Abstract
Stigma and discrimination negatively impact the prevention, treatment, and care of HIV. The COVID-19 pandemic increased this complexity and created a cluster of synergistic health contexts, wherein the physiological aspects of HIV and the social and environmental conditions increased the vulnerability in health outcomes for youth living with HIV (YPLHIV) in Kampala, Uganda. We used interpretive phenomenological analysis (IPA) and the syndemics framework to understand the lived experiences of YPLHIV. From December 2020 to May 2021, six qualitative focus groups were held with 31 youth living with HIV to understand the lived experiences of YPLHIV. The guided questions used were audio-recorded, transcribed verbatim, and coded for thematic analysis. Findings highlight the complexity of intersecting stigma of HIV and COVID-19 that have worsened antiretroviral treatment adherence and mental health issues due to lack of access to critical needs such as fears of food insecurity, health-related worries, the fear of perishing due to COVID-19, and human rights concerns related to gender and sexual identity. The study recommends addressing human rights–related concerns in addition to health-related concerns to comprehensively mitigate the syndemics of HIV and COVID-19 for YPLHIV in Uganda.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
In 2020, an estimated 38 million people were living with human immunodeficiency virus (PLHIV) worldwide, among whom 7.3% were children and adolescents between the ages of 0 and 19 (UNICEF, 2020). According to the 2016–2017 Uganda Population-based HIV Impact Assessment Report (UNAIDS, 2017a), Uganda’s HIV infection rate declined from 7.3% in 2011 to 6% in 2016 among adults aged 15–49. Despite the scale-up efforts in HIV treatments in Uganda, the country still has a high prevalence rate among the youths (UNAIDS, 2017a); particularly, female youth have been disproportionately impacted by the epidemic. For instance, Uganda still lags in mother to child transmission elimination rate; two-thirds of newly infected Ugandans are adolescent young girls as they are four times more likely to get HIV compared to boys of the same age group, and only 30% of them utilize HIV testing services (UNAIDS, 2017a; UNICEF, 2020). Marginalized and vulnerable groups in Uganda also face high rates and risks of infection. For instance, in 2016, the prevalence rate of HIV infection among sex workers in Kampala, Uganda’s capital city, was 37% (UNAIDS, 2017a; UNICEF, 2020). Men who have sex with men (MSM) are recognized as one of the high-risk groups for HIV infection. They face stigma and discrimination due to the country’s policy that prescribes life-long imprisonment and possibly the death penalty based on its anti-homosexuality policies (Hladik et al., 2012).
As these troubling statistics exemplify, stigma and discrimination are fundamental structural causes of population health inequalities, including those related to HIV (Andersson et al., 2020; Lowenthal, 2014; Parker, 2012). Stigma profoundly shapes HIV prevention, care, and treatment cascades, especially among vulnerable population groups, including women and girls and other gender minorities such as men who have sex with men (MSM) and transgender populations (Stangl & Sievwright, 2016; UNAIDS, 2007). Among PLHIV, the experience of stigma and discrimination is debilitating and has a marginalizing effect. Specifically, evidence shows that stigma and discrimination are greatly responsible for failures in individuals’ and communities’ access to HIV testing (Parker, 2012; UNAIDS, 2017b), treatment uptake (DeCarlo & Ekstrand, 2016; Katz et al., 2013), and adherence or treatment delays. Worse, PLHIV’s experiences of stigma and discrimination not only socially marginalize them and serve as barriers to treatment but also affect their emotional well-being and constitute a major source of depression, anxiety, increased suicidality, and lower quality of life (Ashaba et al., 2018; Igumbor et al., 2013). Simply put, fighting HIV also requires fighting HIV-related stigma in Uganda and globally.
Goffman (1963) defined stigma as the marking and discrediting of an individual or group based on an actual or perceived attribute (e.g., health condition, self-image, or social rejection), behavior (e.g., disapproval of teen sex), or membership in a group (e.g., HIV-positive individuals). HIV stigma is prejudice or negative attitudes and abuse directed at people living with HIV and AIDS (UNAIDS, 2007). The great majority of PLHIV report experiencing discriminatory and stigmatizing attitudes towards them (UNAIDS, 2007). A host of studies have documented multi-level aspects of HIV-related stigma, from internalized and perceived stigma to secondary and structural layers of stigma (Bennet et al., 2016; Berger et al., 2001; Karamouzian et al., 2017; Lekas et al., 2011; Michalopoulos et al., 2019; Stangl et al., 2019, 2013; Wu et al., 2015). PLHIV can experience these in various combinations or intersections of stigma based on more than one attribute or behavior, including negative self-image (internalized shame) and perceived stigma (i.e., social rejection) due to HIV.
In Uganda, the stigmatization of or prejudice against young people living with HIV (YPLHIV) creates another layer of socio-cultural, political, and structural obstacles, especially as they attempt to access health, educational, and economic needs. These challenges and barriers can be overwhelming when an additional disruption is introduced in the lives of YPLHIV, such as the recent novel coronavirus (SARS-Cov-2 (COVID-19)) pandemic. PLHIV are already at high risk of contracting and dying from COVID-19 infection due to their immunocompromised status (Centers for Disease Control, 2022). HIV infection compromises the immune system of an individual by destroying the immune cells, known as CD4 cells. Discovered in the late 1970s, CD4 cells are white blood cells that fight infections in the human body, and when an individual has a low CD4 count, such as those with HIV infections, it allows opportunistic infections to co-occur, worsening the health (WHO, 2020a). Worse, the pandemic has added challenges to HIV medication adherence and increased psychological stress on this population (Nyoni & Okumu, 2020; Okumu et al., 2021). Such challenges exacerbate the disease burden of HIV measured by financial cost, mortality, morbidity, and other indicators that disproportionately affect young people living with HIV.
In the early days of COVID-19, the Ugandan government enacted country-wide ordinances to mitigate the spread of the disease (Oduor, 2021). These restrictions included suspension of public gatherings, closure of schools and non-essential business, discontinuation of public transportation, and enforcement of a national curfew that exacerbates financial cost, mortality, morbidity, and other indicators that disproportionately affect young people living with HIV. For instance, access to HIV prevention and treatment services in Uganda was impeded considerably, depriving many of their vital needs for these resources. The structural deficiencies that contribute to poor health outcomes for YPLHIV were not factored into the implementation of this policy. For example, many families in Uganda were reportedly rationing food by reducing the number of meals in a day and some reported receiving government support; at the same time, disparities in accessing food assistance were also reported (Acayo, 2020). Lack of access to food could have dire consequences for those who are immunocompromised and need proper nutrition to keep up with their good health (WHO, 2020a). Also, LGBTQIA + groups have historically been persecuted in Uganda due to sexual orientation and gender identity laws; COVID-19 aggravated the situation. Reports from the country highlighted widespread discrimination by the Ugandan Government against LGBTQIA + communities during the pandemic (European Union, 2021). Profiling and persecutions can have cascading mental and physical health implications for those with HIV.
Given these contexts, this study proposes to understand the lived experiences of YPLHIV in Uganda during the COVID-19 pandemic, using a qualitative methodology of interpretive phenomenological analysis (IPA). The following overarching guiding question was used: what are the lived experiences of living with HIV during the COVID-19 pandemic in Uganda?
Methodology
Epistemology is the theory of knowledge that informs phenomenological approach's method, validity, and scope. It is based on the paradigm of postmodernism and subjectivity. It emphasizes the importance of participant experiences and provides a powerful tool for gaining insights into people’s lives. In general, phenomenological approaches use qualitative inquiry in exploring participants’ behaviors and data collection techniques to focus on understanding individuals’ lived experiences (Sutton & Austin, 2015). This requires gathering in-depth information and perceptions through inductive, qualitative methods such as interviews, focus group discussions, participant observations, and representations from the participants’ perspectives. IPA adds idiographic and hermeneutic processes in constructing insightful interpretations of the participants' lived experiences that bring to light the critical issues within the context of those experiences (Goldstein, 2017). It assumes that the fundamental qualities and context of a phenomenon are experienced and interpreted uniquely by individuals. It attempts to uncover these lived experiences and interpretations using a process of in-depth reflective inquiry (Smith, et al., 2009). In doing so, IPA ties in the researcher-participant knowledge and experiences in bringing light to a new phenomenon. It illuminates the experiences of research participants within the context of researchers’ prior knowledge and conceptions.
Reflections
Reflexivity in IPA requires researchers to be mindful of assumptions based on their prior experiences to present the participants’ lived experiences. As such, this study uses several presumed assumptions that underlie the purpose of the study. First, we assumed that YLPHIV are living under the cluster of multiple disease contexts, i.e., the syndemics of HIV, COVID-19, and mental stress due to the onset of the COVID-19 pandemic led the researchers to this inquiry.
Anthropologist Merrill Singer conceptualized the syndemics model during the HIV health crisis in Hertford, CT, to describe the combined epidemics of substance abuse, violence, and HIV/AIDS, collectively known as the SAVA syndemics, which created a disproportionate burden of disease among people of color in the USA (Singer, 2000). Therefore, the syndemics framework recognizes the presence of two or more disease states that adversely interact, negatively affecting the mutual course of each disease trajectory and contributing to vulnerability and social inequities. Other researchers such as Dyer and colleagues (Dyer et al., 2012) have suggested that the lens of syndemic context could be used to address the complex nature of stigma YPLHIV face. Thus, syndemics examine the social, economic, environmental, and political milieu in which a population is immersed. Prior social, behavioral, and medical interventions have substantially improved HIV morbidity in Uganda (Stoneburner et al., 2004). However, very few interventions account for the syndemics’ influence on HIV (Sullivan et al., 2015), especially within the context of the COVID-19 pandemic.
Furthermore, because researchers are the primary instrument in qualitative research, the authors must speak to their personal and professional experiences to disclose any possible biases (Patton, 2002). This requires screening for researchers’ preconceived notions and potential biases and examining the social setting in collecting, analyzing, and representing the data and providing transparency is critical for interpretations (Rettke et al., 2018; Rolfe, 2006; Smith, 1996). Accordingly, out of the five researchers conducting this study, four were involved in various research associated with HIV in the sub-Saharan African countries, including Uganda. Three of the researchers are from the East African region and two of these researchers are from Uganda. One of the researchers has been in a practice setting in Kampala, Uganda’s capital city, providing resources and services to the participants. The same researcher collected the data using focus groups for this study, while others attended the sessions through the password-protected Zoom platform. These prior experiences and connections of the four researchers may create researcher bias towards the meaning-making of the data whereby researchers’ viewpoints may override the participants’ experiences (Smith et al., 2009). To avoid such researcher bias, our data analysis and write up process were triangulated by two other researchers not associated with the region, and one of them is new to the area of study. Another layer of researcher bias was that all researchers were focused on social stigma and health-related outcomes based on the social, economic, and political influencers (Love et al., 2020; Smith et al., 2009) which could influence the presuppositions surrounding stigma-related issues. Finally, some of the participants were receiving their HIV treatment at the data collection site and its sister clinic; this may have influenced their responses to the questions posed, leaning towards social desirability to the setting or researchers.
Ethical Considerations
Our objective for this study was to have an in-depth understanding of the complexity surrounding stigma and discrimination among YPLHIV in Uganda. Youths, ages 18 to 25, living with HIV (YPLHIV) participated in six focus groups with N = 31 participants in Kampala, Uganda. We collaborated with Uganda’s National AIDS Control Program, the Ministry of Health, the Most At-Risk Populations Initiative (MARPI) clinic, and its sister network, Uganda Network of Young People Living with HIV/AIDS (UNYPA) in Kampala. The institutional review board (IRB) for protecting human subjects for primary research involving human subjects at The University of Texas at Arlington over-sighted this study. Locally, Uganda’s Ministry of Health approved the study. The participants were provided with verbal information about the study, its risks and benefits, and the voluntary nature of the study; confidentiality was guaranteed within the risk of being part of a focus group. Although participants were known to have HIV-positive status as per the inclusion criteria protocol, the researchers reminded participants to keep their HIV status and other information (i.e., the mode of infection and behavioral habits) confidential during the focus group sessions to avoid further stigmatization. Participants were also reminded to use their own judgment because anything shared within a focus group may not guarantee complete confidentiality because of the very nature of focus groups and group dynamics. Participants verbally consented and were informed they could leave without penalty at any time if they felt uncomfortable. Finally, participants were informed that they could access free mental health counseling services from the professionals on the premises if needed. All participants received bus fare and snacks as incentives to participate in the study, and they all used pseudonyms during the FGDs.
Sampling
We used purposeful sampling to recruit N = 31 young adults for the study. They included men, women, men having sex with men (MSM), sex workers, and perinatally infected young people, aged 18 to 24, who receive/d services at the MARPI and UNYPA in Uganda. We conducted five focus group discussions (FGDs) and one follow-up FGD. The six focus groups were homogenous in characteristics that they were all HIV positive; however, they differed by gender and behavioral characteristics, e.g., drug use, sexual orientation, and sex-workers. Because of confidentiality issues, we were careful not to profile them based on how they acquired the disease or sexual behavior. All groups had five members except for one with six participants. The participants were screened for eligibility and provided verbal informed consent during the recruitment process. The screening procedures were conducted in person following a prescribed recruitment script. While our study employed purposeful sampling, we used the maximum variation approach (Palinkas et al., 2015; Patton, 2002) to include as much diversity in representation of the HIV-related experiences as possible in our study. Our goal was to reach a thematic saturation in understanding the lived experiences of the stigma associated with HIV.
Data Collection
The data were collected for six months, from December 2020 to May 2021. We used the IPA data collection method to understand how YPLHIV are experiencing the COVID-19 contexts in Uganda. This involved asking questions focused on personal and group meaning and sense-making of lived experiences during the COVID-19 pandemic using few guided questions while allowing a free flow of conversation with the goal of getting rich and detailed data (Smith et al., 2009). We used focus groups since they are inherently social in nature and create a synergistic quality that allows researchers to capture nuances during participant interactions where participants ultimately determine how conversations unfold surrounding topics of interest (Cyr, 2017). The follow-up session provided the opportunity for feedback and member-checking on the research findings with the participants. The goal was to tell the participants’ stories using exemplars from their own narratives and ground the research on their lived experiences instead of using the researchers’ perspectives only (Sutton & Austin, 2015). When conducting focus groups, participants generated more sensitive and personal topics of discussion concerning their health and seeking services. Personal disclosures are often not solicited by interviewers but rather volunteered by participants due to the nature of the peer environment within focus groups (Rettke et al., 2018). We used verbal cues and used guided follow-up questions that explored what it means to be living with HIV during the COVID-19 pandemic in Uganda. We started with questions such as what major challenges have you faced as a young person living with HIV in Uganda? What prejudices or discrimination have you faced due to your HIV status, especially during the COVID-19 pandemic? What other challenges have you faced as a PLHIV during the COVID-19 pandemic? How have you coped with these challenges?
All recordings from the FGDs were translated and transcribed verbatim by a professional translation service in Uganda who spoke Swahili and English fluently. They complied with the ethical standards specified by the ethical board overseer of this study on confidentiality of the transcripts. As mentioned, participants used pseudonyms during FGD recordings to ensure confidentiality, and only voice recordings were used. Since the participants used both languages intermittently, three other researchers from the region who also spoke Swahili and English fluently verified the accuracy of the translation to ensure inter-coder validity.
Data Analysis
Thematic analyses were used to understand HIV stigma experiences and manifestations. These involved six major steps (Smith et al., 2009): (1) reading and re-reading by immersing in the original data and ensuring that the participants are the focus of the analysis; (2) in initial noting, three of the five researchers used Dedoose (version 9.0) (Socio Cultural Research Consultants, 2021) to conduct open and line-by-line coding of transcripts, delineating some of the core descriptive, linguistic, and conceptual comments that focused on the phenomena while de-contextualizing participant’s explicit meaning making of the contexts or content of their lived world; (3) developing emergent themes involved establishing a coding scheme and creating categories chronologically as they emerged; while (4) developing super-ordinate themes involved searching for connections and patterns across emergent themes, charting them, and mapping them in understanding how those themes fit together; (5) these former processes were carried out with each of the cases, and the final step involved (6) synthesizing and looking for patterns across cases and presented in the form of graphic framework.
Each of the researchers independently coded the transcripts separately and then discussed them as a group, in the regular subsequent meetings, to ensure interrater reliability and inter-coder agreements. Dedoose (version 9.0) (SocioCultural Research Consultants, 2021) allows each researcher to blindly code, post individual coding, and rate the codes as agreed upon by all the researchers. Additionally, the researchers triangulated the qualitative data through member checking and debriefing with the participants to understand the concept and context of HIV stigma among YPLHIV during COVID-19 in Uganda. Next, relevant themes were extracted using IPA principles described earlier (Smith, 1996) in categorizing resultant codes into descriptive and analytical themes. This was to ensure confirmability that the research participants shaped the findings and not the researchers’ personal and professional biases, motivations, or interests. The final process included synthesizing the emergent themes and organizing them to develop a broader understanding of what those themes mean in relation to the health outcomes of YPLHIV.
Results
Descriptive
Our focus group participants (mean age = 22.35, range 19–25, standard deviation = 1.94; n = 31) identified themselves as men (n = 16), women (n = 14), and transgender (1) youths. Most reported knowing their HIV status for the last ten years (n = 16/30; 50.1%); n = 15 (48.4%) of the participants reported that they acquired HIV, perinatally. Among the 31 youths, only about half of them (n = 15; 48.4%) said they were unemployed and self-rated their overall health as fair (n = 14/31; 45.2%). Several reported being unemployed or having no income source (n = 13/31; 41.9%). Slightly under two-thirds of the participants reported not adequately adhering to their antiretroviral (ARV) treatment medications (n = 20/31; 64.5%) and considered themselves at low to medium risk for adverse HIV-health conditions. See Table 1 for other sample characteristics.
Major Themes and Excerpts
Based on the thematic analysis, we identified five sub-themes: (a) fear of increased vulnerability to COVID-19; (b) healthcare service–related challenges and discrimination; (c) gender- and identity-related stigma and discrimination; (d) food insecurity; and (e) ARV treatment adherence challenges and barriers and mental health issues.
Fear of Increased Vulnerability to COVID-19
The COVID-19 pandemic has shown the extraordinary resiliency among YPLHIV amidst the challenges they have faced. At the same time, the pandemic-related stigma associated with those with HIV-positive status and the COVID-19 pandemic also exposed the fears, uncertainties, and powerlessness to how the new virus could compromise their lives. Fear of heightened vulnerability to COVID-19 was a source of threat for our participants living with HIV. Our research participants were fearful that COVID-19 and not the HIV may take their life away, “If they told me that I have COVID, I’d first fear [for myself] because I have HIV.” Another participant reported, “That’s why people have been maybe stigmatizing COVID-19 people, even [if people] just suspect so much that…. they think that [if] I get COVID-19, I might not survive [because I have HIV].”
One participant spoke of being highly susceptible to COVID-19:
People are scared that if I get close to someone with COVID-19, I might end up the same route, and its worse for us because we as the [HIV] positive people are part of the vulnerable groups that are highly susceptible to being affected with COVID.
So, the truth is not good but [laughs….] I am so vulnerable. My immune system has impairment, though for me, at the moment, I am undetectable, but the truth is my immune system is impaired. So, I can’t risk to get another virus into myself.
These expressions of vulnerability to death due to impaired immune system are substantial fears of the unknown for our research participants. Lack of knowledge and information around the new viral disease and how the COVID-19 may impact those with HIV generated much misinformation.
Healthcare Service–Related Challenges and Discrimination
Our participants feared the new virus and feared complications and interactions of different antiretroviral (ARV) drugs they must take to keep the HIV load down. The participants understood an enduring physical, mental, and emotional traumas of discrimination and marginalization from their historical experiences and felt that their treatment, if diagnosed with COVID-19, will be different than those of regular persons who may get COVID-19. They expressed that the health care providers must understand how they are treating the coronavirus when dealing with their patients who also have HIV.
Um, I’m also thinking that uh there’ll be different kind of treatment because you know there’s also this issue of drug interactions. I’m thinking if they’re going to give me COVID-19 treatment, they need to first know my ARVs that I’m taking.
Another participant added to this and said,
They [Health Care Workers] also need to know are they going to be okay with the new drugs they’re administering into my body. They all need to be there and working at the same time. Yeah, so it should be a special treatment.
These statements also bring forth the participants’ mistrust in the knowledge of healthcare providers about treatment protocols of COVID-19 for PLHIV.
Providing home delivery of medications and care services is critical for PLHIV. Health care clinics like MARPI have been instrumental for our research participants. For instance, one of the male participants spoke about a healthcare service provider discretely bringing ARV and food to him during the pandemic:
I’ve not disclosed to my family. I’ve only disclosed to a friend who disappointed me, and then I kept it to myself plus my health worker who I tell now everything because also personally, she brought me medicine during COVID-19. She’s the same person also who brought me…food.
However, this statement also reflects on the persistence of community stigma related to HIV-status and the ways healthcare community have failed to comprehensively address stigma in the broader society despite decades of HIV treatment and prevention discovery. Structural and cultural stigma around HIV is still a struggle for our participants, so are affordability of medications. One of the male participants spoke about not being able to afford to go to the health facilities during the pandemic:
Although there are widespread attempts at addressing the COVID-19, it can kill. It doesn't matter if you are positive or negative it treats us the same, but we are facing a challenge during this COVID-19 period, that even up to now some young people living with HIV can’t afford to go to the health facilities for their drugs.
From these anecdotes, it was clear that although the HIV medical providers are critical workforce and provided support for our participants during the pandemic, the stigma and the hidden nature of the HIV status, the inconsistency in medication distribution and uptake due to the medical community’s inability to address structural and cultural stigma, and lack of affordability of HIV treatment were still a challenge for our research participants. The unpredictability of the COVID-19 pandemic, the medical unknowns and fears, and shortages of medicines and resources have created a complex situation for those with HIV in Uganda.
Gender- and Identity-Related Stigma and Discrimination
The stigma of HIV is already interconnected with the negative identifications of being sexually promiscuous and this was being collated with COVID-19 for some of the participants. They expressed that the general assumption is that those who have HIV are also more likely to have COVID-19. One participant who identified self as the LGBTQIA + member expressed such dual stigma in the following manner: “In the quarantine times, we used to have a bus from our facility, so it had [Agency] Staff Bus. Those people used to say, ‘them there have brought COVID-19 to us.’”.
Another participant who acquired HIV from birth described her experiences of witnessing one of her friends, who also has HIV, being excommunicated by the community because of the HIV-positive status. They assumed that the friend was stigmatized as someone who is most likely to bring COVID-19 to the village because of the HIV status.
Here in-- somewhere in [the village], they told her [her friend] not to come to the village again because she was a COVID-19 suspect, but she had turned negative.
HIV has created a multiplier effect on stigma for them along with their identity. Now the pandemic has made them even more vulnerable. Our participants who identified themselves as men having sex with men (MSM) reported, “…it so happens that you’re a MSM, you’re positive, and you also have COVID-19 in Uganda, right now you’re at a very big disadvantage.” Another participant who was summoned by the police added:
The government should at least endeavor that if you’re arrested, you're not embarrassed. I was beaten and totally undressed….I was undressed and totally embarrassed. As an MSM, you do not have a say. You’re a curse.
Yet another participant added:
On that point of being arrested by the police,...you become a center of attraction that everyone wants to use, even the media. Those things are actually real. Even while I was arrested no one wanted to be in the same cell with me thinking I would rape them, so I was in a cell alone.
These were some of the prior experiences of stigma felt by our participants. However, with the onslaught of COVID-19, situation was much worse,
If I’m personally lucky, I know where our services are offered from, I just thank God for that because they’ll do whatever they can in their power to make sure they save my life but there’s a brother out there in Kyanamukaka (used to refer to the very remotest place in Uganda), he contracted COVID-19, he has HIV, and he is an MSM. He’s not aware of where he can access the services that can be of help to him. He doesn’t know which health care workers can offer him the treatment he requires and the care he needs; that one will just die. At least me as 25, I’m lucky I know where to access all the services.
These experiences related by the study participants reflected on fear of losing their lives due to COVID-19 amid dealing with their gender status and human rights concerns, resource scarcity for health services, and other basic needs during the COVID-19 pandemic, along with dealing with the stigma of HIV.
Food Insecurity
Resource scarcity, including access to food and medicine, has been a significant challenge for our research participants. As stated earlier, many families struggled and rationed food during the earlier days of pandemic and subsequently due to many challenges such as loss of work. Daily earners, who rely on sex-work, were struggling to nourish themselves and struggled with HIV medication–related challenges because of the social context or empty stomach. One of the participants spoke of taking medicine discretely:
The other thing was, it–mostly it happened like during lockdowns because lockdown wasn’t so easy, it affected us all and taking the medicine in time, you have to get up first before everyone… when you’ve already eaten [to take the medicine].
Another participant spoke of lack of food:
In the lockdown it was so hard to get food–to get what to eat like because things were not well off. I had to swallow medicine on empty stomach. I had to swallow the medicine because I didn’t want to miss it or pass the time. So, I could swallow the medicine on empty stomach. Imagine I used to take very early in the morning at around 7:00 am, and I get [nothing] to eat between lunch hours.
That period, my friend, it’s not easy; it destabilizes, and you do all sorts of things. People would ask, what’s up with you? You don’t feel yourself and all that. I could just tell them I’m not fine. I’m a little bit dizzy. I’m sick or something. I could not tell–I could not just open to them and all that.
Another male participant who acquired HIV in birth observed that his fellow HIV community were being challenged by food scarcity and how that created barriers to medication adherence:
If I have no food, then at one point, I’ll fail. I’ve experienced it even during this COVID-19 since I work with the young people, they’ve experienced it. For the past ten years, if you go through their files, they’ve never missed a drug for a day but for the past seven months of COVID-19, I’ve questioned them in the past three appointments, why the drug is not balancing. They’re like, ‘We spend two days, no food three days and I’m advised by an uncle, by my dad not to take the drugs because there’s no food.’
This speaks volume about the failure of the national and international health community trying to eradicate HIV on how they overlooked the social and ecological determinants of HIV context during the pandemic. The entirety of the focus was placed on how to address the COVID-19 pandemic, and without addressing food insecurity and their health conditions, it was clear for our research participants that the HIV health community had failed them.
ARV Adherence and Mental Health Issues
Adhering to treatment schedules of the antiretroviral medicines (ARV) to keep the immune system healthy is critical for those with HIV from further worsening their health. Beyond food-related challenges to ARV adherence discussed in the previous section, HIV-related stigma presented a further barrier to adherence among our participants, particularly when COVID-19-related lockdowns prevented participants from discretely taking ARV. Several participants spoke of added challenges related to taking ARV during the COVID-19 pandemic and the associated social lockdowns:
Right now, I live at our home just as I explained to you, but now my dad doesn’t know about it. Even my siblings don’t know about it. It’s just within me alone. I am hiding while swallowing it.
I’m the one who has to pick it. I’m the one supposed to know how my life is standing. I’m the one supposed to know that now I’ve eaten and taken some drinks. I’m supposed to know that now this is water for swallowing medication. Now I have to hide it from them. Someone can come into my room, so I’ve to endeavor to make sure that when they come in, they should not see it.
Another participant expressed psychological issues related to the fear of running out of HIV medicines during the lockdown:
Uh, even [when the] medicine getting finished [during] the lockdown, and I had to spend some good time without medicine, I was so worried and depressed.
Disparities in delivery and access to ARV drugs were of major concern to our research participants. Relevant to this factor, one participant spoke of running out of drugs and delay in medicine access during the pandemic’s social distancing regulations:
For me, COVID-19 has affected me, my drugs–I wasn’t able to go to my facilitaty to get my drugs, and it took almost a week for my facility to bring my drugs to me.
New difficulties accessing HIV medication due to the lockdowns often led to mental health issues as participants feared the results of not being able to access needed medication. One of the participants, who described himself as a sex worker, shared the mental health stress of not being able to access medications during the pandemic and said that he was concerned that he would run out of medicine during the lockdown and “I had to spend like some good time without medicine, I was so worried and depressed.” Clearly, whether participants had access to ARV, COVID-19-related lockdowns created difficult contexts for adhering to needed medication regimens.
Synthesis of the Subthemes
We further synthesized these emergent sub-themes based on our research participants’ lived experience and organized them into super-ordinate themes while maintaining the integrity of the participants’ experiences and contexts. As described earlier in the “Data Analysis” section, developing super-ordinate theme involved searching for connections and patterns across emergent themes, charting them, and mapping them in understanding how those themes fit together. In summary, the five emergent subthemes from the data were (a) fear of increased vulnerability to COVID-19, (b) healthcare service–related challenges and discrimination, (c) food insecurity, (d) gender- and identity-related stigma and discrimination, and (e) ARV adherence and mental health issues. These subthemes clustered around super-ordinate themes: major concerns for our participants and perceived health impacts during the COVID-19 pandemic. The major concerns were related to health-related concerns and human rights concerns, while perceived health impacts had implications to ARV treatment adherence and mental health issues.
Discussion
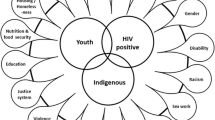
Based on our study results, the COVID-19 pandemic created a cluster of issues that exacerbated the perceived HIV-related health outcomes by disrupting the ARV treatment adherence and increased mental stress creating a context of syndemics that worsened health outcomes for our participants. Our proposed syndemics model (see Fig. 1) captures the multi-level factors contributing to worsening HIV-related health. This syndemic model is unique and important since it also considers human rights as one of the determinants of syndemics of HIV health outcomes. To our knowledge, no other syndemic models prior to this study have highlighted human rights concerns as one of the key factors to consider when addressing HIV- and COVID-19-related health issues.
Participant narratives revealed a wide array of struggles faced by YPLHIV related to stigmatization in their daily lives while dealing with the elevated health risks created by challenges of the COVID-19 pandemic that have created a high risk for health and human conditions. A variety of stigma manifestations affected participants’ sense of belonging and shared identity and increased discrimination and prejudice associated with positive status. Fear, stigma, and scarcity of resources negatively influenced medication adherence, further exasperated by the pandemic-related food insecurity and social distancing requirements. The fear of falling ill has always existed. However, as participants observed, the nature of COVID-19 has brought many concerns, irrespective of coronavirus infection, as our participants have stated. The pervasive impacts of COVID-19 show that almost anything can become a trigger for rumination, and daily actions become laced with risk, especially if one is living with a chronic disease such as HIV.
The participants’ health-related concerns revealed that they had difficulty coping with HIV and the context of COVID-19 and could not trust their healthcare providers, family members, or people from their community to help them navigate those difficulties. They feared that their health would deteriorate, that they could contract the new virus, and that complications may arise while attempting to treat both; they feared being stigmatized all over again for a disease anyone could acquire, and they feared lack in training of health care workers on dealing with the dual pandemic of HIV and COVID-19. Collectively, these fears and logistical issues relating to food and treatment access worsened their ability to adhere to their medication schedules. This worsened their ability to stay on track with their medications. Studies have shown that the proportion of people missing their HIV medications and appointments with healthcare providers increased during the pandemic increasing the susceptibility to higher rates of HIV transmissions (Hochstatter et al., 2021). At the onset of the COVID-19 pandemic, a study on modeling ARV treatment disruption and its effects on HIV predicted mother-to-child transmission by 1.6 times and expected an estimated 296,000 deaths for those with HIV in the first year of the pandemic (Jewell et al., 2020). More recent reports have suggested that the susceptibility to different variants for PLHIV is not significantly different in risk factors than that of the rest of the population; disparities in access to medications can put higher burden of the disease and mental stress among those with HIV (Brown et al., 2021). Moving forward, it is critically important that policymakers and practitioners develop shared understandings of the connections between a lack of HIV medication adherence, COVID-19-related supply issues and lockdown measures, and a discriminatory healthcare system in order to bring urgently needed support to PLHIV.
At the beginning of the pandemic, Uganda already had a limited quantity of HIV-related health supplies. The pandemic further affected the supply chain issues related to HIV/AIDS commodities amid new logistical issues concerning acquiring protective equipment and medical supplies for COVID-19 (WHO, 2020b). In particular, the lack of sufficient test kits was of critical concern at the onset of the pandemic (Adepoju, 2020). Without widespread testing kits availability, many will not know if they need to seek health services or are safe to go to work. Ensuring access to free or affordable screening, testing, and care should be strategized effectively for the most vulnerable and hard-to-reach populations. Although these foci are critical in addressing the syndemics of both HIV and COVID-19, less attention has been paid to different forms of stigma manifestations and their health outcomes for the vulnerable populations such as YPLHIV during the pandemic (Small et al., 2020).
Indeed, human rights issues constituted a major area of concern. Stigma and discrimination based on (suspicions of) COVID-19 infection, on signs and symptoms of COVID-19, and public health–related measures on social distancing, directed towards the HIV-related marginalized groups, prevented our research participants from accessing care and creating a significant problem contributing to social and psychological challenges. They described many socio-economic and political barriers that exist in Uganda where they cannot protect their own health. They also expressed fear of misdirected interpersonal and public stigma and discrimination from their own communities, law enforcements, and healthcare providers and how the presence of fake news/misinformation and lack of infrastructure created mental stress and barriers to ARV treatment adherence. These fears were substantiated by their experiences: participants reported experiencing heightened severity in stigma and abuse during the pandemic, which was even more critical for those identified as LGBTQIA + .
Advocating for the rights of LGBTQIA + community is a critical human rights issue, especially during the pandemic. Many of our participants, who identified themselves as MSM or transgender, reported facing misguided stigma and violence in the community and discrimination within the prison system during the pandemic. For example, COVID-19 lockdown and public health measures were unevenly applied to Uganda’s LGBTQIA + population. The Human Rights Awareness and Promotion Forum (HRAPF) (2020) in Kampala reported that the city’s police raided an LGBTQIA + shelter on the outskirts of Kampala and arrested 14 youths, between the ages of 18 and 25, who were exiled from their own homes due to their sexual orientation. Despite being inside the shelter, they were charged of violating social distancing rules that banned gatherings of more than 10 people in public spaces due to the COVID-19-related restrictions. Such discriminatory and targeted prosecutions were also reported by our study participants. Such stigmatization and persecutions can demoralize and create mental stress and poor physical health manifestations that can be detrimental to our study participants. In light of these findings, it is troubling that despite warnings about human rights concerns for women and LGBTQIA + groups in sub-Saharan Africa, comparatively little research has focused on the impacts of the pandemic on the daily lives of those affected by HIV (Small et al., 2020).
Food and nutrition are not only fundamental human rights, but they are also crucial social determinants of health required to maintain quality of life for PLHIV (Tsai et al., 2011). Access to food must be prioritized as part of the ARV treatment services in Uganda. Several participants in this study expressed a high degree of food insecurity, resulting in difficulties maintaining their health and immunity. This is congruent with the UNAIDS report (UNAIDS, 2020) that COVID-19 response measures have compromised programs related to HIV and undermined human rights while exacerbating inequalities among PLHIV. Although the Uganda COVID-19 Crisis Response and Recovery Support program’s efforts to target the most vulnerable to mitigate COVID-19 pandemic, this program failed to recognize the unique needs of YPLHIV, an immune-compromised population who already struggles with stigma and exile from their own communities, and whose health outcomes hinge on access to food and nutrition.
This failure to recognize the unique needs and health and human rights concerns of YLPHIV had demonstrable consequence during the COVID-19 pandemic: it worsened the adherence to HIV medications, increased mental health concerns, and increased risk for worsening health. All these factors created a context of syndemics for YPLHIV in our study. With the advent of COVID-19, misinformation and conspiracies have only added to the prevailing mistrust with the HIV health service provision system, further magnifying barriers to the prevention and treatment of HIV. In this context, findings from the current study highlight the clear benefits and urgency of using the syndemic framework to better understand the lived experiences of YPLHIV in Uganda during COVID-19. The syndemic context frames the perceived experiences of stigma and challenges that reflect on mental health concerns along with the physical health concerns related to medication and treatment adherences while addressing other social determinants of health and human rights concerns.
Our findings highlight the need to promote evidence-based COVID-19 measures that support the lives of those who have HIV in mitigating the challenges they face daily, such as ensuring consistent and protected HIV treatment services, while maintaining the dignity of YPLHIV. Addressing these intersecting challenges through the multi-level intervention approach (Stangl et al., 2019) that foregrounds the importance of promoting human rights offers a promising strategy for providing comprehensive support to YPLHIV in a syndemic context. Interventions to promote better health and medication adherence should target efforts to reach YPLHIV through community-based awareness. Indeed, engaging affected communities from the beginning in all response measures to HIV and COVID-19 could build trust between service providers and the recipients and ensure program suitability, program effectiveness, and sustainability. Most importantly, it is critical to address the challenges faced by the YPLHIV through the syndemic lens to further develop interventions that put the physiological aspects of HIV, the social community conditions of the COVID-19 pandemic in which it exists, and the human rights violations in which the disease may have proliferated.
Strengths and Limitations of the Study
Limitations to this study include the data and sampling issues. Data were collected from a limited number of health clinics in Uganda. The sample is not representative of the population of YPLHIV with similar contexts and thus findings have limited transferability. Our data are also constituted by participants’ self-reported, anecdotal recollection and is subjected to recall bias, i.e., biased caused by differences in the accuracy or completeness of the participants’ recollections and how they retrieved information regarding events or experiences from the past. Furthermore, despite our attempt to capture what it means to live with HIV-positive health status during the pandemic, our team may not have captured all forms of the mental and physical health impacts of living in a syndemic context.
Despite these limitations, this study provides one of the first snapshots of the vulnerability and struggles experienced by YPLHIV on multiple levels and demonstrates insights into how they dealt with these emergent challenges in the era of COVID-19 pandemic. Uganda was in its second wave of the pandemic at the time of the data collection and, therefore, the interpretations of the participants’ views should be evaluated in this context. Nonetheless, Ugandans, like others around the world, are still experiencing burst of new COVID-19 infections and, currently, only 35% of the people in Uganda have received their first dose of vaccine and only 34% are expected to be fully vaccinated by August 1, 2022 (Institute for Health Metrics & Evaluation-IHME, 2022). Clearly, our study offers insights that will be applicable to Uganda’s social and public health for years to come. Furthermore, the persistence of the secondary impacts of COVID-19–including many social and economic challenges that predated the pandemic–makes this study important and timely in evaluating some of the needs and challenges of the HIV community in Uganda.
Conclusion and Recommendations
Stigmatizing attitudes related to the syndemics of HIV and COVID-19 constrain YPLHIV’s overall health and quality of life. Our study results align with the syndemic framework’s conceptualization of how multiple epidemics (HIV, stigma, and COVID-19) jointly affect the well-being of YPLHIV. Findings from this study can inform social workers and health service providers about stigma reduction strategies to foster enabling HIV adherence environments for YPLHIV during the COVID-19 pandemic. These strategies include leveraging multiple sources of support and culturally responsive, trauma-informed community-based awareness, ensuring food availability, making public service announcements in delineating between HIV- and COVID-19-related symptoms and treatments, improved trainings to healthcare providers, and continuing to address stigma-related issues and human rights concerns.
Because COVID-19 is a relatively new epidemic compared to HIV, obtaining the infrastructure and know-how to handle both diseases can be challenging. Developing evidence-based treatment efficacy approaches is critical in managing these dual-pandemics. As healthcare facilities are not fully equipped with the knowledge to treat HIV clients with COVID-19, developing and sharing evidence-based knowledge on treatments are critical along with mandated trainings for healthcare workers attending to HIV clients. Priority must be given to making any evidence-based and accurate information available to the public, especially to immune-compromised populations. Addressing misinformation about vaccine uptake will require proactive distribution of knowledge to curtail the stigma associated with COVID-19, HIV, and sexual orientation. It is also critical to bring awareness to those with weakened immune system in promoting mask mandates, staying up to date with the durations of COVID-19 vaccine effectiveness and booster shots availabilities, and the general well-being of the affected (CDC, 2022). Furthermore, social workers can play a critical role in advocating for the needs of immune-compromised populations through policymaking and lobbying in public and private sectors.
In light of recent reports of inadequate COVID-19 testing throughout Africa (Adepoju, 2020, 2021) and the gradual lifting of COVID-19 restrictions globally, Uganda’s government must consider protecting those who are immune-compromised by providing continuous support through services such as free testing, PPE, vaccines, medical care, and ARV medications particularly as part of its government-funded COVID-19 Crisis Response and Recovery Support efforts. These efforts should be in place to reach them in urban and rural settings. These efforts must also prioritize providing protection and resources to those involved in sex work or with other vulnerabilities related to sexual orientation and identity who have lost income-generating opportunities during the pandemic. Indeed, as several of this study’s participants noted, their fear of losing their livelihood was as terrifying as the fear of losing a life to COVID-19, particularly to those who identified as sex workers. Additionally, social workers and other health service providers must continue to advocate for HIV prevention strategies by making it easy to access community resources such as HIV testing kits, drug refills including Pre-Exposure Prophylaxis (PrEP) and Post-Exposure Prophylaxis (PEP) drugs, condoms, and Personal Protective Equipment (PPE). More importantly, social workers working in the international context must leverage the local communities’ human and health resources to ensure the continuation of ARV treatments, food access, and the protection of human rights of PLHIV during these challenging times.
Our global pandemic response has been geographically determined, i.e., where we live determine whether we would have access to a COVID-19 vaccine and the types of resources our communities and governments mobilize in response. The disproportionate distribution of resources impeded the ability of countries in the Global South to meet their population’s health needs, causing delays and sometimes deaths. As of December 2021, for example, 60% of the populations in the USA were fully vaccinated and 73% had at least one dose. In developing countries such as Uganda, only 24% of the population were fully vaccinated against the coronavirus (IHME, 2022; Mayo Foundation for Medial Education and Research, 2022). Given these health and resource inequity, our study challenges social workers to advocate for global vaccine equity while maintaining the support and resources necessary for HIV prevention and treatments and address and advocate for the human rights and dignity of vulnerable populations, such as some of our research participants with HIV particularly among vulnerable populations with diverse identities and needs. To this end, we recommend that future research and intervention efforts employ a syndemic framework with human rights at its center to comprehensibly address HIV-related challenges faced by the YPLHIV in Uganda.
Availability of Data and Materials
Will be provided if asked.
Code Availability
Will be provided if asked.
References
Acayo, G. (2020). To address food insecurity in Uganda post COVID-19 the government must act now. International Institute for Environment and Development. Retrieved September 11, 2021, from https://www.iied.org/address-food-insecurity-uganda-post-covid-19-government-must-act-now
Adepoju, P. (2021). As COVID-19 vaccines arrive in Africa, Omicron is reducing supply and increasing demand. Nature medicine. https://doi.org/10.1038/d41591-021-00073-x
Adepoju, P. (2020). Africa’s struggle with inadequate COVID-19 testing. The Lancet Microbe, 1(1), E12. https://doi.org/10.1016/S2666-5247(20)30014-8
Andersson, G. Z., Reinius, M., Eriksson, L. E., et al. (2020). Stigma reduction interventions in people living with HIV to improve health-related quality of life. Lancet HIV, 7(2), e129–e140.
Ashaba, S., Cooper-Vince, C., Maling, S., Rukundo, G. Z., Akena, D., & Tsai, A. C. (2018). Internalized HIV stigma, bullying, major depressive disorder, and high-risk suicidality among HIV-positive adolescents in rural Uganda. Global Mental Health 5, e22. https://doi.org/10.1017/gmh.2018.15
Bennett, D. S., Traub, K., Mace, L., Juarascio, A., & O’Hayer, C. V. (2016). Shame among people living with HIV: A literature review. AIDS Care, 28(1), 87–91.
Berger, B. E., Ferrans, C. E., & Lashley, F. R. (2001). Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health, 24(6), 518–529. https://doi.org/10.1002/nur.10011 PMID: 11746080.
Brown, L. B., Spinelli, M. A., & Gandhi, M. (2021). The interplay between HIV and COVID-19: Summary of the data and response to date. Current Opinion in HIV and AIDS, 16(1), 63–73. https://doi.org/10.1097/COH.0000000000000659
Centers for Disease Control. (2022). COVID-19: COVID-19 vaccines for moderately or severely immunocompromised people. U.S. Department of Health and Human Services, National Institutes of Health. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/immuno.html
Cyr, J. (2017). The unique utility of focus groups for mixed-methods research. PS Polit Sci \& Polit., 50(4), 1038–1042.
DeCarlo, P., & Ekstrand, M. (2016). How does stigma afect HIV prevention and treatment. Cent AIDS Prev Stud Community Engagem Core Prep Oct. https://prevention.ucsf.edu/sites/prevention.ucsf.edu/filesStigmaFSUpdatefnal_20161020.pdf
Dyer, T. P., Shoptaw, S., Guadamuz, T. E., Plankey, M., Kao, U., Ostrow, D., Chmiel, J. S., Herrick, A., & Stall, R. (2012). Application of syndemic theory to Black men who have sex with men in the Multicenter AIDS Cohort Study. J Urban Heal., 89(4), 697–708. https://doi.org/10.1007/s11524-012-9674-x
European Union (EU). (2020). Answer given by High Representative/Vice-President Borrell on behalf of the European Commission ref: E-002939/20. https://www.europarl.europa.eu/doceo/document/E-9-2020-002939-ASW_EN.html#def1
Goffman, E. (1963). Stigma: Notes on the management of spoiled identity (p. 1963). Prentice Hall.
Goldstein, S.E. (2017). Reflexivity in narrative research: Accessing meaning through the participant researcher relationship. Qualitative Psychology, 4(2), 149–164. https://doi.apa.org/doiLanding?doi=10.1037%2Fqup0000035
Health Metrics and Evaluation-IHME. (2022). COVID-19 results briefing. Retrieved from https://www.healthdata.org/sites/default/files/covid_briefs/190_briefing_Uganda.pdf
Hladik, W., Barker, J., Ssenkusu, J. M., Opio, A., Tappero, J. W., Hakim, A., Serwadda, D., & Crane Survey Group. (2012). HIV infection among men who have sex with men in Kampala, Uganda–A respondent driven sampling survey. PLoS ONE, 7(5), e38143. https://doi.org/10.1371/journal.pone.0038143
Hochstatter, K. R., Akhtar, W. Z., Dietz, S., Pe-Romashko, K., Gustafson, D. H., Shah, D. V., Krechel, S., Liebert, C., Miller, R., El-Bassel, N., & Westergaard, R. P. (2021). Potential influences of the COVID-19 pandemic on drug use and HIV care among people living with HIV and substance use disorders: Experience from a pilot mHealth intervention. AIDS and Behavior, 25(2), 354–359. https://doi.org/10.1007/s10461-020-02976-1
Human Rights Awareness and Promotion Forum (HRAPF). (2020). By any means necessary: Defending human rights in Uganda in the time of COVID-19. UNAIDS. https://rstesa.unaids.org/special-initiatives/item/297-by-any-means-necessary-defending-human-rights-in-uganda-in-the-time-of-covid-19
Igumbor, J., Stewart, A., & Holzemer, W. (2013). Comparison of the health-related quality of life, CD4 count and viral load of AIDS patients and people with HIV who have been on treatment for 12 months in rural South Africa. SAHARA-J J Soc Asp HIV/AIDS., 10(1), 25–31. https://doi.org/10.1080/17290376.2013.807070
Jewell, B.L., Mudimu, E., Stover, J., Ten Brink, D., Phillips, A.N., Smith, J.A., Martin-Hughes, R., Teng, Y., Glaubius, R., Mahiane, S.G., Bansi-Matharu, L., Taramusi, I., Chagoma, N., Morrison, M., Doherty, M., Marsh, K., Bershteyn, A., Hallett, T.B., & Kelly, S.L. (2020). HIV modelling consortium. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: Results from multiple mathematical models. Lancet HIV, 7(9), e629-e640. https://doi.org/10.1016/S2352-3018(20)30211-3
Karamouzian, M., Knight, R., Gilbert, M., & Shoveller, J. (2017). A review of measures used to assess HIV-related stigma among young people living with HIV: Missing accounts of sex and gender. Vulnerable Child Youth Stud., 12(3), 241–257. https://doi.org/10.1080/17450128.2016.1274462
Katz, I. T., Ryu, A. E., Onuegbu, A. G., et al. (2013). Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. Journal of the International AIDS Society, 16, 18640. https://doi.org/10.7448/IAS.16.3.18640
Lekas, H. M., Siegel, K., & Leider, J. (2011). Felt and enacted stigma among HIV/HCV-coinfected adults: The impact of stigma layering. Qualitative Health Research, 21(9), 1205–1219. https://doi.org/10.1177/1049732311405684
Love, B., Vetere, A., & Davis, P. (2020). Should interpretive phenomenological analysis (IPA) be used with focus groups? Navigating the bumpy road of “Iterative Loops,” idiographic journeys, and “Phenomenological Bridges”. International Journal of Qualitative Methods, 19. https://doi.org/10.1177/1609406920921600
Lowenthal, E. D., Bakeera-Kitaka, S., Marukutira, T., Chapman, J., Goldrath, K., & Ferrand, R. A. (2014). Perinatally acquired HIV infection in adolescents from sub-Saharan Africa: A review of emerging challenges. The Lancet Infectious Diseases, 14(7), 627–639. https://doi.org/10.1016/S1473-3099(13)70363-3
Mayo Foundation for Medial Education and Research. (2022). U.S. COVID-19 vaccine tracker: See your state’s progress. Retrieved from https://www.mayoclinic.org/coronavirus-covid-19/vaccine-tracker
Michalopoulos, L. M., Meinhart, M., Barton, S. M., Kuhn, J., Mukasa, M. N., Namuwonge, F., Feiring, C., & Ssewamala, F. (2019). Adaptation and validation of the shame questionnaire among Ugandan youth living with HIV. Child Indicators Research, 12(3), 1023–1042. https://doi.org/10.1007/s12187-018-9570-3
Nyoni, T., & Okumu, M. (2020). COVID-19-compliant strategies for supporting treatment adherence among people living with HIV in sub-Saharan Africa. AIDS and Behavior, 24(9), 2473–2476. https://doi.org/10.1007/s10461-020-02888-0
Odour, M. (2021). Uganda imposes another lockdown: What are the restrictions? | Africanews. Published 2021. Accessed September 11, 2021. https://www.africanews.com/2021/06/07/uganda-imposes-another-lockdown-what-are-the-restrictions/
Okumu, M., Nyoni, T., & Byansi, W. (2021). Alleviating psychological distress and promoting mental wellbeing among adolescents living with HIV in sub-Saharan Africa, during and after CoVID-19. Global Public Health, 16 (6):964–973. https://doi.org/10.1080/17441692.2021.1912137
Palinkas, L. A., Horwitz, S. M., Green, C. A., Wisdom, J. P., Duan, N., & Hoagwood, K. (2015). Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health, 42(5), 533–544. https://doi.org/10.1007/s10488-013-0528-y
Parker, R. (2012). Stigma, prejudice and discrimination in global public health. Cadernos De Saúde Pública, 28(1), 164–169. https://doi.org/10.1590/s0102-311x2012000100017
Patton, M.Q. (2002). Qualitative research and evaluation methods. 3rd Sage Publications. Thousand Oaks, CA
Rettke, H., Pretto, M., Spichiger, E., Frei, I. A., & Spirig, R. (2018). Using reflexive thinking to establish rigor in qualitative research. Nursing Research, 67(6), 490–497. https://doi.org/10.1097/NNR.0000000000000307
Rolfe, G. (2006). Validity, trustworthiness, and rigour: Quality and the idea of qualitative research. Journal of Advanced Nursing, 53(3), 304–310. https://doi.org/10.1111/j.1365-2648.2006.03727.x
Singer, M. (2000). A dose of drugs, a touch of violence, a case of AIDS: Conceptualizing the SAVA syndemic. Free Inq Creat Sociol., 28(1), 13–24.
Small, E., Sharma, B. B., & Nikolova, S. P. (2020). COVID-19 and gender in LMICs: Potential lessons from HIV pandemic. AIDS and Behavior, 24(11), 2995–2998. https://doi.org/10.1007/s10461-020-02932-z
Smith, J. A., Flowers, P., & Larkin, M. (2009). Interpretative phenomenological analysis: Theory, method, and research (p. 2009). Sage.
Smith, J. A. (1996). Beyond the divide between cognition and discourse: Using interpretative phenomenological analysis in health psychology. Psychology & Health, 11(2), 261–271. https://doi.org/10.1080/08870449608400256
SocioCultural Research Consultants, LLC. (2021). Dedoose Version 9.0.17, web application for managing, analyzing, and presenting qualitative and mixed method research data. Los Angeles, CA. https://www.dedoose.com/userguide/appendix
Stangl, A. L., Earnshaw, V. A., Logie, C. H., van Brakel, W., Simbayi, L. C., Barre, I., Dovidio, J. F. (2019). The health stigma and discrimination framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Medicine, 17(31), https://doi.org/10.1186/s12916-019-1271-3
Stangl, A., & Sievwright, K. (2016). HIV-related stigma and children. In T. Chenneville (Ed.) A clinical guide to pediatric HIV (297–315). Springer https://link.springer.com/chapter/10.1007/978-3-319-49704-4_12
Stangl, A. L., Lloyd, J. K., Brady, L. M., Holland, C. E., & Baral, S. (2013). A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: How far have we come? Journal of the International AIDS Society, 16, 18734. https://doi.org/10.7448/IAS.16.3.18734
Stoneburner, R. L., & Low-Beer, D. (2004). Population-level HIV declines and behavioral risk avoidance in Uganda. Science, 304(2004), 714–718. https://doi.org/10.1126/science.1093166
Sullivan, K. A., Messer, L. C., & Quinlivan, E. B. (2015). Substance abuse, violence, and HIV/AIDS (SAVA) syndemic effects on viral suppression among HIV positive women of color. AIDS Patient Care and STDs, 29(S1), S42–S48. https://doi.org/10.1089/apc.2014.0278
Sutton, J., & Austin, Z. (2015). Qualitative research: Data collection, analysis, and management. The Canadian Journal of Hospital Pharmacy, 68(3), 226–231. https://doi.org/10.4212/cjhp.v68i3.1456
Tsai, A. C., Bangsberg, D. R., Emenyonu, N., Senkungu, J. K., Martin, J. N., & Weiser, S. D. (2011). The social context of food insecurity among people living with HIV/AIDS in rural Uganda. Social Science and Medicine, 73(12), 1717–1724. https://doi.org/10.1016/j.socscimed.2011.09.026
UNAIDS. (2020). AIDSinfo | UNAIDS. Published 2020. Retrieved September 6, 2021, from https://aidsinfo.unaids.org/
UNAIDS. (2017a). Uganda HIV/AIDS country progress report July 2016-June 2017. https://www.unaids.org/sites/default/files/country/documents/UGA_2018_countryreport.pdf
UNAIDS. (2017b). Agenda for zero discrimination in health-care settings | UNAIDS. Retrieved September 11, 2021, from https://www.unaids.org/en/resources/documents/2017b/2017b-agenda-zero-discrimination-health-care
UNAIDS. (2007). Reducing HIV stigma and discrimination: A critical part of national AIDS programmes: A resource for national stakeholders in the HIV response. Retrieved September 11, 2021, from https://www.unaids.org/sites/default/files/media_asset/jc1521_stigmatisation_en_0.pdf
UNICEF. (2020). Global and Regional Trends. Retrieved from https://data.unicef.org/topic/hivaids/global-regional-trends/
World Health Organization (WHO). (2020a). HIV/AIDS. Retrieved from https://www.who.int/health-topics/hiv-aids#tab=tab_1
World Health Organization (WHO). (2020b). WHO: Access to HIV medicines severely impacted by COVID-19 as AIDS response stalls. Retrieved from https://www.who.int/news/item/06-07-2020b-who-access-to-hiv-medicines-severely-impacted-by-covid-19-as-aids-response-stall
Wu, X., Chen, J., Huang, H., Liu, Z., Li, X., & Wang, H. (2015). Perceived stigma, medical social support and quality of life among people living with HIV/AIDS in Hunan. China. Appl Nurs Res., 28(2), 169–174. https://doi.org/10.1016/j.apnr.2014.09.011
Author information
Authors and Affiliations
Contributions
Sharma, B.B.: conceptualization of the study, data collection, coding, and write up. Small, E.: conceptualization of the study, data collection, coding, and write up. Okumu, M.: conceptualization and write up. Mwima, S.: data collection and write up. Patel, M.: data coding and write up.
Corresponding author
Ethics declarations
Ethics Approval
The institutional review board (IRB) for the protection of human subjects for primary research involving human subjects at the University of Texas at Arlington over-sighted this study (IRB # 2021–0075.1–Protocol was approved). Locally, Uganda’s Ministry of Health approved the study.
Consent to Participate
Participants were read consent.
Consent for Publication
Participants were notified that the study will be published and that their identity will be kept confidential in the process.
Conflict of Interest
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sharma, B.B., Small, E., Okumu, M. et al. Addressing the Syndemics of HIV, Mental Health, and COVID-19 Using the Health and Human Rights Framework among Youth Living with HIV, in Uganda: an Interpretive Phenomenological Study. J. Hum. Rights Soc. Work 7, 285–298 (2022). https://doi.org/10.1007/s41134-022-00221-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41134-022-00221-4