Abstract
Purpose
Rotator cuff (RC) tears affect many individuals around the globe. Ambiguity of rotator cuff repair surgical outcomes is currently a limitation that is associated with fat accumulation and atrophy in the rotator cuff muscles. To improve the efficacy of rotator cuff repairs, a deeper understanding of the root causes is required. Traditionally, the term “fat infiltration” has been used to described fatty changes in muscle after rotator cuff tears. This paper introduces the concept of fat expansion as a more appropriate description for the appearance of fatty rotator cuff tear pathological changes. Furthermore, the contribution of fibroadipogenic progenitor (FAP) cells to pathological changes associated with rotator cuff injuries is presented to characterize the molecular basis of impairment. Lastly, the field of regenerative engineering is discussed as a promising solution to the pathological changes associated with rotator cuff tears.
Methods
The connection between fatty infiltration, fat expansion, fat accumulation, fibroadipogenic cells, and regenerative engineering in the context of rotator cuff tears was explored using the databases PubMed and Google Scholar.
Results
Numerous articles have supported the role of muscle resident fibroadipogenic cells as a contributor to rotator cuff tear pathological changes. In addition, regenerative engineering solutions prove to improve the pathological changes associated with rotator cuff tears.
Conclusion
The term fat expansion is more appropriate to describe fat accumulation associated with rotator cuff tears, and the employment of regenerative engineering treatment strategies improve the pathological changes associated with rotator cuff tears.
Lay Summary
Fat accumulation after rotator cuff tears has been associated with post-operative complications. Infiltration or entering of adipocytes from the external muscle environment has historically been the reported cause of the rapid increase in fat and muscle atrophy observed after rotor cuff tears. This review will dismiss the use of the term fat infiltration and acknowledge the implications of muscle resident stem cells, known as fibroadipogenic (FAP) cells, to rotator cuff tear pathological changes. Additionally, regenerative engineering, a field which seeks to regenerate various tissues using biomaterial-based scaffolds and stem cells, will be discussed as a potential solution for pathological changes.




Similar content being viewed by others
Data Availability
No datasets were generated or analyzed for the writing of this manuscript.
References
Post M, Silver R, Singh M. Rotator cuff tear: diagnosis and treatment. Clin Orthop. 1983;173:78–91.
Freedman BR, Mooney DJ, Weber E. Advances toward transformative therapies for tendon diseases. Sci Translational Med. 2022;14:eabl8814. https://doi.org/10.1126/scitranslmed.abl8814.
Saveh-Shemshaki N, Nair LS, Laurencin CT. Nanofiber-based matrices for rotator cuff regenerative engineering. Acta Biomaterialia. 2019;94:64–81. https://doi.org/10.1016/j.actbio.2019.05.041.
Laron D, Samagh SP, Liu X, Kim HT, Feeley BT. Muscle degeneration in rotator cuff tears. J Shoulder Elbow Surg. 2012;21:164–74. https://doi.org/10.1016/j.jse.2011.09.027.
Lemos DR, Babaeijandaghi F, Low M, Chang C-K, Lee ST, Fiore D, et al. Nilotinib reduces muscle fibrosis in chronic muscle injury by promoting TNF-mediated apoptosis of fibro/adipogenic progenitors. Nat Med. 2015;21:786–94. https://doi.org/10.1038/nm.3869.
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty infiltration of disrupted rotator cuff muscles. Rev Rhum Engl Ed. 1995;62(6):415–22.
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;(304):78–83.
Longo UG, Mazzola A, Magrì F, Catapano S, De Salvatore S, Carotti S, et al. Histological, radiological and clinical analysis of the supraspinatus tendon and muscle in rotator cuff tears. BMC Musculoskelet Disord. 2023;24:127. https://doi.org/10.1186/s12891-023-06237-9.
Sevivas N, Serra SC, Portugal R, Teixeira FG, Carvalho MM, Silva N, et al. Animal model for chronic massive rotator cuff tear: behavioural and histologic analysis. Knee Surg Sports Traumatol Arthrosc. 2015;23:608–18. https://doi.org/10.1007/s00167-014-3441-3.
Kim HM, Galatz LM, Lim C, Havlioglu N, Thomopoulos S. The effect of tear size and nerve injury on rotator cuff muscle fatty degeneration in a rodent animal model. J Shoulder Elbow Surg.2012;21(7):847–58. https://doi.org/10.1016/j.jse.2011.05.004.
Meyer GA, Gibbons MC, Sato E, Lane JG, Ward SR, Engler AJ. Epimuscular fat in the human rotator cuff is a novel beige depot. Stem Cells Transl Med. 2015;4:764–74. https://doi.org/10.5966/sctm.2014-0287.
Agha O, Diaz A, Davies M, Kim HT, Liu X, Feeley BT. Rotator cuff tear degeneration and the role of fibro-adipogenic progenitors. Ann NY Acad Sci. 2021;1490:13–28. https://doi.org/10.1111/nyas.14437.
Singh A, Gibbons MC, Anakwenze OA, Cheng T, Azimi H, Schenk S, Ward SR. Histological quantification of chronic human rotator cuff muscle degeneration. J Shoulder Elbow Surg.2016;25(10): E336–7. https://doi.org/10.1016/j.jse.2016.07.070.
Arrighi N, Moratal C, Clément N, Giorgetti-Peraldi S, Peraldi P, Loubat A, et al. Characterization of adipocytes derived from fibro/adipogenic progenitors resident in human skeletal muscle. Cell Death Dis. 2015;6:e1733–e1733. https://doi.org/10.1038/cddis.2015.79.
Chavez JA, Summers SA. Lipid oversupply, selective insulin resistance, and lipotoxicity: molecular mechanisms. Biochim Biophys Acta. 2010;1801:252–65. https://doi.org/10.1016/j.bbalip.2009.09.015.
Vishvanath L, Gupta RK. Contribution of adipogenesis to healthy adipose tissue expansion in obesity. J Clin Invest. 2019;129:4022–31. https://doi.org/10.1172/JCI129191.
Wang Y, Shyh-Chang N. Sphingolipids mediate lipotoxicity in muscular dystrophies. Life Medicine. 2022;1:273–5. https://doi.org/10.1093/lifemedi/lnac015.
Laurencin CT, Khan Y, Regenerative engineering. Sci Transl Med. 2012;4:160ed9. https://doi.org/10.1126/scitranslmed.3004467.
Shemshaki NS, Kan HM, Barajaa M, Otsuka T, Lebaschi M, Mishra N, Nair LS, Laurencin CT. Muscle degeneration in chronic massive rotator cuff tears of the shoulder: addressing the real problem using a graphene matrix. Proc Natl Acad Sci. 2022;119(33):e2208106119. https://doi.org/10.1073/pnas.2208106119.
Monga I, Kaur K, Dhanda SK. Revisiting hematopoiesis: applications of the bulk and single-cell transcriptomics dissecting transcriptional heterogeneity in hematopoietic stem cells. Brief Funct Genomics. 2022;21(3):159–76. https://doi.org/10.1093/bfgp/elac002.
Boldt C. What is tumor-infiltrating lymphocyte (TIL) therapy? MD Anderson Cancer Center; Cancerwise. 2021(4). https://www.mdanderson.org/cancerwise/what-is-tumor-infiltrating-lymphocyte-til-therapy--6-things-to-know.h00-159460056.html.
Perrin J, Capitao M, Mougin-Degraef M, Guérard F, Faivre-Chauvet A, Rbah-Vidal L, Gaschet J, Guilloux Y, Kraeber-Bodere F, Cherel M, Barbet J. Cell tracking in cancer immunotherapy. Front Med (Lausanne). 2020;7:34. https://doi.org/10.3389/fmed.2020.00034.
Hartwell MJ, Harold RE, Sweeney PT, Seitz AL, Marra G, Saltzman MD. Imbalance in axial-plane rotator cuff fatty infiltration in posteriorly worn glenoids in primary glenohumeral osteoarthritis: An MRI-based Study. Clin Orthop Relat Res. 2021;479(11):2471–9. https://doi.org/10.1097/CORR.0000000000001798.
Werthel JD, Boux de Casson F, Walch G, Gaudin, P, Moroder, P, Sanchez-Sotelo, J, Chaoui, J, Burdin, V. Three-dimensional muscle loss assessment: a novel computed tomography-based quantitative method to evaluate rotator cuff muscle fatty infiltration. J Shoulder Elbow Surg. 2022;31(1):165–74. https://doi.org/10.1016/j.jse.2021.07.029.
Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599–605. https://doi.org/10.1016/S1058-2746(99)90097-6.
Xu J, Liu B, Qiao Y, Ye Z, Su W, Zhao J. The 3-dimensional fatty infiltration in the overall supraspinatus can be predicted by localized sectional accumulation units: a cross-sectional study in patients with atraumatic small-to-massive rotator cuff tears. JBJS. 2023;105:380. https://doi.org/10.2106/JBJS.22.00767.
Davis DL, Kesler T, Gilotra MN, Almardawi R, Hasan SA, Gullapalli RP, et al. Quantification of shoulder muscle intramuscular fatty infiltration on T1-weighted MR images: a viable alternative to the Goutallier classification system. Skeletal Radiol. 2019;48:535–41. https://doi.org/10.1007/s00256-018-3057-7.
Addison O, Marcus RL, Lastayo PC, Ryan AS. Intermuscular fat: a review of the consequences and causes. Int J Endocrinol. 2014;2014:309570. https://doi.org/10.1155/2014/309570.
Uezumi A, Fukada S, Yamamoto N, Takeda S, Tsuchida K. Mesenchymal progenitors distinct from satellite cells contribute to ectopic fat cell formation in skeletal muscle. Nat Cell Biol. 2010;12:143–52. https://doi.org/10.1038/ncb2014.
Joe AWB, Yi L, Natarajan A, Le Grand F, So L, Wang J, et al. Muscle injury activates resident fibro/adipogenic progenitors that facilitate myogenesis. Nat Cell Biol. 2010;12:153–63. https://doi.org/10.1038/ncb2015.
Contreras O, Rossi FMV, Theret M. Origins, potency, and heterogeneity of skeletal muscle fibro-adipogenic progenitors—time for new definitions. Skeletal Muscle. 2021;11:16. https://doi.org/10.1186/s13395-021-00265-6.
Hansen JB, Kristiansen K. Regulatory circuits controlling white versus brown adipocyte differentiation. Biochem J. 2006;398:153–68. https://doi.org/10.1042/BJ20060402.
Stumm J, Vallecillo-García P, Vom Hofe-Schneider S, Ollitrault D, Schrewe H, Economides AN, et al. Odd skipped-related 1 (Osr1) identifies muscle-interstitial fibro-adipogenic progenitors (FAPs) activated by acute injury. Stem Cell Research. 2018;32:8–16. https://doi.org/10.1016/j.scr.2018.08.010.
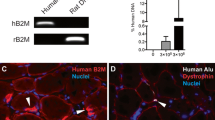
Liu X, Ning AY, Chang NC, Kim H, Nissenson R, Wang L, et al. Investigating the cellular origin of rotator cuff muscle fatty infiltration and fibrosis after injury. Muscles Ligaments Tendons J. 2016;6:6–15. https://doi.org/10.11138/mltj/2016.6.1.006.
Shirasawa H, Matsumura N, Shimoda M, Oki S, Yoda M, Tohmonda T, et al. Inhibition of PDGFR signaling prevents muscular fatty infiltration after rotator cuff tear in mice. Sci Rep. 2017;7:41552. https://doi.org/10.1038/srep41552.
Davies MR, Liu X, Lee L, Laron D, Ning AY, Kim HT, et al. TGF-β small molecule inhibitor SB431542 reduces rotator cuff muscle fibrosis and fatty infiltration by promoting fibro/adipogenic progenitor apoptosis. PLoS ONE. 2016;11:e0155486. https://doi.org/10.1371/journal.pone.0155486.
Lee C, Agha O, Liu M, Davies M, Bertoy L, Kim HT, et al. Rotator cuff fibro-adipogenic progenitors demonstrate highest concentration, proliferative capacity, and adipogenic potential across muscle groups. J Orthop Res. 2020;38:1113–21. https://doi.org/10.1002/jor.24550.
Han X. Lipidomics: developments and applications. J Chromatogr B Analyt Technol Biomed Life Sci. 2009;877:2663. https://doi.org/10.1016/j.jchromb.2009.07.007.
Flück M, Ruoss S, Möhl CB, Valdivieso P, Benn MC, von Rechenberg B, et al. Genomic and lipidomic actions of nandrolone on detached rotator cuff muscle in sheep. J Steroid Biochem Mol Biol. 2017;165:382–95. https://doi.org/10.1016/j.jsbmb.2016.08.005.
Rutkowski JM, Stern JH, Scherer PE. The cell biology of fat expansion. J Cell Biol.2015;208(5):501–12. https://doi.org/10.1083/jcb.201409063.
Tamilarasan KP, Temmel H, Das SK, Al Zoughbi W, Schauer S, Vesely PW, et al. Skeletal muscle damage and impaired regeneration due to LPL-mediated lipotoxicity. Cell Death Dis. 2012;3:e354–e354. https://doi.org/10.1038/cddis.2012.91.
Reggio A, De Paolis F, Bousselmi S, Cicciarelli F, Bernardini S, Rainer A, et al. A 3D adipogenesis platform to study the fate of fibro/adipogenic progenitors in muscular dystrophies. Dis Model Mech. 2023;16:dmm049915. https://doi.org/10.1242/dmm.049915.
Liu X, Liu M, Lee L, Davies M, Wang Z, Kim H, et al. Trichostatin A regulates fibro/adipogenic progenitor adipogenesis epigenetically and reduces rotator cuff muscle fatty infiltration. J Orthop Res. 2021;39:1452–62. https://doi.org/10.1002/jor.24865.
Iio R, Manaka T, Takada N, Orita K, Nakazawa K, Hirakawa Y, et al. Parathyroid hormone inhibits fatty infiltration and muscle atrophy after rotator cuff tear by browning of fibroadipogenic progenitors in a rodent model. Am J Sports Med. 2023;51:3251–60. https://doi.org/10.1177/03635465231190389.
Lee C, Liu M, Agha O, Kim HT, Liu X, Feeley BT. Beige fibro-adipogenic progenitor transplantation reduces muscle degeneration and improves function in a mouse model of delayed repair of rotator cuff tears. J Shoulder Elbow Surg. 2020;29:719–27. https://doi.org/10.1016/j.jse.2019.09.021.
Lee C, Liu M, Agha O, Kim HT, Feeley BT, Liu X. Beige FAP transplantation improves muscle quality and shoulder function after massive rotator cuff tears. J Orthop Res. 2020;38:1159–66. https://doi.org/10.1002/jor.24558.
Tashjian RZ, Kim SK, Roche MD, Jones KB, Teerlink CC. Genetic variants associated with rotator cuff tearing utilizing multiple population-based genetic resources. J Shoulder Elbow Surg. 2021;30:520–31. https://doi.org/10.1016/j.jse.2020.06.036.
Gladstone JN, Bishop JY, Lo IKY, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35:719–28. https://doi.org/10.1177/0363546506297539.
Washington KS, Shemshaki NS, Laurencin CT. The role of nanomaterials and biological agents on rotator cuff regeneration. Regen Eng Transl Med. 2021;7:440–9. https://doi.org/10.1007/s40883-020-00171-1.
Hee CK, Dines JS, Dines DM, Roden CM, Wisner-Lynch LA, Turner AS, et al. Augmentation of a rotator cuff suture repair using rhPDGF-BB and a type I bovine collagen matrix in an ovine model. Am J Sports Med. 2011;39:1630–40. https://doi.org/10.1177/0363546511404942.
Ratner BD. A pore way to heal and regenerate: 21st century thinking on biocompatibility. Regenerative Biomaterials. 2016;3:107–10. https://doi.org/10.1093/rb/rbw006.
Zhao S, Su W, Shah V, Hobson D, Yildirimer L, Yeung KWK, et al. Biomaterials based strategies for rotator cuff repair. Colloids Surf, B. 2017;157:407–16. https://doi.org/10.1016/j.colsurfb.2017.06.004.
Chen P, Cui L, Chen G, You T, Li W, Zuo J, et al. The application of BMP-12-overexpressing mesenchymal stem cells loaded 3D-printed PLGA scaffolds in rabbit rotator cuff repair. Int J Biol Macromol. 2019;138:79–88. https://doi.org/10.1016/j.ijbiomac.2019.07.041.
Tang X, Saveh Shemshaki N, Vernekar VN, Prabhath A, Kuyinu E, Kan H-M, et al. The treatment of muscle atrophy after rotator cuff tears using electroconductive nanofibrous matrices. Regen Eng Transl Med. 2021;7:1–9. https://doi.org/10.1007/s40883-020-00186-8.
Huang K, Su W, Zhang X, Chen C, Zhao S, Yan X, et al. Cowpea-like bi-lineage nanofiber mat for repairing chronic rotator cuff tear and inhibiting fatty infiltration. Chem Eng J. 2020;392:123671. https://doi.org/10.1016/j.cej.2019.123671.
Dai W, Kawazoe N, Lin X, Dong J, Chen G. The influence of structural design of PLGA/collagen hybrid scaffolds in cartilage tissue engineering. Biomaterials. 2010;31:2141–52. https://doi.org/10.1016/j.biomaterials.2009.11.070.
Laurencin C, Khan Y, El-Amin SF. Bone graft substitutes. Expert Rev Med Devices. 2006;3:49–57. https://doi.org/10.1586/17434440.3.1.49.
Yamaguchi M, Shinbo T, Kanamori T, Wang P, Niwa M, Kawakami H, et al. Surface modification of poly(l-lactic acid) affects initial cell attachment, cell morphology, and cell growth. J Artif Organs. 2004;7:187–93. https://doi.org/10.1007/s10047-004-0267-7.
Kim HM, Dahiya N, Teefey SA, Keener JD, Galatz LM, Yamaguchi K. Relationship of tear size and location to fatty degeneration of the rotator cuff. J Bone Joint Surg Am. 2010;92:829–39. https://doi.org/10.2106/JBJS.H.01746.
Arslantunali D, Dursun T, Yucel D, Hasirci N, Hasirci V. Peripheral nerve conduits: technology update. Med Devices (Auckl). 2014;7:405–24. https://doi.org/10.2147/MDER.S59124.
Wang Y, Zhang Y, Li X, Zhang Q. The progress of biomaterials in peripheral nerve repair and regeneration. J Neurorestoratol. 2020;8:252–69. https://doi.org/10.26599/JNR.2020.9040022.
Wang D, Zhang X, Huang S, Liu Y, Fu BS, Mak KK, et al. Engineering multi-tissue units for regenerative medicine: bone-tendon-muscle units of the rotator cuff. Biomaterials. 2021;272:120789. https://doi.org/10.1016/j.biomaterials.2021.120789.
Roßbach BP, Gülecyüz MF, Kempfert L, Pietschmann MF, Ullamann T, Ficklscherer A, et al. Rotator cuff repair with autologous tenocytes and biodegradable collagen scaffold: a histological and biomechanical study in sheep. Am J Sports Med. 2020;48:450–9. https://doi.org/10.1177/0363546519892580.
Willbold E, Wellmann M, Welke B, Angrisani N, Gniesmer S, Kampmann A, Hoffmann A, Cassan D, Menzel H, Hoheisel AL, Glasmacher B, Reifenrath J. Possibilities and limitations of electrospun chitosan‐coated polycaprolactone grafts for rotator cuff tear repair. J Tissue Eng Regen Med. 2020;14(1):186–97. https://doi.org/10.1002/term.2985.
Melamed E, Beutel BG, Robinson D. Enhancement of acute tendon repair using chitosan matrix. Am J Orthop (Belle Mead NJ). 2015;44(5):212–6.
Zheng Z, Ran J, Chen W, Hu Y, Zhu T, Chen X, et al. Alignment of collagen fiber in knitted silk scaffold for functional massive rotator cuff repair. Acta Biomater. 2017;51:317–29. https://doi.org/10.1016/j.actbio.2017.01.041.
Van Kampen C, Arnoczky S, Parks P, Hackett E, Ruehlman D, Turner A, et al. Tissue-engineered augmentation of a rotator cuff tendon using a reconstituted collagen scaffold: a histological evaluation in sheep. Muscles Ligaments Tendons J. 2013;3:229–35.
Derwin KA, Badylak SF, Steinmann SP, Iannotti JP. Extracellular matrix scaffold devices for rotator cuff repair. J Shoulder Elbow Surg. 2010;19:467–76. https://doi.org/10.1016/j.jse.2009.10.020.
Aleemardani M, Zare P, Seifalian A, Bagher Z, Seifalian AM. Graphene-based materials prove to be a promising candidate for nerve regeneration following peripheral nerve injury. Biomedicines. 2021;10:73. https://doi.org/10.3390/biomedicines10010073.
Shin SR, Li Y-C, Jang H, Khoshakhlagh P, Akbari M, Nasajpour A, et al. Graphene-based materials for tissue engineering. Adv Drug Deliv Rev. 2016;105:255–74. https://doi.org/10.1016/j.addr.2016.03.007.
Li J, Yang S, Yu J, Cui R, Liu R, Lei R, et al. Lipid- and gut microbiota-modulating effects of graphene oxide nanoparticles in high-fat diet-induced hyperlipidemic mice. RSC Adv. 2018;8:31366–71. https://doi.org/10.1039/C8RA06058D.
Saveh Shemshaki N, Kan H-M, Barajaa M, Otsuka T, Lebaschi A, Mishra N, et al. Muscle degeneration in chronic massive rotator cuff tears of the shoulder: addressing the real problem using a graphene matrix. Proc Natl Acad Sci U S A. 2022;119:e2208106119. https://doi.org/10.1073/pnas.2208106119.
Li W-J, Laurencin CT, Caterson EJ, Tuan RS, Ko FK. Electrospun nanofibrous structure: a novel scaffold for tissue engineering. J Biomed Mater Res. 2002;60:613–21. https://doi.org/10.1002/jbm.10167.
Tang X, Saveh-Shemshaki N, Kan H-M, Khan Y, Laurencin CT. Biomimetic electroconductive nanofibrous matrices for skeletal muscle regenerative engineering. Regen Eng Transl Med. 2020;6:228–37. https://doi.org/10.1007/s40883-019-00136-z.
Jiang X, Wu S, Kuss M, Kong Y, Shi W, Streubel PN, et al. 3D printing of multilayered scaffolds for rotator cuff tendon regeneration. Bioactive Materials. 2020;5:636–43. https://doi.org/10.1016/j.bioactmat.2020.04.017.
Huynh T, Kim JT, Dunlap G, Ahmadi S, Wolchok JC. In vivo testing of an injectable matrix gel for the treatment of shoulder cuff muscle fatty degeneration. J Shoulder Elbow Surg. 2020;29:e478–90. https://doi.org/10.1016/j.jse.2020.03.038.
Silva G, Ferraresi C, de Almeida RT, Motta ML, Paixão T, Ottone VO, et al. Infrared photobiomodulation (PBM) therapy improves glucose metabolism and intracellular insulin pathway in adipose tissue of high-fat fed mice. Lasers Med Sci. 2018;33:559–71. https://doi.org/10.1007/s10103-017-2408-2.
Li M, Chi X, Wang Y, Setrerrahmane S, Xie W, Xu H. Trends in insulin resistance: insights into mechanisms and therapeutic strategy. Sig Transduct Target Ther. 2022;7:1–25. https://doi.org/10.1038/s41392-022-01073-0.
Peng Y, Li X, Wu W, Ma H, Wang G, Jia S, Zheng C. Effect of mechanical stimulation combined with platelet-rich plasma on healing of the rotator cuff in a murine model. Am J Sports Med. 2022;50(5):1358–68. https://doi.org/10.1177/03635465211073339.
Kubo Y, Hoffmann B, Goltz K, Schnakenberg U, Jahr H, Merkel R, et al. Different frequency of cyclic tensile strain relates to anabolic/catabolic conditions consistent with immunohistochemical staining intensity in tenocytes. Int J Mol Sci. 2020;21:1082. https://doi.org/10.3390/ijms21031082.
Shah S, Esdaille CJ, Bhattacharjee M, Kan H-M, Laurencin CT. The synthetic artificial stem cell (SASC): shifting the paradigm of cell therapy in regenerative engineering. Proc Natl Acad Sci. 2022;119:e2116865118. https://doi.org/10.1073/pnas.2116865118.
Han S, Sun J, He S, Tang M, Chai R. The application of graphene-based biomaterials in biomedicine. Am J Transl Res. 2019;11:3246–60.
Wu SY, An SS, Hulme J. Current applications of graphene oxide in nanomedicine. Int J Nanomedicine. 2015;10(Spec Iss):9–24. https://doi.org/10.2147/IJN.S88285.
Acknowledgements
We would like to thank our funding agency: NIH Building Infrastructure Leading to Diversity (BUILD) UTEP/NIH /2TL4GM118971. Original images were created using BioRender.
Funding
NIH Building Infrastructure Leading to Diversity (BUILD) UTEP/NIH /2TL4GM118971.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Significance
Muscle atrophy and fat accumulation complicate current therapeutic approaches to treating rotator cuff tears. Understanding and acknowledging the true pathological contributors to rotator cuff tears is critical for developing regenerative engineering treatment strategies for rotator cuff tears.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Merriman Jr, M.A., Chapman, J.H., Whitfield, T. et al. Fat Expansion Not Fat Infiltration of Muscle Post Rotator Cuff Tendon Tears of the Shoulder: Regenerative Engineering Implications. Regen. Eng. Transl. Med. (2023). https://doi.org/10.1007/s40883-023-00324-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40883-023-00324-y