Abstract
Objectives
While national medical guidelines recommend genetic testing for all individuals with non-syndromic autism spectrum disorder (ASD), there is underutilization of genetic testing. This study aims to define the perspectives and approaches to initial genetic testing of ASD diagnosticians in order to improve utilization.
Methods
A prospective cross-sectional study was conducted using an anonymous online survey distributed to 59 staff neurologists, developmental-behavioral pediatricians, psychologists, post-graduate physician fellows, and nurse practitioners from a single academic medical center. Questions explored knowledge, attitudes, and practices of initial genetic testing for ASD among diagnosticians.
Results
Among the 30 respondents (51% response rate), a lack of comprehensive pre-test genetic counseling was identified and forgetfulness was the most prevalent reason for not recommending genetic testing (n = 7/23, 30%). Insurance prior authorization (PA) for genetic testing was a major barrier for clinicians. More than half of respondents (n = 13/25, 52%) reported being uncomfortable with the PA process.
Conclusions
Variability in knowledge and practices among ASD diagnosticians regarding genetic testing was identified. Therefore, potential interventions like clinician and administrative staff education, as well as genetic counselor integration into ASD clinics, may be useful to improve genetic testing utilization.
Similar content being viewed by others
The post-genomic era has placed genetic testing at the forefront of clinical evaluation for individuals with autism spectrum disorder (ASD). Identifying a disease-causing variant can provide diagnostic clarity, guide medical decision-making, influence family planning, and help prognosticate on other medical issues in the affected person (Ellison et al., 2012). There is consensus among medical organizations that genetic testing be offered to all individuals with ASD (Hyman et al., 2020; Satya-Murti et al., 2013; Schaefer et al., 2013; Volkmar et al., 2014). However, completion rates of any genetic testing range between 16 and 41% in the USA (Amiet et al., 2014; Cuccaro et al., 2014; Kiely et al., 2016; Moreno-De-Luca et al., 2020; Narcisa et al., 2013; Zhao et al., 2019b) despite a majority of parents (69–98%) supporting ASD genetic testing (Ayhan et al., 2021; Chen et al., 2013; Codina-Solà et al., 2017; Wagner et al., 2020; Xu et al., 2016; Zhao et al., 2019a). Subspecialty clinics like the Boston Children’s Hospital Autism Spectrum Center (ASC), where it is standard practice to recommend chromosomal microarray (CMA) and fragile X testing for all children with ASD, are only slightly better with a completion rate of 59.8% among toddlers (Harris et al., 2020). There is a gap between national guidelines and genetic testing completion rates and the reason why is unknown.
Issues regarding the expense of testing and lack of insurance coverage have been raised by clinicians and families alike (Harrington et al., 2018; Hendel et al., 2021; Rutz et al., 2019; Xu et al., 2016). Insurance coverage for medically necessary genetic testing varies in the USA (Riggs et al., 2014), despite multiple guidelines recommending at least a CMA for children newly diagnosed with ASD without a readily identifiable genetic syndrome (Hyman et al., 2020; Satya-Murti et al., 2013; Schaefer et al., 2013; Volkmar et al., 2014). Insurance companies may not support genetic testing for various reasons. Genetic testing is expensive and is often an excluded benefit. Some payers reject that genetic testing is medically necessary and claim it is “experimental,” despite standardized analysis methods and known impact on clinical care (Riggs et al., 2014). In order to prevent families from receiving an unwelcome bill for genetic testing not covered under their child’s medical insurance plan, many clinical practices in the USA seek prior authorization before proceeding with DNA collection for genetic testing (Barton et al., 2018). While rates of genetic testing completion are slightly higher (33.8–61.7%) in countries like France, Spain, and Israel where universal public healthcare includes genetic testing, underutilization of genetic testing remains evident (Amiet et al., 2014; Codina-Solà et al., 2017; Hendel et al., 2021).
In addition to cost and insurance coverage of genetic testing, clinician factors have been implicated. Limited knowledge of genetics and test result interpretation, as well as failure to review recommendations with families, may impact whether a child with autism obtains genetic testing (Codina-Solà et al., 2017; Hendel et al., 2021; Rutz et al., 2019; Soda et al., 2021; Wofford et al., 2019). Neurologists, developmental pediatricians, and geneticists have shown variability in genetic test ordering practices (Barton et al., 2018; Domínguez-Carral et al., 2017; Harrington et al., 2018; Wofford et al., 2019). Prior research has focused primarily on the family’s perspective and on views of general pediatricians who may not be comfortable with diagnosing ASD or pursuing genetic testing (Amiet et al., 2014; Codina-Solà et al., 2017; Cuccaro et al., 2014; Harrington et al., 2018; Narcisa et al., 2013; Rutz et al., 2019; Wagner et al., 2020; Zhao et al., 2019a, 2019b). Prior studies have not evaluated the challenges of non-genetics specialists like developmental pediatricians and child neurologists, who diagnose the majority of children and adults with ASD (Hyman et al., 2020). The goal of this study was to evaluate non-geneticist subspecialist perspectives on genetic testing for ASD in order to identify key areas for improvement to increase genetic testing completion rates.
Method
Participants
Participants were recruited from a single academic medical center, The Boston Children’s Hospital Autism Spectrum Center (ASC). The ASC includes physicians, nurse practitioners, and developmental psychologists from the Department of Neurology and the Division of Developmental Medicine with expertise in ASD. Individuals with suspected ASD undergo comprehensive diagnostic evaluations by either Neurology or Developmental Medicine clinicians based upon their needs and associated medical issues after a centralized intake process. Neurology evaluations are supervised by a staff neurologist or neurology nurse practitioner, with developmental psychology visits conducted separately on a referral basis. Evaluations in Developmental Medicine are often team-based visits supervised by both a developmental-behavioral pediatrician and developmental psychologist. Psychologists were included in this study since they provide essential counseling on new ASD diagnoses, including possible etiologies, and often arrange follow-up medical care, even though ordering and interpretation of genetic testing is outside of their scope of practice. Trainees include fellows in developmental-behavioral pediatrics, neurodevelopmental disabilities, and developmental psychology. All trainees led autism evaluations under the supervision of a staff clinician at the ASC. All trainees and staff clinicians had received prior education regarding institutional guidelines to recommend genetic testing for all individuals newly diagnosed with ASD.
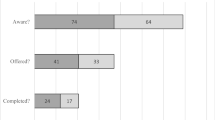
Of the 59 potential respondents who had been in practice at the Boston Children’s Hospital ASC for at least 6 months, About half (n = 30/59, 51%) completed the questionnaire. The response rate was similar across the Department of Neurology and the Division of Developmental Medicine (Table 1). The majority of respondents was physicians, including attending physicians (n = 15/30, 50%) and physician fellows in developmental-behavioral pediatrics and neurodevelopmental disabilities (n = 8, 27%). Most of the respondents diagnosed patients with ASD at least 1–3 times per month (n = 26, 87%). All clinicians endorsed recommending genetic testing for patients, with 25 (83%) always and 5 (17%) often doing so. Clinicians reported that patient families are interested in genetic testing, including CMA, either often (n = 20/29, 69%), sometimes (n = 8, 28%), or always (n = 1, 3%).
Procedure
An anonymous online survey was distributed to clinicians and results were collected between October and November 2018. Study data were collected and managed using REDCap electronic data capture tools hosted at Boston Children’s Hospital (Harris et al., 2009, 2019). Respondents could opt into a gift card raffle by providing an email address, which was not linked to their responses.
Measures
An 18-question survey was designed about knowledge, attitudes, and practices regarding ASD genetic testing after gathering perspectives from meetings with staff Neurology and Developmental Medicine clinicians. Respondents were asked about their approach to completing ASD genetic tests in clinic, barriers to testing, and opportunities for improvement in a free-text section (See Supplementary Materials). Non-personally identifiable demographic information was collected on clinician type, level of training, and frequency of diagnosing ASD.
Data Analyses
Descriptive analysis was performed using all available responses, excluding missing data and answers marked as “not applicable” by individual question. Thematic analysis was performed on free-text comments at the end of the survey. The Boston Children’s Hospital Institution Review Board confirmed the protocol to be exempt from review, including a waiver of informed consent.
Results
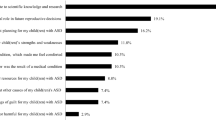
Regarding pre-test genetic counseling, most respondents reviewed the importance and yield of genetic testing in ASD, the possible outcomes, the financial burden, and need for insurance prior authorization with families (Fig. 1). However, only 40% of clinicians reported that they discuss the specific methodology of initial testing options, such as discussing that microarray only detects deletions and duplications, and only 3% discussed concerns of identifying consanguinity based upon single-nucleotide polymorphism (SNP) microarrays.
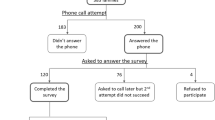
Among the 23 clinicians who provided at least one reason why they may not recommend genetic testing (Fig. 2), forgetfulness (n = 7/23, 30%) was the most commonly identified reason. Other reasons included insufficient time during clinic visits (n = 6, 26%), concerns about parental anxiety (n = 5, 22%), assumptions that insurance would not cover genetic testing (n = 5, 22%), and limited knowledge of how to obtain insurance authorization (n = 5, 22%). Twenty-five clinicians rated the overall process for ordering CMA on a 5-point Likert scale ranging from 1 as “very difficult” to 5 as “very easy,” and the median score was 2 or “somewhat difficult.”
Nearly all clinicians (n = 25/28, 89%) requested that the patient’s caregivers contact the insurance company as the first step to obtain insurance authorization for genetic testing, while only two (7%) requested their administrative or nursing staff to begin the process of insurance authorization, and one clinician (4%) started the authorization process on their own. Clinicians had various ways of addressing initial denial of insurance coverage for testing: 8 of 26 (31%) respondents contact the insurance company themselves, 8 (31%) refer the family to a geneticist, 5 (19%) do not pursue genetic testing further, and 5 (19%) ask nursing or administrative staff to contact the insurance agency.
Clinicians reported a wide range of comfort with different aspects of obtaining genetic testing for children with ASD (Fig. 3). Areas where clinicians felt most comfortable included ordering genetic testing in the electronic health record, explaining recommendations to families and completing a letter of medical necessity for the insurance authorization process. However, less than half of clinicians (n = 12/25, 48%) reported feeling comfortable with the overall process of obtaining insurance authorization. This finding remained true even when stratifying by clinician role. In fact, 47% (n = 7/15) of attending physicians, the medical professionals with the highest level of training and experience, were uncomfortable with obtaining insurance authorization.
Four themes emerged from free-text responses from clinicians when asked to describe challenges and opportunities for improvement on genetic testing in ASD. Of the 14 responses, 50% highlighted the difficulties with obtaining insurance coverage for genetic tests, ranging from confusion around how to obtain authorization to the “long battle” of getting insurance authorization, and concern about high deductibles for patient families. Other clinicians (n = 3, 21%) mentioned that research-based genetic testing impacted their clinical practice, with three referring families to a research study looking at whole exome sequencing (the Simons Foundation Autism Research Initiative SPARK study (Feliciano et al., 2018) in lieu of clinical genetic testing. The need for additional administrative support was highlighted by two other clinicians (14%). Comments from two psychologists included deferring responsibility of genetic testing to physicians and requesting additional family friendly resources about genetic testing.
Discussion
This study detailed the perspectives of non-genetics ASD clinicians towards genetic testing. In this single-center survey, all clinicians recommended testing and believed most families were interested in genetic evaluation, concerns regarding insurance authorization, lack of sufficient office visit time, forgetfulness, and fear of escalating parental anxiety limit standard of care genetic testing completion. These findings supported previous work in a smaller cohort of clinicians (Barton et al., 2018) and shed new light on the impact of the practice environment on ASD genetic testing. To address forgetfulness, specialists may benefit from automated reminders or a computer decision support system through the electronic health record to encourage discussion of genetic testing options, as have been done in other pediatric contexts (Marin et al., 2021; Nguyen & Menon, 2021). Referral to a geneticist and/or genetic counselor may alleviate some of the barriers, but access to genetics specialists is limited (Mikat-Stevens et al., 2015). The burden of genetic testing often then falls upon the diagnosing clinician given the high prevalence of ASD at 1 in 44 children in the USA (Maenner et al., 2021). A team approach of building capacity within ASD specialty clinics for first-tier testing combined with select referrals to geneticists may be useful.
Clinicians reported the greatest discomfort with obtaining insurance authorization when compared to other aspects of the testing process, including at the attending physician level. This discomfort may be related to the fact that clinicians care for patients with many different insurance plans with frequently changing policies, which is extremely challenging for clinicians and their administrative staff to navigate (Barton et al., 2018). Furthermore, there was variability among clinicians’ responses to initial insurance denials. Some clinicians reported that they submit referrals to a geneticist for help, while others abandoned testing all together. Developing a centralized administrative team to assist clinicians with obtaining insurance authorization and designing a standard protocol to address insurance authorization denials may streamline the genetic testing process to ensure equity in access to standard of care genetic testing.
Clinicians reported that research-based genetic testing was sometimes offered to families in lieu of clinical genetic testing, in part due to challenges with insurance authorization. It is important to note that not all research studies permit result disclosure and even those that do (such as the SPARK study) are not able to provide results in real time. Therefore, research-based testing should largely not be used as a replacement for clinical laboratory assessment.
While the majority of clinicians discussed basic topics in pre-test genetic counseling, there is room for improvement. The use of CMA for copy number variant detection only and the possibility of identifying parental relatedness were rarely discussed with families. If limitations of testing are not discussed, families may incorrectly assume that no further testing is needed or available (Cohen et al., 2013). Additionally, revealing incidental results regarding consanguinity could heighten distress when unexpected compared to being tempered by appropriate pre-test counseling (Helm et al., 2014). This suggests a role for certified genetic counselors integrated into ASD clinics and the development of standardized educational materials for clinicians to use during their visits. Certified genetic counselors are masters-level licensed clinicians who have expertise in genetics and variant interpretation, as well as interpersonal, psychosocial, and counseling skills. Incorporating a genetic counselor into multidisciplinary clinics in a variety of specialties has been shown to increase appropriate ordering of genetic testing, more accurately determine risk of an underlying genetic syndrome, and reduce a family’s anxiety regarding genetic conditions (Ingles et al., 2008; Kishan et al., 2016; Knapke et al., 2012). Given the fast-moving genetic landscape, ASD clinics could benefit tremendously from genetic counselors, including over videoconferencing platforms (Brown et al., 2021; Kubendran et al., 2017).
Limitations and Future Research
As this survey from a small sample focused on a single academic center, the generalizability of these findings may be limited. Non-geneticist autism subspecialists were the selected population of this study due to the institutional expectations that they recommend and consider ordering initial genetic testing, but the valuable perspectives of genetics professionals were not included. Other institutions may have different workflows and personnel involved, which could lead to different outcomes. Regardless of the process though, given the dearth of clinical genetics professionals and long wait times, innovations are needed to empower non-geneticist clinicians to participate in autism genetic testing (Stoll et al., 2018). Additional limitations include possible non-response bias (those who think more favorably about genetic testing in ASD may have been more likely to complete the survey), lack of perspective from the autistic individual or their family, and a focus on forced choice instead of open-ended questions. Nevertheless, challenges with pre-test genetic counseling and the process of genetic testing were acknowledged using this anonymous ASD clinician survey. Future efforts may explore the efficacy and stakeholder experience upon implementation of the following interventions aimed at addressing some of the barriers to genetic test completion such as clinician education on genetic counseling, development of a standardized workflow for genetic testing authorization, and the integration of genetic counselors into clinic visits.
Data Availability
The data that support the findings of this study are available from the corresponding author, S. J. S., upon reasonable request.
References
Amiet, C., Couchon, E., Carr, K., Carayol, J., Cohen, D. (2014) Are there cultural differences in parental interest in early diagnosis and genetic risk assessment for autism spectrum disorder? Frontiers in Pediatrics, 2(32). https://doi.org/10.3389/fped.2014.00032
Ayhan, A. B., Beyazıt, U., Topuz, Ş, Tunay, Ç. Z., Abbas, M. N., & Yılmaz, S. (2021). Autism spectrum disorder and genetic testing: Parents’ attitudes-data from Turkish sample. Journal of Autism and Developmental Disorders, 51(9), 3331–3340. https://doi.org/10.1007/s10803-020-04798-5
Barton, K. S., Tabor, H. K., Starks, H., Garrison, N. A., Laurino, M., & Burke, W. (2018). Pathways from autism spectrum disorder diagnosis to genetic testing. Genetics in Medicine, 20(7), 737–744. https://doi.org/10.1038/gim.2017.166
Brown, E. G., Watts, I., Beales, E. R., Maudhoo, A., Hayward, J., Sheridan, E., & Rafi, I. (2021). Videoconferencing to deliver genetics services: A systematic review of telegenetics in light of the COVID-19 pandemic. Genetics in Medicine, 23(8), 1438–1449. https://doi.org/10.1038/s41436-021-01149-2
Chen, L.-S., Xu, L., Huang, T.-Y., & Dhar, S. U. (2013). Autism genetic testing: A qualitative study of awareness, attitudes, and experiences among parents of children with autism spectrum disorders. Genetics in Medicine, 15(4), 274–281. https://doi.org/10.1038/gim.2012.145
Codina-Solà, M., Pérez-Jurado, L. A., Cuscó, I., & Serra-Juhé, C. (2017). Provision of genetic services for autism and its impact on Spanish families. Journal of Autism and Developmental Disorders, 47(10), 2947–2956. https://doi.org/10.1007/s10803-017-3203-4
Cohen, J., Hoon, A., & Wilms Floet, A. M. (2013). Providing family guidance in rapidly shifting sand: Informed consent for genetic testing. Developmental Medicine and Child Neurology, 55(8), 766–768. https://doi.org/10.1111/dmcn.12102
Cuccaro, M. L., Czape, K., Alessandri, M., Lee, J., Deppen, A. R., Bendik, E., Dueker, N., Nations, L., Pericak-Vance, M., & Hahn, S. (2014). Genetic testing and corresponding services among individuals with autism spectrum disorder (ASD). American Journal of Medical Genetics Part A Part A, 164A(10), 2592–2600. https://doi.org/10.1002/ajmg.a.36698
Domínguez-Carral, J., López-Pisón, J., Macaya, A., Bueno Campaña, M., García-Pérez, M. A., & Natera-de Benito, D. (2017). Genetic testing among Spanish pediatric neurologists: Knowledge, attitudes and practices. European Journal of Medical Genetics, 60(2), 124–129. https://doi.org/10.1016/j.ejmg.2016.11.007
Ellison, J. W., Ravnan, J. B., Rosenfeld, J. A., Morton, S. A., Neill, N. J., Williams, M. S., Lewis, J., Torchia, B. S., Walker, C., Traylor, R. N., Moles, K., Miller, E., Lantz, J., Valentin, C., Minier, S. L., Leiser, K., Powell, B. R., Wilks, T. M., & Shaffer, L. G. (2012). Clinical utility of chromosomal microarray analysis. Pediatrics, 130(5), e1085–e1095. https://doi.org/10.1542/peds.2012-0568
Feliciano, P., Daniels, A. M., Green Snyder, L. A., Beaumont, A., Camba, A., Esler, A., Gulsrud, A. G., Mason, A., Gutierrez, A., Nicholson, A., Paolicelli, A. M., McKenzie, A. P., Rachubinski, A. L., Stephens, A. N., Simon, A. R., Stedman, A., Shocklee, A. D., Swanson, A., Finucane, B., … Chung, W. K. (2018). SPARK: A US cohort of 50,000 families to accelerate autism research. Neuron, 97(3), 488–493https://doi.org/10.1016/j.neuron.2018.01.015
Harrington, J. W., Emuren, L., Restaino, K., & Schrier Vergano, S. (2018). Parental perception and participation in genetic testing among children with autism spectrum disorders. Clinical Pediatrics, 57(14), 1642–1655. https://doi.org/10.1177/0009922818803398
Harris, H. K., Sideridis, G. D., Barbaresi, W. J., Harstad, E. (2020). Pathogenic yield of genetic testing in autism spectrum disorder. Pediatrics, 146(4). https://doi.org/10.1542/peds.2019-3211
Harris, P. A., Taylor, R., Minor, B. L., Elliott, V., Fernandez, M., O’Neal, L., McLeod, L., Delacqua, G., Delacqua, F., Kirby, J., & Duda, S. N. (2019). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208. https://doi.org/10.1016/j.jbi.2019.103208
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Helm, B. M., Langley, K., Spangler, B., & Vergano, S. (2014). Three clinical experiences with SNP array results consistent with parental incest: A narrative with lessons learned. Journal of Genetic Counseling, 23(4), 489–495. https://doi.org/10.1007/s10897-013-9669-0
Hendel, Y., Meiri, G., Flusser, H., Michaelovski, A., Dinstein, I., & Menashe, I. (2021). Factors affecting family compliance with genetic testing of children diagnosed with autism spectrum disorder. Journal of Autism and Developmental Disorders, 51(4), 1201–1209. https://doi.org/10.1007/s10803-020-04589-y
Hyman, S. L., Levy, S. E., Myers, S. M. (2020). Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics, 145(1). https://doi.org/10.1542/peds.2019-3447
Ingles, J., Lind, J. M., Phongsavan, P., & Semsarian, C. (2008). Psychosocial impact of specialized cardiac genetic clinics for hypertrophic cardiomyopathy. Genetics in Medicine, 10(2), 117–120. https://doi.org/10.1097/GIM.0b013e3181612cc7
Kiely, B., Vettam, S., & Adesman, A. (2016). Utilization of genetic testing among children with developmental disabilities in the United States. The Application of Clinical Genetics, 9, 93–100. https://doi.org/10.2147/TACG.S103975
Kishan, A. U., Gomez, C. L., Dawson, N. A., Dvorak, R., Foster, N. M., Hoyt, A., Hurvitz, S. A., Kusske, A., Silver, E. L., Tseng, C., & McCloskey, S. A. (2016). Increasing appropriate BRCA1/2 mutation testing: The role of family history documentation and genetic counseling in a multidisciplinary clinic. Annals of Surgical Oncology, 23(5), 634–641. https://doi.org/10.1245/s10434-016-5545-0
Knapke, S., Nagarajan, R., Correll, J., Kent, D., & Burns, K. (2012). Hereditary cancer risk assessment in a pediatric oncology follow-up clinic. Pediatric Blood & Cancer, 58(1), 85–89. https://doi.org/10.1002/pbc.23283
Kubendran, S., Sivamurthy, S., & Schaefer, G. B. (2017). A novel approach in pediatric telegenetic services: Geneticist, pediatrician and genetic counselor team. Genetics in Medicine, 19(11), 1260–1267. https://doi.org/10.1038/gim.2017.45
Maenner, M. J., Shaw, K. A., Bakian, A. V., Bilder, D. A., Durkin, M. S., Esler, A., Furnier, S. M., Hallas, L., Hall-Lande, J., Hudson, A., Hughes, M. M., Patrick, M., Pierce, K., Poynter, J. N., Salinas, A., Shenouda, J., Vehorn, A., Warren, Z., Constantino, J. N., … Cogswell, M. E. (2021). Prevalence and characteristics of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2018. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, D.C. : 2002), 70(11), 1–16. https://doi.org/10.15585/mmwr.ss7011a1
Marin, J. R., Rodean, J., Mannix, R. C., Hall, M., Alpern, E. R., Aronson, P. L., Chaudhari, P. P., Cohen, E., Freedman, S. B., Morse, R. B., Peltz, A., Samuels-Kalow, M., Shah, S. S., Simon, H. K., & Neuman, M. I. (2021). Association of clinical guidelines and decision support with computed tomography use in pediatric mild traumatic brain injury. Journal of Pediatrics, 235, 178-183.e1. https://doi.org/10.1016/j.jpeds.2021.04.026
Mikat-Stevens, N. A., Larson, I. A., & Tarini, B. A. (2015). Primary-care providers’ perceived barriers to integration of genetics services: A systematic review of the literature. Genetics in Medicine, 17(3), 169–176. https://doi.org/10.1038/gim.2014.101
Moreno-De-Luca, D., Kavanaugh, B. C., Best, C. R., Sheinkopf, S. J., Phornphutkul, C., & Morrow, E. M. (2020). Clinical genetic testing in autism spectrum disorder in a large community-based population sample. JAMA Psychiatry, 77(9), 979–981. https://doi.org/10.1001/jamapsychiatry.2020.0950
Narcisa, V., Discenza, M., Vaccari, E., Rosen-Sheidley, B., Hardan, A. Y., & Couchon, E. (2013). Parental interest in a genetic risk assessment test for autism spectrum disorders. Clinical Pediatrics, 52(2), 139–146. https://doi.org/10.1177/0009922812466583
Nguyen, E. D., & Menon, S. (2021). For whom the bell tolls: Acute kidney injury and electronic alerts for the pediatric nephrologist. Frontiers in Pediatrics, 9, 628096. https://doi.org/10.3389/fped.2021.628096
Riggs, E. R., Wain, K. E., Riethmaier, D., Smith-Packard, B., Faucett, W. A., Hoppman, N., Thorland, E. C., Patel, V. C., & Miller, D. T. (2014). Chromosomal microarray impacts clinical management. Clinical Genetics, 85(2), 147–153. https://doi.org/10.1111/cge.12107
Rutz, A., Dent, K. M., Botto, L. D., Young, P. C., & Carbone, P. S. (2019). Brief report: Pediatrician perspectives regarding genetic evaluations of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 49(2), 794–808. https://doi.org/10.1007/s10803-018-3738-z
Satya-Murti, S., Cohen, B. H., Michelson, D. (2013). Model coverage policy - chromosomal microarray analysis for intellectual disabilities . American Academy of Neurology, pp. 1–8
Schaefer, G. B., Mendelsohn, N. J., Practice, P., & Committee, G. (2013). Clinical genetics evaluation in identifying the etiology of autism spectrum disorders: 2013 guideline revisions. Genetics in Medicine, 21(10), 32. https://doi.org/10.1038/gim.2013.32
Soda, T., Pereira, S., Small, B. J., Torgerson, L. N., Muñoz, K. A., Austin, J., Storch, E. A., & Lázaro-Muñoz, G. (2021). Child and adolescent psychiatrists’ perceptions of utility and self-rated knowledge of genetic testing predict usage for autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 60(6), 657–660. https://doi.org/10.1016/j.jaac.2021.01.022
Stoll, K., Kubendran, S., & Cohen, S. A. (2018). The past, present and future of service delivery in genetic counseling: Keeping up in the era of precision medicine. American Journal of Medical Genetics Part c, Seminars in Medical Genetics, 178(1), 24–37. https://doi.org/10.1002/AJMG.C.31602
Volkmar, F., Siegel, M., Woodbury-Smith, M., King, B., McCracken, J., & State, M. (2014). Practice parameter for the assessment and treatment of children and adolescents with autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 53(2), 237–257. https://doi.org/10.1016/j.jaac.2013.10.013
Wagner, K. E., McCormick, J. B., Barns, S., Carney, M., Middleton, F. A., & Hicks, S. D. (2020). Parent perspectives towards genetic and epigenetic testing for autism spectrum disorder. Journal of Autism and Developmental Disorders, 50(9), 3114–3125. https://doi.org/10.1007/s10803-019-03990-6
Wofford, S., Noblin, S., Davis, J. M., Farach, L. S., Hashmi, S. S., Mancias, P., & Wagner, V. F. (2019). Genetic testing practices of genetic counselors, geneticists, and pediatric neurologists With regard to childhood-onset neurogenetic conditions. Journal of Child Neurology, 34(4), 177–183. https://doi.org/10.1177/0883073818821036
Xu, L., Mitchell, L. C., Richman, A. R., & Clawson, K. (2016). What do parents think about chromosomal microarray testing? A qualitative report from parents of children with autism spectrum disorders. Autism Research and Treatment, 2016, 1–9. https://doi.org/10.1155/2016/6852539
Zhao, S., Chen, W. J., Dhar, S. U., Eble, T. N., Kwok, O. M., & Chen, L. S. (2019a). Needs assessment in genetic testing education: A survey of parents of children with autism spectrum disorder in the United States. Autism Research, 12(8), 1162–1170. https://doi.org/10.1002/aur.2152
Zhao, S., Chen, W. J., Dhar, S. U., Eble, T. N., Kwok, O. M., & Chen, L. S. (2019b). Genetic testing experiences among parents of children with autism spectrum disorder in the United States. Journal of Autism and Developmental Disorders, 49(12), 4821–4833. https://doi.org/10.1007/s10803-019-04200-z
Funding
This study was funded by a Boston Children’s Hospital Patient Safety and Quality Graduate Medical Education Grant.
Author information
Authors and Affiliations
Contributions
N. J. A. conceived, designed and executed the study, assisted with data analysis, and wrote the manuscript. M. C. assisted in the conception, design and execution of the study, analyzed the data, and collaborated in the writing and editing of the manuscript. S. J. S. supervised the conception, design, and execution of the study, and collaborated in the writing and editing of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This is a survey without the collection of identifiable information. The Boston Children’s Hospital Institution Review Board has confirmed that no ethical approval is required.
Informed Consent
Informed consent has been waived in this study due to lack of use of identifiable information.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abreu, N.J., Chiujdea, M. & Spence, S.J. Barriers to Genetic Testing Faced by Pediatric Subspecialists in Autism Spectrum Disorders. Adv Neurodev Disord 7, 59–65 (2023). https://doi.org/10.1007/s41252-022-00275-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41252-022-00275-5