibility study. Journal of Developmental and Physical Disabilities, 1–36. https://doi.org/10.1007/s10882-022-09872-7
Woodford, E. C., McLay, L. K., France, K. G., & Blampied, N. M. (2024a). The lighter touch: Less-restriction in sequentially implemented behavioral sleep interventions for children with rare genetic neurodevelopmental conditions. Journal of Autism and Developmental Disorders, 1–22. https://doi.org/10.1007/s10803-024-06234-4
Woodford, E., McLay, L., France, K. G., Blampied, N. M., & Catherine, S. (2024b). Collateral child and parent effects of behavioral sleep interventions for children with rare genetic neurodevelopmental conditions. Advances in Neurodevelopmental Disorders. https://doi.org/10.1007/s41252-024-00399-w
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This research was supported by funding from the Royal Society of New Zealand Marsden Fund Fast-Start Grant (#M1211).
Author information
Authors and Affiliations
Contributions
EW designed and executed the study, completed assessment and intervention with most participants (EW was enrolled in a licensure-track Child and Family Psychology training program at the time of the project), conducted the data analyses, and wrote the paper. LM provided clinical supervision and collaborated with the design and execution of the study and writing of the paper. KF provided clinical supervision and collaborated with the design of the study and editing of the final manuscript. NB collaborated with the design of the study, data analyses, and the editing of the final manuscript. UH collaborated with data collation and editing of references. CS collaborated with editing the manuscript. All authors approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Ethics Approval
This research was approved by the relevant university Human Ethics Committee (HEC 2018–48) and has been conducted in accordance with the tenets of the declaration of Helsinki and its later amendments.
Consent to Participate
Informed consent was obtained from all parent participants, and assent was provided by most children (in cases with an adequate level of comprehension determined in collaboration with parents, interaction with the child, and in consideration of the Communication domain Vineland Adaptive Behavior Scales, Third Edition [VABS-III; Sparrow et al., 2016] results) for both participation in the study and publishing of results.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Woodford, E.C., France, K.G., Blampied, N.M. et al. Behavioral Sleep Interventions for Children with Rare Genetic Neurodevelopmental Conditions: A Retrospective Analysis of Overall Outcomes for 26 Cases. Adv Neurodev Disord (2024). https://doi.org/10.1007/s41252-024-00403-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s41252-024-00403-3