Abstract
Purpose
To investigate the differences in foot kinematics during gait between adults with asymptomatic and symptomatic flatfoot.
Methods
The study included 10 participants (six males and four females, aged 25.7 ± 6.5 years) with symptomatic flatfoot and 10 participants (eight males and two females, aged 21.2 ± 1.0 years) with asymptomatic flatfoot. Multi-segment foot kinematics were captured during barefoot gait analysis using a 3D software. Angles were calculated for the calcaneus with respect to the shank (Sha-Cal), the midfoot with respect to the calcaneus (Cal-Mid), and the metatarsus with respect to the midfoot (Mid-Met) during the stance phase.
Results
Some differences were noted between medium-to-large effect sizes. The symptomatic group had a decreased Mid-Met dorsiflexion angle at the initial contact to 50% of the stance phase compared with the asymptomatic group. The symptomatic group also showed decreased Mid-Met abduction at initial contact, larger Sha-Cal eversion angles at 10% of the stance phase, and larger Cal-Mid eversion angles at 50% and 70% of the stance phase compared to the asymptomatic group. The symptomatic group also had a larger peak Sha-Cal eversion angle than the asymptomatic group.
Conclusion
Adults with symptomatic flatfoot exhibit significant differences in foot kinematics towards decreased forefoot dorsiflexion at initial contact to mid-stance, decreased forefoot abduction at initial contact, and increased rearfoot eversion during the stance phase compared with those with asymptomatic flatfoot during gait. Pain may impair intersegmental motion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Flatfoot is a pathological condition that is frequently encountered in adults. A population-based synthesis and systematic review indicated that the prevalence of flatfoot among adults is 24.5% [1]. Moreover, age, sex, body weight, and footwear can influence prevalence [1,2,3]. Flatfoot is characterized by partial or complete loss (collapse) of the medial longitudinal arch [4]. This abnormal change can subsequently be associated with generalized lower-limb pain, increased lower-limb fatigue, Achilles tendinopathy, patellofemoral disorders, osteoarthritis, and hip pain [5,6,7].
Compared with the normal arched foot, the flatfoot showed greater peak forefoot plantar flexion, forefoot abduction, and rearfoot internal rotation, as well as decreased peak forefoot adduction. In addition, there has been a trend towards increased rearfoot eversion [8]. Such altered foot kinematics associated with greater pronation during gait may place undue loads on the plantar fascia and increase the risk of overuse injuries such as plantar fasciitis. A sonographic study found that patients with plantar fasciitis had a thicker fascia than the controls, with significant correlations between fascial thickness and peak arch and metatarsophalangeal joint angles [9]. Kinematic studies have also indicated that individuals with plantar fasciitis exhibit kinematic alterations during gait [10]. These findings on plantar fasciitisrelated changes suggest certain symptomatic flatfoot can affect foot motion.
Not all flatfoot patients are symptomatic. Identifying the differences between symptomatic and asymptomatic flatfoot is crucial for clarifying the mechanisms that contribute to its pathology. However, to date, evidence is limited because most studies have included individuals with normal foot posture as references. Only three studies have investigated the differences between symptomatic and asymptomatic flatfoot or pronated feet. In an adult population, one study recruited physically active recreational runners with asymptomatic and symptomatic pronated feet; the results indicated that symptomatic feet displayed higher forefoot peak abduction during the stance phase of walking [11]. Additionally, differences in both extrinsic and intrinsic foot muscle morphologies were observed between the groups. Symptomatic pronators demonstrated smaller cross-sectional areas of the flexor digitorum longus and abductor hallucis and thinner peroneus muscles and abductor hallucis than their asymptomatic counterparts. However, the aforementioned findings regarding differences in foot muscle morphology and foot kinematics between symptomatic and asymptomatic pronated feet cannot be extrapolated to flat feet. A walking kinematics study using pediatric and juvenile populations showed that increased forefoot abduction occurred throughout the stance phase in symptomatic flatfooted participants compared to asymptomatic participants [12]. However, another study indicated that gait differences between pediatric and juvenile participants with asymptomatic and symptomatic flatfoot were insignificant [13]. In addition to these controversial findings, gait characteristics may differ between children and adults [14].
Because the knowledge of the kinematic differences between symptomatic and asymptomatic adult flatfoot is limited, this study aimed to investigate the differences in foot kinematics during gait in adults with asymptomatic and symptomatic flatfoot. This study hypothesized that the symptomatic group would exhibit greater forefoot plantar flexion and abduction and greater rearfoot eversion, indicating greater flattening of the medial longitudinal arch, compared to the asymptomatic group.
2 Materials and Methods
2.1 Participants
Participants with flatfoot aged 18–40 years were recruited from the local community via web advertisements. Flatfoot was confirmed by weight-bearing footprints with an arch index, defined as the ratio of the midfoot area to the total foot contact area, excluding the toes, ≥ 0.26 [15, 16]. None of the patients had neuromuscular disorders, other lower extremity abnormalities, or a history of major lower limb surgery. Participants who used foot orthotics in their daily lives were also excluded. Among the 20 participants, 10 (eight males and two females) were bilaterally asymptomatic and did not report any pain or discomfort, while 10 (six males and four females) reported unilateral (n = 3) or bilateral pain (n = 7) at the calcaneal tubercle, plantar fascia insertion point, or medial longitudinal arch 6 months before the experiment. This was performed under at least one clinical condition (pain while getting out of bed in the morning, or pain during prolonged static or dynamic action) [10, 17]. Ethical approval was granted by the Medical Ethics Committee of the Kaohsiung Armed Forces General Hospital (KAFGHIRB 108 − 030). All the participants were informed of the purpose, procedures, and risks of the study. Written informed consent was obtained from all participants.
2.2 Instrumentation and Procedures
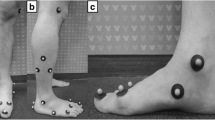
All participants were required to visit the test laboratory for a single testing session. Before data collection, the participant was clothed in close fitting pants, and then subjected to 5 min of low intensity jogging as a warm-up. Subsequently, they were required to walk barefoot at a self-selected speed on a 5-m walkway. The tested foot was randomly selected from asymptomatic and bilaterally symptomatic participants. Painful feet were selected in participants with unilateral symptoms. A Vicon motion capture system (100 Hz; Vicon Motion Systems Ltd., Oxford, UK) with eight cameras was used to assess the three-dimensional motion of the foot. Reflective markers (9 mm in diameter) were attached to the skin, according to the marker set of the Leardini foot model (Fig. 1) [18]. This multisegmental foot model included the shank, calcaneus, midfoot, and metatarsus. A force plate (1000 Hz, AMTI, Watertown, MA, USA) was used to capture the ground reaction forces and identify the stance phase of the gait. Motion and force data were collected synchronously using Vicon Nexus software. Three successful trials with heel contact to the ipsilateral toe-off were performed on the force plate (the entire stance phase of the foot) [12]. Walking speed was recorded using a digital camera (60 Hz) [19].
2.3 Data Analysis and Statistics
Customs software (MATLAB 2020a; MathWorks, Natick, MA, USA) was used to process data. Marker data were smoothed using a fourth-order Butterworth 10-Hz low-pass filter. Angles were calculated for the calcaneus with respect to the shank (Sha-Cal), the midfoot with respect to the calcaneus (Cal-Mid), and the metatarsus with respect to the midfoot (Mid-Met). Foot strike and toe-off were determined using vertical ground reaction force data at a threshold of 20 N [20]. Kinematic data for each trial were interpolated to 101 points during the stance phase. Thereafter, the sagittal and transverse planes of Mid-Met and frontal planes of Cal-Mid and Sha-Cal were averaged at initial contact (IC) of 10%, 30%, 50%, and 70% and the toe-off of the stance phase across three trials to construct a representative pattern for the two groups. Cal-Mid and Sha-Cal peak eversions were calculated across three trials to construct a representative pattern for the two groups.
Statistical analyses were performed using SPSS for Windows version 12.0. The results were expressed as mean and standard deviation (SD). The normal distribution of the parameters was measured using the Shapiro–Wilk test. All parameters were compared between the asymptomatic and symptomatic groups using the independent t-test when the distribution was normal and the Mann–Whitney U test when the distribution was not normal. Statistical significance was set at p < 0.05. In addition, the effect size (Cohen’s d) was calculated using the following formula: \(\frac{Mean1-Mean2 }{{SD}_{pooled}}{SD}_{pooled= \sqrt{\left[{(SD1}^{2}+{SD2}^{2})/2\right]}}\) [21]. Cohen’s d value of 0.2 represents a small effect; 0.5 a medium effect; and > 0.8 a large effect[21]. If the Mann–Whitney U test was used for statistical analyses, the non-parametric effect size was calculated using the formula \(r=\frac{\text{Z}}{\sqrt{N}}\). The r value of 0.1–0.3 represents small effect; 0.3–0.5 represents medium effect; >0.5 represents large effect.
3 Results
3.1 Demographic Data
The participant demographics are shown in Table 1. There were no significant differences in age, height, body weight, or body mass index between the asymptomatic (n = 10) and symptomatic (n = 10) groups (p > 0.05).
3.2 Kinematics Data
Both groups walked at similar speed (1.01 ± 0.03 vs. 1.02 ± 0.02; p = 0.29). The Mid-Met angles in the sagittal plane during the stance phase are shown in Table 2. The sagittal plane Mid-Met angle showed a large effect size at the IC (ES = 0.84; p = 0.07) and 50% of the stance phase (ES = 0.92; p = 0.05) and medium effect sizes at 10% (ES = 0.70; p = 0.13) and 30% (ES = 0.43; p = 0.04) of the stance phase. The asymptomatic group showed Mid-Met dorsiflexion at initial contact and at 10% of the stance phase, whereas the symptomatic group showed Mid-Met plantar flexion.
The Mid-Met angles in the transverse plane are presented in Table 3. The symptomatic group showed decreased abduction at initial contact for up to 10% of the stance phase.
The frontal plane Cal-Mid angles are listed in Table 4. They showed medium effect sizes of 50% (ES = 0.73; p = 0.11) and 70% (ES = 0.50; p = 0.27) of the stance phase. The symptomatic group showed a larger Cal-Mid eversion angle than the asymptomatic group at 50% and 70% of the stance phase.
The frontal-plane Sha-Cal angles are listed in Table 5. They showed a medium effect size at 10% (ES = 0.50; p = 0.27) of the stance phase. The symptomatic group showed a larger Sha-Cal eversion angle than the asymptomatic group at 10% of the stance phase.
The Cal-Mid and Sha-Cal peak eversion angles are listed in Table 6. The symptomatic group produced a larger peak Sha-Cal eversion angle than the asymptomatic group, with a medium effect size (ES = 0.51; p = 0.26).
4 Discussion
This study demonstrated differences in forefoot and rearfoot kinematics during gait in adults with asymptomatic and symptomatic flatfoot. In addition to comparing the kinematic differences between neutral and flat feet, the current study provides better insights into the possible etiology of painful flatfoot.
The symptomatic group showed a decrease in the Mid-Met dorsiflexion angle at initial contact to 50% of stance phase compared with the asymptomatic group. At initial contact, the forefoot of the symptomatic group was plantarflexed, which was consistent with that of a previous study that reported increased forefoot plantar flexion at initial contact in individuals with plantar fasciitis [10]. A study also found reductions in the forefoot with respect to the hindfoot dorsiflexion angles of approximately 2.75° and 3.88° for both the asymptomatic and symptomatic sides of individuals with plantar fasciitis when compared with healthy controls [17]. The authors suggested that these findings may be linked to the tightness of the posterior musculotendinous structures in the leg, which is believed to be one of the major contributing factors to the development of plantar fasciitis. Similar findings were reported in a military study [22]. Another adult study suggested that increased medial forefoot plantar flexion at initial contact is a pain-guarding mechanism, potentially resulting from increased plantar intrinsic foot muscle activity [10].
Regarding the transverse plane Mid-Met angle, the symptomatic group showed decreased abduction at initial contact with the early stance (10% of the stance phase). A similar finding was observed in a study that compared individuals with chronic plantar fasciitis and healthy controls [23]. Individuals with pain compensate for the reduction in medial arch collapse, perhaps by managing pain. During the propulsion phase of walking, no substantial differences were found between the symptomatic and asymptomatic groups in the current study. A previous study found that adults with chronic plantar fasciitis showed similar movement patterns of forefoot plantarflexion and adduction during late stance as healthy controls [10] and that flatfoot compared to normal-arched foot had reduced adduction during terminal stance for forefoot motion relative to the rearfoot [8]. However, in recreational runners with symptomatic pronators, larger forefoot peak abduction occurred during the stance phase of walking than in asymptomatic pronators [11, 12]. This disparity may be due to the different nature of the studies, such as purpose and analysis model, and different sample characteristics (for instance, foot posture and physical activity level). Whether foot kinematics differ between individuals with symptomatic flatfoot (i.e., plantar fasciitis) and those with asymptomatic flatfoot should be confirmed in further studies.
Differences in rearfoot kinematics were also observed between the groups. The symptomatic group showed a larger Sha-Cal eversion angle at 10% of the stance phase and a larger Cal-Mid eversion angle at 50% and 70% of the stance phase than the asymptomatic group. The symptomatic group also had a larger peak Sha-Cal eversion angle than did the asymptomatic group. This is in accordance with the previous findings of increased total rearfoot eversion in individuals with plantar fasciitis [10]. Increased rearfoot eversion increases plantar fascial tension via dynamic arch collapse [24]. Although our study participants did not undergo a clinical examination for the diagnosis of plantar fasciitis, the inclusion criterion was the recruitment of possible patient candidates. In contrast, one study found a decrease in rearfoot eversion but an increase in forefoot peak abduction among young physically active adults with pronated feet compared with asymptomatic pronators [11]. The findings of the current study suggest that compared with physically active individuals, adults with flatfoot may adopt different intersegmental foot motions.
This study had some limitations. Although alterations in multi-segment foot kinematics have been noted in symptomatic flatfoot compared to asymptomatic flatfoot, it is not known whether these differences are the cause or result of pain. We did not measure the pain characteristics (such as intensity, symptom duration, time of pain occurrence, and associated activities), physical activity, or exercise habits; hence, their effects on foot kinematics are uncertain. Furthermore, the sample size is relatively small. Therefore, further studies with larger sample sizes are warranted.
5 Conclusion
Adults with symptomatic flatfoot exhibit significant differences in foot kinematics towards decreased forefoot dorsiflexion at initial contact to mid-stance, decreased forefoot abduction at initial contact, and increased rearfoot eversion during the stance phase compared with those with asymptomatic flatfoot during gait. Pain may impair intersegmental motion, which has implications for the pain mechanisms in symptomatic flatfoot. This finding has clinical implications for the development of treatment strategies, such as foot orthotics. However, this requires further investigation.
References
Salinas-Torres, V. M., Salinas-Torres, R. A., Carranza-García, L. E., Herrera-Orozco, J., & Tristán-Rodríguez, J. L. (2023). Prevalence and clinical factors Associated with Pes Planus among children and adults: A Population-based synthesis and systematic review. The Journal of Foot and Ankle Surgery, 62(5), 899–903. https://doi.org/10.1053/j.jfas.2023.05.007.
Chen, J. P., Chung, M. J., & Wang, M. J. (2009). Flatfoot prevalence and foot dimensions of 5- to 13-year-old children in Taiwan. Foot and Ankle International, 30(4), 326–332. https://doi.org/10.3113/fai.2009.0326.
Echarri, J. J., & Forriol, F. (2003). The development in footprint morphology in 1851 Congolese children from urban and rural areas, and the relationship between this and wearing shoes. Journal of Pediatric Orthopaedics B, 12(2), 141–146. https://doi.org/10.1097/01.bpb.0000049569.52224.57.
Lee, M. S., Vanore, J. V., Thomas, J. L., Catanzariti, A. R., Kogler, G., Kravitz, S. R., Miller, S. J., & Gassen, S. C. (2005). Diagnosis and treatment of adult flatfoot. The Journal of Foot and Ankle Surgery, 44(2), 78–113. https://doi.org/10.1053/j.jfas.2004.12.001.
Franco, A. H. (1987). Pes Cavus and pes planus. Analyses and treatment. Physical Therapy, 67(5), 688–694. https://doi.org/10.1093/ptj/67.5.688.
Jung, D. Y., Koh, E. K., & Kwon, O. Y. (2011). Effect of foot orthoses and short-foot exercise on the cross-sectional area of the abductor hallucis muscle in subjects with pes planus: A randomized controlled trial. Journal of Back and Musculoskeletal Rehabilitation, 24(4), 225–231. https://doi.org/10.3233/bmr-2011-0299.
Shibuya, N., Jupiter, D. C., Ciliberti, L. J., VanBuren, V., & La Fontaine, J. (2010). Characteristics of adult flatfoot in the United States. The Journal of Foot and Ankle Surgery, 49(4), 363–368. https://doi.org/10.1053/j.jfas.2010.04.001.
Levinger, P., Murley, G. S., Barton, C. J., Cotchett, M. P., McSweeney, S. R., & Menz, H. B. (2010). A comparison of foot kinematics in people with normal- and flat-arched feet using the Oxford Foot Model. Gait & Posture, 32(4), 519–523. https://doi.org/10.1016/j.gaitpost.2010.07.013.
Wearing, S. C., Smeathers, J. E., Yates, B., Sullivan, P. M., Urry, S. R., & Dubois, P. (2004). Sagittal movement of the medial longitudinal arch is unchanged in plantar fasciitis. Medicine and Science in Sports and Exercise, 36(10), 1761–1767. https://doi.org/10.1249/01.mss.0000142297.10881.11.
Chang, R., Rodrigues, P. A., Van Emmerik, R. E., & Hamill, J. (2014). Multi-segment foot kinematics and ground reaction forces during gait of individuals with plantar fasciitis. Journal of Biomechanics, 47(11), 2571–2577. https://doi.org/10.1016/j.jbiomech.2014.06.003.
Zhang, X., Pauel, R., Deschamps, K., Jonkers, I., & Vanwanseele, B. (2019). Differences in foot muscle morphology and foot kinematics between symptomatic and asymptomatic pronated feet. Scandinavian Journal of Medicine and Science in Sports, 29(11), 1766–1773. https://doi.org/10.1111/sms.13512.
Kerr, C. M., Zavatsky, A. B., Theologis, T., & Stebbins, J. (2019). Kinematic differences between neutral and flat feet with and without symptoms as measured by the Oxford foot model. Gait & Posture, 67, 213–218. https://doi.org/10.1016/j.gaitpost.2018.10.015.
Hösl, M., Böhm, H., Multerer, C., & Döderlein, L. (2014). Does excessive flatfoot deformity affect function? A comparison between symptomatic and asymptomatic flatfeet using the Oxford Foot Model. Gait & Posture, 39(1), 23–28. https://doi.org/10.1016/j.gaitpost.2013.05.017.
Lythgo, N., Wilson, C., & Galea, M. (2009). Basic gait and symmetry measures for primary school-aged children and young adults whilst walking barefoot and with shoes. Gait & Posture, 30(4), 502–506. https://doi.org/10.1016/j.gaitpost.2009.07.119.
Cavanagh, P. R., & Rodgers, M. M. (1987). The arch index: A useful measure from footprints. Journal of Biomechanics, 20(5), 547–551. https://doi.org/10.1016/0021-9290(87)90255-7.
Leung, A. K., Mak, A. F., & Evans, J. H. (1998). Biomedical gait evaluation of the immediate effect of orthotic treatment for flexible flat foot. Prosthetics and Orthotics International, 22(1), 25–34. https://doi.org/10.3109/03093649809164454.
Bovonsunthonchai, S., Thong-On, S., Vachalathiti, R., Intiravoranont, W., Suwannarat, S., & Smith, R. (2019). Alteration of the multi-segment foot motion during gait in individuals with plantar fasciitis: A matched case-control study. Acta of Bioengineering and Biomechanics, 21(4), 73–82.
Leardini, A., Benedetti, M. G., Berti, L., Bettinelli, D., Nativo, R., & Giannini, S. (2007). Rear-foot, mid-foot and fore-foot motion during the stance phase of gait. Gait & Posture, 25(3), 453–462. https://doi.org/10.1016/j.gaitpost.2006.05.017.
Santos, L., Ribeiro, A. S., Schoenfeld, B. J., Nascimento, M. A., Tomeleri, C. M., Souza, M. F., Pina, F. L., & Cyrino, E. S. (2017). The improvement in walking speed induced by resistance training is associated with increased muscular strength but not skeletal muscle mass in older women. European Journal of Sport Science, 17(4), 488–494. https://doi.org/10.1080/17461391.2016.1273394.
Braga, U. M., Mendonça, L. D., Mascarenhas, R. O., Alves, C. O. A., Filho, R. G. T., & Resende, R. A. (2019). Effects of medially wedged insoles on the biomechanics of the lower limbs of runners with excessive foot pronation and foot varus alignment. Gait & Posture, 74, 242–249. https://doi.org/10.1016/j.gaitpost.2019.09.023.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences New York (Vol. 54). Academic.
Harutaichun, P., Boonyong, S., & Pensri, P. (2021). Differences in lower-extremity kinematics between the male military personnel with and without plantar fasciitis. Physical Therapy in Sport, 50, 130–137. https://doi.org/10.1016/j.ptsp.2021.04.007.
Chang, R., van Emmerik, R., & Hamill, J. (2021). Chronic plantar fasciitis reduces rearfoot to medial-forefoot anti-phase coordination. Clinical Biomechanics, 88, 105439. https://doi.org/10.1016/j.clinbiomech.2021.105439.
Lee, S. Y., Hertel, J., & Lee, S. C. (2010). Rearfoot eversion has indirect effects on plantar fascia tension by changing the amount of arch collapse. Foot (Edinb), 20(2–3), 64–70. https://doi.org/10.1016/j.foot.2010.06.003.
Funding
This study was supported by a grant from Zuoying Armed Forces General Hospital (KAFGH-ZY-A-109025).
Author information
Authors and Affiliations
Contributions
Conceptualization and investigation, Wei-Chi Tsai and Zong-Rong Chen; data processing, Jui-Tse Hsu; writing-original draft, Zong-Rong Chen and Chen-Yi Song; writing-review and editing, Zong-Rong Chen and Chen-Yi Song.
Corresponding author
Ethics declarations
Ethical Approval
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the Human Research Ethics Committee of Kaohsiung Armed Forces General Hospital (No. KAFGHIRB 108 − 030).
Consent to Participate
All participant written the informed consent.
Consent to Publish
All participant consent to publish data.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tsai, WC., Chen, ZR., Hsu, JT. et al. Multi-Segment Foot Kinematics during Gait in Adults with Asymptomatic and Symptomatic Flatfoot. J. Med. Biol. Eng. 44, 471–477 (2024). https://doi.org/10.1007/s40846-024-00877-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-024-00877-5