Abstract
Research has established associations between poor mental health and lifestyle risk behaviors among adolescents, yet gaps exist in understanding whether digital health interventions for adolescents targeting these behaviors will improve mental health and wellbeing. This study aimed to evaluate how effective digital health interventions targeting lifestyle risk behaviors are in improving mental health/wellbeing among adolescents (10–24 years old). We also aimed to understand how effects vary by participant and intervention characteristics, and intervention adherence and engagement. Through systematic review with meta-analysis, 5229 records were identified. 17 studies were included representing 9070 participants (15.3 mean age, 1.2 SD). Interventions had small but statistically non-significant positive effects on physical and psychosocial quality of life, depressive symptoms and anxiety at follow-up compared to usual care controls. Digital health delivery methods included text messaging, mobile applications, websites and email, or a combination of these. Intervention adherence, engagement and satisfaction were measured poorly across studies. Despite small changes, potential exists for digital health interventions to improve mental health or wellbeing outcomes among adolescents due to the shared nature of risk and protective factors for mental health and chronic diseases.
Similar content being viewed by others
Introduction
Adolescence is a critical life-stage for development of physical and mental health. Health promoting behaviors need to be established and maintained to ensure good physical and mental health and wellbeing during adolescence and into adulthood (World Health Organization, 2014). However, due to an increase in unhealthy lifestyle behaviors adolescents are at risk of chronic diseases in adulthood such as cardiovascular disease (Barbaresko et al., 2018) and obesity (Farhat et al., 2010). Rates of mental health conditions among adolescents are increasing, with global estimations that 14% of 10–19-year-olds experience a mental health condition or disorder (World Health Organization, 2021) and half of all mental disorders emerge at the age of 14 (Kessler et al., 2007). Emerging research demonstrates that during the first year of the Coronavirus Disease 2019 (COVID-19) pandemic the prevalence of mental health conditions increased to 25% (Racine et al., 2021), yet whether this increased prevalence will remain and the potential long-term implications of this are still unknown. Research has established associations between poor mental health among adolescents and lifestyle risk behaviors including physical inactivity (Sampasa-Kanyinga et al., 2020), sub-optimal diet (O'Neil et al., 2014), sedentary behavior (Rodriguez-Ayllon et al., 2019), poor sleep hygiene, alcohol intake (Lima et al., 2020) and tobacco/e-cigarette smoking (Javed et al., 2022; Lawrence et al., 2022). There is growing evidence that interventions to improve lifestyle risk behaviors are associated with improvements in mental health and wellbeing outcomes (Dale et al., 2014), as well as physical health outcomes, such as obesity (Galani et al., 2007). Yet, most previous research was conducted in adults and only 35% of these studies were conducted in healthy populations (Dale et al., 2014). This study aims to cover existing knowledge gaps in understanding whether interventions targeting lifestyle risk behaviors will improve mental health and wellbeing among adolescents, especially in the context of digital health.
Digital health interventions are increasingly popular for achieving health objectives such as healthy lifestyle management (Chatterjee et al., 2021) and address health system shortcomings (e.g., access issues) (Kang et al., 2018). Healthcare systems need to provide preventive healthcare to adolescents in formats that are acceptable and engaging to them and can be delivered on a large scale. Additionally, given half of all mental disorders are established in adolescence but are undetected for many years (World Health Organization, 2022), digital health interventions may provide an opportunity to reach these young people. Previous systematic reviews have demonstrated that digital health school-based interventions addressing multiple lifestyle risk behaviors were effective for improving physical activity, fruit and vegetable intake and reducing screen time (Champion et al., 2019). Previous systematic reviews have also shown the effectiveness of digital health interventions for diet and physical activity behaviors (Rose et al., 2017) and supporting weight management (Kouvari et al., 2022) among adolescents. Furthermore, there is increasing research into the application of digital health interventions for prevention of mental health conditions among adolescents (Bantjes, 2022; Bergin et al., 2020; Werner-Seidler et al., 2020). However, this is the first study of its kind to specifically focus on the effectiveness of such interventions on improving mental health or wellbeing outcomes.
Current Study
Emerging evidence suggests interventions which aim to improve lifestyle risk behaviors are associated with improvements in mental health and wellbeing outcomes, and digital health interventions provide the opportunity to be delivered at scale to reach adolescents and provide healthy lifestyle management. The current study aimed to investigate the effectiveness of digital health interventions targeting key lifestyle risk behaviors (physical activity, diet, sedentary behavior, sleep, alcohol and/or smoking) on mental health or wellbeing outcomes among adolescents. A second aim is to evaluate how the effects of digital health interventions vary by participant characteristics (e.g., gender, age) intervention characteristics (e.g., delivery method, frequency, duration, type of risk behaviors) and intervention adherence and engagement.
Methods
Protocol and Registration
This systematic review was conducted and reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement guidelines (Page et al., 2021) (Supplementary File 1) and followed the predetermined methods documented in a protocol. The review was prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO; Registration Number: CRD42021247738).
Eligibility Criteria
Studies were included that met the following criteria: (1) randomised controlled trials (RCTs) or cluster randomised controlled trials (cRCTs); (2) participants were adolescents 10–24 years, defined by the Lancet definition of adolescence (Kinghorn et al., 2018), all genders were included who were free from existing mental health diagnosis, not pregnant or post-partum and free of acute illness or other significant chronic disease that requires specific diet and/or physical activity management (e.g. type 1 diabetes mellitus); (3) intervention focused on one or more of the following six lifestyle risk behaviors: dietary behaviors, physical activity, sedentary behaviors, sleep, alcohol and/or tobacco; (4) an outcome of mental health or wellbeing. The list of outcomes was adapted from another systematic review (Melissa Bujtor, 2019) and included both psychological well-being (self-efficacy, self-esteem, self-image, self-concept, quality of life, health related quality of life, positive affect) and psychological ill-being outcomes (stress, anxiety, depressive symptoms, psychological distress, negative affect); (5) digital health intervention of any duration, including mobile technology (mobile phone applications, text messaging), websites, social media, smart watches, activity trackers, email and Personal Digital Assistant use; (6) A comparator group receiving standard or usual care (no intervention); (7) All settings were included including community, home or school-based and health care; (8) published in any language and; (9) studies published after 2005. The cut-off date of 2005 was selected as the current generation of adolescents (‘Generation Z’) appeared in the population after 1995, and the oldest of this generation were 10 years old in 1995.
Information Sources and Search Strategy
Ten major electronic databases (Pre-Medline, Medline, Cochrane, Cochrane Central Register of Controlled Trials, Embase, CINAHL, AMED, Informit, Scopus and Web of Science) were systematically searched on 25th June, 2021 and updated on August 17, 2022. The database searches were developed in conjunction with an academic librarian. Search terms included combinations, truncations and synonyms of the following (1) digital health (telehealth; eHealth, mHealth, mobile applications, text messaging, internet, social media, smartwatch, fitness tracker, personal digital assistant) (2) physical activity, diet, sedentary behavior, sleep, alcohol and/or smoking (3) mental health and wellbeing (self-esteem, self-efficacy, quality of life, anxiety, depressive symptoms, self-image, resilience, stress) and (4) adolescent. Database RCT filters were applied to maximise the results of RCTs and cRCTs and limits were set to only identify papers published from 2005 to current. The full electronic search strategy for each database is available in Supplementary File 2.
Study Selection
One author (RR) carried out all electronic database searches. Search results across databases were merged using Endnote X9 reference management software and duplicates of the same study were removed. Following merging the results in Endnote, they were then uploaded to the systematic review management tool, Covidence (Veritas Health Innovation Ltd, Melbourne, Australia). Following the Cochrane Handbook of Systematic Reviews and the PRISMA Statement for study selection, two researchers (RR and SSJ) independently screened titles and abstracts against the inclusion and exclusion criteria. Any disagreements were discussed and resolved by consensus between two authors (RR and SSJ). Where a decision was unresolved, a third author (SRP) was consulted.
Data Collection Process
For studies meeting the inclusion criteria, information was extracted using a pre-designed electronic data extraction table in Covidence. Two authors independently extracted the data (RR and SSJ) and a third author independently cross-checked a 20% random sample for accuracy (AT). Extracted data included primary outcome data of interest and information on participant characteristics, study characteristics and intervention characteristics. Corresponding authors were contacted for missing, incomplete or unclear data.
Data Synthesis and Analysis
A qualitative synthesis of baseline participant and overall study and intervention characteristics, as well as primary outcome data of interest and data on intervention satisfaction, engagement and adherence was completed. Primary outcome data were grouped by each mental health or wellbeing outcome for a quantitative synthesis. For example, any data from studies that measured change in anxiety between groups was pooled. Where possible, for all study arms, the mean and standard deviation for the outcome of interest was extracted at baseline, post intervention and any follow-ups. Next, data was entered into Review Manager (RevMan; version 5.4, Cochrane, London, UK) software for meta-analyses. If studies included multiple intervention arms, only the most complex intervention was used in the meta-analyses, defined as having the largest number of intervention components. All outcomes of interest were continuous in distribution. Where two or more studies measured the same continuous outcome, they were combined using an inverse variance random effects model, using the standardised mean difference (SMD) and 95% confidence interval (CI). Results of the meta-analyses are presented using forest plots for each outcome. Heterogeneity between studies was assessed using tau2 and the I2 statistic. I2 statistic of > 50% indicate substantial heterogeneity between studies. Significance of heterogeneity was identified using the Cochran’s Q (χ2) test (P < 0.1). Sensitivity analyses were performed excluding the studies with high risk of bias to elucidate whether this caused any difference in the pooled results. For each outcome, small-study effects were evaluated using funnel plots. The published protocol was adhered to in full, however once data was synthesized the protocol was amended to add the sensitivity analysis to understand whether removing studies at high risk of bias improved precision, reduced possible heterogeneity and improved the reliability of the pooled effects.
Risk of Bias Assessment
The Cochrane Collaboration’s tool was used to assess the risk of bias at the individual study level (Sterne et al., 2019). Two Cochrane Risk of Bias tools were used: for randomized trials (RoB 2) and for cRCTs (RoB 2 cRCT). The RoB 2 and RoB 2 cRCT domains for risk of bias assessment included randomization process, deviations from the intended interventions, missing outcome data, measurement of the outcome and selection of the reported result. The judgement within each domain was assessed to produce an overall risk of bias judgement as low risk, some concerns or high risk of bias. Two authors (RR and SJ) independently evaluated each study for risk of bias. Any discrepancies were resolved by a third author (SRP).
Results
Study Selection
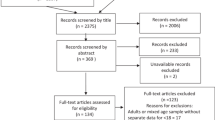
The search found 5362 articles from all electronic database searches. After exclusion of duplicates, 5229 articles were screened by title and abstract and 5089 were excluded. A total of 140 full-text articles were assessed for eligibility and 123 were excluded with reasons listed in Fig. 1. Seventeen full-text articles representing 17 unique studies were included in this review.
Participant and Study Characteristics
Thirteen of the studies were RCTs and four were cRCTs. All were published in English. Seven studies were conducted in the USA, three in the Netherlands, and one each in Hong Kong, Iceland, Spain, Australia, Taiwan, Turkey and Thailand. There was a total of 9070 participants, ranging in age from 10 to 24 years, with a pooled mean age (pooled SD) of 15.3 (1.2). On average, 55.8% of participants were female (range 16–100%). Interestingly, some studies only reported a percentage of how many participants identified as male/female/other and therefore the exact number of participants for each gender is not presented. 12/17 (70.6%) of studies reported ethnicity. Three studies included only participants of one ethnicity (n = 2 Chinese and n = 1 Thai) (Chan et al., 2022; Chen et al., 2018; Likhitweerawong et al., 2021). Five of the studies were targeted at adolescents who had overweight or obesity (Chen et al., 2018; Jones et al., 2008; Köse & Yıldız, 2021; Likhitweerawong et al., 2021; Lopez et al., 2021). For further participant details please refer to Table 1. Length of follow-up ranged from 1 to 25 months. Nine studies targeted more than one lifestyle risk factor (9/17, 52.9%) (Chen et al., 2018; Egilsson et al., 2021; Jones et al., 2008; Köse & Yıldız, 2021; Lopez et al., 2021; Lubans et al., 2012; Richardson et al., 2021; Rodgers et al., 2018; Slootmaker et al., 2010). Three studies targeted smoking only (Cremers et al., 2015; Graham et al., 2021; Guo et al., 2014), two studies targeted sleep only (Chan et al., 2022; De Bruin et al., 2016) and one each targeted only diet (Likhitweerawong et al., 2021), physical activity (Thompson et al., 2016), and alcohol (Vargas-Martínez et al., 2019). Five studies specifically targeted adolescents with overweight or obesity (Chen et al., 2018; Jones et al., 2008; Köse & Yıldız, 2021; Likhitweerawong et al., 2021; Lopez et al., 2021). Attrition rates across studies varied, with four studies having attrition rates above 30% (Cremers et al., 2015; De Bruin et al, 2016; Egilsson et al., 2021; Vargas-Martínez et al., 2019). Full details of participant and study characteristics are available in Table 1 and 2 respectively.
Intervention Characteristics
The method of delivering digital health interventions varied across the 17 studies. Four interventions used a combination of digital health delivery methods including fitness trackers (Chen et al., 2018), websites (Chen et al., 2018; Cremers et al., 2015; Richardson et al., 2021), mobile phone applications (Chen et al., 2018; Lopez et al., 2021; Richardson et al., 2021) and text messaging (Chen et al., 2018; Cremers et al., 2015; Lopez et al., 2021). Five interventions were delivered via text messaging alone (Graham et al., 2021; Guo et al., 2014; Köse & Yıldız, 2021; Lubans et al., 2012; Thompson et al., 2016), four were delivered through a website (De Bruin et al., 2016; Jones et al., 2008; Slootmaker et al., 2010; Vargas-Martínez et al., 2019), three were mobile phone applications (Egilsson et al., 2021; Likhitweerawong et al., 2021; Rodgers et al., 2018) and one was delivered via email (Chan et al., 2022). Intervention duration ranged from 6 weeks (De Bruin et al., 2016; Egilsson et al., 2021; Rodgers et al., 2018) to 12 months (Cremers et al., 2015; Lubans et al., 2010). Eleven of the interventions had the digital component only (Chan et al., 2022; Cremers et al., 2015; De Bruin et al., 2016; Egilsson et al., 2021; Graham et al., 2021; Jones et al., 2008; Likhitweerawong et al., 2021; Richardson et al., 2021; Rodgers et al., 2018; Slootmaker et al., 2010; Vargas-Martínez et al., 2019), whereas six studies were multicomponent and included the digital component alongside other intervention components e.g. classroom curriculum, interactive workshops (Chen et al., 2018; Guo et al., 2014; Köse & Yıldız, 2021; Lopez et al., 2021; Lubans et al., 2012; Thompson et al., 2016). Due to the complexity across interventions in terms of duration, components and exposure, the results are unable to be pooled to adequately demonstrate frequency of intervention exposure. There were several behavior change theories underpinning the interventions including cognitive behavioral therapy (CBT) (Chan et al., 2022; De Bruin et al., 2016; Jones et al., 2008), social cognitive theory (SCT) (Chen et al., 2018; Graham et al., 2021; Lubans et al., 2012), I-Change Model (Cremers et al., 2015; Vargas-Martínez et al., 2019), motivational interviewing (Köse & Yıldız, 2021) and self-determination theory (SDT) (Thompson et al., 2016). Five of 17 studies used co-design with adolescents in intervention development (Egilsson et al., 2021; Graham et al., 2021; Guo et al., 2014; Richardson et al., 2021; Thompson et al., 2016). Full details of the intervention characteristics are available in Table 3.
Mental Health or Wellbeing Outcomes
For two of the included studies, the outcome data of interest was not presented in the manuscript and was unavailable after contacting the corresponding author (Cremers et al., 2015; Thompson et al., 2016). All data used in the meta and sensitivity analyses are available in Supplementary File 3. Forest plots for meta-analyses are available in Fig. 2. Forest plots for sensitivity analysis are available in Fig. 3.
Quality of Life
Four studies (4/17, 23.5%) measured quality of life (QOL) (Chen et al., 2018; Köse & Yıldız, 2021; Likhitweerawong et al., 2021; Vargas-Martínez et al., 2019), with all having sufficient data to perform meta-analyses and used two QOL measures that are validated in adolescent populations: Pediatric Quality of Life Inventory (PedsQL) (Chen et al., 2018; Köse & Yıldız, 2021; Likhitweerawong et al., 2021) and EQ-5D-5L (Vargas-Martínez et al., 2019). One study measured QOL as the primary outcome (Vargas-Martínez et al., 2019). Only one study showed significant effects of the intervention (Köse & Yıldız, 2021), which used text messaging to deliver the intervention over 6-months. Two separate meta-analyses were performed due to one paper reporting QOL for the physical and psychosocial subscales separately and not the total summary score. Overall, meta-analyses indicated that compared with usual care controls, interventions increased physical QOL levels but did not reach a significant level (SMD 0.30, 95% CI − 0.05 to 0.66, P = 0.10). There was significant heterogeneity amongst studies (Tau2 = 0.09, I2 = 70%; P = 0.02). Similarly, interventions increased psychosocial QOL levels but did not reach a significant level compared to control with significant heterogeneity amongst studies (SMD 0.38, 95% CI − 0.08 to 0.83, P = 0.10; Tau2 = 0.16, I2 = 82%, P = 0.001). One study had high RoB (Köse & Yıldız, 2021) and therefore the sensitivity analysis was performed on the remaining three studies. For physical QOL, the sensitivity analyses showed non-significant positive effects of the intervention (SMD 0.05, 05% CI − 0.06 to 0.16; P = 0.37) with no heterogeneity (Tau2 = 0.00, I2 = 0%, P = 0.41). For psychosocial QOL, there was also non-significant positive effects of the intervention compared to control (SMD 0.17, 95% CI − 0.18 to 0.52; P = 0.34) and there was substantial heterogeneity across studies (Tau2 = 0.06, I2 = 59%, P = 0.09).
Self-efficacy
Five (5/17, 29.4%) studies measured self-efficacy (Chen et al., 2018; Cremers et al., 2015; Egilsson et al., 2021; Guo et al., 2014; Slootmaker et al., 2010). Self-efficacy was measured across different domains including physical activity (Chen et al., 2018; Slootmaker et al., 2010), nutrition (Chen et al., 2018), smoking cessation (Cremers et al., 2015; Guo et al., 2014) and general self-efficacy (Egilsson et al., 2021). Due to this variability, meta-analysis was not possible. Three studies used study-specific questionnaires (Cremers et al., 2015; Guo et al., 2014; Slootmaker et al., 2010), one study used the Health Behavior Questionnaire (Chen et al., 2018) and one used the General Self Efficacy Scale (GSE) (Egilsson et al., 2021). Both the Health Behavior Questionnaire and GSE have been validated in adolescent populations previously. No studies measured self-efficacy as a primary outcome. Significant effects of the intervention were seen across three studies measuring physical activity and nutrition self-efficacy (Chen et al., 2018), self-efficacy in smoking cessation (Guo et al., 2014) and self-efficacy in sports (significant among males only) (Slootmaker et al., 2010).
Depressive Symptoms
Six studies measured depressive symptoms (6/17, 35.3%) (Chan et al., 2022; Egilsson et al., 2021; Graham et al., 2021; Jones et al., 2008; Lopez et al., 2021; Richardson et al., 2021), with five having sufficient data for meta-analyses (Chan et al., 2022; Egilsson et al., 2021; Graham et al., 2021; Jones et al., 2008; Lopez et al., 2021). Depressive symptoms were measured using various validated measures including Hospital Anxiety and Depression Scale (HADS) (Chan et al., 2022), Children’s Depression Inventory (CDI) (Egilsson et al., 2021), Patient Health Questionnaire-2 (PHQ-2) (Graham et al., 2021) and Center for Epidemiological Studies Depression Scale for Children (CES-DC) (Jones et al., 2008; Lopez et al., 2021). No studies measured depressive symptoms as the primary outcome. Overall, the results of the meta-analysis revealed that compared with usual care controls, interventions decreased depressive symptoms but did not reach a significant level compared to control (SMD − 0.02, 95% CI − 0.09 to 0.05, P = 0.60) and results were homogenous across studies (Tau2 = 0.00, I2 = 0%, P = 0.60). For depressive symptoms, three studies had a high RoB (Egilsson et al., 2021; Jones et al., 2008; Lopez et al., 2021) and sensitivity analysis was performed on the remaining two studies. Sensitivity analysis showed a non-significant decrease in depressive symptom levels comparing intervention to usual care controls (SMD − 0.05, 95% CI − 0.21 to 0.12; P = 0.59), and results had little heterogeneity (Tau2 = 0.01, I2 = 23%, P = 0.26).
Anxiety
Four studies measured anxiety (4/17, 23.5%) all with sufficient data for meta-analyses (Chan et al., 2022; De Bruin et al., 2016; Egilsson et al., 2021; Graham et al., 2021). Anxiety was measured using the following questionnaires: Hospital Anxiety and Depression Scale (HADS) (Chan et al., 2022), Youth Self Report (De Bruin et al., 2016), Multidimensional Anxiety Scale (MASC) (Egilsson et al., 2021) and Generalized Anxiety Disorder (GAD-2) (Graham et al., 2021). No studies measured anxiety as the primary outcome. Overall, meta-analysis showed that compared with usual care controls, interventions decreased anxiety levels but did not reach a significant level with substantial heterogeneity amongst studies (SMD − 0.13, 95% CI − 0.45 to 0.19, P = 0.42; Tau2 = 0.07, I2 = 69%; P = 0.02). Two of the studies measuring anxiety had a high RoB (De Bruin et al., 2016; Egilsson et al., 2021). The sensitivity analysis on two remaining studies (Chan et al., 2022; Graham et al., 2021), showed a non-significant decrease in anxiety levels comparing intervention to usual care controls in the sensitivity analysis (SMD − 0.04, 95% CI − 0.11 to 0.04) and results were homogenous across trials (Tau2 = 0.00, I2 = 0%, P = 0.61).
Positive and Negative Affect
One study measured both positive and negative affect (Rodgers et al., 2018) and one study measured negative affect only (De Bruin et al., 2016). Although meta-analysis is recommended for 2 or more studies for better precision, significant heterogeneity existed between studies for negative affect and therefore results are summarised in a narrative synthesis. Affect was measured using Youth Self Report (De Bruin et al., 2016) and Positive and Negative Affect Schedule Children (PANAS-C) (Rodgers et al., 2018). No studies measured affect as the primary outcome. Rodgers and colleagues found no interaction effects for positive or negative affect and De Bruin and colleagues found no significant intervention effects on negative affect.
Self-esteem
One study measured self-esteem as a secondary outcome (Lubans et al., 2010, 2012) using the selective scales from Marsh’s Physical Self-Description Questionnaire which is validated in an adolescent population. There were no significant effects of the intervention on self-esteem.
Intervention Satisfaction, Engagement and Adherence
Data on intervention satisfaction, engagement and adherence was poorly reported across studies. Four of 17 (23.5%) studies reported data on intervention satisfaction for participants, with over half of participants finding interventions acceptable (satisfaction 57–91%) (Egilsson et al., 2021; Lubans et al., 2012; Slootmaker et al., 2010; Thompson et al., 2016). Eight of 17 (47.1%) studies reported data on participant engagement or adherence with the intervention, assessed by the amount of the intervention received or accessed by participants which ranged from 22.5% to 83.1% across studies (Chan et al., 2022; Egilsson et al., 2021; Jones et al., 2008; Likhitweerawong et al., 2021; Lopez et al., 2021; Lubans et al., 2012; Slootmaker et al., 2010; Vargas-Martínez et al., 2019). Adherence to the intervention was reported to drop over time in five studies (Chan et al., 2022; Egilsson et al., 2021; Jones et al., 2008; Slootmaker et al., 2010; Vargas-Martínez et al., 2019). One study had a technical issue and therefore could not assess engagement or adherence (Rodgers et al., 2018).
Risk of Bias
Table 4 and 5 and Figs. 4 and 5 summarise the risk of bias assessment for RCTs and cRCTs. Nine of 17 studies (52.9%) had an overall RoB judged as high (Cremers et al., 2015; De Bruin et al., 2016; Egilsson et al., 2021; Guo et al., 2014; Jones et al., 2008; Köse & Yıldız, 2021; Lopez et al., 2021; Lubans et al., 2012; Rodgers et al., 2018). Twelve of 17 studies (76.5%) were judged as some concerns or high in the domain’risk of bias due to deviations from intended intervention’, largely due to not blinding the participants and study personnel to intervention assignment, which is typically not possible in digital health interventions. Three of these studies also did not use appropriate analysis techniques for their data (Köse & Yıldız, 2021; Lopez et al., 2021; Rodgers et al., 2018). Across cRCTs, all were judged as some concerns for their randomization process as no information was provided. Of the four cRCTs, two had baseline differences between groups (Cremers et al., 2015; Vargas-Martínez et al., 2019). No significant publication bias was found from assessing funnel plots (Supplementary File 4).
Discussion
Previous research has shown effectiveness of digital health interventions for improving diet and physical behaviors (Rose et al., 2017), supporting weight management (Kouvari et al., 2022) and prevention of mental health conditions among adolescents (Bantjes, 2022; Bergin et al., 2020; Werner-Seidler et al., 2020), yet no previous research informs us of the effectiveness of digital health interventions which target lifestyle risk behaviors on improving mental health or wellbeing among adolescents. This study found that digital health interventions targeting lifestyle risk behaviors among adolescents were associated with small, but non-significant improvements in quality of life, depressive symptoms and anxiety. After excluding studies at high risk of bias, the sensitivity analyses did not change the effects. This review also showed that digital health interventions were wide-ranging in delivery method, duration and targeted risk behaviors. Co-design was rarely used in intervention development and data on intervention satisfaction, engagement and adherence were poorly reported across included studies, therefore it was unclear whether adolescents found the digital health interventions useful. Thus, mental health and wellbeing are measured outcomes in digital health interventions targeting lifestyle risk behaviors, but further work is needed to develop interventions for adolescents which have more of a holistic view, targeting the complex interplay of physical and mental health and measuring the transfer effect of one to the other.
This study identified several potential reasons for the small effects lifestyle digital health interventions can have on adolescent mental health and wellbeing. Firstly, many of the studies did not measure mental health or wellbeing as a primary outcome and so were possibly not powered to detect changes in these outcomes. Secondly, due to the sparsity of studies found in this review, results were pooled for conceptually related mental health and wellbeing outcomes (Johnston et al., 2022). Despite all being validated in an adolescent population, up to five different patient reported outcome measures were used. Furthermore, the small effect may be due to a floor effect. Incidences of mental health diagnosis for anxiety and depressive symptoms among adolescents range from 20–25% (Racine et al., 2021). As included studies only recruited otherwise healthy adolescents (i.e., no existing mental health diagnosis), participants baseline scores may have been within a healthy range and therefore only minimal improvements were seen. However, studies have shown that there are risks and considerations to both including or excluding people with a mental health diagnosis from digital mental health interventions, with consensus leaning toward ensuring that interventions are delivered to those who are in need (McCall et al., 2021). Previous research has suggested that small effects of digital health interventions targeting the prevention of mental health disorders still hold potential to have broad impact due to the increased number of adolescents able to access the intervention. Moreover, digital health interventions may be more acceptable because of the reduced stigma compared to targeted mental health interventions (Cuijpers, 2022; Montero-Marin et al., 2022). It must also be noted that five of the 17 studies only recruited adolescents who had overweight or obesity (Chen et al., 2018; Jones et al., 2008; Köse & Yıldız, 2021; Likhitweerawong et al., 2021; Lopez et al., 2021). As previous research shows, motivation is an important factor to sustain behavior change to promote weight loss in this population (Sundar et al., 2019; Woo & Park, 2020). However, this review did not choose to exclude these studies as per our protocol and due to the variation in weight categories of adolescents which exists naturally.
This review revealed that digital health interventions for lifestyle risk behaviors that assessed mental health or wellbeing outcomes were diverse, both in their content or focus and in the delivery method. Due to interest in six different lifestyle risk behaviors, the review found that nine of 17 (52.9%) interventions targeted more than one behavior, with physical activity and diet being the most prevalent. Further, only one of the 17 interventions assessed mental health or wellbeing as a primary outcome (Vargas-Martínez et al., 2019). Interventions targeting lifestyle risk behaviors that specifically look to improve mental health or wellbeing may look different in relation to the content and behavior change techniques used, compared to those which focus specifically on improving lifestyle risk behaviors (Hollis et al., 2017; Martin et al., 2013). Previous research has shown that there is a ‘clustering effect’, where adolescents who engage in multiple lifestyle risk behaviors have a higher prevalence of mental health symptoms (Champion et al., 2018; Gardner et al., 2023). Today’s adolescents have reported that issues that affect their ability to maintain a healthy lifestyle are broad, but also interconnected and need to be considered in a multidimensional context (Valanju et al., 2022). Preventive interventions which target both the risk and protective factors for chronic diseases and mental health will also be cost-effective. Hence, there is likely to be considerable benefits when designing future digital health interventions by shifting the focus and aiming to improve lifestyle risk behaviors which are shared risk and protective factors for future development of chronic diseases and mental health (Carbone, 2020; Gardner et al., 2023).
There were vast differences in the digital health delivery method across the 17 included studies, with a combination of five different formats used. The differences in delivery methods for digital health interventions make it unclear which method is most effective. Adolescents are digital natives and use technology daily (Moreno et al., 2022), however, to effectively engage with digital health interventions they must have high digital health literacy skills. Previous research has shown that adolescents often rate their digital health literacy higher than demonstrated (Taba et al., 2022). Furthermore, it is essential that adolescents are engaged and satisfied with these interventions for them to be effective. Out of the 17 studies identified in this review, only five provided data on engagement with the intervention, which ranged broadly. Previous research has aimed to investigate adolescent engagement with digital health interventions across multiple areas (Aschbrenner et al., 2019; Thornton et al., 2022; Wong et al., 2020), however, all suggest that more rigorous RCTs are needed to understand engagement. Three strategies identified to increase adolescent engagement in digital health interventions include personalization, just-in-time adaptation, and co-design with the end user (Partridge & Redfern, 2018). Only five of the 17 studies included in this review discussed the use of co-design of the intervention with adolescents. Engaging with adolescents throughout the entire research process is recognized in the WHO framework for developing and implementing digital health interventions for young people (World Health Organization, 2020). Lack of intervention co-design with adolescents potentially explains the broad range of engagement across studies and lack of significant results. Interestingly, three of the studies which reported co-designing the intervention with adolescents also reported data on satisfaction or retention, which was above 90% for two studies (Richardson et al., 2021; Thompson et al., 2016). Future digital lifestyle interventions should ensure the use of co-design, with meaningful engagement of adolescents at every step, as well as determining the digital health literacy level of participants and tailoring the intervention to suit. This is critical to ensure that adolescent’s knowledge and views are recognised and represented to enhance engagement, satisfaction, and intervention effectiveness.
This study is not without limitations. Firstly, due to the variety of studies and outcomes included, meta-analyses were based on a small number of studies and significant heterogeneity was present for most outcomes except depressive symptoms. Due to pooling of mental health and wellbeing outcomes, the variation in measurements should be considered when interpreting results. Further to this point, we were not able to adequately address our second aim due to variations in the data. We have provided a narrative synthesis of these variables where a quantitative analysis was inappropriate. Second, risk of bias was judged as high or had some concerns for many of the studies, which was mainly due to blinding of participants and outcome assessors. Third, the influence of publication bias must be considered. Grey literature was not searched in this review which may limit the number of included research studies, as negative study outcomes are less-likely to be published in peer-reviewed journals. Finally, very few studies reported a qualitative evaluation of the intervention to understand the barriers and enablers, which would enable a deeper understanding and interpretation of the usefulness of the interventions and allow planning for future research.
Conclusion
No previous research is available on the effectiveness of digital health interventions which target lifestyle risk behaviors on improving mental health or wellbeing among adolescents. This systematic review with meta-analyses revealed that digital health interventions targeting lifestyle risk behaviors amongst adolescents had small but non-significant positive effects on quality of life, anxiety and depressive symptoms at follow-up compared to usual care controls. Intervention satisfaction, engagement and adherence was poorly reported across included studies. Despite the shared nature of risk and protective factors for mental health and chronic diseases, this study highlights the scarcity of evaluation of mental health or wellbeing outcomes in digital health interventions targeting lifestyle risk behaviors among adolescents. It is recommended that future digital lifestyle health interventions consider a more holistic approach, focusing on the interplay between lifestyle risk behaviors and mental health and wellbeing.
Data availability
All data generated or analyzed during this study are included in this published article. Search strategy for this study is available as Supplementary File 2. Data collection tables are available as Tables 1–3 and Supplementary File 3.
References
Aschbrenner, K. A., Naslund, J. A., Tomlinson, E. F., Kinney, A., Pratt, S. I., & Brunette, M. F. (2019). Adolescents’ use of digital technologies and preferences for mobile health coaching in public mental health settings. Frontiers in Public Health. https://doi.org/10.3389/fpubh.2019.00178
Bantjes, J. (2022). Digital solutions to promote adolescent mental health: Opportunities and challenges for research and practice. PLOS Medicine, 19(5), e1004008. https://doi.org/10.1371/journal.pmed.1004008
Barbaresko, J., Rienks, J., & Nöthlings, U. (2018). Lifestyle indices and cardiovascular disease risk: A meta-analysis. American Journal of Preventive Medicine, 55(4), 555–564. https://doi.org/10.1016/j.amepre.2018.04.046
Bergin, A. D., Vallejos, E. P., Davies, E. B., Daley, D., Ford, T., Harold, G., Kidner, M., Long, Y., Merry, S., Moriss, R., Sayal, K., Sonuga-Barke, E., Robinson, J., Torous, J., & Hollis, C. (2020). Preventive digital mental health interventions for children and young people: a review of the design and reporting of research. npj Digital Medicine, 3(1), 133–35. https://doi.org/10.1038/s41746-020-00339-7
Carbone, S. (2020). Evidence review: The primary prevention of mental health conditions. Victorian Health Promotion Foundation.
Champion, K. E., Mather, M., Spring, B., Kay-Lambkin, F., Teesson, M., & Newton, N. C. (2018). Clustering of multiple risk behaviors among a sample of 18-year-old Australians and associations with mental health outcomes: A latent class analysis. Frontiers in Public Health, 6, 135. https://doi.org/10.3389/fpubh.2018.00135
Champion, K. E., Parmenter, B., McGowan, C., Spring, B., Wafford, Q. E., Gardner, L. A., Thornton, L., McBride, N., Carrett, E. L., Teesson, M., & Newton, N. C. (2019). Effectiveness of school-based eHealth interventions to prevent multiple lifestyle risk behaviours among adolescents: A systematic review and meta-analysis. Lancet Digit Health, 1(5), e206–e221. https://doi.org/10.1016/s2589-7500(19)30088-3
Chan, N. Y., Lam, S. P., Zhang, J., Chan, J. W. Y., Yu, M. M. W., Suh, S., Yang, C.-M., Okajima, I., Martin, A., Wing, Y. K., & Li, S. X. (2022). Efficacy of email-delivered versus face-to-face group cognitive behavioral therapy for insomnia in youths: A randomized controlled trial. Journal of Adolescent Health, 70(5), 763–773.
Chatterjee, A., Prinz, A., Gerdes, M., & Martinez, S. (2021). Digital Interventions on healthy lifestyle management: systematic review. Journal of Medical Internet Research, 23(11), e26931. https://doi.org/10.2196/26931
Chen, J. L., Guedes, C. M., & Lung, A. E. (2018). Smartphone-based healthy weight management intervention for Chinese American adolescents: Short-term efficacy and factors associated with decreased weight. Journal of Adolescent Health. Retrieved from https://ezproxy.library.usyd.edu.au/login?url=http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=cctr&AN=CN-01668678
Cremers, H. P., Mercken, L., Candel, M., de Vries, H., & Oenema, A. (2015). A web-based, computer-tailored smoking prevention program to prevent children from starting to smoke after transferring to secondary school: Randomized controlled trial. Journal of Medical Internet Research. https://doi.org/10.2196/jmir.3794
Cuijpers, P. (2022). Universal prevention of depression at schools: Dead end or challenging crossroad? Evidence Based Mental Health, 25(3), 96–98. https://doi.org/10.1136/ebmental-2022-300469
Dale, H., Brassington, L., & King, K. (2014). The impact of healthy lifestyle interventions on mental health and wellbeing: A systematic review. Mental Health Review Journal, 19(1), 1–26. https://doi.org/10.1108/MHRJ-05-2013-0016
De Bruin, E., Bogels, S., Oort, F., & Meijer, A. M. (2016). Improvements of adolescent psychopathology after insomnia treatment: Results from a randomized controlled trial over 1 year. Journal of Sleep Research, 25(Supplement 1), 91.
Egilsson, E., Bjarnason, R., & Njardvik, U. (2021). Usage and weekly attrition in a smartphone-based health behavior intervention for adolescents: Pilot randomized controlled trial. JMIR Formative Research, 5(2), e21432.
Farhat, T., Iannotti, R. J., & Simons-Morton, B. G. (2010). Overweight, obesity, youth, and health-risk behaviors. American Journal of Preventive Medicine, 38(3), 258–267. https://doi.org/10.1016/j.amepre.2009.10.038
Galani, C., & Schneider, H. (2007). Prevention and treatment of obesity with lifestyle interventions: Review and meta-analysis. International Journal of Public Health, 52, 348–359. https://doi.org/10.1007/s00038-007-7015-8
Gardner, L. A., Champion, K. E., Chapman, C., Newton, N. C., Slade, T., Smout, S., Teesson, M., & Sunderland, M. (2023). Multiple lifestyle risk behaviours and hierarchical dimensions of psychopathology in 6640 Australian adolescents. Australian & New Zealand Journal of Psychiatry. https://doi.org/10.1177/00048674221080406
Graham, A. L., Amato, M. S., Cha, S., Jacobs, M. A., Bottcher, M. M., & Papandonatos, G. D. (2021). Effectiveness of a vaping cessation text message program among young adult e-cigarette users a randomized clinical trial. JAMA Internal Medicine. https://doi.org/10.1001/jamainternmed.2021.1793
Guo, J. L., Liao, J. Y., Chang, L. C., Wu, H. L., & Huang, C. M. (2014). The effectiveness of an integrated multicomponent program for adolescent smoking cessation in Taiwan. Addictive Behaviors, 39(10), 1491–1499. https://doi.org/10.1016/j.addbeh.2014.05.009
Hollis, C., Falconer, C. J., Martin, J. L., Whittington, C., Stockton, S., Glazebrook, C., & Davies, E. B. (2017). Annual research review: Digital health interventions for children and young people with mental health problems—a systematic and meta-review. Journal of Child Psychology and Psychiatry, 58(4), 474–503. https://doi.org/10.1111/jcpp.12663
Javed, S., Usmani, S., Sarfraz, Z., Sarfraz, A., Hanif, A., Firoz, A., Baig, R., Sharath, M., Walia, N., Chérrez-Ojeda, I., & Ahmed, S. (2022). A scoping review of vaping, e-cigarettes and mental health impact: Depression and suicidality. Journal of Community Hospital Internal Medicine Perspectives, 12(3), 33–39. https://doi.org/10.55729/2000-9666.1053
Johnston, B. C., Patrick, D. L., Devji, T., Maxwell, L. J., Bingham III, C. O., Beaton, D., Boers, M., Briel, M., Busse, J. W., Carrasco-Labra, A., Christensen, R., da Costa, B. R., El Dib, R., Lyddiatt. A., Ostelo, R. W., Shea, B., Singh, J., Terwee, C. B., Williamson, P. R., …, Guyatt, G. H. (2022). Patient-reported outcomes. In J. P. T. Higgins, J. Chandler, M. Cumpston, T. Li, M. J. Page, & V. A. Welch (Eds.), Cochrane handbook for systematic reviews of interventions. Retrieved from www.training.cochrane.org/handbook
Jones, M., Luce, K. H., Osborne, M. I., Taylor, K., Cunning, D., Doyle, A. C., Wilfley, D. E., & Taylor, C. B. (2008). Randomized, controlled trial of an Internet-facilitated intervention for reducing binge eating and overweight in adolescents. Pediatrics, 121(3), 453–462. https://doi.org/10.1542/peds.2007-1173
Kang, M. R. F., Sanci, L., Steinbeck, K., Jan, S., Hawke, C., Luscombe, G., Kong, M., & Usherwood, T. (2018). Access 3: Young people and the health system in the digital age—final research report. Retrieved from https://www.health.nsw.gov.au/kidsfamilies/youth/Pages/access-study.aspx
Kessler, R. C., Angermeyer, M., Anthony, J. C., De Graaf, R., Demyttenaere, K., Gasquet, I., Girolamo, G. D., Gluzman, S., Gureje O., Haro J. M., Kawakami, N., Karam, A., Levinson, D., Mora, M. E. M., Browne, M. A. O., Posada-Villa, J., Stein, D. J., Tsang, C. H. A., … Ustün, T. B. (2007). Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry, 6(3), 168–176.
Kinghorn, A., Shanaube, K., Toska, E., Cluver, L., & Bekker, L.-G. (2018). Defining adolescence: Priorities from a global health perspective. The Lancet Child & Adolescent Health, 2(5), e10. https://doi.org/10.1016/S2352-4642(18)30096-8
Köse, S., & Yıldız, S. (2021). Motivational support programme to enhance health and well-being and promote weight loss in overweight and obese adolescents: A randomized controlled trial in Turkey. International Journal of Nursing Practice, 27(1), 1–10. https://doi.org/10.1111/ijn.12878
Kouvari, M., Karipidou, M., Tsiampalis, T., Mamalaki, E., Poulimeneas, D., Bathrellou, E., Panagiotakos, D., & Yannakoulia, M. (2022). Digital health interventions for weight management in children and adolescents: Systematic review and meta-analysis. J Med Internet Res, 24(2), e30675. https://doi.org/10.2196/30675
Lawrence, D., Johnson, S. E., Mitrou, F., Lawn, S., & Sawyer, M. (2022). Tobacco smoking and mental disorders in Australian adolescents. Australian & New Zealand Journal of Psychiatry, 56(2), 164–177. https://doi.org/10.1177/00048674211009617
Likhitweerawong, N., Boonchooduang, N., Kittisakmontri, K., Chonchaiya, W., & Louthrenoo, O. (2021). Effectiveness of mobile application on changing weight, healthy eating habits, and quality of life in children and adolescents with obesity: A randomized controlled trial. BMC Pediatrics, 21(1), 499.
Lima, F., Sims, S., & O’Donnell, M. (2020). Harmful drinking is associated with mental health conditions and other risk behaviours in Australian young people. Australian and New Zealand Journal of Public Health, 44(3), 201–207. https://doi.org/10.1111/1753-6405.12978
Lopez, K. E., Salvy, S.-J., Fink, C., Werner, J., Wee, C. P., Hegedus, E., Gonzalez, J., Fox, D. S., & Vidmar, A. P. (2021). Executive functioning, depressive symptoms, and intervention engagement in a sample of adolescents enrolled in a weight management program. Childhood Obesity, 17(4), 281–290. https://doi.org/10.1089/chi.2020.0334
Lubans, D. R., Morgan, P. J., Callister, R., Collins, C. E., & Plotnikoff, R. C. (2010). Exploring the mechanisms of physical activity and dietary behavior change in the Program X intervention for adolescents. Journal of Adolescent Health, 47(1), 83–91. https://doi.org/10.1016/j.jadohealth.2009.12.015
Lubans, D. R., Morgan, P. J., Okely, A. D., Dewar, D., Collins, C. E., Batterham, M., Callister, R., & Plotnikoff, R. C. (2012). Preventing obesity among adolescent girls. Archives of Pediatrics & Adolescent Medicine, 166(9), 821–827. https://doi.org/10.1001/archpediatrics.2012.41
Martin, J., Chater, A., & Lorencatto, F. (2013). Effective behaviour change techniques in the prevention and management of childhood obesity. International Journal of Obesity, 37(10), 1287–1294. https://doi.org/10.1038/ijo.2013.107
McCall, H. C., Hadjistavropoulos, H. D., & Loutzenhiser, L. (2021). Reconsidering the ethics of exclusion criteria in research on digital mental health interventions. Ethics & Behavior, 31(3), 171–180. https://doi.org/10.1080/10508422.2019.1684295
Melissa Bujtor, S. T. (2019). Associations between combined modifiable lifestyle behaviours and mental health in children and adolescents: a systematic review. Retrieved from https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=112748
Montero-Marin, J., Allwood, M., Ball, S., Crane, C., De Wilde, K., Hinze, V., Jones, B., Lord, L., Nuthall, E., Raja, A., Taylor, L., Tudor, K., Blakemore, S.-J., Byford, S., Dalgleish, T., Ford, T., Greenberg, M. T., Ukoumunne, O. C., Williams, J. M. G., & Kuyken, W. (2022). School-based mindfulness training in early adolescence: What works, for whom and how in the MYRIAD trial? Evidence Based Mental Health, 25(3), 117–124. https://doi.org/10.1136/ebmental-2022-300439
Moreno, M. A., Binger, K., Zhao, Q., Eickhoff, J., Minich, M., & Uhls, Y. T. (2022). Digital technology and media use by adolescents: Latent class analysis. JMIR Pediatrics and Parenting, 5(2), e35540. https://doi.org/10.2196/35540
O’Neil, A., Quirk, S. E., Housden, S., Brennan, S. L., Williams, L. J., Pasco, J. A., Berk, M., & Jacka, F. N. (2014). Relationship between diet and mental health in children and adolescents: A systematic review. American Journal of Public Health, 104(10), e31-42. https://doi.org/10.2105/ajph.2014.302110
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ, 372, n71. https://doi.org/10.1136/bmj.n71
Partridge, S. R., & Redfern, J. (2018). Strategies to engage adolescents in digital health interventions for obesity prevention and management. Healthcare (Basel). https://doi.org/10.3390/healthcare6030070
Racine, N., McArthur, B. A., Cooke, J. E., Eirich, R., Zhu, J., & Madigan, S. (2021). Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis. JAMA Pediatrics, 175(11), 1142–1150. https://doi.org/10.1001/jamapediatrics.2021.2482
Richardson, L., Parker, E. O., Zhou, C., Kientz, J., Ozer, E., & McCarty, C. (2021). Electronic health risk behavior screening with integrated feedback among adolescents in primary care: Randomized controlled trial. Journal of Medical Internet Research, 23(3), e24135. https://doi.org/10.2196/24135
Rodgers, R. F., Donovan, E., Cousineau, T., Yates, K., McGowan, K., Cook, E., Lowy, A. S., & Franko, D. L. (2018). BodiMojo: Efficacy of a mobile-based intervention in improving body image and self-compassion among adolescents. Journal of Youth & Adolescence, 47(7), 1363–1372. https://doi.org/10.1007/s10964-017-0804-3
Rodriguez-Ayllon, M., Cadenas-Sánchez, C., Estévez-López, F., Muñoz, N. E., Mora-Gonzalez, J., Migueles, J. H., Molina-García, P., Henriksson, H., Mena-Molina, A., Martínez-Vizcaíno, V., Catena, A., Löf, M., Erickson, K. I., Lubans, D. R., Ortega, F. B., & Esteban-Cornejo, I. (2019). Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: A systematic review and meta-analysis. Sports Medicine (Auckland, N. Z.), 49(9), 1383–1410. https://doi.org/10.1007/s40279-019-01099-5
Rose, T., Barker, M., Maria Jacob, C., Morrison, L., Lawrence, W., Strömmer, S., Vogel, C., Woods-Townsend, K., Farrell, D., Inskip, H., & Baird, J. (2017). A systematic review of digital interventions for improving the diet and physical activity behaviors of adolescents. Journal of Adolescent Health, 61(6), 669–677. https://doi.org/10.1016/j.jadohealth.2017.05.024
Sampasa-Kanyinga, H., Colman, I., Goldfield, G. S., Janssen, I., Wang, J., Podinic, I., Tremblay, M. S., Saunders, T. J., Sampson, M., & Chaput, J.-P. (2020). Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: A systematic review. International Journal of Behavioral Nutrition and Physical Activity, 17(1), 72. https://doi.org/10.1186/s12966-020-00976-x
Slootmaker, S. M., Chinapaw, M. J., Seidell, J. C., van Mechelen, W., & Schuit, A. J. (2010). Accelerometers and Internet for physical activity promotion in youth? Feasibility and effectiveness of a minimal intervention. Preventive Medicine, 51(1), 31–36.
Sterne, J. A. C., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H-Y., Corbett, M. S., Eldridge, S. M., Emberson, J. R., Hernán, M. A., Hopewell, S., Hróbjartsson, A., Junqueria, D. R., Jüni, P., Kirkham, J. J., Lasserson, T., Li, T., … Higgins, J. P. T. (2019). RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ, 366, 14898. https://doi.org/10.1136/bmj.l4898
Sundar, T. K. B., Løndal, K., Riiser, K., Lagerløv, P., Glavin, K., & Helseth, S. (2019). Adolescents with overweight or obesity: A qualitative study of participation in an internet-based program to increase physical activity. SAGE Open Nursing, 5, 2377960819884786. https://doi.org/10.1177/2377960819884786
Taba, M., Allen, T. B., Caldwell, P. H. Y., Skinner, S. R., Kang, M., McCaffery, K., & Scott, K. M. (2022). Adolescents’ self-efficacy and digital health literacy: A cross-sectional mixed methods study. BMC Public Health, 22(1), 1223. https://doi.org/10.1186/s12889-022-13599-7
Thompson, D., Cantu, D., Ramirez, B., Cullen, K. W., Baranowski, T., Mendoza, J., Anderson, B., Jago, R., Rodgers, W., & Liu, Y. (2016). Texting to increase adolescent physical activity: Feasibility assessment. American Journal of Health Behavior, 40(4), 472–483. https://doi.org/10.5993/ajhb.40.4.9
Thornton, L., Brown, H. M., Osman, B., Stewart, C., Whife, J., Champion, K. E., Gardner, L. A., McBride, N., Allsop, S., Spring, B., & Teesson, M. (2022). Factors associated with adolescents’ engagement with a Healthy Lifestyles app. Procedia Computer Science, 206, 56–67. https://doi.org/10.1016/j.procs.2022.09.085
Valanju, R., Barani, M., Mautner, D., Al Hadaya, I., Cross, A., Gunawardana, M., Lambie, A., McMahon, E., Narula, A., Ren, B., Rose, D., Sharda, A., Sinnett, A., Tanvir, A., Tran, H., Yan, F., Mandoh, M., Cheng, H. L., Mihrshahi, S., … Partridge, S. R. (2022). Youth perspective on chronic disease prevention. The Lancet Child & Adolescent Health, 6(7), 456–458. https://doi.org/10.1016/S2352-4642(22)00131-6
Vargas-Martínez, A. M., Trapero-Bertran, M., Lima-Serrano, M., Anokye, N., Pokhrel, S., & Mora, T. (2019). Measuring the effects on quality of life and alcohol consumption of a program to reduce binge drinking in Spanish adolescents. Drug and Alcohol Dependence. https://doi.org/10.1016/j.drugalcdep.2019.107597
Werner-Seidler, A., Huckvale, K., Larsen, M. E., Calear, A. L., Maston, K., Johnston, L., Torok, M., O-Dea, B., Batterham, P. J., Schweizer, S., Skinner, S. R., Steinbeck, K., Ratcliffe, J., Oei, J-L., Patton, G., Wong, I., Beames, J., Wong, Q. J. J., … Christensen, H. (2020). A trial protocol for the effectiveness of digital interventions for preventing depression in adolescents: The Future Proofing Study. Trials, 21(1), 2. https://doi.org/10.1186/s13063-019-3901-7
Wong, C. A., Madanay, F., Ozer, E. M., Harris, S. K., Moore, M., Master, S. O., Moreno, M., & Weitzman, E. R. (2020). Digital health technology to enhance adolescent and young adult clinical preventive services: Affordances and challenges. Journal of Adolescent Health, 67(2), S24–S33. https://doi.org/10.1016/j.jadohealth.2019.10.018
Woo, S., & Park, K. H. (2020). Motivating children and adolescents in obesity treatment. Journal of Obesity & Metabolic Syndrome, 29(4), 260–269. https://doi.org/10.7570/jomes20026
World Health Organization. (2014). Health for the World’s Adolescents: A second chance in the second decade. World Health Organization. Retrieved from https://apps.who.int/adolescent/second-decade/
World Health Organization. (2020). Youth-centred digital health interventions: a framework for planning, developing and implementing solutions with and for young people. World Health Organization. Retrieved from https://www.who.int/publications/i/item/9789240011717
World Health Organization. (2021). Adolescent mental health. World Health Organization. Retrieved from https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health#:~:text=Globally%2C%20one%20in%20seven%2010,illness%20and%20disability%20among%20adolescents.
World Health Organization. (2022). Adolescent and young adult health. World Health Organization. Retrieved from https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
RR designed the study protocol, designed and implemented the search strategy, screened and coded articles and extracted data, led the meta-analysis, interpreted the findings and write-up of results, drafted the initial manuscript; SSJ provided input to the study protocol, screened and coded articles and extracted data and revised the manuscript; AT screened and coded articles and extracted data and revised the manuscript; KH provided input to the study protocol, assisted with interpretation of findings and revised the manuscript; AS provided input to the study protocol and revised the manuscript; LAG provided input to the study protocol and revised the manuscript; KEC provided input to the study protocol and revised the manuscript; JR provided input to the study protocol and revised the manuscript; SRP provided input to the study protocol, provided input to coding of articles and extracted data, assisted with interpretation of findings and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interests.
Preregistration
The review was prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO; registration number: CRD42021247738). https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=247738
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Raeside, R., Jia, S.S., Todd, A. et al. Are Digital Health Interventions That Target Lifestyle Risk Behaviors Effective for Improving Mental Health and Wellbeing in Adolescents? A Systematic Review with Meta-analyses. Adolescent Res Rev (2023). https://doi.org/10.1007/s40894-023-00224-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40894-023-00224-w