Abstract
Background
Intervertebral fusion removes a considerable region of lumbar ligaments and muscles and increases degenerative diseases in adjacent segments. Therefore, an interspinous fixation device must be developed to overcome these drawbacks. The purpose of the present study is to design a lumbar spine interspinous fixation device that minimizes both tissue removal during interspinous fixation surgery and degenerative changes of adjacent lumbar segments after the surgery.
Methods
The lumbar interspinous fixation device was designed by employing spike and ratchet structures in the device fixation part to minimize the removal of soft tissue during interspinous fixation surgery and to reduce the stress concentration after the surgery. The part connecting two spinous processes was designed as spring element to allowing normal lumbar behavior after the surgery. Finite element analysis was performed to design spring elements, confirm the structural stability of the fixation device, and compute the intervertebral disc pressure and flexion–extension motions of intact and defect lumbar vertebrae models that were validated in this study.
Results
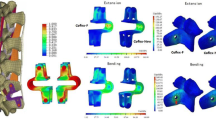
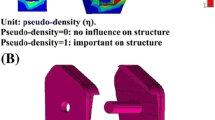
The structural stability of the currently designed interspinous fixation device was confirmed. Under physiological loading conditions, the maximum displacement is 0.4 mm and the maximum stress is 173.5 MPa under the maximum load of 250 N, which accounts for 18.3% of the yield strength of the LIFD material (950 MPa). When the interspinous fixation device was inserted, the intervertebral disc pressure was reduced by 80–92% compared with the defect model that mimics intervertebral fusion. Both a significant reduction in the flexion motion (from 10.7° to 6.0°) up to the normal behavior and a minimal reduction in the extension motion (from − 4.6° to − 3.1°) were achieved, which is consistent with the main role of the LIFD reported in the literature.
Conclusions
The interspinous fixation device designed in this work, which is structurally stable and can minimize the tissue removal during interspinous fixation surgery, can reduce the intervertebral disc pressure and maintain the normal lumbar behavior. Therefore, the device can minimize degenerative diseases in adjacent lumbar segments of lumbar vertebrae after the surgery.









Similar content being viewed by others
References
Kaner, T., & Ozer, A. F. (2013). Dynamic stabilization for challenging lumbar degenerative diseases of the spine: A review of the literature. Advances in Orthopedics,2013, 753470. https://doi.org/10.1155/2013/753470.
Kaner, T., Sasani, M., Oktenoglu, T., & Ozer, A. F. (2010). Dynamic stabilization of the spine: A new classification system. Turkish Neurosurgery,20(2), 205–215.
Szpalski, M., Gunzburg, R., & Pope, M. H. (1999). Dynamic neutralization: A new concept for restabilization of the spine. Lumbar segmental instability (pp. 233–240). Philadelphia, PA: Lippincott Williams & Wilkins.
Yue, J. J. (2008). Classification of spine arthroplasty devices. In J. J. Yue, R. Bertagnoli, P. C. McAfee, & H. S. An (Eds.), Motion preservation surgery of the spine: Advanced techniques and controversies (pp. 21–35). Philadelphia, PA: Saunders/Elsevier.
Gardner, A., & Pande, K. C. (2002). Graf ligamentoplasty: A 7-year follow-up. European Spine Journal,11, S157–S163. https://doi.org/10.1007/s00586-002-0436-4.
Kanayama, M., Hashimoto, T., & Shigenobu, K. (2005). Rationale, biomechanics, and surgical indications for graf ligamentoplasty. Orthopedic Clinics of North America,36(3), 373–377. https://doi.org/10.1016/j.ocl.2005.02.013.
Kanayama, M., Hashimoto, T., Shigenobu, K., Harada, M., Oha, F., Ohkoshi, Y., et al. (2001). Adjacent-segment morbidity after Graf ligamentoplasty compared with posterolateral lumbar fusion. Journal of Neurosurgery,95(1), 5–10. https://doi.org/10.3171/spi.2001.95.1.0005.
Onda, A., Otani, K., Konno, S., & Kikuchi, S. (2006). Mid-term and long-term follow-up data after placement of the Graf stabilization system for lumbar degenerative disorders. Journal of Neurosurgery-Spine,5(1), 26–32. https://doi.org/10.3171/spi.2006.5.1.26.
Kanayama, M., Hashimoto, T., Shigenobu, K., Togawa, D., & Oha, F. (2007). A minimum 10-year follow-up of posterior dynamic stabilization using Graf artificial ligament. Spine,32(18), 1992–1996. https://doi.org/10.1097/BRS.0b013e318133faae.
Sengupta, D. K. (2005). Dynamic stabilization devices in the treatment of low back pain. Neurology India,53(4), 466–474.
Senegas, J. (2002). Mechanical supplementation by non-rigid fixation in degenerative intervertebral lumbar segments: The Wallis system. European Spine Journal,11, S164–S169. https://doi.org/10.1007/s00586-002-0423-9.
Kim, D. H., Cammisa, F. P., & Fessler, R. G. (2006). Historical review of Spinal artroplasty and dynamic stabilization. Dynamic reconstruction of the spine (pp. 3–15). New York: Thieme.
Kabir, S. M. R., Gupta, S. R., & Casey, A. T. H. (2010). Lumbar interspinous spacers: A systematic review of clinical and biomechanical evidence. Spine,35(25), E1499–E1506. https://doi.org/10.1097/BRS.0b013e3181e9af93.
Hyo-Joo Lim, M. D., Sung-Woo Roh, M. D., Sang-Ryong Jeon, M. D., & Seung-Chul Rhim, M. D. (2004). Early experience with interspinous U in the management of the degenerative lumbar disease. Korean Journal of Spine,1(4), 456–462.
Chen, Y. H., Xu, D., Xu, H. Z., Chi, Y. L., Wang, X. Y., & Huang, Q. S. (2009). Coflex interspinous dynamic internal fixation for the treatment of degenerative lumbar spinal stenosis. Zhongguo Gu Shang,22(12), 902–905.
Stromqvist, B. (1993). Postlaminectomy problems with reference to spinal-fusion. Acta Orthopaedica Scandinavica,64, 87–89.
Samani, J. S. (2002). Study of a semi-rigid interspinous U fixation system. Spinal Surgery, Child Orthopaedics, p. 1707.
Niinomi, M. (1998). Mechanical properties of biomedical titanium alloys. Materials Science and Engineering A: Structural Materials Properties Microstructure and Processing,243(1–2), 231–236.
Heo, S., Son, K., Park, J. H., & Lee, S. J. (2006). Biomechanical analysis of lumbar interspinous process fixators. Journal of the Korean Society of Precision Engineering,23(3), 195–202.
Shirazi-Adl, A., Ahmed, A. M., & Shrivastava, S. C. (1986). A finite element study of a lumbar motion segment subjected to pure sagittal plane moments. The Journal of Biomechanics,19(4), 331–350.
Sharma, M., Langrana, N. A., & Rodriguez, J. (1995). Role of ligaments and facets in lumbar spinal stability. Spine (Phila Pa 1976),20(8), 887–900.
Kim, Y., & Kim, T. W. (2010). Finite element analysis of the effects of pedicle screw fixation nut loosening on lumbar interbody fusion based on the elasto-plateau plasticity of bone characteristics. Spine,35(6), 599–606.
Zheng, J., Yang, Y. H., Lou, S. L., Zhang, D. S., & Liao, S. H. (2015). Construction and validation of a three-dimensional finite element model of degenerative scoliosis. Journal of Orthopaedic Surgery and Research,10, 189.
He, L., Zhang, M. C., Feng, F., Pang, M., Xie, P. G., Chen, R. Q., et al. (2016). Stress distribution over lumbosacral vertebrae and axial transsacral rod after axial lumbar interbody fusion (AxiaLIF): Finite element analysis. International Journal of Clinical and Experimental Medicine,9(7), 13372–13383.
Wang, K., Jiang, C., Wang, L., Wang, H., & Niu, W. (2018). The biomechanical influence of anterior vertebral body osteophytes on the lumbar spine: A finite element study. The Spine Journal,18(12), 2288–2296. https://doi.org/10.1016/j.spinee.2018.07.001.
Markolf, K. L., & Morris, J. M. (1974). The structural components of the intervertebral disc. A study of their contributions to the ability of the disc to withstand compressive forces. The Journal of Bone and Joint Surgery,56(4), 675–687.
Goel, V. K., & Kim, Y. E. (1989). Effects of injury on the spinal motion segment mechanics in the axial-compression mode. Clinical Biomechanics,4(3), 161–167. https://doi.org/10.1016/0268-0033(89)90020-X.
Renner, S. M., Natarajan, R. N., Patwardhan, A. G., Havey, R. M., Voronov, L. I., Guo, B. Y., et al. (2007). Novel model to analyze the effect of a large compressive follower pre-load on range of motions in a lumbar spine. Journal of Biomechanics,40(6), 1326–1332.
Rohlmann, A., Neller, S., Claes, L., Bergmann, G., & Wilke, H. J. (2001). Influence of a follower load on intradiscal pressure and intersegmental rotation of the lumbar spine. Spine (Phila Pa 1976),26(24), E557–E561.
Grosland, N. M. (1998). Spinal adaptations in response to interbody fusion systems: A theoretical investigation. Iowa: The University of Iowa.
Freudiger, S., Dubois, G., & Lorrain, M. (1999). Dynamic neutralisation of the lumbar spine confirmed on a new lumbar spine simulator in vitro. Archives of Orthopaedic and Trauma Surgery,119(3–4), 127–132. https://doi.org/10.1007/s004020050375.
Nachemson, A. (1960). Lumbar Intradiscal Pressure: Experimental studies on post-mortem material. Acta Orthopaedica Scandinavica,43, 1–104. https://doi.org/10.3109/ort.1960.31.suppl-43.01.
Lv, Q. B., Gao, X., Pan, X. X., Jin, H. M., Lou, X. T., Li, S. M., et al. (2018). Biomechanical properties of novel transpedicular transdiscal screw fixation with interbody arthrodesis technique in lumbar spine: A finite element study. Journal of Orthopaedic Translation,15, 50–58.
Park, W. M., Kim, C. H., Kim, Y. H., Chung, C. K., & Jahng, T. A. (2015). The change of sagittal alignment of the lumbar spine after dynesys stabilization and proposal of a refinement. Journal of Korean Neurosurgical Society,58(1), 43–49.
Ahn, Y. H., Chen, W. M., Lee, K. Y., Park, K. W., & Lee, S. J. (2008). Comparison of the load-sharing characteristics between pedicle-based dynamic and rigid rod devices. Biomedical Materials,3(4), 044101.
Zander, T., Rohlmann, A., & Bergmann, G. (2004). Influence of ligament stiffness on the mechanical behavior of a functional spinal unit. Journal of Biomechanics,37(7), 1107–1111.
Liu, C., Kamara, A., & Yan, Y. H. (2018). Investigation into the biomechanics of lumbar spine micro-dynamic pedicle screw. BMC Musculoskeletal Disorders,19(1), 231.
Schultz, A. B., Warwick, D. N., Berkson, M. H., & Nachemson, A. L. (1979). Mechanical-properties of human lumbar spine motion segments. 1. Responses in flexion, extension, lateral bending, and torsion. Journal of Biomechanical Engineering-Transactions of the ASME,101(1), 46–52.
Yamamoto, I., Panjabi, M. M., Crisco, T., & Oxland, T. (1989). 3-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine,14(11), 1256–1260. https://doi.org/10.1097/00007632-198911000-00020.
Tencer, A. F., Ahmed, A. M., & Burke, D. L. (1982). Some static mechanical-properties of the lumbar intervertebral joint, intact and injured. Journal of Biomechanical Engineering-Transactions of the ASME,104(3), 193–201.
Ranu, H. S., Denton, R. A., & King, A. I. (1979). Pressure distribution under an intervertebral-Disk—experimental-study. Journal of Biomechanics,12(10), 807–812.
Nachemson, A. L. (1981). Disk pressure measurements. Spine,6(1), 93–97. https://doi.org/10.1097/00007632-198101000-00020.
Shirazi-Adl, S. A., Shrivastava, S. C., & Ahmed, A. M. (1984). Stress analysis of the lumbar disc-body unit in compression: A three-dimensional nonlinear finite element study. Spine (Phila Pa 1976),9(2), 120–134.
Park, J. H., Heo, S., Son, K., & Lee, S. J. (2006). Biomechanical analysis of lumbar interspinous process fixators and design of miniaturization and advanced flexibility. Transactions of the Korean Society of Mechanical Engineers - A,30(12), 1509–1517.
Meir, A., McNally, D. S., Fairbank, J. C., Jones, D., & Urban, J. P. (2008). The internal pressure and stress environment of the scoliotic intervertebral disc—a review. Proceedings of the Institution of Mechanical Engineers, Part H,222(2), 209–219. https://doi.org/10.1243/09544119JEIM303.
Hutton, W. C., Elmer, W. A., Bryce, L. M., Kozlowska, E. E., Boden, S. D., & Kozlowski, M. (2001). Do the intervertebral disc cells respond to different levels of hydrostatic pressure? Clinical Biomechanics (Bristol, Avon),16(9), 728–734.
Filippiadis, D. K., Mazioti, A., Papakonstantinou, O., Brountzos, E., Gouliamos, A., Kelekis, N., et al. (2012). Quantitative discomanometry: Correlation of intradiscal pressure values to pain reduction in patients with intervertebral disc herniation treated with percutaneous, minimally invasive, image-guided techniques. Cardiovascular and Interventional Radiology,35(5), 1145–1153. https://doi.org/10.1007/s00270-011-0255-2.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP; No. NRF-2016R1A2B4012561, NRF-2013R1A1A2062436).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Heo, M., Yun, J., Park, SH. et al. Design of a Lumbar Interspinous Fixation Device for Minimally Invasive Surgery and Spine Motion Stabilization. J. Med. Biol. Eng. 40, 1–10 (2020). https://doi.org/10.1007/s40846-019-00485-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-019-00485-8