Abstract
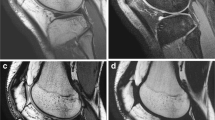
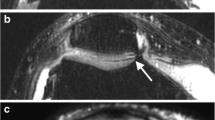
The aim of this present study is to evaluate the reduction of susceptibility artifacts by increasing bandwidth (BW) and echo train length (ETL) in proton density turbo spin echo (PD TSE) sequences with and without fat saturation (FS) and in turbo inversion recovery magnitude (TIRM) sequences. We compared: (1) TIRM coronal (COR) with TIRM COR with high (H) BW and Long ETL; (2) PD TSE sagittal (SAG) FS with the PD TSE SAG FS with (H) BW; (3) PD TSE SAG with PD TSE SAG with (H) BW; (4) PD TSE SAG with PD TSE SAG with (H) BW and Long ETL. A quantitative analysis measured the extent of the susceptibility artifacts. A qualitative analysis evaluated the susceptibility artifacts, image distortion and effectiveness of fat suppression. The depiction of cartilage, menisci, muscles, tendons and bone marrow were also qualitatively analyzed. In the quantitative analysis, modified TIRM appears superior. In the qualitative analysis, the modified TIRM appears superior in 8/10 characteristics. The modified PD TSE FS is superior to the conventional regarding the susceptibility artifacts, image distortion and the depiction of bone marrow and cartilage and fat saturation. The modified PD TSE with (H) BW is found to be superior to the conventional PD TSE only in cartilage. In these sequences, when ETL was increased there were significant differences in four characteristics (ghost artifacts, cartilage, menisci and muscles). TIRM sequences with an increased BW and ETL are proposed to be used in daily clinical practice.



Similar content being viewed by others
References
Lin, E. (2010). Magnetic resonance imaging of the knee: Clinical significance of common findings. Current Problems in Diagnostic Radiology, 39, 152–159.
Koch, K. M., Hargreaves, B. A., Pauly, K. B., Chen, W., Gold, G. E., & King, K. F. (2010). Magnetic resonance imaging near metal implants. Journal of Magnetic Resonance Imaging, 32, 773–787.
Hargreaves, B. A., Worters, P. W., Pauly, K. B., Pauly, J. M., Koch, K. M., & Gold, G. E. (2011). Metal-induced artifacts in MRI. American Journal of Roentgenology, 197, 547–555.
Simmons, A., Tofts, P. S., Barker, G. J., & Arridge, S. R. (1994). Sources of intensity nonuniformity in spin echo images at 1.5T. Magnetic Resonance in Medicine, 32, 121–128.
Beuf, O., Briguet, A., Lissac, M., & Davis, R. (1996). Magnetic resonance imaging for the determination of magnetic susceptibility of materials. Journal of Magnetic Resonance Series B, 112, 111–118.
Bakker, C. J., Bhagwandien, R., Moerland, M. A., & Ramos, L. M. (1994). Simulation of susceptibility artifacts in 2D and 3D Fourier transform spin-echo and gradient-echo magnetic resonance imaging. Magnetic Resonance Imaging, 12, 767–774.
Bakker, C. J., Moerland, M. A., Bhagwandien, R., & Beersma, R. (1992). Analysis of machine-dependent and object-induced geometric distortion in 2DFT MR imaging. Magnetic Resonance Imaging, 10, 597–608.
Schenck, J. F. (1996). The role of magnetic susceptibility in magnetic resonance imaging: MRI magnetic compatibility of the first and second kinds. Medical Physics, 23, 815–850.
Ludeke, K. M., Roschmann, P., & Tischler, R. (1985). Susceptibility artefacts in NMR imaging. Magnetic Resonance Imaging, 3, 329–343.
Escobedo, E. M., Hunter, J. C., Zink-Brody, G. C., Wilson, A. J., Harrison, S. D., & Fisher, D. J. (1996). Usefulness of turbo spin-echo MR imaging in the evaluation of meniscal tears: Comparison with a conventional spin-echo sequence. American Journal of Roentgenology, 167, 1223–1227.
Ha, T. P., Li, K. C., Beaulieu, C. F., Bergman, G., Ch’en, I. Y., Eller, D. J., et al. (1998). Anterior Cruciate Ligament injury: Fast spin-echo MR imaging with arthroscopic correlation in 217 examinations. American Journal of Roentgenology, 170, 1215–1219.
Bredella, M. A., Tirman, P. F., Wischer, T. K., Belzer, J., Taylor, A., & Genant, H. K. (2000). Reactive synovitis of the knee joint: MR imaging appearance with arthroscopic correlation. Skeletal Radiology, 29, 577–582.
Jansson, K. A., Karjalainen, P. T., Harilainen, A., Sandelin, J., Soila, K., Tallroth, K., et al. (2001). MRI of anterior cruciate ligament repair with patellar and hamstring tendon autografts. Skeletal Radiology, 30, 8–14.
Lee, J. H., Singh, T. T., & Bolton, G. (2002). Axial fat-saturated FSE imaging of knee: Appearance of meniscal tears. Skeletal Radiology, 31, 384–395.
Lee, M. J., Kim, S., Lee, S. A., Song, H. T., Huh, Y. M., Kim, D. H., et al. (2007). Overcoming artifacts from metallic orthopedic implants at high-field-strength MR imaging and multidetector CT. RadioGraphics, 27, 791–803.
Viano, A. M., Gronemeyer, S. A., Haliloglu, M., & Hoffer, F. A. (2000). Improved MR imaging for patients with metallic implants. Magnetic Resonance Imaging, 18, 287–295.
White, L. M., Kim, J. K., Mehta, M., Merchant, N., Schweitzer, M. E., Morrison, W. B., et al. (2000). Complications of total hip arthroplasty: MR imaging-initial experience. Radiology, 215, 254–262.
Olsen, R. V., Munk, P. L., Lee, M. J., Janzen, D. L., MacKay, A. L., Xiang, Q. S., et al. (2000). Metal artifact reduction sequence: Early clinical applications. Radiographics, 20, 699–712.
Chang, S. D., Lee, M. J., Munk, P. L., Janzen, D. L., MacKay, A., & Xiang, Q. S. (2001). MRI of spinal hardware: Comparison of conventional T1-weighted sequence with a new metal artifact reduction sequence. Skeletal Radiology, 30, 213–218.
Stradiotti, P., Curti, A., Castellazzi, G., & Zerbi, A. (2009). Metal related artifacts in instrumented spine. Techniques for reducing artifacts in CT and MRI: State of the art. European Spine Journal, 18, 102–108.
Petersilge, C. A., Lewin, J. S., Duerk, J. L., Yoo, J. U., & Ghaneyem, A. J. (1996). Optimizing imaging parameters for MR evaluation of the spine with titanium pedicle screws. American Journal of Roentgenology, 166, 1213–1218.
Kaur, P., Kumaran, S. S., Tripathi, R. P., Khushu, S., & Kaushik, S. (2007). Protocol error artifacts in MRI: Sources and remedies revisited. Radiography, 13, 291–306.
White, L. M., & Buckwalter, K. A. (2002). Technical considerations: CT and MR imaging in the postoperative orthopedic patient. Seminars in Musculoskeletal Radiology, 6, 5–17.
Kurtz, S., Ong, K., Lau, E., Mowat, F., & Halpern, M. (2007). Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. Journal of Bone and Joint Surgery. American Volume, 89, 780–785.
Prodromos, C. C., Han, Y., Rogowski, J., Joyce, B., & Shi, K. (2007). A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy, 23, 1320–1325.
Potter, H. G., Nestor, B. J., Sofka, C. M., Ho, S. T., Peters, L. E., & Salvati, E. A. (2004). Magnetic resonance imaging after total hip arthroplasty: Evaluation of periprosthetic soft tissue. Journal of Bone and Joint Surgery. American Volume, 86, 1947–1954.
Lu, W., Pauly, K. B., Gold, G. E., Pauly, J. M., & Hargreaves, B. A. (2009). SEMAC: slice encoding for metal artifact correction in MRI. Magnetic Resonance in Medicine, 62, 66–76.
Suh, J. S., Jeong, E. K., Shin, K. H., Cho, J. H., Na, J. B., Kim, D. H., et al. (1998). Minimizing artifacts caused by metallic implants at MR imaging: Experimental and clinical studies. American Journal of Roentgenology, 171, 1207–1213.
Tartaglino, L. M., Flanders, A. E., Vinitski, S., & Friedman, D. P. (1994). Metallic artifacts on MR images of the post-operative spine: Reduction with fast spin-echo techniques. Radiology, 190, 565–569.
Delfaut, E. M., Beltran, J., Johnson, G., Rousseau, J., Marchandise, X., & Cotten, A. (1999). Fat suppression in MR imaging: Techniques and pitfalls. Radiographics, 19, 373–382.
Deely, D. M., & Schweitzer, M. E. (1997). MR imaging of bone marrow disorders. Radiologic Clinics of North America, 35, 193–212.
Steiner, R. M., Mitchell, D. G., Rao, V. M., & Schweitzer, M. E. (1993). Magnetic resonance imaging of diffuse bone marrow disease. Radiologic Clinics of North America, 31, 383–409.
Eustace, S., Keogh, C., Blake, M., Ward, R. J., Oder, P. D., & Dimasi, M. (2001). MR imaging of bone oedema: Mechanisms and interpretation. Clinical Radiology, 56, 4–12.
Ulbrich, E. J., Sutter, R., Aguiar, R. F., Nittka, M., & Pfirrmann, C. W. (2012). STIR sequence with increased receiver bandwidth of the inversion pulse for reduction of metallic artifacts. American Journal of Roentgenology, 199, 735–742.
Lavdas, E., Mavroidis, P., Hatzigeorgiou, V., Roka, V., Arikidis, N., Oikonomou, G., et al. (2012). Elimination of motion and pulsation artifacts using BLADE sequences in knee MR imaging. Magnetic Resonance Imaging, 30, 1099–1110.
Yoshioka, H., Stevens, K., Hargreaves, B. A., Steines, D., Genovese, M., Dillingham, M. F., et al. (2004). Magnetic resonance imaging of articular cartilage of the knee: Comparison between fat suppressed threedimensional SPGR imaging, fat -suppressed FSE imaging, and fat suppressed three-dimensional DEFT imaging, and correlation with arthroscopy. Journal of Magnetic Resonance Imaging, 20, 857–864.
Lavdas, E., Topalzikis, T., Mavroidis, P., Kyriakis, I., Roka, V., Kostopoulos, S., et al. (2013). Comparison of PD BLADE with fat saturation (FS), PD FS and T2 3D DESS with water excitation (WE) in detecting articular knee cartilage defects. Magnetic Resonance Imaging, 31, 1255–1262.
Lee, Y., Han, Y., & Park, H. (2014). A new susceptibility-weighted image reconstruction method for the reduction of background phase artifacts. Magnetic Resonance in Medicine, 71, 1324–1335.
Kaushik, S. S., Karr, R., Runquist, M., Marszalkowski, C., Sharma, A., Rand, S. D., et al. (2017). Quantifying metal-induced susceptibility artifacts of the instrumented spine at 1.5T using fast-spin echo and 3D-multispectral MRI. Journal of Magnetic Resonance Imaging, 45, 51–58.
Acknowledgements
The authors would like to thank radiographer Ioannis Kaffes and Anna Vlachopoulou for their contribution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mavroidis, P., Boci, N., Kostopoulos, S. et al. Investigation of the Possibility to Reduce Susceptibility Artifacts in MRI Knee Examination. J. Med. Biol. Eng. 37, 644–652 (2017). https://doi.org/10.1007/s40846-017-0260-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-017-0260-2