Abstract
Purpose
Physical fitness indicates favorable statuses of well-being and health and, more specifically, the ability to perform sports and daily activities. In the paper, we studied heart rate variability with electrocardiogram (ECG) signals under levels of exercise intensities for subjects with different grades of cardiopulmonary fitness.
Methods
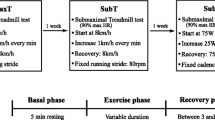
Based on the targeted maximum heart rate, three graded upright biking exercise levels were defined for the experiment: light, moderate, and vigorous. ECG signals were accessed under the rest, at three exercise intensity levels, and in their retrieval periods subsequently. The subjects were in the top 20%, middle, and bottom 20% groups of cardiopulmonary fitness norms from university freshman. Firstly, the major of heart rate variability (HRV) indices performed by spectral and time-domain analyses from collected ECG signals were explored. Statistical analysis was then conducted to identify physiological signal indices with significant differences.
Results
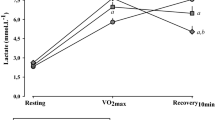
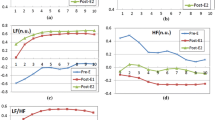
All appeared significant differences between the three groups in the frequency domain HRV indices, including high-frequency power (HF), total power (TP), normalized high-frequency power (nHF), normalized low-frequency power (nLF), and LF/HF. The time domain HRV parameters, meanwhile, did not exhibit significant differences among the three groups throughout the graded exercises and in the recover periods.
Conclusions
A multiple comparison test on the TP indicated significant differences in most between-group comparisons (except for between groups middle and bottom during moderate exercise, top and middle during recovery from moderate exercise, and middle and bottom during recovery from vigorous exercise). Significant differences were found in most between-group comparisons (except for between groups middle and bottom at rest and during recovery from light and medium exercise and between top and middle during recovery from vigorous exercise).




Similar content being viewed by others
References
Akselrod, S., Gordon, D., Ubel, F. A., Shannon, D. C., Barger, A. C., Cohen, R. J., et al. (1981). Power spectrum analysis of heart rate fluctuation: A quantitative probe of beat-to-beat cardiovascular control. Science,213(4504), 220–222.
Ahuja, N.D., Agarwal, A.K., Mahajan, N.M., Mehta, N.H., Kapadia, H.N., et al. (2003). GSR and HRV: Its application in clinical diagnosis. In: Proceedings of the 16th IEEE Symposium of Computer-Based Medical Systems, New York, USA, pp. 279–283.
Wolf, M. M., Varigos, G. A., Hunt, D., Sloman, J. G., et al. (1978). Sinus arrhythmia in acute myocardial infarction. Medical Journal of Australia,2(2), 52–53.
Hirsch, J. A., & Bishop, B. (1981). Respiratory sinus arrhythmia in humans: How breathing pattern modulates heart rate. American Journal of Physiology,241(4), H620–H629.
Vanderlei, L. C. M., Pastre, C. M., Hoshi, R. A., de Carvalho, T. D., de Godoy, M. F., et al. (2009). Basic notions of heart rate variability and its clinical applicability. Brazilian Journal of Cardiovascular Surgery,24(2), 205–217.
Kochiadakis, G. E., Lees, P. J., Kanoupakis, E. M., Igoumenidis, N. E., Manios, E. G., Vardas, P. E., et al. (1997). Spectral analysis of heart rate variability in the analysis of autonomic nervous system activity during tilt-table testing in patients with unexplained syncope (pp. 367–369). Lund, Sweden: Computers in Cardiology.
Hoyer, D., Pompe, B., Chon, K. H., Hardraht, H., Wicher, C., Zwiener, U., et al. (2005). Mutual information function assesses autonomic information flow of heart rate dynamics at different time scales. IEEE Transactions on Biomedical Engineering,52(4), 584–592.
Melillo, P., Jovic, A., De Luca, N., Pecchia, L., et al. (2015). Automatic classifier based on heart rate variability to identify fallers among hypertensive subjects. Healthcare Technology Letters,2(4), 89–94.
Zhu, Y., Yang, X., Wang, Z., Peng, Y., et al. (2014). An evaluating method for autonomic nerve activity by means of estimating the consistency of heart rate variability and QT variability. IEEE Transactions on Biomedical Engineering,61(3), 938–945.
Schiecke, K., Pester, B., Piper, D., Benninger, F., Feucht, M., Leistritz, L., et al. (2016). Nonlinear directed interactions between HRV and EEG activity in children with TLE. IEEE Transactions on Biomedical Engineering,63(12), 2497–2504.
Valenza, G., Nardelli, M., Lanata, A., Gentili, C., Bertschy, G., Kosel, M., et al. (2016). Predicting mood changes in bipolar disorder through heartbeat nonlinear dynamics. IEEE Journal of Biomedical and Health Informatics,20(4), 1034–1043.
Jung, S. J., Shin, H. S., Chung, W. Y., et al. (2014). Driver fatigue and drowsiness monitoring system with embedded electrocardiogram sensor on steering wheel. IET Intelligent Transport Systems,8(1), 43–50.
Puig, J., Freitas, J., Carvalho, M. J., Puga, N., Ramos, J., Fernandes, P., et al. (1993). Spectral analysis of heart rate variability in athletes. Journal of Sports Medicine and Physical Fitness,33(1), 44–48.
Malik, M. (1996). Task force of the european society of cardiology and the North American Society of Pacing and Electrophysiology. Circulation,93(5), 1043–1065.
La Rovere, M. T., Bigger, J. T., Jr., Marcus, F. I., Mortara, A., Schwartz, P. J., et al. (1998). Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. Lancet,351(9101), 478–484.
Liu, P. Y., Tsai, W. C., Lin, L. J., Li, Y. H., Chao, T. H., Tsai, L. M., et al. (2003). Time domain heart rate variability as a predictor of long term prognosis after acute myocardial infarction. Journal of the Formosan Medical Association,102(7), 474–479.
Janssen, M. J., de Bie, J., Swenne, C. A., Oudhof, J., et al. (1993). Supine and standing sympathovagal balance in athletes and controls. European Journal of Applied Physiology,67(2), 164–167.
Macor, F., Fagard, R., Amery, A., et al. (1996). Power spectral-analysis of RR interval and blood-pressure short-term variability at rest and during dynamic exercise: Comparison between cyclists and controls. International Journal of Sports Medicine,17(3), 175–181.
Morris, J. N., Everitt, M. G., Pollard, R., Chave, S. P., Semmence, A. M., et al. (1980). Vigorous exercise in leisure-time: Protection against coronary heart disease. Lancet,2(8206), 1207–1210.
De-Meersman, R. E. (1992). Respiratory sinus arrhythmia alteration following training in endurance athletes. European Journal of Applied Physiology and Occupational Physiology,64(5), 434–436.
Da Silva, V. P., de Oliveira, N. A., Silveira, H., Mello, R. G. T., Deslandes, A. C., et al. (2015). Heart rate variability indexes as a marker of chronic adaptation in athletes: A systematic review. Annals of Noninvasive Electrocardiology,20(2), 108–118.
Ignico, A. A., & Mahon, A. D. (1995). The effects of a physical fitness program on low-fit children. Research Quarterly for Exercise and Sport,66(1), 85–90.
Marshall, S. J., Sarkin, J. A., Sallis, J. F., McKenzie, T. L., et al. (1998). Tracking of health-related fitness components in youth ages 9 to 12. Medicine & Science in Sports & Exercise,30(6), 910–916.
Boreham, C., Twisk, J., Neville, C., Savage, M., Murray, L., Gallagher, A., et al. (2002). Associations between physical fitness and activity patterns during adolescence and cardiovascular risk factors in young adulthood: The Northern Ireland Young Hearts Project. International Journal of Sports Medicine,23, S22–26.
Riebe, D., Ehrman, J. K., Liguori, G., Magal, M., et al. (2018). acsm’s guidelines for exercise testing and prescription (10th ed.). Philadelphia: Lippincott Williams & Wilkins.
Fox, S. M., 3rd, Naughton, J. P., Haskell, W. L., et al. (1971). Physical activity and the prevention of coronary heart disease. Annals of Clinical Research,3(6), 404–432.
Powers, S. K., & Howley, E. T. (2018). Exercise physiology: Theory and application to fitness and performance (10th ed.). New York: McGraw-Hill Education.
Pan, J., & Tompkins, W. J. (1985). A real-time QRS detection algorithm. IEEE Transactions on Biomedical Engineering,32(3), 230–236.
Shaffer, F., & Ginsberg, J. P. (2017). An overview of heart rate variability metrics and norms. Frontiers in Public Health,5, 258.
Bulica, M., & Dan Moga, V. (1999). Frequency domain methods for measurement of heart rate variability. Studies in Health Technology and Informatics,68, 359–364.
Middleton, N., & De Vito, G. (2005). Cardiovascular autonomic control in endurance-trained and sedentary young women. Clinical Physiology and Functional Imaging,25(2), 83–89.
Moak, J. P., Goldstein, D. S., Eldadah, B. A., Saleem, A., Holmes, C., Pechnik, S., et al. (2007). Supine low-frequency power of heart rate variability reflects baroreflex function, not cardiac sympathetic innervation. Heart Rhythm,4(12), 1523–1529.
Buchheit, M., & Gindre, C. (2006). Cardiac parasympathetic regulation: Respective associations with cardiorespiratory fitness and training load. American Journal of Physiology: Heart and Circulatory Physiology,291(1), H451–H458.
Ishida, R., & Okada, M. (1997). Spectrum analysis of heart rate variability for the assessment of training effects. Rinsho Byori,45(7), 685–688.
Shin, K., Minamitani, H., Onishi, S., Yamazaki, H., Lee, M., et al. (1997). Autonomic differences between athletes and nonathletes: Spectral analysis approach. Medicine and Science in Sports and Exercise,29(11), 1482–1490.
Lin, C. H., & Huang, H. J. (2010). The effect of stationary cycling on heart rate variability in high school elite basketball players. Physical Education Journal of NPTUE,13, 302–311.
Acknowledgements
This study was supported by the Ministry of Science and Technology (Grant MOST 105-2221-E-035-095-MY2), Taiwan. This manuscript was edited by Wallace Academic Editing, Taiwan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, CK., Lin, SL., Huang, CY. et al. Statistical Analysis on Heart Rate Variability for Graded Cardiopulmonary Groups with Different Exercise Intensities. J. Med. Biol. Eng. 40, 440–450 (2020). https://doi.org/10.1007/s40846-020-00514-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-020-00514-x