Abstract
Offline volunteering was faced with new challenges during the COVID-19 pandemic. Using a survey experiment with 1207 student participants, we test the impact of informing subjects about blood donation urgency (shortage information), and secondly, the effect of providing information about measures taken to reduce SARS-CoV-2 transmission at blood donation centers (hygiene information), on their inclination to donate during and after the COVID-19 lockdown. The results show that shortage information increases extensive-margin willingness to donate for non-donors by 15 percentage points (pp), on average, and increases the willingness to donate quickly for all respondents. Hygiene information, however, reduces prior donors’ intention to donate again by 8pp, on average, and reduces the willingness of non-donors to donate quickly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The voluntary donation of whole blood is widely accepted to be a good proxy of offline volunteering. However, the supply of whole blood is uncertain due to large donation fluctuations, which can be induced by shocks (e.g., Slonim et al., 2014; Spekman et al., 2021; Adena & Harke, 2022). One such shock, the COVID-19 pandemic, has impacted many aspects of daily life, and caused a dramatic reduction in donations across Europe (Chandler et al., 2021). In Germany, for instance, the pandemic lockdown caused confusion about whether blood donation was still allowed, and whether blood was still demanded to the same extent, e.g., due to decreases in elective surgeries (Vassallo et al., 2021). Further, donating blood coincided with an increased risk of personal harm via infection risk.
This study aims to assess the impact of information policies, which (1) communicate the reduced supply of blood, and (2) communicate measures used to reduce disease transmission at blood donation centers. On the one hand, potential blood donors may not be sufficiently well-informed about shortages, or they may be distracted by the pandemic. This would make it important to shift the attention of prior donors back to donating by informing prior donors and new donors about the shortage (e.g., Bruhin et al., 2015; Heger et al., 2020). Consequently, the German Red Cross and the Federal Center for Health Education have urged the general public to donate blood more often through various media outlets. On the other hand, donors may feel unsure about donation if there is a greater risk of being exposed to a disease while donating, which could be exacerbated by greater risk aversion during the pandemic (e.g., Abel et al., 2021; Harrison et al., 2022). In reaction to this, many blood donation centers have informed donors on their web pages about the hygiene measures taken to prevent transmission of SARS-CoV-2 at donation centers. How these two contrasting information policies affect blood donor motivation is another, unanswered, question.
We complement the existing literature on blood donations (e.g., Lacetera et al., 2012; Bruhin et al., 2020; Heger et al., 2020; Meyer & Tripodi, 2021; Goette & Tripodi, 2022), by implementing a donation appeal based on current supply shortages in a novel context—the COVID-19 pandemic (see e.g., Ou-Yang et al., 2020; García-Erce et al., 2021; Bilancini et al., 2022; Weidmann et al., 2022). Since our study includes both donors and non-donors, we add to the literature on first-time blood donors by assessing whether non-donors are as responsive as prior donors to shortage appeals (Wu et al., 2001; Mohammed & Essel, 2018). We classify someone as a “donor” if they report having donated whole blood at least once before in Germany \((N=552)\). Thus, “non-donors” had never donated whole blood (in Germany) \((N=655)\). We find that non-donors intend to donate in response to shortage appeals similarly to donors, but are not willing to donate as quickly. Respondents also react to the blood bank’s supply level of their own blood group.
Whether hygiene measures have a positive or negative impact on donations could depend on how acute the risk of infection actually is and how this is perceived by donors, on the vulnerability of the donation population, and on whether there are additional donation requirements, e.g., making a donation appointment, tracking potential COVID-19 contacts, and wearing a mask. We find that the hygiene measures crowd out existing donors at the extensive margin and reduce the speed of intended donation for non-donors. We observe an increased variance of donors’ intentions in response to hygiene measures, rather than a location-shift. Fear of contracting SARS-CoV-2 robustly explains the heterogeneous impact of the hygiene information.
2 Descriptive evidence of donation behavior during COVID-19
To motivate our survey experiment, we show descriptive evidence of self-reported donation behavior before and after the onset of the COVID-19 pandemic. These results show heterogeneity in donation behavior over time. Table 1 shows summary statistics from respondents to our study of donations from all persons who donated at least once in 2019 or 2020. We see a slight drop in donations in our full sample from 2019 to 2020. However, our data also include a significant fraction of donors who donated more in 2020 than 2019. Further, regression results, shown in Table A.3, Online Appendix (“OA” hereafter), all robustly suggest that knowledge of donation permission as well as information about shortages from the donation organization, potentially mitigated the reduction of blood supply during the pandemic.
3 Experimental design
3.1 Participants and timing
We conducted the survey at two large German universities (Tuebingen and Cologne) via “SoSci Survey” (details provided in OA).Footnote 1
Students donate blood more frequently than the general population due to education and age (Priller & Schupp, 2011). As expected, 46% of our (\(N=1207\)) final sample were previous donors of whole blood. The invitation e-mail intentionally contained no information regarding ‘blood donation’ and said they could win one of five 50-Euro vouchers. We used a student sample, as firstly, the group of recipients reached includes both prior donors and non-donors and secondly, to capture assessments during the height of the COVID-19 pandemic.
At the University of Tuebingen, an invitation e-mail was sent to 27,480 students on January 18, 2021. At the University of Cologne, 2000 students were asked to take part in the survey via the experimental-economics ORSEE-Network (Greiner, 2015), and a further 890 students were contacted via e-mail, which happened between January 15 and February 9, 2021. 1857 participants started the survey, and 1713 participants completed the survey, giving an average response rate of 5.64%. For an overview of responses by location, see Table A.1, OA.
During the entire period of data collection, 15 January to 16 February, 2021, the German pandemic restrictions were at their most stringent with a stringency index of 83.33/100 (Hale et al., 2021).
3.2 Questionnaire
The questionnaire for our survey experiment is divided into three different sections. Section one contains questions regarding the COVID-19 pandemic, including knowledge and perceived impact of state-imposed restrictions, and fear of a SARS-CoV-2 infection. Section two asks about personal history and motivation for blood donation and includes the experimental treatments. Section three elicits personal attitudes, socio-demographics and social preferences. For some questions subjects can click ‘prefer not to answer’ due to privacy reasons.
3.3 Treatments
We implement two main experimental treatments—one emphasizing the urgency of blood donations, shortage, and the other reflecting the COVID-19 sanitary measures at blood donation centers, hygiene. Both treatments differed slightly for Cologne and Tuebingen and were tailored according to the local regulations. The control group did not receive any additional information and answered an otherwise identical questionnaire. People who are permanently deferred from blood donation (193 respondents) were not part of the experimental treatments. Randomization was stratified by university location and donor status, with an equal treatment probability within each location-donor status stratum.
The shortage treatment was implemented in Tuebingen by showing the blood group barometer from the German Red Cross in Baden-Wuerttemberg and Hesse (Figure A.1, OA). This showed participants the levels of blood in storage by blood group on a daily basis. The levels ranged from “satisfactory blood supply” to “state of emergency, numerous donations are needed today.” The blood group barometer as of 7 January 2021 was shown, which had a “worryingly low blood supply” for 7 out of 8 blood groups, and a “low blood supply” for blood group AB+ (p. 8, OA). There was no blood group barometer available for Cologne. Hence, the Cologne subjects saw a media statement from the local news emphasizing the need for donors with blood groups O and A. Finally, the shortage treatment did not mention the COVID-19 pandemic.
The hygiene treatment showed participants the blood donation regulations in Tuebingen and Cologne. The wording and text style were the same as the presentation on the local donation centers’ websites. In Tuebingen, the regulations required donors to wear a mask, make an appointment before donating, and to refrain from donating in case of a SARS-CoV-2 infection, any SARS-CoV-2 symptoms, close contacts with a SARS-CoV-2 infection, or having recently been in a high-risk area. Donors infected with SARS-CoV-2 could donate again once four weeks had passed since recovering or ending quarantine. The Cologne requirements were very similar (Figure A.1, OA). When interpreting the hygiene treatment, we identify a reduced form effect of 1) sorting (in or out) donors who may not be eligible to donate due to restrictions, and 2) behavioral effects other than information provision, such as salience.
3.4 Outcomes
We measure donation intention by asking respondents “Will you donate blood?”. Responses are “I will donate blood within the next week”, “... within the next month”, “... after the end of the current SARS-CoV-2 lockdown”, “...will donate again after the minimum waiting period” (previous donors only), and “I will not donate blood”. Non-responses to this question (also an option) were removed from the analysis. Will donate, captures donation willingness at the extensive margin and takes the value 1 for all responses except “I will not donate blood”, coded as 0.
Initially, we had 1520 respondents that were not excluded from blood donation permanently and eligible to be in the experimental conditions. 7 respondents did not answer whether they had donated blood in the past and 11 persons responded with a relative speed index (RSI) of above 2, which is considered too fast, and were hence omitted.Footnote 2 Since responding to donation intention was voluntary, there were 295 non-responses, which do not systematically differ across treatments (joint test of equality of means: \(p=0.6522\)). Hence, we have 1207 observations of donation intention and will donate, and Table 2 tabulates these variables by donor status, i.e., whether someone is a “donor” or “non-donor”.
3.5 Covariates
All control variables that are not part of heterogeneity analyses are explained in the OA. Covariates of interest include: Cologne is a dummy for Cologne participants. Blood type is from self-reported measures. Donors are informed by the blood donation center about their blood group, which is reported on the donor ID card. Fear asks “How afraid are you of contracting the SARS-CoV-2 virus?” measured on a 5-point scale from “not at all” to “very afraid”. Time preference and risk (attitude) are measured using the Falk et al. (2018) items that have been experimentally validated for Germany. Covariates are balanced across treatments (Table A.2, OA).
4 Results
4.1 Extensive-margin analysis
We now turn to the experimental results, focusing first on the extensive margin, as measured by the variable will donate. Results are shown in Table 3, where we use a logistic regression model with robust standard errors. We report average marginal effects for all logistic regressions.
Table 3, column 1 regresses the binary dependent variable will donate on the two treatment dummies without controls, pooling donors and non-donors together. Informing participants about the shortage increases the donation willingness by 10.4pp, on average. This is driven by non-donors becoming willing to donate, showing an increase of 14.8pp relative to the control group (column 5). The extensive-margin willingness of prior donors does not change in response to the treatment, on average.
Second, the hygiene treatment causes a reduction in donation willingness of -7.3pp, on average in (column 1), which was entirely driven by prior donors (-7.7pp, column 4). Hence, communication of the the COVID-19 donation regulations crowds out the motivation of prior donors. It is unlikely that the reduction in donation willingness is driven by sorting out of donors who have recently been infected with SARS-CoV-2, as they could intend to donate next month.
Together, these findings suggest that providing information about the supply shortage is useful to maintain or increase the blood supply, and that informing donors about hygiene requirements, despite attempting to reduce uncertainty about safety, potentially makes the costs of donation more salient. These costs could come from, e.g., mask-wearing, or increased salience of donation risks, which we address below.
4.2 Intensive-margin analysis
In the next specification, we tested if there was a change in the willingness to donate quickly in response to our treatments. The shortage treatment should have a stronger effect on immediate donations, as respondents are told that the shortage is occurring at present. Further, treatment effects of both conditions might be smaller if some donors are fearful of contracting SARS-CoV-2 while donating, who might postpone donation to after the COVID-19 lockdown has ended.
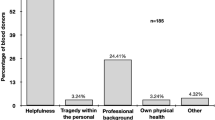
First, in the top-left panel of Fig. 1, we show the distributions of responses to donation intentions by treatment. These show a significant shift to the left (intention to donate faster) for the shortage condition (Mann–Whitney U test (“MW-U” hereafter): \(p<0.0000\)), and a marginally significant shift to the right for the hygiene treatment (MW-U: \(p=0.1023\)). The shortage condition shows significant intention to donate faster than the hygiene condition (MW-U: \(p<0.0000\)).Footnote 3
In the second from top panel in the left column of Figure 1, we focus on donors, who intend to donate more quickly in the shortage condition (MW-U: \(p=0.0007\)), but do not intend to donate less quickly in the hygiene condition (MW-U: \(p=0.9108\)). The variance of donors’ intentions in the hygiene condition is greater than in the control condition (Fligner–Killeen’s test: \(p=0.0121\)), which we explore below. Non-donors, shown in the third from top panel of Figure 1, intend to donate more quickly in the shortage condition (MW-U: \(p=0.0005\)) and less quickly in the hygiene condition (MW-U: \(p=0.0696\)).
For all intensive-margin analyses, we ran ordered logistic regressions with next week taking the lowest category, next month taking the second-lowest, and so on. This means the coefficient sign should be interpreted opposite to above. These regressions deliver similar results (Table 4 shows a summary, see Tables A.4–A.7, OA, for full results). The shortage condition consistently shows a positive impact on the intention to donate quickly, while hygiene is less robust.
Distribution of responses to donation intention by experimental condition. Left column (top 3 panels): all subjects (\(N=1077\)), donors (\(N=422\)), and non-donors (\(N=655\)). Right column (top 3 panels): respondents belonging to ABO blood group O (\(N=227\)), blood group A (\(N=208\)) and blood groups B and AB (\(N=113\)). Bottom two panels: respondents with high fear of contracting SARS-CoV-2 (scale items 4 and 5, \(N=296\)) and low fear (scale items 1–3, \(N=777\)). Bottom two panels include only non-missing fear observations
4.3 Heterogeneity analyses
We now conduct heterogeneity analyses. One test that might suggest donors are reacting to the supply shortage specifically, is an heterogeneity analysis by own blood group. The shortage treatment in both Tuebingen and Cologne highlighted that blood groups O and A are especially needed. Hence, one expects that respondents with these blood groups will intend to donate fastest. Responses by blood group are shown in the right column of Figure 1. We find that intentions to donate quickly increase in the shortage treatment for blood groups O (MW-U: \(p=0.0735\)) and A (MW-U: \(p=0.0039\)), but less so for blood groups B and AB (MW-U: \(p=0.575\), ties prevented exact calculation). This is robust when estimating ordered logistic regressions by blood group (Table 4, columns 3–6, and Table A.7, OA).
One might ask why the hygiene treatment backfired. This might depend on the increased risk of personal harm via infection risk, or increased donation cost due to waiting times. Survey evidence has found a baseline reduction in donations for individuals with high fear of SARS-CoV-2 infection risks (Chandler et al., 2021), but not yet identified interactions with policies.
First, we explore whether there are effect differences along fear of contracting the SARS-CoV-2 virus. We split subjects into a high-fear group (reporting 4 or 5, \(N=296\)) and a low-fear group (1 to 3, \(N=777\)). Responses by fear group are shown in the bottom two panels of Figure 1. The hygiene treatment shows a significant reduction in donation intention speed for high-fear (MW-U: \(p=0.0161\)), but not for low-fear (MW-U: \(p=0.6617\)). Hence, one potential channel is the increased salience of contracting SARS-CoV-2 due to hygiene information. In column 7 of Table 4, we estimate interactions between treatments and fear in an ordered logistic regression. The significantly positive interaction effect of the hygiene treatment with high fear suggests that the hygiene treatment likely backfired by making donation risks more salient. The effect magnitude, but not significance, is robust to including interactions with risk, time, and base controls (Table A.5, OA).
Next, we focus on sensitivity to, e.g., scheduling appointments, as proxied by time preference (which we label patience here for readability). Spearman’s \(\rho\) (patience, fear) is 0.0782, indicating time is a separate dimension. We do not find significant or large differences in the hygiene treatment by below-median patience (Figure A.2, OA, \(N=471\), MW-U: \(p=0.1625\)) or above-or-equal-to-median patience (Figure A.2, OA, \(N=598\), MW-U: \(p=0.4021\)). Interaction effects from ordered logistic regressions are less than half the size of the fear interaction and insignificant (column 3 of Table A.5, OA).
We do not find differences in the hygiene treatment between below-or-equal-to-median risk tolerance (\(N=569\)) and above-median risk tolerance (\(N=508\)) individuals (Figure A.2, OA, MW-U risk-tolerant: \(p=0.2322\), MW-U risk-averse: \(p=0.2455\)). Interaction effects from ordered logistic regressions are small and insignificant (column 1, Table A.5, OA). Spearman’s \(\rho\) (risk, fear) is \(-0.2622\), indicating that fear and risk tolerance are somewhat related.
4.4 Social pressure
An important question raised by the literature on the welfare effects of giving is whether social pressure drives giving (DellaVigna et al., 2012). In our study, the Tuebingen shortage treatment may induce social pressure as the blood groups with low (high) storage levels show sad (happy) emojis (Figure A.1, OA). The Cologne treatment does not contain this framing. Both treatments indicate that blood groups with A and O are urgently needed. Hence, we test the social pressure effect of emojis by analyzing effect heterogeneity between Tuebingen and Cologne.
Figure A.2, OA, shows the distributions of responses for Tuebingen and Cologne. Both Tuebingen and Cologne respondents intend to donate more quickly in response to the shortage treatment (MW-U: \(p<0.0000\) and \(p=0.0678\), respectively). We also estimate interaction effects between treatments and the Cologne dummy in an ordered logistic regression (Table A.6, OA). The odds-ratio (transformed from Table A.6) for the shortage group in Tuebingen (reference group) is 0.53 (\(p<0.0000\)), and the odds-ratio of the interaction between shortage and Cologne is 1.11, and insignificant (\(p=0.7479\)). This suggests our results are not entirely driven by social pressure or framing.
5 Discussion and conclusion
Our experimental evidence supports the interpretation that donors weigh up costs and benefits for offline volunteering during a pandemic lockdown, but only if they are sufficiently informed. Information campaigns, such as those already implemented, can help in such situations. Communicating the increased marginal impact of blood donation causes greater donation willingness of non-donors at the extensive margin, and affects the temporal donation willingness of both donors and non-donors. Further, shortage information does not cause crowding-out (Müller & Rau, 2020). On the other hand, the reduced willingness to donate when given hygiene information is important for policymakers and practitioners to consider and in contrast to the results of Ou-Yang et al. (2020). Hence, hygiene restrictions should not necessarily be removed, but their communication could be considered. Our findings are applicable to other offline volunteering settings where persons are in close contact, such as stem cell donation, plasma donation, and many other settings where supply and demand is uncertain.
The results show the potential for short-term responses to market information, and suggest it is effective to target information policies to all potential market participants.
Data availability
The replication and supplementary material for the study is available at https://doi.org/10.17632/4yt79j7nbm.1.
Notes
https://www.soscisurvey.de/en/index. Last accessed January 24th, 2024.
It is suggested that an RSI of 2.0 and above should be considered critically. See https://www.soscisurvey.de/help/doku.php/en:results:variables for details.
We left the category “just donated and waiting” (\(N=130\)) out of all intensive-margin analyses, which are not significantly differently distributed across treatments (Responses: 47 control, 40 shortage, 43 hygiene).
References
Abel, M., Byker, T., & Carpenter, J. (2021). Socially optimal mistakes? Debiasing COVID-19 mortality risk perceptions and prosocial behavior. Journal of Economic Behavior & Organization, 183, 456–480. https://doi.org/10.1016/j.jebo.2021.01.007
Adena, M., & Harke, J. (2022). COVID-19 and pro-sociality: How do donors respond to local pandemic severity, increased salience, and media coverage? Experimental Economics, 25(3), 824–844. https://doi.org/10.1007/s10683-022-09753-y
Bilancini, E., Boncinelli, L., Di Paolo, R., et al. (2022). Prosocial behavior in emergencies: Evidence from blood donors recruitment and retention during the COVID-19 pandemic. Social Science & Medicine, 314, 115438. https://doi.org/10.1016/j.socscimed.2022.115438
Bruhin, A., Goette, L., Roethlisberger, A., et al. (2015). Call of duty: The effects of phone calls on blood donor motivation. Transfusion, 55(11), 2645–2652. https://doi.org/10.1111/trf.13236
Bruhin, A., Goette, L., Haenni, S., et al. (2020). Spillovers of prosocial motivation: Evidence from an intervention study on blood donors. Journal of Health Economics, 70, 102244. https://doi.org/10.1016/j.jhealeco.2019.102244
Chandler, T., Neumann-Böhme, S., Sabat, I., et al. (2021). Blood donation in times of crisis: Early insight into the impact of COVID-19 on blood donors and their motivation to donate across European countries. Vox Sanguinis, 116(10), 1031–1041. https://doi.org/10.1111/vox.13103
DellaVigna, S., List, J. A., & Malmendier, U. (2012). Testing for altruism and social pressure in charitable giving. The Quarterly Journal of Economics, 127(1), 1–56. https://doi.org/10.1093/qje/qjr050
Falk, A., Becker, A., Dohmen, T., et al. (2018). Global evidence on economic preferences. The Quarterly Journal of Economics, 133(4), 1645–1692. https://doi.org/10.1093/qje/qjy013
García-Erce, J. A., Romón-Alonso, Í., Jericó, C., et al. (2021). Blood donations and transfusions during the COVID-19 pandemic in Spain: Impact according to autonomous communities and hospitals. International Journal of Environmental Research and Public Health, 18(7), 3480. https://doi.org/10.3390/ijerph18073480
Goette, L., & Tripodi, E. (2022). Social recognition: Experimental evidence from blood donors. CESifo Working Paper No. 9719.https://doi.org/10.2139/ssrn.4097845
Greiner, B. (2015). Subject pool recruitment procedures: Organizing experiments with ORSEE. Journal of the Economic Science Association, 1(1), 114–125. https://doi.org/10.1007/s40881-015-0004-4
Hale, T., Angrist, N., Goldszmidt, R., et al. (2021). A global panel database of pandemic policies (Oxford COVID-19 government response tracker). Nature Human Behaviour, 5(4), 529–538. https://doi.org/10.1038/s41562-021-01079-8
Harrison, G. W., Hofmeyr, A., Kincaid, H., et al. (2022). Subjective beliefs and economic preferences during the COVID-19 pandemic. Experimental Economics, 25(3), 795–823. https://doi.org/10.1007/s10683-021-09738-3
Heger, S. A., Slonim, R., Garbarino, E., et al. (2020). Redesigning the market for volunteers: A donor registry. Management Science, 66(8), 3528–3541. https://doi.org/10.1287/mnsc.2019.3371
Lacetera, N., Macis, M., & Slonim, R. (2012). Will there be blood? Incentives and displacement effects in pro-social behavior. American Economic Journal: Economic Policy, 4(1), 186–223. https://doi.org/10.1257/pol.4.1.186
Meyer, C. J., & Tripodi, E. (2021). Image concerns in pledges to give blood: Evidence from a field experiment. Journal of Economic Psychology, 87, 102434. https://doi.org/10.1016/j.joep.2021.102434
Mohammed, S., & Essel, H. B. (2018). Motivational factors for blood donation, potential barriers, and knowledge about blood donation in first-time and repeat blood donors. BMC Hematology, 18(1), 36. https://doi.org/10.1186/s12878-018-0130-3
Müller, S., & Rau, H. A. (2020). Motivational crowding out effects in charitable giving: Experimental evidence. Journal of Economic Psychology, 76, 102210. https://doi.org/10.1016/j.joep.2019.102210
Ou-Yang, J., Li, S. J., Bei, Ch., et al. (2020). Blood donor recruitment in Guangzhou, China, during the 2019 novel coronavirus (COVID-19) epidemic. Transfusion, 60(11), 2597–2610. https://doi.org/10.1111/trf.15971
Priller, E., & Schupp, J. (2011). Soziale und ökonomische Merkmale von Geld-und Blutspendern in Deutschland. DIW Wochenbericht, 78(29), 3–10.
Slonim, R., Wang, C., & Garbarino, E. (2014). The market for blood. Journal of Economic Perspectives, 28(2), 177–96. https://doi.org/10.1257/jep.28.2.177
Spekman, M. L. C., Ramondt, S., Quee, F. A., et al. (2021). New blood donors in times of crisis: Increased donation willingness, particularly among people at high risk for attracting SARS-CoV-2. Transfusion, 61(6), 1822–1829. https://doi.org/10.1111/trf.16334
Vassallo, R. R., Bravo, M. D., & Kamel, H. (2021). Pandemic blood donor demographics—Do changes impact blood safety? Transfusion, 61(5), 1389–1393. https://doi.org/10.1111/trf.16320
Weidmann, C., Derstroff, M., Klüter, H., et al. (2022). Motivation, blood donor satisfaction and intention to return during the COVID-19 pandemic. Vox Sanguinis, 117(4), 488–494. https://doi.org/10.1111/vox.13212
Wu, Y., Glynn, S. A., Schreiber, G. B., et al. (2001). First-time blood donors: Demographic trends. Transfusion, 41(3), 360–364. https://doi.org/10.1046/j.1537-2995.2001.41030360.x
Acknowledgements
We thank Patrick Kampkötter, Martin Karlsson, Daniel Kühnle, Mario Macis, Maximilian Perl, Robert Slonim, Daniel Wiesen, Joachim Winter, and Johanna Zenzes, for helpful comments and suggestions, as well as Max Grossman and Ruben Krauspe for excellent research assistance.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ehmann, S., Haylock, M. & Heynold, A.K. Offline volunteering during COVID-19: a survey experiment with prior and prospective blood donors. J Econ Sci Assoc (2024). https://doi.org/10.1007/s40881-024-00164-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40881-024-00164-8