Abstract
Purpose
The efficacy of sleep extension therapy using a remote support system (SET-R) was investigated in university students with increased social jetlag (SJL).
Methods
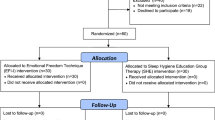
For this two-arm parallel randomized controlled trial, we recruited Japanese university students with SJL ≥ 60 min. The SET-R provided an individualized sleep schedule for gradual sleep extension using email and sleep hygiene education, stimulus control therapy, and progressive muscle relaxation as web content. The control group was sent an email that encouraged them to record their sleep. The duration of the intervention program was two weeks. The primary outcome was the mean change in SJL two weeks later, assessed using the Munich ChronoType Questionnaire (MCTQ). The other outcomes included Pittsburgh Sleep Quality Index, Epworth Sleepiness Scale (ESS), Insomnia Severity Index, Patient Health Questionnaire-9 (PHQ-9), and sleep quiz. A follow-up survey was conducted 6 months after the intervention.
Results
Of 54 students, 26 were assigned to an intervention group and 28 to a control group. The difference in the mean change in SJL between the two groups (n = 26, n = 27) at two weeks was statistically significant (27.7 min, P = 0.048). The scores for the ESS, PHQ-9, and sleep quiz were improved in the intervention group relative to the control group. At the 6-month follow-up point, the difference in the mean change in SJL between the two groups (n = 22, n = 27) was not statistically significant, but scores for the PHQ-9, and sleep quiz remained significant.
Conclusions
This study demonstrated the efficacy of the SET-R among university students with increased SJL.
Trial Registration
The study was registered with the UMIN Clinical Trials Registry (UMIN000042634, 2021/02/01).


Similar content being viewed by others
Change history
12 July 2023
A Correction to this paper has been published: https://doi.org/10.1007/s41105-023-00476-y
Abbreviations
- SJL:
-
Social jetlag
- BMI:
-
Body mass index
- BDNF:
-
Brain-derived neurotrophic factor
- RCT:
-
Randomized controlled trial
- SET-R:
-
Sleep extension therapy using a remote support system
- SKUSH:
-
Student of Kyoto University Sleep Health
- MCTQ:
-
Munich ChronoType Questionnaire
- PSQI:
-
Pittsburgh Sleep Quality Index
- ESS:
-
Epworth Sleepiness Scale
- ISI:
-
Insomnia Severity Index
- PHQ-9:
-
Patient Health Questionnaire-9
- PMR:
-
Progressive muscle relaxation
- MSF:
-
Mid-sleep on free days
- MSW:
-
Midpoint of sleep-in workdays
- TIB:
-
Time in bed
- TST:
-
Total sleep time
- SOL:
-
Sleep onset latency
- SD:
-
Standard deviation
- GLM:
-
Generalized linear models
References
Furihata R, Uchiyama M, Takahashi S, Suzuki M, Konno C, Osaki K, Konno M, Kaneita Y, Ohida T, Akahoshi T, Hashimoto S, Akashiba T. The association between sleep problems and perceived health status: a Japanese nationwide general population survey. Sleep Med. 2012;13(7):831–7.
Roenneberg T, Pilz LK, Zerbini G, Winnebeck EC. Chronotype and social jetlag: a (self-) critical review. Biology (Basel). 2019;8(3):54.
Seton C, Fitzgerald DA. Chronic sleep deprivation in teenagers: practical ways to help. Paediatr Respir Rev. 2021;40:73–9.
Tamura N, Komada Y, Inoue Y, Tanaka H. Social jetlag among Japanese adolescents: association with irritable mood, daytime sleepiness, fatigue, and poor academic performance. Chronobiol Int. 2022;39(3):311–22.
de Zwart BJ, Beulens JWJ, Elders P, Rutters F. Pilot data on the association between social jetlag and obesity-related characteristics in Dutch adolescents over one year. Sleep Med. 2018;47:32–5.
Tan C, Sato K, Shiotani H. The relationship between social jetlag and subjective sleep quality: differences in young and middle-aged workers. Sleep Biol Rhythms. 2023;21(1):7–12.
Qu Y, Li T, Xie Y, Tao S, Yang Y, Zou L, Zhang D, Zhai S, Tao F, Wu X. Association of chronotype, social jetlag, sleep duration and depressive symptoms in Chinese college students. J Affect Disord. 2022;320:735–41.
Haraszti R, Ella K, Gyöngyösi N, Roenneberg T, Káldi K. Social jetlag negatively correlates with academic performance in undergraduates. Chronobiol Int. 2014;31(5):603–12.
Danner F, Phillips B. Adolescent sleep, school start times, and teen motor vehicle crashes. J Clin Sleep Med. 2008;4(6):533–5.
Chan NY, Zhang J, Yu MW, Lam SP, Li SX, Kong AP, Li AM, Wing YK. Impact of a modest delay in school start time in Hong Kong school adolescents. Sleep Med. 2017;30:164–70.
Thacher PV, Onyper SV. Longitudinal outcomes of start time delay on sleep, behavior, and achievement in high school. Sleep. 2016;39(2):271–81.
Dewald-Kaufmann JF, Oort FJ, Meijer AM. The effects of sleep extension and sleep hygiene advice on sleep and depressive symptoms in adolescents: a randomized controlled trial. J Child Psychol Psychiatry. 2014;55(3):273–83.
Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006;23(1–2):497–509.
The Ministry of Health LaWoJ. Sleep Guidelines for Health Promotion 2014. 2014 [updated 2014; cited 2022 May, 01]; Available from: https://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/0000047221.pdf.
Shimamoto T, Furihata R, Nakagami Y, Tateyama Y, Kobayashi D, Kiyohara K, Iwami T. Providing brief personalized therapies for insomnia among workers using a sleep prompt app: randomized controlled trial. J Med Internet Res. 2022;24(7): e36862.
Roenneberg T, Kuehnle T, Juda M, Kantermann T, Allebrandt K, Gordijn M, Merrow M. Epidemiology of the human circadian clock. Sleep Med Rev. 2007;11(6):429–38.
Kitamura S, Hida A, Aritake S, Higuchi S, Enomoto M, Kato M, Vetter C, Roenneberg T, Mishima K. Validity of the Japanese version of the Munich ChronoType Questionnaire. Chronobiol Int. 2014;31(7):845–50.
Doi Y, Minowa M, Uchiyama M, Okawa M, Kim K, Shibui K, Kamei Y. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000;97(2–3):165–72.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–5.
Munezawa T. Development of the Japanese version of the Insomnia Severity Index (ISI-J). Jpn J Psychiatr Treat. 2009;24:219–25.
Muramatsu K, Miyaoka H, Kamijima K, Muramatsu Y, Tanaka Y, Hosaka M, Miwa Y, Fuse K, Yoshimine F, Mashima I, Shimizu N, Ito H, Shimizu E. Performance of the Japanese version of the Patient Health Questionnaire-9 (J-PHQ-9) for depression in primary care. Gen Hosp Psychiatry. 2018;52:64–9.
Carney CE, Buysse DJ, Ancoli-Israel S, Edinger JD, Krystal AD, Lichstein KL, Morin CM. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. 2012;35(2):287–302.
Nakazaki K, Kitamura S, Motomura Y, Hida A, Kamei Y, Miura N, Mishima K. Validity of an algorithm for determining sleep/wake states using a new actigraph. J Physiol Anthropol. 2014;33(1):31.
Zachariae R, Lyby MS, Ritterband LM, O’Toole MS. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia - a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. 2016;30:1–10.
Espie CA, Emsley R, Kyle SD, Gordon C, Drake CL, Siriwardena AN, Cape J, Ong JC, Sheaves B, Foster R, Freeman D, Costa-Font J, Marsden A, Luik AI. Effect of digital cognitive behavioral therapy for insomnia on health, psychological well-being, and sleep-related quality of life: a randomized clinical trial. JAMA Psychiat. 2019;76(1):21–30.
Seyffert M, Lagisetty P, Landgraf J, Chopra V, Pfeiffer PN, Conte ML, Rogers MA. Internet-delivered cognitive behavioral therapy to treat insomnia: a systematic review and meta-Analysis. PLoS ONE. 2016;11(2): e0149139.
Stock AA, Lee S, Nahmod NG, Chang AM. Effects of sleep extension on sleep duration, sleepiness, and blood pressure in college students. Sleep Health. 2020;6(1):32–9.
Schwartz J, Simon RD Jr. Sleep extension improves serving accuracy: a study with college varsity tennis players. Physiol Behav. 2015;151:541–4.
Van Ryswyk E, Weeks R, Bandick L, O’Keefe M, Vakulin A, Catcheside P, Barger L, Potter A, Poulos N, Wallace J, Antic NA. A novel sleep optimisation programme to improve athletes’ well-being and performance. Eur J Sport Sci. 2017;17(2):144–51.
Furihata R, Uchiyama M, Suzuki M, Konno C, Konno M, Takahashi S, Kaneita Y, Ohida T, Akahoshi T, Hashimoto S, Akashiba T. Association of short sleep duration and short time in bed with depression: a Japanese general population survey. Sleep Biol Rhythms. 2015;13(2):136–45.
Reynold AM, Bowles ER, Saxena A, Fayad R, Youngstedt SD. Negative effects of time in bed extension: a pilot study. J Sleep Med Disord. 2014;1(1):1002.
Casement MD, Livingston NR, Allen NB, Forbes EE. Feasibility, acceptability and affective consequences of at-home sleep extension in young women with depressive symptoms: a pilot study. J Sleep Res. 2021;30(2): e13045.
Moseley L, Gradisar M. Evaluation of a school-based intervention for adolescent sleep problems. Sleep. 2009;32(3):334–41.
Acknowledgements
We would like to thank the individuals that participated in this study. We would like to thank Douglas Scientific Editing Services for English-language editing.
Funding
This work was supported by JSPS KAKENHI Grant Number 20K07967, and 22H03412.
Author information
Authors and Affiliations
Contributions
All authors contributed to and have approved the final manuscript. RF, TS, YM, SK, YT, SO, KK, and TI contributed to the study design, data collection, data interpretation, and preparation of the manuscript. KK independently performed the allocation. RF performed the statistical data analyses.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised to update the conflict of interest statement.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Furihata, R., Shimamoto, T., Makino, Y. et al. Efficacy of sleep extension therapy using a remote support system in university students with increased social jetlag: a parallel, single-blind, randomized controlled trial. Sleep Biol. Rhythms 21, 359–368 (2023). https://doi.org/10.1007/s41105-023-00453-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-023-00453-5