Abstract
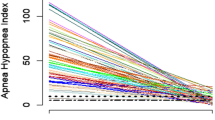
During long-term follow-up of the patients with obstructive sleep apnea syndrome (OSAS) under the positive airway pressure (PAP) therapy, it waits to be explored whether or when routine retitrations are indicated. We prospectively followed up 133 patients for 10 years to define which demographical or polysomnographic factors should be taken into account to determine the need for retitration. Patients were retitrated at 1st, 2nd, 5th, and 10th follow-up years. A change in pressures ≥ 2cmH2O was present in more than half of the patients at 2nd and 5th years. Changes in weight for at least 10 kg showed a significant correlation with the changes in pressures ≥ 2cmH2O (p = 0.023) and ≥ 3cmH2O (p = 0.047) at 2nd year. OSAS-related complaints, nasal or upper airway surgery, or emergence of cardiovascular diseases were not correlated with the changes in pressures. Apnea–hypopnea index (AHI) at diagnostic night was positively correlated with the changes in pressures ≥ 3cmH2O at 1st and 5th years. The percentage of N3 sleep at first titration night showed positive correlation with changes in pressures ≥ 3cmH2O at 2nd and 5th years. The index of periodic leg movements in sleep (PLMS) and PLMS-arousal index at first titration night was positively correlated with any change in pressures at 2nd and 5th years. Our findings showed that vast changes in weight, high AHI at diagnostic night, increased duration of deep NREM sleep and high PLMS and PLMS-arousal indices at first titration night should be noted as important indicators for retitration within the first 5 years of follow-up.

Similar content being viewed by others
References
Spicuzza L, Caruso D, Di Maria G. Obstructive sleep apnoea syndrome and its management. Ther Adv Chronic Dis. 2015;6:273–85.
Grunstein R, Sullivan C. Continuous positive airway pressure for sleep breathing disorders. In: Kryger M, Roth T, Dement W, editors. Principles and Practice of Sleep Medicine, 3ed. Saunders Company: Philadelphia, W.B; 2000. p. 894–912.
Sullivan CE, Issa FG, Berthon Jones M. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981;8225:862–5.
Loredo JS, Ancoli-Israel S, Kim EJ, Lim WJ, Dimsdale JE. Effect of continuous positive airway pressure versus supplemental oxygen on sleep quality in obstructive sleep apnea: a placebo-CPAP-controlled study. Sleep. 2006;29:564–71.
Kohli P, Balachandran JS, Malhotra A. Obstructive sleep apnea and the risk for cardiovascular disease. Curr Atherosc Rep. 2011;13:138–46.
Deshpande S, Joosten S, Turton A, Edwards BA, Landry S, Mansfield DR, Hamilton GS. Oronasal masks require a higher pressure than nasal and nasal Pillow masks for the treatment of obstructive sleep apnea. J Clin Sleep Med. 2016;12:1263–8.
Tanahashi T, Nagano J, Yamaguchi Y, Kubo C, Sudo N. Factors that predict adherence to continuous positive airway pressure treatment in obstructive sleep apnea patients: a prospective study in Japan. Sleep Biol Rhyth. 2012;10:126–35.
Smith I, Lasserson TJ. Pressure modification for improving usage of continuous positive airway pressure machines in adults with obstructive sleep apnea. Cochrane Database Syst Rev. 2009;7:CD003531.
Farre R, Montserrat JM, Rigau J, Trepat X, Pinto P, Navajas D. Response of automatic continuous positive airway pressure devices to different sleep breathing patterns: a bench study. Am J Respir Crit Care Med. 2002;166:469–73.
Marrone O, Insalaco G, Bonsignore MR, Romano S, Salvaggio A, Bonsignore G. Sleep structure correlates of continuous positive airway pressure variations during application of an autotitrating continuous positive airway pressure machine in patients with obstructive sleep apnea syndrome. Chest. 2002;121:759–67.
Callahan CY, Norman RG, Taxin Z, Mooney AM, Rapoport DM, Ayappa I. Multinight recording and analysis of continuous positive airway pressure airflow in the home for titration and management of sleep disordered breathing. Sleep. 2013;36:535–45.
Konermann M, Sanner B, Burmann-Urbanek M. Constancy of CPAP pressures in long-term monitoring of patients with obstructive sleep apnoea. Dtsch Med Wochenschr. 1995;120:125–9.
Netzer NC, Juhász J, Hofmann M, Hohl K, Strohl KP, Küpper TEAH. The need for pressure changes in CPAP therapy 2–3 months after initial treatment A prospective trial in 905 patients with sleep-disordered breathing. Sleep Breath. 2011;15:107–12.
Choi S, Mullins R, Crosby JH, Davies RJ, Stradling JR. Is (re)titration of nasal continuous positive airway pressure for obstructive sleep apnoea necessary? Sleep Med. 2001;2:431–5.
Berry RB, Albertario CL, Harding SM, for the American Academy of Sleep Medicine, et al. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Version 2.5. Darien: American Academy of Sleep Medicine; 2018.
Funding
This study was funded by the local sources of the Department of Neurology, Cerrahpasa Faculty of Medicine, Istanbul University-Cerrahpasa.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Gulcin Benbir Senel declares no conflicts of interest. Pinar Bekdik Sirinocak declares no conflicts of interest. Derya Karadeniz declares no conflicts of interest.
Ethical approval
Our study was conducted in accordance with the statement of Helsinki and it was approved by Local Ethical Committee (with a number of 83045809–604.01.02–150111).
Research involving human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Retitration at 1st year | |||||
|---|---|---|---|---|---|
Changes in pressures (n, number of the patients) | Changes in body weight | ||||
Decrease at least 10 kg | Decrease at least 5 kg | Any change | Increase at least 5 kg | Increase at least 10 kg | |
Decrease at least 3 mbar | 0 | 8 | 0 | 7 | 0 |
Decrease at least 2 mbar | 0 | 4 | 1 | 1 | 0 |
Decrease at least 1 mbar | 3 | 5 | 2 | 5 | 0 |
No change | 0 | 2 | 8 | 0 | 0 |
Increase at least 1 mbar | 0 | 6 | 3 | 20 | 10 |
Increase at least 2 mbar | 0 | 0 | 5 | 5 | 0 |
Increase at least 3 mbar | 0 | 0 | 3 | 1 | 0 |
Retitration at 2nd year | |||||
|---|---|---|---|---|---|
Changes in pressures (n, number of the patients) | Changes in body weight | ||||
Decrease at least 10 kg | Decrease at least 5 kg | Any change | Increase at least 5 kg | Increase at least 10 kg | |
Decrease at least 3 mbar | 4 | 9 | 0 | 5 | 2 |
Decrease at least 2 mbar | 1 | 4 | 0 | 4 | 0 |
Decrease at least 1 mbar | 1 | 0 | 7 | 0 | 3 |
No change | 0 | 1 | 8 | 0 | 0 |
Increase at least 1 mbar | 2 | 6 | 0 | 12 | 6 |
Increase at least 2 mbar | 0 | 1 | 5 | 0 | 4 |
Increase at least 3 mbar | 1 | 0 | 3 | 0 | 5 |
Retitration at 5th year | |||||
|---|---|---|---|---|---|
Changes in pressures (n, number of the patients) | Changes in body weight | ||||
Decrease at least 10 kg | Decrease at least 5 kg | Any change | Increase at least 5 kg | Increase at least 10 kg | |
Decrease at least 3 mbar | 4 | 8 | 1 | 1 | 0 |
Decrease at least 2 mbar | 1 | 5 | 0 | 2 | 0 |
Decrease at least 1 mbar | 4 | 6 | 4 | 3 | 1 |
No change | 0 | 0 | 6 | 1 | 0 |
Increase at least 1 mbar | 1 | 1 | 3 | 1 | 5 |
Increase at least 2 mbar | 0 | 0 | 3 | 2 | 4 |
Increase at least 3 mbar | 0 | 0 | 0 | 4 | 0 |
Retitration at 10th year | |||||
|---|---|---|---|---|---|
Changes in pressures (n, number of the patients) | Changes in body weight | ||||
Decrease at least 10 kg | Decrease at least 5 kg | Any change | Increase at least 5 kg | Increase at least 10 kg | |
Decrease at least 3 mbar | 1 | 5 | 0 | 0 | 0 |
Decrease at least 2 mbar | 3 | 8 | 0 | 1 | 0 |
Decrease at least 1 mbar | 2 | 1 | 5 | 1 | 0 |
No change | 0 | 0 | 4 | 0 | 0 |
Increase at least 1 mbar | 0 | 0 | 9 | 18 | 8 |
Increase at least 2 mbar | 0 | 1 | 1 | 3 | 2 |
Increase at least 3 mbar | 0 | 1 | 1 | 8 | 6 |
Rights and permissions
About this article
Cite this article
Senel, G.B., Sirinocak, P.B. & Karadeniz, D. Determinants of the changes in positive airway pressure for the retitration in patients with obstructive sleep apnea syndrome. Sleep Biol. Rhythms 18, 321–329 (2020). https://doi.org/10.1007/s41105-020-00274-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-020-00274-w