Abstract
Objectives
Oral sensory, communication, and feeding issues are frequently observed to co-occur in autistic children. The study attempted to explore the association between oral sensory deficits, feeding, and communication deficits in autistic children.
Methods
Behavioral Pediatric Feeding Assessment Scale (BPFAS), Child Sensory Profile 2 (SP-2), and Communication and Symbolic Behavior Scales Developmental Profile Infant/Toddler Checklist (CSBS-DP) were administered to forty autistic children in the age range of 2.5-7 years. The correlation among the three domains was determined using Spearman’s rank correlation coefficient.
Results
A low negative correlation was found between SP-2 scores and CSBS-DP (r = −0.24, p = 0.13), indicating that the higher the oral sensory scores, the poorer the communication skills. SP-2 and BPFAS scores had a moderate positive correlation (r = 0.47, p = 0.002) i.e., higher scores in SP-2 were associated with higher scores in feeding, indicating that oral sensory issues were directly related to the feeding issues.
Conclusions
The overall findings indicated that the presence of oral sensory issues is associated with feeding and communication deficits in autistic children.
Study Registration
Clinical Trial Registry of India CTRI/2020/07/02681
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Autism Spectrum Disorder (ASD) is “a heterogeneous group of neurodevelopmental disorders characterized by impairment in social interaction, communication, and stereotyped/limited behaviors” (American Psychiatric Association, 2013, p. 50). It is estimated that one in 100 children globally have ASD (Zeidan et al., 2022). Based on DSM-5, hypersensitivity or hyposensitivity towards sensory information or stimuli is a diagnostic criterion of ASD. A neurological disorder called Sensory Processing Disorder (SPD) causes difficulties in absorbing, processing, and reacting to sensory information from the environment and within one’s own body (Ayers, 1963). Some of the senses that are affected are visual, auditory, olfaction (smell), tactile, gustatory (taste), vestibular (balance and spatial orientation), and proprioception (the awareness of one’s limbs in space).
Around 70% of autistic children have SPD (Baker et al., 2008; Ben-Sasson et al., 2007; Kientz & Dunn, 1997; Tomchek & Dunn, 2007). In India, around 98% of autistic children exhibit SPD (Shah et al., 2015). Baker et al. (2008) reported the presence of different sensory processing patterns including difficulties in auditory filtering, seeking sensation, under responsiveness in movement and vestibular input, and typical and varied responsiveness in visual, auditory, movement, taste, and smell. It needs to be noted that SPD is not identified as a critical indicator for the diagnosis of ASD (Miller et al., 2007; Suarez, 2012). Research is currently focused on figuring out how autistic children vary from other children. As autistic children exhibit an early beginning of sensory processing problems, a child’s cognitive and speech development could be impacted at an early age (Ben-Sasson et al., 2007; Talay-Ongan & Wood, 2000). Early sensory features have been shown to predict different adaptive behaviors (Williams et al., 2018).
An oral sensation is a form of tactile sensation that is specifically located in the mouth. Oral hypersensitivity and hyposensitivity are the two groups of oral sensitivity disorders in autistic children. Oral sensory development is a normal aspect of childhood development that must be considered when assessing infants. They are the elements that make up the motor-sensory patterns learned during the formation of both basic and complex skills such as eating and speaking. Autistic children struggle to register and modulate sensory inputs in one or more sensory systems to varying degrees (Yack et al., 2015). This makes it difficult to initiate and execute movements or create a feedback system. Evidence from clinical practice has revealed that hyposensitivity and hypersensitivity symptoms coexisted, potentially leading to feeding issues and poor speech intelligibility (Aswathy et al., 2016).
Almost 90% of autistic children are reported to have feeding problems (Kodak & Piazza, 2008). Feeding problems exhibited in autistic children could be attributed to maternal anxiety and maladaptive feeding strategies (Zlomke et al., 2020). Allen et al. (2015) reported that feeding issues and ASD symptoms reported by the parents were positively correlated with behavioral problems, parental stress, and sleep problems in 2-5-year-old autistic children. However, no significant correlation was found among the severity of ASD, a child’s cognitive ability, age, and vocabulary. Autistic children exhibited more problems in feeding and presented atypical oral sensory sensitivity of either hyposensitivity or hypersensitivity. They ate a limited variety of foods, and consumed fewer fruits and vegetables, proteins, starches, and dairy products when compared to normal. Furthermore, autistic children with atypical oral sensitivity also rejected food, exhibited a more limited food repertoire, consumed a limited variety of foods, needed special utensils, struggled with the texture of food, and were picky eaters (Bandini et al., 2010; Chistol et al., 2017; Schreck & Williams, 2006). Furthermore, it has been reported that food selectivity is linked to sensory processing impairment, especially oral sensory, in children diagnosed with ASD (Cermak et al., 2010; Suarez et al., 2014; Zobel-Lachiusa et al., 2015). Fear of unfamiliarity, sensory impairment, social compliance deficits, and biological food aversion are the causes of feeding problems in ASD (Cumine et al., 2000), whereas limited food repertoire could be linked to inadequate nutrient intake (Herndon et al., 2009).
One of the factors that inhibit and influence verbal communication development in autistic children could be the abnormality in the perception of external sensory stimuli (Patten et al., 2013). Roughly, 25-50% of autistic children are not able to communicate verbally to meet their desires (Baghdadli et al., 2012; Lord et al., 2004; Sigman & McGovern, 2005) and this often develops after the age of 5 (Pickett et al., 2009). It has been found from the literature that non-verbal children have substantially worse outcomes than verbal autistic children. In autistic children, acquiring functional verbal communication and/or development of speech before age 5 predicted educational success, work, independence, and social interactions (Kobayashi et al., 1992; Venter et al., 1992). Patten et al. (2013) hypothesized atypical sensory behaviors as a factor constraining verbal communication development in autistic children. They indicated that hypo-responsiveness and behaviors related to sensory seeking were associated with the verbal communication of the child; that is, those children who belonged to the non-verbal ASD category were exhibiting higher sensory-seeking behaviors and hypo-responsiveness to the sensory stimuli. However, hyper-responsiveness did not vary evidently in both verbal and non-verbal children. Observational evidence has suggested that preschool autistic children had hypo-responsiveness to stimuli including social stimuli, which correlated with impaired communication. Liss et al. (2006) used cluster analysis and identified elevated levels of hypo-responsiveness and sensory-seeking behaviors, which were associated with poor communication in autistic children. Hilton et al. (2007) suggested that the severity of the social-communicative symptoms was linked to the three sensory response trends such as hypo-responsiveness and/or hyper-responsiveness, and sensory seeking. Watson et al. (2011) reported that hypo-responsiveness had a positive correlation with social communication, whereas language and adaptive skills were negatively correlated.
While several studies have revealed that oral sensory, feeding, and communication deficits co-occur in autistic children, they have mostly concentrated on measuring the oral sensory abnormalities in autistic children and their relationship to feeding concerns. Food selectivity in autistic children may be related to poor sensory processing, particularly oral sensory sensitivity, according to current research (Suarez, 2012; Zobel-Lachiusa et al., 2015). Furthermore, children with abnormal oral sensitivity among those with ASD refused food more frequently and ate less. Very few studies have hypothesized oral sensory deficits as a reason or a component that restricted the occurrence of functional verbal communication in autistic children. One of the most frequently mentioned causes of delayed verbal communication development in autistic children is sensory abnormalities in the detection of external cues. However, this explanation has received less attention than others. Therefore, in the present study, the aim was to assess the correlation between oral sensory issues with feeding and communication in autistic children.
Method
Participants
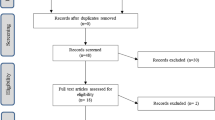
Participants were recruited from different tertiary care hospitals and private centers based on the inclusion and exclusion criteria. Forty participants either already diagnosed with ASD, of any severity, based on DSM-5 criteria and Childhood Autism Rating Scale (CARS; Schopler et al., 1988), attending therapy, or with a new diagnosis of ASD in the age range of 2.5-7 years (mean age = 4.18; SD = 1.06) were selected for the study. Participants were excluded if they presented other neurodevelopmental disorders such as attention-deficit/hyperactivity disorder (ADHD), intellectual disability (ID), or specific language impairment (SLI). Details of the participants along with the severity are provided in Table 1.
Procedure
Approval and informed consent were obtained from the parents of the participants. After receiving the approval, general background information was collected from the parents/caregivers of participants. This included birth history, family history, and developmental milestones in terms of motor, speech and language, social skills, and behavioral skills.
After collecting the background information, an informal evaluation was done of the participants. Results revealed poor verbal and non-verbal communication and feeding skills. Following this SP-2, CSBS-DP and BPFAS questionnaires were administered to identify the relationship among these three domains in autistic children. Though these test materials were not developed in India, they are being widely used in India to assess sensory skills, communication aspects, and feeding behaviors, respectively.
The parents/caregivers were either native speakers of Malayalam or Kannada or were fluent in English. For the SP-2 administration, the clinician interviewed the parents in their native language and recorded their responses regarding the child’s performance in response to the stimuli. To acquire the results, the raw scores were analyzed and appraised. English-speaking parents/caregivers were given the CSBS-DP and BPFAS checklists and instructed to record the responses themselves. An interview was conducted for parents who had trouble responding to the questions in writing or reading. Total scores for each of the test materials were summed up and compared with the normative to identify the issues and deficits. All the details were documented in the data collection sheet and Excel sheet.
Measures
Child Sensory Profile 2, one of the variations of Sensory Profile-2, was used to measure oral sensory difficulties (SP-2; Dunn, 2014). It contains several sensory sections such as visual, auditory, touch, movement, body position, oral sensory, and social emotional responses. Only 10 items from the oral sensory section were used as the study objective was to investigate oral sensory issues and their association with feeding and communication deficits in autistic children.
The Behavioral Pediatric Feeding Assessment Scale (BPFAS; Crist & Napier-Phillips, 2001) is a validated 35-item parental report questionnaire with 70 items designed to examine children’s feeding behaviors and difficulties. This test was used as it measures the mealtime behavioral issues, such as parental stress and anxiety during feeding time, and the need for forceful feeding on refusal to eat in addition to the participants’ feeding abilities.
Communication and Symbolic Behavior Scales Developmental Profile Infant/Toddler Checklist (CSBS-DP; Wetherby & Prizant, 2002) measures communication skills using seven communication predictors including emotional expression and eye gaze, communication, gestures, sound production, word production, word comprehension, and object use. Total scores were calculated for the oral sensory section of SP-2, BPFAS, and CSBS-DP.
Data Analyses
Oral Sensory Section of SP-2
The child’s frequency of each item behavior was measured on a Likert scale that ranged from 1 (almost never = 10% or less) to 5 (almost always = 90% or more). Out of a possible 50 points, the total score for the oral sensory section was calculated and was then classified as, “less than others” (score less than 7), “just like many others” (score between 8 and 24), “more than others” (score 25-32), and “much more than others” (score between 33 and 50).
Behavioral Pediatric Feeding Assessment Scale (BPFAS)
The first 25 Likert-style items are about the child’s feeding behaviors (which are added together to get the child frequency score (CFS), and the next 10 are about parental mealtime strategies and feelings (totaled to get the parent frequency score (PFS)). Total frequency score (TFS) was calculated by adding the CFS and PFS. “Is this a problem for you?” poses a yes/no question after each of the Likert-style objects. The child problem score (CPS) was calculated using questions that can be answered either as “yes” or “no” for the first 25 Likert-style items, whereas the parent problem score (PPS) was calculated using the last 10 questions. The total problem score was calculated by adding the CPS and PPS (TPS). All 35 Likert scale items ranged from 1 to 5, with 1 being “never” and 5 being “always.” When the questionnaire was graded, favorable scores were converted because questions were given as either positive or negative. The resulting TFS was graded on a scale of 175 points. The TPS was scored out of a maximum of 35 points, with one point awarded for each “yes” response. As a result, higher TPS and TFS scores were suggestive problematic feeding behaviors and parental difficulties in dealing with them, respectively.
Communication and Symbolic Behavior Scales Developmental Profile Infant/Toddler Checklist (CSBS-DP)
The test had 24 questions with points ranging from 0 to 4 in seven language predictors. Items marked “Not Yet” received a score of 0, “Sometimes” received one point, and “Often” received two points. “None” received 0 points, and questions with numbered choices received 1 to 4 points. The sum of the points in each cluster yielded seven distinct cluster scores, namely “emotion and use of eye gaze,” “use of communication,” “use of gestures,” “use of sounds,” “use of words,” “understanding of words,” and “use of objects”. The cluster scores were added up to create three composite scores including “communication composite,” “expressive speech composite,” and “symbolic composite”. These scores when added together provided the final score that was then compared to the normative score. The lesser the score, the more at risk for developing communication impairment.
After scoring, the results were subjected to statistical analysis. Spearman’s rank correlation was used to investigate the relationship between oral sensory difficulties and each of the independent variables, CSBS-DP and BPFAS. The strength of association and relationship between the variables was also examined. In addition to establishing the correlation, this step also helped to check the linearity in the relationship between the SP-2 scores and each of the independent variables. SPSS Statistics version 21 was used for all analyses.
Results
The present study looked at the SP-2 ratings for any variations in oral sensory sensitivity processing subscales. The mean and standard deviation for different classifications is given in Table 2. On average, autistic children scored higher, indicating more atypical oral sensory processing. Among 40 autistic children, 23 (57%) revealed oral sensory scores between 25 and 32, classified as “more than others” (mean = 28.52; SD = 2.3), and 10 (25%) scored between 8 and 24, classified as “just like the majority of others” (mean = 17.40, SD = 3.43) and 7 (18%) between 33 and 50, classified as “much more than others” (mean = 39.14, SD = 4.59). The mean age of the oral sensory subgroups was not notably different, and gender was not significantly related to any of these factors.
Table 3 shows the mean, standard deviation, and range for the expression, expressive speech, symbolic composites, and overall score. On average, autistic children had poorer cut-offs for all the composites and total scores indicating their falling in the range of concern, i.e., they were not communicating their needs as expected for their age. Furthermore, the overall mean of the expressive speech composite was less compared to the communication and symbolic composite scores.
Table 4 shows the mean, standard deviation, and range for the total frequency score (TFS) and total problem score (TPS). On average, autistic children had problematic behaviors exhibited during feeding time and parental difficulties in dealing with them. Investigators also noted that mealtime induced stress in families of autistic children.
Correlation Between Oral Sensory and Communication
Spearman’s rank correlation was performed as the data violated the normality assumption and was found to be a correlation coefficient of −0.29 (p-value = 0.075). A weak negative correlation existed between these two variables which was not statistically significant. Figure 1 shows the scatter diagram of the analysis.
Correlation Between Oral Sensory and Feeding
Spearman’s rank correlation was performed as data violated the normality assumption. A moderate positive correlation existed between oral sensory score with TFS and TPS with statistical significance. Spearman’s rank correlation coefficient 0.43 p-value = 0.006 for oral sensory and TFS (Figure 2) and 0.005 for oral sensory and TPS (Figure 3).
Discussion
The present study investigated oral sensory issues and their association with feeding and communication deficits in autistic children and attempted to find out the correlation among the three variables. The primary objective was to explore the oral sensory issues found among autistic children. In the present study, on average, autistic children scored higher in the oral sensory processing section of SP-2, indicating increased atypical oral sensory processing. The majority of the children had selective eating habits especially concerning food textures, compared to other oral sensory issues. In addition, they exhibited a craving for food, taste and smell, ate only certain tastes, and were limited to certain food textures. Previous studies have also reported that autistic children have greater oral sensory problems (Ermer & Dunn, 1998; Hazen et al., 2014; Leekam et al., 2007; Nadon et al., 2011; Rogers et al., 2003; Tomchek & Dunn, 2007). However, in the present study, no considerable differences in oral sensory processing in terms of age and gender were observed.
Previous research has confirmed that autistic children possess greater feeding challenges and food preferences than children who are typically developing (Bandini et al., 2010; Ledford & Gast, 2006; Schreck & Williams, 2006; Sharp et al., 2013; Williams et al., 2005; Zimmer et al., 2012). The present study evaluated how abnormal oral sensory processing may be associated with feeding problems and food selection. It was observed that the majority of the children scored “more than others” on SP-2 of the oral sensory processing section, suggesting higher oral sensory processing deficits in autistic children. Furthermore, the findings of this study revealed that children with unusual oral sensory sensitivity also had feeding issues. They chewed food poorly, ate less variety of fruits and vegetables, ate strained/soft food, got up from the table during mealtime, spat food, and exhibited tantrums during feeding time. They also took more than 20 min to finish their meal. A great number of parents of autistic children reported mealtime behavioral issues, such as parental stress and anxiety during feeding time, and the need for forceful feeding on refusal to eat. This suggests that children who exhibit oral sensory issues may have food selectivity and restrictive eating behaviors. This is consistent with earlier research in the literature that claimed autistic children may have particular food preferences due to sensory dysfunction, specifically oral sensory issues (Cermak et al., 2010; Suarez, 2012; Zobel-Lachiusa et al., 2015). Children who have oral sensory sensitivity can restrict their diet to foods that they prefer, find manageable, or tolerate (Cermak et al., 2010). In the present study, mealtime was a cause of stress in families of autistic children, a finding congruent with previous qualitative studies (Ausderau & Juarez, 2013; Marquenie et al., 2011; Suarez, 2012; Zobel-Lachiusa et al., 2015). However, parents’ preferences for food were not collected for the current study analysis and hence, it is not clear if the food options and preferences of parents had influenced the food selectivity/food habits of autistic children. Furthermore, it was noted that parents’ choices of food were restricted to a lesser variety of meals, leading to a limited number of children’s food repertoires (Chistol et al., 2018). Besides, only the food that was offered was rejected by the autistic children, as reported by the parents.
Even though this study has not assessed oral sensory sensitivity, it could provide information regarding food selectivity behaviors in autistic children to delineate variations between over and under-sensitivity towards stimuli. For instance, oral over-sensitivity can make textures challenging and make it difficult to eat, whereas oral under-sensitivity in which children may not seem to interpret sensation sufficiently can lead to a child eating significant quantities of a certain food or stuffing food in the mouth (Cermak et al., 2010). In several studies, neurobiological processes were suggested to understand how oral sensitiveness could lead to food-selective behavior. Food selectivity in children diagnosed with ASD is influenced by medical, genetic, cultural, maternal, and developmental influences (Sharp et al., 2013; Takasaki & Baron-Cohen, 2012), restricted preferences and/or behavior rigidity (Johnson et al., 2014; Schreck et al., 2004; Suarez et al., 2014), and differing perceptions of smell and taste sensations (Bennetto et al., 2007).
The next objective of this study was to find out the correlation between oral sensory and communication issues. On scoring CSBS-DP to check for communicative competence, autistic children had poorer cut-offs for all the composite and total scores of CSBS-DP indicating that they came in the range of concern i.e., they were not communicating their needs as expected of their age. The test also provided insight into the oral production capacity of the participants (though not exhaustive) through the “expressive speech composite” score. Among the 3 composite scores (communication, expressive speech, and symbolic), the expressive speech composite score was found to be the lowest for participants. This indicates that autistic children have reduced expressive vocabulary and poor oral production. With respect to other communication deficits, the children showed poor name call response, not paying attention to speech, or pointing to objects, requesting for objects, asking for help, and overall poor communication skills. This finding is in congruence with the previous studies reporting autistic children having deficiencies in social communication at all ages and levels (Tager-Flusberg et al., 2001).
Results of the current study suggest a low negative correlation between the oral sensory processing score of SP-2 and CSBS-DP (r = −0.24, p = 0.13), indicating that the higher the oral sensory scores, the higher the oral sensory dysfunction, and the poorer communication skills including poor oral production. It was also observed that those children who fell in the category of “just like the majority of others” in the oral sensory processing section of SP-2 also exhibited communication impairment. Similar findings are reported in the literature suggesting that oral sensory issues and communication difficulties are common in autistic children (Baranek et al., 2013; Watson et al., 2011). In addition, it is reported in the literature that both sensory hypo-responsiveness and sensory-seeking behaviors are negatively correlated with language skills indicating that sensory processing skills play an important role in the rate of language acquisition and communication skills (Watson et al., 2011). Furthermore, oral sensory problems may not be considered the only issue limiting the growth of communication development in autistic children. Unusual sensory responses can lead to some of the signs of communication associated with ASD, not exclusively addressed in the current study. Therefore, it cannot be emphatically stated that oral sensory deficits can cause communication issues. It was interesting to note that even with therapeutic intervention, children were exhibiting atypical oral sensory processing, feeding issues, and communication deficits.
The current study provides insight into autistic children having feeding and communication problems due to oral sensory issues. Although the impact of sensory processing problems on verbal communication has been hypothesized, no studies in the literature have specifically addressed the potential for sensory response patterns to be a factor constraining the development of verbal communication (i.e., by grouping participants based on the presence or absence of verbal communication) in autistic children. Hence, the present study is a preliminary attempt aimed at highlighting the importance of addressing the oral sensory issues. In summary, a clear link between oral sensory and feeding issues has been established. Feeding issues exhibited included ritualized eating, food rejection, and mealtime refusal. Besides, a relationship between oral sensory issues and communication deficits has been identified, particularly with oral production. This hints at the necessity to examine the oral sensory processing deficits in autistic children as it could lead to other problematic behaviors such as communication and feeding deficits. It is always advisable for a team of medical specialists including speech-language pathologists, clinical psychologists, occupational therapists, nutritionists, dieticians, and others to work together to identify and manage autistic children. Working with a multidisciplinary team will be helpful for autistic children who experience extraordinary oral sensory sensitivity, feeding issues, and communication difficulties.
Limitations and Future Research
The present study did not relate the results to the severity of the disorder or quantify the type and nature of therapeutic intervention received. Since the study used different self-reported measurement tools to assess the sensory, feeding, and communication skills, common test administration bias could have affected the test results. More research is warranted in the future to recognize and address problems related to oral sensory, feeding, and oral communication. Furthermore, with the limited sample, the relationship or extent to which behavior aligns with feeding and oral communication requires further investigation. Autistic children have variable over-sensitivity and under-sensitivity issues. However, only limited studies on over and under-sensitivity of taste/smell stimuli have been published. This calls for future studies focusing on the same. The current study has indicated that sensory influences could be manifested in autistic children as food selectivity. Further studies are necessary to clarify the extent of the relationship among feeding issues, food selectivity, and oral sensory processing factors. In-depth studies on the relationship between oral production and oral sensory issues or sensory issues and communication skills will be a fruitful area of research in the future. The present study is based on a cross-sectional design which limits the conclusions that can be drawn from the data. By the use of a cross-sectional design, no causal relationship regarding the investigated variables can be drawn as what is seen are only correlations that speak of associations and not predictions of causality.
Change history
12 June 2023
Added unnecessary data in the section head Limitations and Future Research.
References
Allen, S. L., Smith, I. M., Duku, E., Vaillancourt, T., Szatmari, P., Bryson, S., Fombonne, E., Volden, J., Waddell, C., Zwaigenbaum, L., Roberts, W., Mirenda, P., Bennett, T., Elsabbagh, M., & Georgiades, S. (2015). Behavioral pediatrics feeding assessment scale in young children with autism spectrum disorder: Psychometrics and associations with child and parent variables. Journal of Pediatric Psychology, 40(6), 581–590. https://doi.org/10.1093/jpepsy/jsv006
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed, pp. 50–59). American Psychiatric Publishing.
Aswathy, A. K., Manoharan, A., & Manoharan, A. (2016). Addressing oral sensory issues and possible remediation in children with autism spectrum disorders: Illustrated with a case study. International Journal of Medical and Health Sciences, 10(7), 400–403.
Ausderau, K., & Juarez, M. (2013). The impact of autism spectrum disorders and eating challenges on family mealtimes. ICAN: Infant, Child, and Adolescent Nutrition, 5(5), 315–323. https://doi.org/10.1177/1941406413502808
Ayres, A. J. (1963). The development of perceptual-motor abilities: A theoretical basis for treatment of dysfunction. American Journal of Occupational Therapy, 17(6), 221–225 https://pubmed.ncbi.nlm.nih.gov/14072429/
Baghdadli, A., Assouline, B., Sonié, S., Pernon, E., Darrou, C., Michelon, C., Picot, M. C., Aussilloux, C., & Pry, R. (2012). Developmental trajectories of adaptive behaviors from early childhood to adolescence in a cohort of 152 children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(7), 1314–1325. https://doi.org/10.1007/s10803-011-1357-z
Baker, A. E., Lane, A., Angley, M. T., & Young, R. L. (2008). The relationship between sensory processing patterns and behavioral responsiveness in autistic disorder: A pilot study. Journal of Autism and Developmental Disorders, 38(5), 867–875. https://doi.org/10.1007/s10803-007-0459-0
Bandini, L. G., Anderson, S. E., Curtin, C., Cermak, S., Evans, E. W., Scampini, R., Maslin, M., & Must, A. (2010). Food selectivity in children with autism spectrum disorders and typically developing children. The Journal of Pediatrics, 157(2), 259–264. https://doi.org/10.1016/j.jpeds.2010.02.013
Baranek, G. T., Watson, L. R., Boyd, B. A., Poe, M. D., David, F. J., & McGuire, L. (2013). Hypo-responsiveness to social and non-social sensory stimuli in children with autism, children with developmental delays, and typically developing children. Development and Psychopathology, 25(2), 307–320. https://doi.org/10.1017/S0954579412001071
Bennetto, L., Kuschner, E. S., & Hyman, S. L. (2007). Olfaction and taste processing in autism. Biological Psychiatry, 62(9), 1015–1021. https://doi.org/10.1016/j.biopsych.2007.04.019
Ben-Sasson, A., Cermak, S. A., Orsmond, G. I., Tager-Flusberg, H., Carter, A. S., Kadlec, M. B., & Dunn, W. (2007). Extreme sensory modulation behaviors in toddlers with autism spectrum disorders. American Journal of Occupational Therapy, 61(5), 584–592. https://doi.org/10.5014/ajot.61.5.584
Cermak, S. A., Curtin, C., & Bandini, L. G. (2010). Food selectivity and sensory sensitivity in children with autism spectrum disorders. Journal of the American Dietetic Association, 110(2), 238–246. https://doi.org/10.1016/j.jada.2009.10.032
Chistol, L. T., Bandini, L. G., Must, A., Phillips, S., Cermak, S. A., & Curtin, C. (2017). Sensory sensitivity and food selectivity in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(2), 583–591. https://doi.org/10.1007/s10803-017-3340-9
Chistol, L. T., Bandini, L. G., Must, A., Phillips, S., Cermak, S. A., & Curtin, C. (2018). Sensory sensitivity and food selectivity in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(2), 583–591. https://doi.org/10.1007/s10803-017-3340-9
Crist, W., & Napier-phillips, A. (2001). Mealtime behaviors of young children: A comparison of normative and clinical data. Journal of Developmental & Behavioral Pediatrics, 22(5), 279–286. https://doi.org/10.1097/00004703-200110000-00001
Cumine, V., Leach, J., & Stevenson, G. (2000). The pre-school child with autism. .
Dunn, W. (2014). Child Sensory Profile–2 user’s manual. Pearson.
Ermer, J., & Dunn, W. (1998). The sensory profile: A discriminant analysis of children with and without disabilities. American Journal of Occupational Therapy, 52(4), 283–290. https://doi.org/10.5014/ajot.52.4.283
Hazen, E. P., Stornelli, J. L., O’Rourke, J. A., Koesterer, K., & McDougle, C. J. (2014). Sensory symptoms in autism spectrum disorders. Harvard Review of Psychiatry, 22(2), 112–124. https://doi.org/10.1097/01.HRP.0000445143.08773.58
Herndon, A. C., DiGuiseppi, C., Johnson, S. L., Leiferman, J., & Reynolds, A. (2009). Does nutritional intake differ between children with autism spectrum disorders and children with typical development? Journal of Autism and Developmental Disorders, 39(2), 212–222. https://doi.org/10.1007/s10803-008-0606-2
Hilton, C., Graver, K., & LaVesser, P. (2007). Relationship between social competence and sensory processing in children with high functioning autism spectrum disorders. Research in Autism Spectrum Disorders, 1(2), 164–173. https://doi.org/10.1016/j.rasd.2006.10.002
Johnson, C. R., Turner, K., Stewart, P. A., Schmidt, B., Shui, A., Macklin, E., & Hyman, S. L. (2014). Relationships between feeding problems, behavioral characteristics and nutritional quality in children with ASD. Journal of Autism and Developmental Disorders, 44(9), 2175–2184. https://doi.org/10.1007/s10803-014-2095-9
Kientz, M. A., & Dunn, W. (1997). A comparison of the performance of children with and without autism on the sensory profile. American Journal of Occupational Therapy, 51(7), 530–537. https://doi.org/10.5014/ajot.51.7.530
Kobayashi, R., Murata, T., & Yoshinaga, K. (1992). A follow-up study of 201 children with autism in Kyushu and Yamaguchi areas, Japan. Journal of Autism and Developmental Disorders, 22(3), 395–411. https://doi.org/10.1007/BF01048242
Kodak, T., & Piazza, C. C. (2008). Assessment and behavioral treatment of feeding and sleeping disorders in children with autism spectrum disorders. Child and Adolescent Psychiatric Clinics of North America, 17(4), 887–905. https://doi.org/10.1016/j.chc.2008.06.005
Ledford, J. R., & Gast, D. L. (2006). Feeding problems in children with autism spectrum disorders: A review. Focus on Autism and Other Developmental Disabilities, 21(3), 153–166. https://doi.org/10.1177/10883576060210030401
Leekam, S. R., Nieto, C., Libby, S. J., Wing, L., & Gould, J. (2007). Describing the sensory abnormalities of children and adults with autism. Journal of Autism and Developmental Disorders, 37(5), 894–910. https://doi.org/10.1007/s10803-006-0218-7
Liss, M., Saulnier, C., Fein, D., & Kinsbourne, M. (2006). Sensory and attention abnormalities in autistic spectrum disorders. Autism: The International Journal of Research and Practice, 10(2), 155–172. https://doi.org/10.1177/1362361306062021
Lord, C., Risi, S., & Pickles, A. (2004). Trajectory of language development in autistic spectrum disorders. In M. L. Rice & S. F. Warren (Eds.), Developmental language disorders: From phenotypes to etiologies (pp. 7–29). Lawrence Erlbaum Associates Publishers.
Marquenie, K., Rodger, S., Mangohig, K., & Cronin, A. (2011). Dinnertime and bedtime routines and rituals in families with a young child with an autism spectrum disorder. Australian Occupational Therapy Journal, 58(3), 145–154. https://doi.org/10.1111/j.1440-1630.2010.00896.x
Miller, L. J., Schoen, S. A., James, K., & Schaaf, R. C. (2007). Lessons learned: A pilot study on occupational therapy effectiveness for children with sensory modulation disorder. American Journal of Occupational Therapy, 61(2), 161–169. https://doi.org/10.5014/ajot.61.2.161
Nadon, G., Feldman, D. E., Dunn, W., & Gisel, E. (2011). Association of sensory processing and eating problems in children with autism spectrum disorders. Autism Research and Treatment, 2011, 1–8. https://doi.org/10.1155/2011/541926
Patten, E., Ausderau, K. K., Watson, L. R., & Baranek, G. T. (2013). Sensory response patterns in nonverbal children with ASD. Autism Research and Treatment, 1–9.
Pickett, E., Pullara, O., O’Grady, J., & Gordon, B. (2009). Speech acquisition in older nonverbal individuals with autism: A review of features, methods, and prognosis. Cognitive and Behavioral Neurology, 22(1), 1–21. https://doi.org/10.1097/WNN.0b013e318190d185
Rogers, S., Hepburn, S., & Wehner, E. (2003). Parent reports of sensory symptoms in toddlers with autism and those with other developmental disorders. Journal of Autism and Developmental Disorders, 33(6), 631–642. https://doi.org/10.1023/b:jadd.0000006000.38991.a7
Schopler, E., Reichler, R. J., & Renner, B. R. (1988). The Childhood Autism Rating Scale. Western Psychological Services.
Schreck, K., & Williams, K. (2006). Food preferences and factors influencing food selectivity for children with autism spectrum disorders. Research in Developmental Disabilities, 27(4), 353–363. https://doi.org/10.1016/j.ridd.2005.03.005
Schreck, K. A., Williams, K., & Smith, A. F. (2004). A comparison of eating behaviors between children with and without autism. Journal of Autism and Developmental Disorders, 34(4), 433–438. https://doi.org/10.1023/b:jadd.0000037419.78531.86
Shah, S. P., Joshi, A., & Kulkarni, V. (2015). Prevalence of sensory processing dysfunction and patterns on sensory profile of children with autism spectrum disorder in Mumbai: A pilot study. Indian Journal of Occupational Therapy, 47(2), 52–57.
Sharp, W. G., Jaquess, D. L., & Lukens, C. T. (2013). Multi-method assessment of feeding problems among children with autism spectrum disorders. Research in Autism Spectrum Disorders, 7(1), 56–65. https://doi.org/10.1016/j.rasd.2012.07.001
Sigman, M., & McGovern, C. W. (2005). Improvement in cognitive and language skills from preschool to adolescence in autism. Journal of Autism and Developmental Disorders, 35(1), 15–23. https://doi.org/10.1007/s10803-004-1027-5
Suarez, M. A. (2012). Sensory processing in children with autism spectrum disorders and impact on functioning. Pediatric Clinics of North America, 59(1), 203–214. https://doi.org/10.1016/j.pcl.2011.10.012
Suarez, M. A., Nelson, N. W., & Curtis, A. B. (2014). Longitudinal follow-up of factors associated with food selectivity in children with autism spectrum disorders. Autism, 18(8), 924–932. https://doi.org/10.1177/1362361313499457
Tager- Flusberg, H., Joseph, R., & Folstein, S. (2001). Current directions in research on autism. Mental Retardation and Developmental Disabilities Research Reviews, 7(1), 21-29. 10.1002/1098-2779(200102)7:1<21::AID-MRDD1004>3.0.CO;2-3.
Talay-Ongan, A., & Wood, K. (2000). Unusual sensory sensitivities in autism: A possible crossroads. International Journal of Disability, Development and Education, 47(2), 201–212. https://doi.org/10.1080/713671112
Tavassoli, T., & Baron-Cohen, S. (2012). Taste identification in adults with autism spectrum conditions. Journal of Autism and Developmental Disorders, 42(7), 1419–1424. https://doi.org/10.1007/s10803-011-1377-8
Tomchek, S. D., & Dunn, W. (2007). Sensory processing in children with and without autism: A comparative study using the short sensory profile. The American Journal of Occupational Therapy, 61(2), 190–200. https://doi.org/10.5014/ajot.61.2.190
Venter, A., Lord, C., & Schopler, E. (1992). A follow-up study of high-functioning autistic children. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 33(3), 489–507. https://doi.org/10.1111/j.1469-7610.1992.tb00887.x
Watson, L. R., Patten, E., Baranek, G. T., Poe, M., Boyd, B. A., Freuler, A., & Lorenzi, J. (2011). Differential associations between sensory response patterns and language, social, and communication measures in children with autism or other developmental disabilities. Journal of Speech, Language, and Hearing Research, 54(6), 1562–1576. https://doi.org/10.1044/1092-4388(2011/10-0029)
Wetherby, A. M., & Prizant, B. M. (2002). Communication and symbolic behavior scales: Developmental profile. Paul H Brookes Publishing Co..
Williams, K. E., Gibbons, B. G., & Schreck, K. A. (2005). Comparing selective eaters with and without developmental disabilities. Journal of Developmental and Physical Disabilities, 17(3), 299–309. https://doi.org/10.1007/s10882-005-4387-7
Williams, K. L., Kirby, A. V., Watson, L. R., Sideris, J., Bulluck, J., & Baranek, G. T. (2018). Sensory features as predictors of adaptive behaviors: A comparative longitudinal study of children with autism spectrum disorder and other developmental disabilities. Research in Developmental Disabilities, 81, 103–112. https://doi.org/10.1016/j.ridd.2018.07.002
Yack, E., Sutton, S., & Aquilla, P. (2015). Building bridges through sensory integration (3rd ed.). Therapy for children with autism and other pervasive developmental disorders.
Zeidan, J., Fombonne, E., Scorah, J., Ibrahim, A., Durkin, M. S., Saxena, S., Yusuf, A., Shih, A., & Elsabbagh, M. (2022). Global prevalence of autism: A systematic review update. Autism Research, 15(5), 778–790. https://doi.org/10.1002/aur.2696
Zimmer, M. H., Hart, L. C., Manning-Courtney, P., Murray, D. S., Bing, N. M., & Summer, S. (2012). Food variety as a predictor of nutritional status among children with autism. Journal of Autism and Developmental Disorders, 42(4), 549–556. https://doi.org/10.1007/s10803-011-1268-z
Zlomke, K., Rossetti, K., Murphy, J., Mallicoat, K., & Swingle, H. (2020). Feeding problems and maternal anxiety in children with autism spectrum disorder. Maternal and Child Health Journal, 24(10), 1278–1287. https://doi.org/10.1007/s10995-020-02966-8
Zobel-Lachiusa, J., Andrianopoulos, M. V., Mailloux, Z., & Cermak, S. A. (2015). Sensory differences and mealtime behavior in children with autism. The American Journal of Occupational Therapy, 69(5), 6905185050. https://doi.org/10.5014/ajot.2015.016790
Acknowledgements
We would like to acknowledge the participants and the head of the departments of the private centers who allowed us to interact and collect data from their patient population.
Funding
Open access funding provided by Manipal Academy of Higher Education, Manipal
Author information
Authors and Affiliations
Contributions
Conceptualization: Nivedya Maria Raj, Kadiyali Damodar Veena; data curation: Nivedya Maria Raj; formal analysis: Nivedya Maria Raj, Kadiyali Damodar Veena; Investigation: Nivedya Maria Raj; methodology: Nivedya Maria Raj, Kadiyali Damodar Veena; project administration: Nivedya Maria Raj, Kadiyali Damodar Veena; resources: Nivedya Maria Raj, Kadiyali Damodar Veena; validation: Nivedya Maria Raj, Kadiyali Damodar Veena; visualization: Nivedya Maria Raj, Kadiyali Damodar Veena; writing—original draft: Nivedya Maria Raj, Kadiyali Damodar Veena; writing—review and editing: Bellur Rajashekhar, Ashitha Sreelakshmi C. A.
Corresponding author
Ethics declarations
Ethics Approval
Ethical approval for the study was obtained from Institutional Research Committee (IRC) of Manipal College of Health Professions, MAHE, Manipal and Kasturba Medical College and Kasturba Hospital—Institutional Ethics Committee (IEC approval 206/2020) of MAHE, Manipal.
Consent to Participate
Informed consent was obtained from the parents of children included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Raj, N.M., Veena, K.D., Rajashekhar, B. et al. Oral Sensory Issues with Feeding and Communication Skills in Autistic Children. Adv Neurodev Disord 8, 271–280 (2024). https://doi.org/10.1007/s41252-023-00338-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41252-023-00338-1