Abstract
Objective
Sleep disorders are common during prenatal and postpartum periods which can be associated with physical and psychological maternal and neonatal outcomes. The aim of this study was to determine the psychometric properties of the Persian version of Postpartum Sleep Quality Scale.
Methods
In this study, 280 women who had given birth two to four months prior to the study were selected using cluster sampling in the year 2020. Construct validity of Postpartum Sleep Quality Scale was assessed through exploratory and confirmatory factor analyses. Internal consistency and test–retest were used to determine the reliability of the scale.
Results
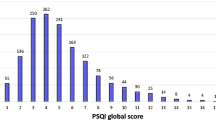
The content validity index of the scale was 0.88 and the content validity ratio was 0.94. In the exploratory factor analysis, the single-factor structure was extracted. The fit indices confirmed the model validity. The Cronbach's alpha coefficient was 0.78 and the intra-class correlation coefficient (95% confidence interval) was 0.97 (0.94 to 0.98). The criterion validity also showed the positive correlation of the scale with the Pittsburgh Sleep Quality Index.
Conclusion
The present study indicates that the Persian version of Postpartum Sleep Quality Scale is a valid and reliable tool for evaluating the postpartum sleep quality in Iranian women.


Similar content being viewed by others
Change history
11 April 2024
In this article the incorrect use of the accent entity has been corrected.
References
Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials. Sleep Med Rev. 2021. https://doi.org/10.1016/j.smrv.2021.101556.
Denison HJ, Jameson KA, Sayer AA, Patel HP, Edwards MH, Arora T, et al. Poor sleep quality and physical performance in older adults. Sleep Health. 2021;7(2):205–11. https://doi.org/10.1016/j.sleh.2020.10.002.
Matsui K, Yoshiike T, Nagao K, Utsumi T, Tsuru A, Otsuki R, et al. Association of subjective quality and quantity of sleep with quality of life among a general population. Int J Environ Res Public Health. 2021;18(23):12835. https://doi.org/10.3390/ijerph182312835.
Lee S, Kim JH, Chung JH. The association between sleep quality and quality of life: a population-based study. Sleep Med. 2021;84:121–6. https://doi.org/10.1016/j.sleep.2021.05.022.
Li S, Fong DYT, Wong JYH, McPherson B, Lau EYY, Ip MSM. The association between nonrestorative sleep and health-related quality of life in Chinese adults: a cross-sectional study. Qual Life Res. 2021;30(9):2521–30. https://doi.org/10.1007/s11136-021-02832-2.
Hunter LP, Rychnovsky JD, Yount SM. A selective review of maternal sleep characteristics in the postpartum period. J Obstet Gynecol Neonatal Nurs. 2008;38:60–8. https://doi.org/10.1111/j.1552-6909.2008.00309.x.
Yang Y, Li W, Ma TJ, Zhang L, Hall BJ, Ungvari GS, et al. Prevalence of poor sleep quality in perinatal and postnatal women: a comprehensive meta-analysis of observational studies. Front Psychiatry. 2020;11:161. https://doi.org/10.3389/fpsyt.2020.00161.
Goyal D, Gay CL, Lee KA. Patterns of sleep disruption and depressive symptoms in new mothers. J Perinat Neonatal Nurs. 2007;21:123–9. https://doi.org/10.1097/01.JPN.0000270629.58746.96.
Gueron-Sela N, Shahar G, Volkovich E, Tikotzky L. Prenatal maternal sleep and trajectories of postpartum depression and anxiety symptoms. J Sleep Res. 2021;30(4): e13258. https://doi.org/10.1111/jsr.13258.
Iranpour S, Kheirabadi GR, Esmaillzadeh A, Heidari-Beni M, Maracy MR. Association between sleep quality and postpartum depression. J Res Med Sci. 2016;7(21):110. https://doi.org/10.4103/1735-1995.193500.
Stremler R, McMurray J, Brennenstuhl S. Self-reported sleep quality and actigraphic measures of sleep in new mothers and the relationship to postpartum depressive symptoms. Behav Sleep Med. 2020;18(3):396–405. https://doi.org/10.1080/15402002.2019.1601629.
Okun ML, Mancuso RA, Hobel CJ, Schetter CD, Coussons-Read M. Poor sleep quality increases symptoms of depression and anxiety in postpartum women. J Behav Med. 2018;41:703–10. https://doi.org/10.1007/s10865-018-9950-7.
Doering JJ, Szabo A, Goyal D, Babler E. Sleep Quality and Quantity in low-income postpartum women. MCN Am J Matern Child Nurs. 2017;42:166–72. https://doi.org/10.1097/NMC.0000000000000323.
Aksu A, Vefikulucay YD. The relationship of postpartum sleep quality and breastfeeding self-efficacy of Turkish mothers. Scand J Caring Sci. 2019;33(4):833–9. https://doi.org/10.1111/scs.12679.
Kalmbach DA, O’Brien LM, Pitts DS, Sagong C, Arnett LK, Harb NC, Cheng P, Drake CL. Mother-to-infant bonding is associated with maternal insomnia, snoring, cognitive arousal, and infant sleep problems and colic. Behav Sleep Med. 2021;28:1–17. https://doi.org/10.1080/15402002.2021.1926249.
Carrega J, Lee SY, Clark P, Cranford J, Lloyd S. Impact of the quality of postpartum sleep and its health determinants on human milk volume. MCN Am J Matern Child Nurs. 2020;45(5):289–95. https://doi.org/10.1097/NMC.0000000000000645.
Sit D, Luther J, Buysse D, Dills JL, Eng H, Okun M, et al. Suicidal ideation in depressed postpartum women: associations with childhood trauma, sleep disturbance and anxiety. J Psychiatr Res. 2015;66:95–104. https://doi.org/10.1016/j.jpsychires.2015.04.021.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. https://doi.org/10.1016/0165-1781(89)90047-4.
Tsai PS, Wang SY, Wang MY, Su CT, Yang TT, Huang CJ, et al. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res. 2005;14:1943–52. https://doi.org/10.1007/s11136-005-4346-x.
Yang CL, Yu CH, Chen CH. Development and validation of the postpartum sleep quality scale. J Nurs Res. 2013;21:148–54. https://doi.org/10.1097/jnr.0b013e3182921f80.
Boz İ, Selvi N. Testing the psychometric properties of the postpartum sleep quality scale in Turkish Women. J Nurs Res. 2018;26:385–92. https://doi.org/10.1097/jnr.0000000000000253.
Polit DF, Beck CT. In: Wolters Kluwer Health, editor. Essentials of nursing research:Appraising evidence for nursing practice, 9 th edition: Philadelphia;2018.
Kalfoss M. Translation and adaption of questionnaires: a nursing challenge. SAGE Open Nurs. 2019;5:1–13. https://doi.org/10.1177/2377960818816810.
Hajizadeh E, Asghari M. Statistical methods and analyses in health and biosciences a research methodological approach. Tehran: Jahade Daneshgahi Publications. 2011; 395:395–410.
Watkins MW. Exploratory factor analysis: a guide to best practice. J Black Psychol. 2018;44(3):219–46. https://doi.org/10.1177/0095798418771807.
Rencher AC, hristensen WF. In: wiley, editor. Methods of Multivariate Analysis: united States; 2012.P. 435–475.
Tinsley HE, Weiss DJ. In: Academic Press, editor. Interrater reliability and agreement. In H. E. A. Tinsley & S. D. Brown (Eds.), Handbook of applied multivariate statistics and mathematical modeling: New York; 2000. P. 95–124.
Chen SL, Chen CH. Effects of lavender tea on fatigue, depression, and maternal-infant attachment in sleep-disturbed postnatal women. Worldviews Evid Nursing. 2015;12:370–9. https://doi.org/10.1111/wvn.12122.
Acknowledgements
The research protocol was approved & Supported by Student Research Committee, Tabriz University of Medical Sciences (Grant Number: 61917).
Funding
The research Supported by Student Research Committee, Tabriz University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
MM, SMAC, MM and RH contributed to the design of the study. MM, RH and MM contributed to the implementation and analysis plan. MM, MA, SMAC, MM and RH has written the first draft of this manuscript and all authors have critically read the text and contributed with inputs and revisions, and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hassanzadeh, R., Asghari Jafarabadi, M., Mohammad-Alizadeh Charandabi, S. et al. Psychometric properties of the Persian version of Postpartum Sleep Quality Scale. Sleep Biol. Rhythms 20, 569–575 (2022). https://doi.org/10.1007/s41105-022-00405-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-022-00405-5