Abstract
Purpose
Finite element analysis (FEA) was used to evaluate the effects of different thicknesses, numbers, and positions of the miniplate applied in bilateral sagittal split osteotomy (BSSO) under two occlusal conditions.
Methods
An FEA model of the mandibles was constructed and combined with different thicknesses (0.6 or 1 mm), number (one or two), positions (upper or lower) of a miniplate and was divided into six models. In addition, external forces were applied to the muscles to simulate the intercuspal position (ICP) and right unilateral molar clench. This study used the reaction force of the temporomandibular joints and the stress of the mandible as observation indexes.
Results
The results of this study show that, under ICP, the 0.6 mm lower model generated greater TMJ force reaction compared to the 0.6 mm upper model. The same trend was seen in the 1 mm lower model compared to the 1 mm upper model. Regarding the stress of the bone on the screw-implanted sites, under ICP, screw 10 showed greater stress than screw 2, and screw 11 showed greater stress than screw 3. The stress values of the miniplates showed, under ICP, point 1-c was greater than point 3-c, and point 1-b was greater than point 3-b.
Conclusion
In the case of BSSO mandibular advancement surgery, implanting the miniplate at the upper position can reduce the force on the TMJ and the stress on the distal segment of the mandible. The miniplate can also resist the tensile stress more effectively. In addition, implanting two miniplates with thinner sizes may be an alternative in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The prevalence of type II malocclusion is 20.2% [1], and cases with skeletal discrepancy require surgical intervention to achieve ideal results. Intraoral vertical ramus osteotomy (IVRO) and bilateral sagittal split osteotomy (BSSO) are commonly used for treating type II malocclusion with mandibular deficiency. Compared with IVRO, BSSO has the advantages of extensive bony contact and rigid fixation, so the period of intermaxillary fixation (IMF) can be reduced or even spared [2]. In patients with mandibular deficiency, BSSO has been proven to have a positive long-term effect on patients’ quality of life [3]. However, BSSO also has some disadvantages, including bad split, neurosensory disturbance, and other complications associated with implanted screws and miniplates (e.g., infection, implant exposure, palpability), which require further management, such as removal [4].
Since the period of post-operation IMF after BSSO is shortened or spared, rigid fixation plays a rather important role in bone healing. The most commonly used methods for rigid fixation are monocortical miniplate fixation or bicortical screw fixation. The latter has a higher mandibular canal penetration incidence rate [5]. Matsushita et al. recommended monocortical miniplate fixation over bicortical screw fixation for rigid fixation in BSSO [6]. Many studies have investigated the reasons for removing the screws and miniplates after BSSO. Infection and implanted material exposure were the main reasons [7,8,9,10]. Other reasons such as palpability [7, 8, 10], discomfort with foreign matter [8], and irritation [7] were also reported and eventually resulted in the removal of the implants. Thus, even with miniplates, the thickness and discomfort caused by foreign matter are so bothersome that some patients ask them to be removed. The use of thinner miniplates may reduce the rate of plate removal due to the aforementioned reasons.
Finite element analysis (FEA) has been proven to be a powerful tool for analyzing the biomechanics of maxillofacial surgery [11]. Many studies have used FEA to analyze the different types and positions of rigid fixations and the strain and stability on the miniplates and mandibles [12,13,14,15,16,17,18,19]. Among studies that have used FEA to analyze the biomechanics of BSSO, most of them explored different rigid fixation methods with different plate designs and positions. However, the biomechanics of thickness was seldom assessed. Therefore, the biomechanics of miniplate thickness is worth exploring. In addition, some studies using FEA have analyzed the biomechanics of multiple miniplates and have designed the miniplate to be implanted at a lower position (below the middle portion or near the inferior border of the mandible) [12,13,14,15]. Nonetheless, such implant positions are clinically inaccessible by the intraoral approach, requiring access via a transoral approach (e.g., trocar), which results in wounds on the face and a compromised esthetic outcome. Considering the operability of the surgery and esthetics, the intraoral approach and placement of the miniplates close to the superior border of the mandible for rigid fixation would be appropriate and applicable in routine clinical practice. Positions of miniplate fixation are therefore limited by the surgical approach and may affect the biomechanics of the overall mandible structure.
According to the above literature, BSSO has different mechanical effects due to different configurations, the number and position of the implants, and the strain applied to the mandible. Therefore, the primary purpose of this study was to use FEA to evaluate the biomechanical effects of different thicknesses, numbers, and positions of the miniplate applied in BSSO surgery under different occlusal conditions. The study results can provide a biomechanical reference for surgeons performing BSSO.
2 Materials and Methods
2.1 Building a Simulation Geometry Model
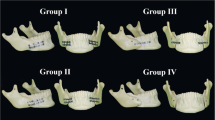
In this study, we evaluated the biomechanical effects of different thicknesses, numbers, and positions of the miniplate applied in BSSO surgery under different occlusal forces. Therefore, an FEA computer model of the mandible implanted with miniplates was established in this study. The model consists of four parts, namely, the mandibular cortical bone, cancellous bone, miniplates, and screws (Fig. 1a). The configuration of the established mandibular model was primarily obtained from a previous study [20], and is divided into two parts: cortical bone and cancellous bone. This study used 3D computer-aided design CAD software (Solidworks 2016, Dassault Systèmes SolidWorks Corp, Waltham, MA, USA) for computer graphics. The peripheral contour of cortical bone and cancellous bone of mandible was imported into Solidworks, and loft function was used to establish the complete solid model of cortical bone and cancellous bone of mandible. The computer model of the mandible was cut with reference to the previous literature to simulate the BSSO surgery for the treatment of mandibular deficiency (The horizontal fracture line was just superior to the lingula and ran on the oblique ridge of the ramus. The anterior vertical fracture line was carried inferiorly to the second molar. The posterior vertical fracture line started from the posterior end of the horizontal cut, continued posteriorly to the lingula and met the anterior fracture line at the mandible border [21].), and the distal segment was advanced by 4 mm [22, 23]. In addition, the miniplates, screws, cortical bone, and cancellous bone were combined using CAD software Solidworks. Six computer models (Fig. 1b) were built in this study, primarily focusing on different thicknesses (0.6 or 1 mm), numbers (one or two), and implanted positions (upper or lower) of miniplates in BSSO surgery. After the 3D computer models were established, the models were imported into FEA software (ANSYS Workbench 19.0, ANSYS, Inc., Canonsburg, PA) for analysis.
2.2 Loading Conditions and Boundary Conditions
This study mainly investigated two common occlusal conditions with more significant stress in clinical practice [23]. The two occlusal conditions are intercuspal position (ICP) and right unilateral molar clench (RMOL). ICP is characterized by maximum intercuspation of the posterior teeth, while RMOL involves contact of the right (unilateral) posterior teeth. In this FEA, it was necessary to provide different boundary conditions and loading conditions according to these two different occlusion conditions. This study was primarily based on the data and methods of external force given in previous studies [20, 23,24,25,26]. The temporomandibular joint (TMJ) was set as the fixed end with the displacement setting method in boundary conditions. This displacement values for this point’s X-axis, Y-axis, and Z-axis were all 0 (this setting can allow this point to rotate freely). In the setting of the loading condition, the external forces were applied to the muscles of the superficial masseter (SM), deep masseter (DM), medial pterygoid (MP), anterior temporalis (AT), middle temporalis (MT), and posterior temporalis (PT) (Fig. 2a). The magnitude and direction of the external force are shown in Table 1. In addition, based on different occlusal conditions, the locations at the incisor, canine, premolar, and molar were fixed accordingly (Fig. 2b), as shown in Table 1. Figure 3 shows the setting of the loading condition. The external forces were applied to the muscles. As to the incised site of the mandible, where the miniplate was in contact with the mandible, the contact was set as no separation, primarily to simulate the surface without separation, but also to allow slight frictionless sliding.
2.3 Material properties of the model
This research model consists of four parts, namely cortical bone, cancellous bone, miniplates, and screws. The material properties used in this study were also obtained from the previous literature [23]. Table 2 shows the material properties used for the simulations in this study. All materials were assumed to be homogeneous, isotropic, and linear elastic. In this study, the material properties were expressed by Young’s modulus (E) and Poisson’s ratio (ν). As to the miniplate, titanium alloy was primarily used as the simulated material. The bone was also divided into cortical bone and cancellous bone. In addition, the meshing of the computer model of the FEA in this study was tested by the convergence test (The convergence test is mainly based on mesh size control. The mesh sizes of convergence test were 5 mm, 4 mm, 3 mm, 2 mm, 1 mm, and 0.9 mm. Total deformation was used as the observation index of the convergence test.), and the 5% stop criteria of the convergence test were reached in all models (Table 3). The mesh size used in this study was 1 mm. Therefore, this study’s finite element mesh model was reasonable for investigating the biomechanical effects of different thicknesses, numbers, and implanted positions of miniplates under different occlusal conditions. Table 4 shows the number of nodes and meshes of the six computer models in this study (Fig. 4). The meshing process was carried out in ANSYS Workbench.
2.4 Evaluation index
After FEA, this study used the reaction force of the TMJs and the von Mises stress of the mandibular models as the primary observation index. In addition, the stress of the bone at the screw implantation sites was also observed. Figure 5a primarily shows the position of each screw and the corresponding screw number. Furthermore, the stress of the four specific points at the cutting edges of proximal and distal segments was observed, and the points and corresponding labels are shown in Fig. 5b. The distribution of von Mises stress on the left and right sides of the miniplates and the mandible was observed to investigate the biomechanical effects of two different thicknesses, numbers, and implanted positions of the miniplates on mandibular deficiency treated after BSSO under different occlusal conditions.
3 Results
After FEA, the stress distribution of the overall structure and the reaction force at the fixed ends of the bilateral TMJ were obtained. Figure 6 shows the magnitude and direction of the bilateral TMJ reaction force under ICP and RMOL in the six models. The component force value on the X, Y, and Z-axis and total reaction force value under ICP and RMOL in the six models are listed in Table 5. The results show that, under ICP, regardless of the thickness of the miniplate, the TMJ of the lower model had a more significant reaction force than the upper model. In contrast, the difference between the upper and lower models and the upper models was non-significant. In addition, under RMOL, high reaction forces of the contralateral (left) TMJ were observed in all six models.
Figure 7 shows the overall stress distribution of the six models under ICP and RMOL. As can be seen from the stress distribution in the figure, both the 0.6 and 1 mm model exhibited high stress at the cutting edges of the proximal and distal segments under ICP or RMOL. Moreover, compared with the lower model, the upper model showed lower stress on the distal segment of the mandible. In addition, under the same thickness of the miniplate, the upper and lower model had the lowest stress in the distal segment of the mandible, followed by the upper model, with the lower model showing the largest stress. Finally, compared with the 1 mm upper and lower model, the stress distribution of the 1 mm upper model showed no significant difference in the distal segment of the mandible; while in the 0.6 upper and lower model, the stress distribution of the distal segment of the mandible was also similar to the 1 mm upper model.
Figure 8 shows the stress distribution of the mandibular bone at the implantation sites of the screw under ICP and RMOL in the six models. The cortical bone had more significant stress than the spongy bone. Table 6 lists the stress values corresponding to different screw numbers. In the model with only one miniplate implanted (the upper or the lower model), a higher stress value was observed in the mandibular bone at the implantation sites of the screw near the cutting edges of the proximal and distal segments. In addition, under ICP and the working side (right side) of RMOL, the lower model generally revealed higher stress on the mandibular bone around the implanted screw than in the upper model.
Figure 9 shows the stress distribution of the miniplate under ICP and RMOL in the six models. Table 7 lists the stress value corresponding to the sites of the four specific points on the miniplate over the cutting edges of proximal and distal segments by site labels (each label on the miniplate is shown in Fig. 5b). It can be seen that under the premise of the same number and position of miniplates, compared with the 1 mm model, the 0.6 mm model showed higher stress on the miniplate. In addition, the stress on the upper and lower models of the miniplate was lower than that of the upper model or the lower model. Furthermore, the miniplate in the upper model was subject to higher stress than the lower model. Finally, under ICP and the working side of RMOL, it can be observed that the two diagonal points (the upper point of the distal segment and the lower point of the proximal segment) were the most stressed among the four points.
4 Discussion
This study primarily used FEA to explore the biomechanical effects of different thicknesses, numbers, and positions of the miniplate applied in BSSO surgery under different occlusal conditions. The two occlusal conditions investigated in this study were based on the results of previous studies [23], which found that when the jaw is subjected to different occlusal conditions, the intercuspal position (ICP) and right unilateral molar clench (RMOL) result in high stress in the whole mandibular structure. Therefore, this study used these two occlusal conditions to simulate the force on the mandibles.
During and after orthognathic surgery, the surgeon must consider the state of the TMJ. Existing studies have explored how to avoid condylar sag during surgery [27] and have assessed the clinical usefulness of condylar positioning devices [28]. The changes in condylar angle and position after BSSO and TMJ resorption have also been widely studied [29,30,31]. The postoperative status of the TMJ has also been confirmed to affect the stability of surgical outcomes after BSSO [32]. Therefore, in clinical practice, it is important to avoid unnecessary force on the TMJ. In this study, the reaction force on the bilateral TMJ was observed through FEA, and this reaction force represented the magnitude of the force on the TMJ itself. The results of this study indicate that, under ICP, when the implanted position of the miniplate was relatively low, the reaction force of the TMJ increased, which should be avoided in clinical practice. This finding is also compatible with the ideal line of osteosynthesis published by Champy et al. [33]. This concept is also widely used in clinical practice. In addition, under RMOL occlusion, the results of the study reveal that a high reaction force on the contralateral (left side) TMJ is created, so after BSSO surgery, the patient should be instructed to avoid excessive occlusion of the unilateral posterior teeth to avoid excessive force on the contralateral TMJ.
By examining the overall stress distribution of the model, high stress was noted at the cutting edges of the proximal and distal segments. The main reason is that the operation sagittally splits and advances the ascending ramus of the mandible, thus reducing the thickness (cross-sectional area) of the mandible, resulting in high stress. In addition, when the miniplate was implanted at a higher position, the distal segment of the mandible was subjected to lower stress, mainly because the position of the miniplate is closer to the tension side of the mandible, so the influence of tensile stress on the cutting edge could be reduced, thus resulting in lower stress on the distal end of the mandible. Another finding is that in the model with two 0.6 mm miniplates implanted, the stress on the distal segment of the mandible was similar to that of a model with a 1 mm miniplate implanted at the upper position. Placing two miniplates reveals a better biomechanics outcome than placing only one miniplate with the same thickness. Previous studies have reported this result [34,35,36]. However, no studies have compared the biomechanics between one thicker miniplate and two thinner miniplates investigated in our study. In clinical practice, most surgeons choose to implant the miniplate close to the upper edge via the intraoral approach, and 1–2 mm thickness miniplates are selected for better strength. However, a thicker miniplate with a higher implantation site near the mucosal surface may be related to a greater incidence of miniplate removal after surgery, with the reasons of palpability, discomfort with foreign matter, and irritation reported as reasons in previous research [7, 8, 10]. If feasible, reducing the thickness of the miniplate and implanting another thinner miniplate at a lower position can be an alternative.
Nowadays, miniplates and monocortical screws are widely used for rigid fixation in craniofacial surgery. Because the monocortical screw only penetrates a single layer of cortical bone to achieve the fixation effect, the stress of the cortical bone is a concern. Excessive stress may lead to undesirable outcomes such as cortical bone tear or even screw loosening. In this study, the stress distribution of the mandible at the screw implantation sites was observed. Higher stress was noted on the cortical bone because the mandible deforms when the mandible is subjected to an external force. According to Hooke’s law (stress = Young’s coefficient x strain), the stress is proportional to Young’s coefficient. Compared with spongy bone, cortical bone has a more significant Young’s coefficient, so there is more significant stress on the cortical bone. In addition, more significant stress on the bone at the screw implantation site was found when the miniplate was placed at a lower position. Therefore, when the miniplate is implanted, the position of the miniplate should be closer to the upper part of the mandible to reduce the stress generated. Moreover, when only a single miniplate (upper or lower) is implanted, the bone at the screw implantation sites has a higher stress value near the cutting edges of the proximal and distal segments. This finding is compatible with previous researches [13,14,15]. Hence, a screw with increased diameter or length could be considered at those sites to increase the contact area with the bone and reduce the stress there. Alternatively, the implantation of 2 miniplates could also reduce the stress on the bone at the screw implantation sites near the cutting edges of proximal and distal segments.
By observing the stress distribution of the miniplate, high stress on the miniplates was noted at the cutting edges of the proximal and distal segments. A previous study also showed similar results [37]. Therefore, in this study, we found that the stress values corresponded to the sites of the four specific points on the miniplate over the cutting edges of proximal and distal segments. Among the four specific points, the upper point of the distal segment and the lower point of the proximal segment revealed higher stress values under ICP. These findings were in line with a previous study that showed two torsion forces would be generated at the cutting gap after BSSO [38]. The high stress on the diagonal points of the miniplate can also be observed in FEA results from other literature [14, 37]. In addition, when a thin miniplate was implanted, the miniplate was prone to deformation according to Hooke’s law, so higher stress occurred. This consequence can be avoided by inserting one more miniplate. Furthermore, the stress distribution also indicated that a higher position of the miniplates could result in more significant stress on the miniplate. According to a previous study, the result can be explained by the fact that after BSSO surgery the mandible will generate two bending forces when subjected to external force [38]. According to the bending stress formula, this bending stress is proportional to the vertical distance from the bending center, so when the miniplate is fixed at the upper position, to resist the influence of the tensile stress, higher stress is generated. This result also indicates the advantage of implanting a miniplate at a relatively upper position when performing rigid fixation.
This study had some limitations. First, all material properties in this study were assumed to be homogeneous, isotropic, and linearly elastic. This assumption was mainly to simplify the simulation conditions of this study, so the material properties were set with reference to previous studies [20, 23]. Second, some simplifications were made in the simulation model of this study. Only the mandibles were observed in this study, not the entire maxillofacial complex. In addition, this study did not establish an actual tooth model because this study mainly observed the impact of miniplate implantation, and teeth were not the focus of this study. This study fixed the mandible in the occlusal plane in different tooth positions. There have been several studies on this method [20]. The model used in this study is mainly designed for previous studies, simulating two occlusal modes of ICP and RMOL. Therefore, the computer model in this study did not establish a tooth model, and the simplification allowed a shorter computer simulation time. Following the simplifications, although there would likely be some differences between the simulation and real-world data, the model nevertheless revealed apparent trends and relevant patterns that helped inform our understanding of the issues being investigated.
This study used observations from FEA to explore the biomechanical effects of different thicknesses, numbers, and positions of the miniplate applied in BSSO surgery under different occlusal conditions. The FEA results revealed multiple hints that may be useful in clinical practice. Implanting the miniplate at the upper position showed better biomechanical outcomes than at a relatively lower position, including lower stress of the cortical bone at the implantation sites of the screw, lower TMJ reaction forces, and better stress distribution at the distal segment of the mandible. These results echoed the concept of mandibular osteosynthesis published by Champy [33]. Although the values analyzed in this study may slightly differ from the actual clinical situation, the results of this study provide a biomechanical reference for oral maxillofacial surgeons regarding the position, number, and thickness of miniplate implantation during BSSO surgical treatment. It can be used as a preliminary study for future related studies, such as different designs and materials of the implant, to provide clinicians with more biomechanical information about the implanted structure.
5 Conclusion
In BSSO mandibular advancement surgery, implanting the miniplate at the upper position can reduce the force on the TMJ and the stress on the distal segment of the mandible. The miniplate can also resist the tensile stress more effectively. In addition, two miniplates with thinner sizes may have a similar biomechanical strength in the distal segment of the mandible as one thicker miniplate, and may therefore provide an alternative in clinical practice.
Data Availability
Data and materials are available from the corresponding author under at a reasonable request.
Code availability
Not applicable.
References
Cenzato, N., Nobili, A., & Maspero, C. (2021). Prevalence of dental malocclusions in different geographical areas: Scoping review. Dentistry Journal, 9(10), 117.
Hartlev, J., Godtfredsen, E., Andersen, N. T., & Jensen, T. (2014). Comparative study of skeletal stability between postoperative skeletal intermaxillary fixation and no skeletal fixation after bilateral sagittal split ramus osteotomy: An 18 months retrospective study. Journal of Oral & Maxillofacial Research, 5(1), e2.
Paunonen, J., Svedström-Oristo, A. L., Helminen, M., & Peltomäki, T. (2020). Quality of life several years after orthodontic-surgical treatment with bilateral sagittal split osteotomy. Acta Odontologica Scandinavica, 78(5), 358–361.
Verweij, J. P., Houppermans, P. N., Gooris, P., Mensink, G., & van Merkesteyn, J. R. (2016). Risk factors for common complications associated with bilateral sagittal split osteotomy: A literature review and meta-analysis. Journal of Cranio-Maxillofacial Surgery, 44(9), 1170–1180.
Sinha, S., Duong, T., Duy, T. D., Ko, E. C., Chen, Y. R., & Huang, C. (2022). Penetration of inferior alveolar nerve canal increased by bicortical fixation after bilateral sagittal split osteotomy in mandibular prognathism. International Journal of Oral and Maxillofacial Surgery, 51(2), 200–205.
Matsushita, Y., Nakakuki, K., Kosugi, M., Kurohara, K., & Harada, K. (2016). Does intraoral miniplate fixation have good postoperative stability after sagittal splitting ramus osteotomy? Comparison with intraoral bicortical screw fixation. Journal of Oral and Maxillofacial Surgery, 74(1), 181–189.
Kuhlefelt, M., Laine, P., Suominen-Taipale, L., Ingman, T., Lindqvist, C., & Thoren, H. (2010). Risk factors contributing to symptomatic miniplate removal: A retrospective study of 153 bilateral sagittal split osteotomy patients. International Journal of Oral and Maxillofacial Surgery, 39(5), 430–435.
Falter, B., Schepers, S., Vrielinck, L., Lambrichts, I., & Politis, C. (2011). Plate removal following orthognathic surgery. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 112(6), 737–743.
Theodossy, T., Jackson, O., Petrie, A., & Lloyd, T. (2006). Risk factors contributing to symptomatic plate removal following sagittal split osteotomy. International Journal of Oral and Maxillofacial Surgery, 35(7), 598–601.
Little, M., Langford, R. J., Bhanji, A., & Farr, D. (2015). Plate removal following orthognathic surgery. Journal of Cranio-Maxillofacial Surgery, 43(9), 1705–1709.
Lisiak-Myszke, M., Marciniak, D., Bieliński, M., Sobczak, H., Garbacewicz, Ł, & Drogoszewska, B. (2020). Application of finite element analysis in oral and maxillofacial surgery—A literature review. Materials, 13(14), 3063.
Atik, F., Atac, M., Ozkan, A., Kilinc, Y., & Arslan, M. (2016). Biomechanical analysis of titanium fixation plates and screws in sagittal split ramus osteotomies. Nigerian Journal of Clinical Practice, 19(1), 140–144.
Erkmen, E., Simşek, B., Yücel, E., & Kurt, A. (2005). Comparison of different fixation methods following sagittal split ramus osteotomies using three-dimensional finite elements analysis: Part 1: Advancement surgery-posterior loading. International Journal of Oral and Maxillofacial Surgery, 34(5), 551–558.
Sato, F., Asprino, L., Noritomi, P., Da Silva, J., & De Moraes, M. (2012). Comparison of five different fixation techniques of sagittal split ramus osteotomy using three-dimensional finite elements analysis. International Journal of Oral and Maxillofacial Surgery, 41(8), 934–941.
Chang, L. R., Chen, C. C., Jeng, S. F., Chen, Y. R., Hwang, L. C., & Lin, T. S. (2020). Investigation of a modified novel technique in bilateral sagittal splitting osteotomy fixation: Finite element analysis and in vitro biomechanical test. BioMed Research International, 2020, 8707389.
Oguz, Y., Uckan, S., Ozden, A. U., Uckan, E., & Eser, A. (2009). Stability of locking and conventional 2.0-mm miniplate/screw systems after sagittal split ramus osteotomy: Finite element analysis. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 108(2), 174–177.
Tamura, N., Takaki, T., Takano, N., & Shibahara, T. (2018). Three-dimensional finite element analysis of bone fixation in bilateral sagittal split ramus osteotomy using individual models. The Bulletin of Tokyo Dental College, 59(2), 67–78.
Dai, Z., Hou, M., Ma, W., Song, D. L., Zhang, C. X., & Zhou, W. Y. (2016). Evaluation of the transverse displacement of the proximal segment after bilateral sagittal split ramus osteotomy with different lingual split patterns and advancement amounts using the finite element method. Journal of Oral and Maxillofacial Surgery, 74(11), 2286.e1-2286.e11.
Maurer, P., Holweg, S., & Schubert, J. (1999). Finite-element-analysis of different screw-diameters in the sagittal split osteotomy of the mandible. Journal of Cranio-Maxillofacial Surgery, 27(6), 365–372.
Huang, H. L., Su, K. C., Fuh, L. J., Chen, M. Y., Wu, J., Tsai, M. T., & Hsu, J. T. (2015). Biomechanical analysis of a temporomandibular joint condylar prosthesis during various clenching tasks. Journal of Cranio-Maxillofacial Surgery, 43(7), 1194–1201.
Dal, P. (1961). Retromolar osteotomy for the correction of prognathism. Journal of Oral Surgery, 19, 42–47.
Ribeiro-Junior, P. D., Magro-Filho, O., Shastri, K. A., & Papageorge, M. B. (2010). In vitro biomechanical evaluation of the use of conventional and locking miniplate/screw systems for sagittal split ramus osteotomy. Journal of Oral and Maxillofacial Surgery, 68(4), 724–730.
Chang, Y.-H., Chan, M. Y., Hsu, J. T., Hsiao, H. Y., & Su, K. C. (2019). Biomechanical analysis of the forces exerted during different occlusion conditions following bilateral sagittal split osteotomy treatment for mandibular deficiency. Applied Bionics and Biomechanics, 2019, 4989013.
Korioth, T. W., & Hannam, A. G. (1994). Mandibular forces during simulated tooth clenching. Journal of Orofacial Pain, 8(2), 178–189.
Luo, D., Rong, Q., & Chen, Q. (2017). Finite-element design and optimization of a three-dimensional tetrahedral porous titanium scaffold for the reconstruction of mandibular defects. Medical Engineering & Physics, 47, 176–183.
Hijazi, L., Hejazi, W., Darwich, M. A., & Darwich, K. (2016). Finite element analysis of stress distribution on the mandible and condylar fracture osteosynthesis during various clenching tasks. Oral and Maxillofacial Surgery, 20(4), 359–367.
Reyneke, J. P., & Ferretti, C. (2002). Intraoperative diagnosis of condylar sag after bilateral sagittal split ramus osteotomy. British Journal of Oral and Maxillofacial Surgery, 40(4), 285–292.
Costa, F., Robiony, M., Toro, C., Sembronio, S., Polini, F., & Politi, M. (2008). Condylar positioning devices for orthognathic surgery: A literature review. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 106(2), 179–190.
Möhlhenrich, S. C., Winterhalder, P., Ooms, M., Heitzer, M., Kilic, K., Prescher, A., Hölzle, F., Danesh, G., & Modabber, A. (2021). Changes in the temporomandibular joint position depending on the sagittal osteotomy technique and extent of mandibular movement. International Journal of Oral and Maxillofacial Surgery, 50(3), 356–366.
Hirjak, D., Dvoranova, B., Reyneke, J. P., Machon, M., & Neff, A. (2020). Condylar position and mandibular function after bilateral sagittal split osteotomy. Bratislavske Lekarske Listy, 121(6), 379–385.
Bermell-Baviera, A., Bellot-Arcis, C., Montiel-Company, J., & Almerich-Silla, J. (2016). Effects of mandibular advancement surgery on the temporomandibular joint and muscular and articular adaptive changes—A systematic review. International Journal of Oral and Maxillofacial Surgery, 45(5), 545–552.
Hoffmannová, J., Foltán, R., Vlk, M., Klíma, K., Pavlíková, G., & Bulik, O. (2008). Factors affecting the stability of bilateral sagittal split osteotomy of a mandible. Prague Medical Report, 109(4), 286–297.
Champy, M., Loddé, J., Schmitt, R., Jaeger, J., & Muster, D. (1978). Mandibular osteosynthesis by miniature screwed plates via a buccal approach. Journal of Maxillofacial Surgery, 6, 14–21.
He, Y., Zhang, H., Qiao, J., Fu, X., Xu, S., Jin, Q., Liu, J., Chen, Y., Yu, B., & Niu, F. (2022). Biomechanical evaluation of seven fixation methods for sagittal split ramus osteotomy with four advancement levels by finite element analysis. Frontiers in Surgery, 9, 891747.
De Oliveira, L. B., Reis, J. M., Spin-Neto, R., Gabrielli, M. A., Oguz, Y., & Pereira-Filho, V. A. (2016). Mechanical evaluation of six techniques for stable fixation of the sagittal split osteotomy after counterclockwise mandibular advancement. The British Journal of Oral & Maxillofacial Surgery, 54(5), 573–578.
Kuik, K., Ho, J., de Ruiter, M., Klop, C., Kleverlaan, C. J., de Lange, J., & Hoekema, A. (2021). Stability of fixation methods in large mandibular advancements after sagittal split ramus osteotomy: An in vitro biomechanical study. The British Journal of Oral & Maxillofacial Surgery, 59(4), 466–471.
Sigua-Rodriguez, E. A., Caldas, R. A., Goulart, D. R., Hemerson de Moraes, P., Olate, S., Ricardo Barão, V. A., & Ricardo de Albergaria-Barbosa, J. (2019). Comparative evaluation of different fixation techniques for sagittal split ramus osteotomy in 10 mm advancements. Part two: Finite element analysis. Journal of Cranio-maxillofacial Surgery, 47(7), 1015–1019.
Chuong, C. J., Borotikar, B., Schwartz-Dabney, C., & Sinn, D. P. (2005). Mechanical characteristics of the mandible after bilateral sagittal split ramus osteotomy: Comparing 2 different fixation techniques. Journal of Oral and Maxillofacial Surgery, 63(1), 68–76.
Acknowledgements
We would like to thank the Ministry of Science and Technology of Taiwan (MOST 110-2221-E-075A-001), Taichung Veterans General Hospital/ HungKuang University Joint Research Program (TCVGH-HK1118003), Taichung Veterans General Hospital (TCVGH-1117315C) in Taiwan and the 3D Printing Research and Development Group of Taichung Veterans General Hospital for building the simulation computer model of this study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conception and design, BTT, CSC, KHL and CMH; methodology, YCY, CHW and KCS; data curation, YCY and KCS; manuscript writing, BTT and KCS. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tseng, BT., Yen, YC., Cheng, CS. et al. Biomechanical Effects of Different Miniplate Thicknesses and Fixation Methods Applied in BSSO Surgery Under Two Occlusal Conditions. J. Med. Biol. Eng. 42, 445–458 (2022). https://doi.org/10.1007/s40846-022-00733-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-022-00733-4