Abstract
Osteoarthritis (OA) is the leading cause of joint disability, and there are no FDA-approved disease-modifying drugs. The intra-articular delivery of micronized dehydrated human amnion/chorion membrane (AmnioFix, MiMedx, GA) has been shown to have a chondro-protective effect on articular cartilage in the medial meniscus transection (MMT) pre-clinical model of OA and has entered human clinical trials. AmnioFix is a well-characterized extracellular matrix (ECM)-derived therapeutic that contains hundreds of bioactive molecules, but little is known about its therapeutic mechanism in OA. The objective of this study was to elucidate, via local gene expression analysis, the molecular mechanisms of action of AmnioFix during OA development and progression. Lewis rats underwent MMT surgery, and AmnioFix or saline was injected intra-articularly 24 h post-surgery. At 5, 7, and 21 days post-surgery, articular cartilage, synovial membrane, and osteophyte tissues from multiple regions were collected and analyzed by microarray RT-PCR. Results demonstrated regional variation in the effects of amnion treatment on gene expression. Although gene expression was unaltered in articular cartilage and osteophyte tissue, pro- and anti-inflammatory markers were more highly expressed in the medial synovial membrane for the AmnioFix treatment group compared to the saline and naïve control groups. These data suggest that the previously observed chondro-protective effects of AmnioFix treatment may be mediated via alteration of the synovial membrane microenvironment. This work is the first to provide insight into the mechanisms of action of AmnioFix within the articular joint space.
Lay Summary
AmnioFix (MiMedx, Marietta, GA), obtained from placenta, is a promising candidate for treatment of osteoarthritis (OA). AmnioFix has previously demonstrated protection of the cartilage on joint surfaces in an animal model of OA. However, this is the first study to elucidate the mechanisms of action of AmnioFix on multiple tissues within the joint space. Our results demonstrated that AmnioFix acts primarily through the synovial membrane, where it induces the expression of immunomodulatory markers. We suggest that the immunomodulatory properties of AmnioFix influence the microenvironment of the synovial membrane, thereby affecting joint homeostasis and inducing a chondro-protective effect on the articular cartilage. Future work should investigate the phenotype/s of cells recruited to the synovium following AmnioFix treatment, as well as the interaction of AmnioFix with synovial tissue-resident cells. Furthermore, the effects of AmnioFix on other joint disorders such as rheumatoid arthritis, a disease involving inflammation of the synovium, warrants further investigation.




Similar content being viewed by others
References
Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. 2008;59(9):1207–13.
Ren T, van der Merwe Y, Steketee MB. Developing extracellular matrix technology to treat retinal or optic nerve injury. eNeuro. 2015;2(5).
Koob TJ, Lim JJ, Massee M, Zabek N, Denoziere G. Properties of dehydrated human amnion/chorion composite grafts: implications for wound repair and soft tissue regeneration. J Biomed Mater Res B Appl Biomater. 2014;102(6):1353–62.
Koob TJ, Rennert R, Zabek N, Massee M, Lim JJ, Temenoff JS, et al. Biological properties of dehydrated human amnion/chorion composite graft: implications for chronic wound healing. Int Wound J. 2013;10(5):493–500.
Willett NJ, Thote T, Lin ASP, Moran S, Raji Y, Sridaran S, et al. Intra-articular injection of micronized dehydrated human amnion/chorion membrane attenuates osteoarthritis development. Arthritis Res Ther. 2014;16(1):R47.
Salazar-Noratto GE, De Nijs N, Stevens HY, Gibson G, Guldberg RE. Regional gene expression analysis of multiple tissues in an experimental animal model of post-traumatic osteoarthritis. Osteoarthr Cartil. 2018.
Sellam J, Berenbaum F. The role of synovitis in pathophysiology and clinical symptoms of osteoarthritis. Nat Rev Rheumatol. 2010;6(11):625–35.
Kapoor M, Martel-Pelletier J, Lajeunesse D, Pelletier JP, Fahmi H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol. 2011;7(1):33–42.
Shi C, Pamer EG. Monocyte recruitment during infection and inflammation. Nat Rev Immunol. 2014;11(11):762–74.
Zdrenghea MT, Makrinioti H, Muresan A, Johnston SL, Stanciu LA. The role of macrophage IL-10/innate IFN interplay during virus-induced asthma. Rev Med Virol. 2015;25(1):33–49.
Jaguin M, Houlbert N, Fardel O, Lecureur V. Polarization profiles of human M-CSF-generated macrophages and comparison of M1-markers in classically activated macrophages from GM-CSF and M-CSF origin. Cell Immunol. 2013;281(1):51–61.
Martinez FO, Gordon S, Locati M, Mantovani A. Transcriptional profiling of the human monocyte-to-macrophage differentiation and polarization: new molecules and patterns of gene expression. J Immunol (Baltimore, Md : 1950). 2006;177(10):7303–11.
Lacey DC, Achuthan A, Fleetwood AJ, Dinh H, Roiniotis J, Scholz GM, et al. Defining GM-CSF- and macrophage-CSF-dependent macrophage responses by in vitro models. J Immunol (Baltimore, Md: 1950). 2012;188(11):5752–65.
Verreck FA, de Boer T, Langenberg DM, van der Zanden L, Ottenhoff TH. Phenotypic and functional profiling of human proinflammatory type-1 and anti-inflammatory type-2 macrophages in response to microbial antigens and IFN-gamma- and CD40L-mediated costimulation. J Leukoc Biol. 2006;79(2):285–93.
Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 2004;25(12):677–86.
Vannier E, Miller LC, Dinarello CA. Coordinated antiinflammatory effects of interleukin 4: interleukin 4 suppresses interleukin 1 production but up-regulates gene expression and synthesis of interleukin 1 receptor antagonist. Proc Natl Acad Sci U S A. 1992;89(9):4076–80.
Chevalier X, Goupille P, Beaulieu AD, Burch FX, Bensen WG, Conrozier T, et al. Intraarticular injection of anakinra in osteoarthritis of the knee: a multicenter, randomized, double-blind, placebo-controlled study. Arthritis Rheum. 2009;61(3):344–52.
Kraus VB, Birmingham J, Stabler TV, Feng S, Taylor DC, Moorman CT 3rd, et al. Effects of intraarticular IL1-Ra for acute anterior cruciate ligament knee injury: a randomized controlled pilot trial (NCT00332254). Osteoarthr Cartil. 2012;20(4):271–8.
Gallagher B, Tjoumakaris FP, Harwood MI, Good RP, Ciccotti MG, Freedman KB. Chondroprotection and the prevention of osteoarthritis progression of the knee: a systematic review of treatment agents. Am J Sports Med. 2015;43(3):734–44.
Magnano MD, Chakravarty EF, Broudy C, Chung L, Kelman A, Hillygus J, et al. A pilot study of tumor necrosis factor inhibition in erosive/inflammatory osteoarthritis of the hands. J Rheumatol. 2007;34(6):1323–7.
Cho H, Walker A, Williams J, Hasty KA. Study of osteoarthritis treatment with anti-inflammatory drugs: cyclooxygenase-2 inhibitor and steroids. Biomed Res Int. 2015;2015:1–10.
Verbruggen G. Chondroprotective drugs in degenerative joint diseases. Rheumatology. 2006;45(2):129–38.
Acknowledgments
The authors would like to acknowledge MidMedx (Marietta, GA) for providing AmnioFix from five donors for this study, and Clinton Smith (from Project ENGAGES, Georgia Institute of Technology) for assistance with sectioning of histological samples. The authors would also like to acknowledge the Genomics core and the Histology core at the Georgia Institute of Technology, as well as the National Science Foundation Graduate Research Fellowship Program (# DGE-1148903).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Authors Giuliana E. Salazar-Noratto, Catriana C. Nations, and Hazel Y. Stevens have no conflicts to declare. Author Robert E. Guldberg has consulted for MiMedx and owns stock options in the company.
Ethical Approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the Georgia Institute of Technology Institutional Animal Care and Use Committee (IACUC protocol #A14023).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 14 kb)
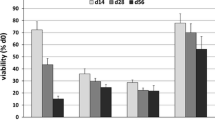
Supplementary Figure 1
Normalized (to control) relative expression (ΔΔCt) of genes significantly different, in the medial articular cartilage, between saline and AmnioFix groups; graphed as means ± SEM. ** indicates significant difference between saline and AmnioFix group for the specific timepoint at p value < 0.01 and *** at p value < 0.001. ### indicates time differences with day 7 for the specified treatment group at p value < 0.001. (PNG 62 kb)
Supplementary Figure 2
Relative expression of genes (ΔCt) of the medial side of the articular cartilage which showed significant differences between all groups (control, saline and AmnioFix), graphed as means ± SEM. * indicates significant difference with the control group for the specified timepoint at p value < 0.05, ** at p value < 0.01, and *** at p value < 0.001. $ indicates significant timepoint difference within group at p value < 0.05, $$ at p value < 0.01, and $$$ at p value < 0.01. (PNG 130 kb)
Supplementary Figure 3
Normalized (to control) relative expression (ΔΔCt) of genes associated with (pro- and anti-)inflammation that have significantly different expression in the medial synovium upon treatment with AmnioFix, graphed as means ± SEM. * indicates significant difference between saline and AmnioFix group for the specific timepoint at p value < 0.05, ** at p value < 0.01, and *** at p value < 0.001. # indicates time differences with day 5 for the specified treatment group at p value < 0.05, ## at p value < 0.01, and ### at p value < 0.001. % indicated time differences with day 7 for the specified treatment group at p value < 0.05, %% at p value < 0.01, and %%% at p value < 0.001. (PNG 66 kb)
Supplementary Figure 4
Normalized (to control) relative expression (ΔΔCt) of (A) genes associated with ECM composition and (B) genes associated with cell death that have significantly different expression in the medial synovium upon treatment with AmnioFix, graphed as means ± SEM. * indicates significant difference between saline and AmnioFix group for the specific timepoint at p value < 0.05, ** at p value < 0.01, and *** at p value < 0.001. # indicates time differences with day 5 for the specified treatment group at p value < 0.05, ## at p value < 0.01, and ### at p value < 0.001. % indicated time differences with day 7 for the specified treatment group at p value < 0.05, %% at p value < 0.01, and %%% at p value < 0.001. (PNG 44 kb)
Supplementary Figure 5
Normalized (to control) relative expression (ΔΔCt) of genes associated with ECM remodeling that have significantly different expression in the medial synovium upon treatment with AmnioFix, graphed as means ± SEM. * indicates significant difference between saline and AmnioFix group for the specific timepoint at p value < 0.05, ** at p value < 0.01, and *** at p value < 0.001. # indicates time differences with day 5 for the specified treatment group at p value < 0.05, ## at p value < 0.01, and ### at p value < 0.001. % indicated time differences with day 7 for the specified treatment group at p value < 0.05, %% at p value < 0.01, and %%% at p value < 0.001. (PNG 49 kb)
Supplementary Figure 6
Relative expression (ΔCt) of genes of the medial side of the synovial membrane which showed significant differences between the control and the operated legs (MMT surgery), regardless of treatment. * indicates significant difference with the control group for the specified timepoint at p value < 0.05, ** at p value < 0.01, and *** at p value < 0.001. # indicates significant difference with day 5 within the group at p value < 0.05, ## at p value < 0.01, and ### at p value < 0.001. $ indicates significant difference with day 7 within the group at p value < 0.05, $$ at p value < 0.01, and $$$ at p value < 0.01. (PNG 72 kb)
Rights and permissions
About this article
Cite this article
Salazar-Noratto, G.E., Nations, C.C., Stevens, H.Y. et al. Localized Osteoarthritis Disease-Modifying Changes due to Intra-articular Injection of Micronized Dehydrated Human Amnion/Chorion Membrane. Regen. Eng. Transl. Med. 5, 210–219 (2019). https://doi.org/10.1007/s40883-018-0087-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40883-018-0087-6