Abstract
Background
The efficacy and safety of golimumab in elderly patients with renal dysfunction are not well evaluated due to the exclusion criteria of clinical trials.
Objective
To assess the persistence and safety of golimumab in elderly rheumatoid arthritis patients with renal dysfunction.
Patients and Methods
In this retrospective observational study, we used Japan's nationwide electronic medical records and claims database to identify patients aged 65 years and older who were newly prescribed golimumab for rheumatoid arthritis between July 2011 and June 2018. Patients were divided into three groups according to estimated glomerular filtration rate (eGFR; high, ≥ 90; moderate, ≥ 60, < 90; low, ≥ 30, < 60), and the persistence of golimumab and adverse events were compared between the groups.
Results
A total of 423 patients met the eligibility criteria. At 6 months, the persistence rates of golimumab were 62.4%, 63.7% and 67.0% in the high, moderate and low eGFR groups, respectively. In Cox proportional hazards regression analysis, baseline eGFR was not associated with golimumab persistence or adverse events, but concomitant methotrexate and low baseline C-reactive protein (CRP) were associated with longer golimumab persistence.
Conclusion
Reduced renal function was not associated with continuation of golimumab or incidence of adverse events, suggesting that the persistence of golimumab therapy in patients with rheumatoid arthritis is independent of the baseline level of renal function. On the other hand, concomitant use of methotrexate and low baseline CRP levels were suggested as factors that may affect the persistence of golimumab treatment.
Similar content being viewed by others
Persistence and adverse events of golimumab in elderly rheumatoid arthritis patients with renal dysfunction are not well known in real-world setting. |
Using an electronic medical records and claim database in Japan, the persistence of golimumab were similar among the high (high, ≥ 90), moderate (moderate, ≥ 60, < 90) and low (low, ≥ 30, < 60) estimated glomerular filtration rate (eGFR) groups. |
The incidence of adverse events were similar among the high, moderate and low eGFR groups. |
1 Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory autoimmune disease that causes progressive joint destruction. Overproduction of cytokines, including tumor necrosis factor-α (TNF-α) and interleukin-6, largely contributes to the cartilage deterioration and bone destruction seen in the disease [1]. To manage RA, methotrexate (MTX) is routinely used as a first-line therapy, but patients who fail to respond adequately to MTX are often prescribed biologics [2, 3]. Biologics include TNF-α inhibitors (TNFi), which are the most commonly used drug therapies [4, 5]. Besides a good initial response to TNFi, tolerability and long-term drug use are also important for disease control in RA.
Findings on the persistence rate of biologics in elderly patients with RA compared with younger patients have been inconsistent, with some reports showing lower persistence [6, 7], others showing no difference [8,9,10], and still others showing higher persistence [11]. Research has shown that the proportion of patients with renal dysfunction increases with age and that renal dysfunction increases the incidence of various adverse events (AEs) in RA including infections [12]. Because the occurrence of AEs is one of the main reasons for discontinuation of biologics, the increased incidence of AEs in elderly patients with impaired renal function may have an impact on the persistence of these agents in this age group.
Patients with renal dysfunction are usually excluded from clinical trials for RA. Therefore, it is important to analyze real-world data when examining the impact of renal function on the persistence rate of biologics. A previous single-center study on patients with RA reported no significant difference in persistence rates of biologics between two groups of patients classified according to renal function [13]. However, the study did not limit its analysis to the elderly, so it remains unclear to what extent renal function affects the persistence rate of biologics and the rate of AEs in the elderly patients with RA.
The recently published Japanese practice guideline suggests that there is still insufficient evidence on the persistence and safety of TNFi in elderly patients with renal dysfunction [14], supporting the need for further research in this area.
Golimumab (GLM) is a fully human monoclonal TNFi that targets a unique TNF-α epitope [15]. It has been approved for treatment of patients with active RA in many countries. In Japan, two GLM doses (50 and 100 mg) can be administered subcutaneously once every 4 weeks for RA treatment. A previous study suggested that GLM may be better tolerated than other TNFi in elderly patients with RA [11]. However, the previous study used only claim-based data and did not assess renal condition, so it remains unclear whether GLM is a tolerable option in elderly patients with RA and renal dysfunction. Therefore, in this study, we evaluated the association between continuous GLM persistence and renal function and the occurrence of AEs in elderly patients with RA by using a large real-world database containing electronic medical records (EMR) and claims.
2 Material and Methods
2.1 Study Design
This was a nationwide, multicenter, cohort study of data on elderly patients with RA in Japan. Patients were identified in a Japanese database of EMR and claims data (called the RWD database [RWD-DB]).
2.2 Data Source
We used the commercially available medical database provided by the Health, Clinic, and Education Information Evaluation Institute (Kyoto, Japan). The RWD-DB includes EMR, claims data, and discharge data from 188 hospitals that cover 16% of the total population of Japan [16, 17]. The relational data tables in the RWD-DB are shown in Online Resource 1. The database did not contain the reasons of GLM discontinuation (e.g. primary response failure, secondary response failure, or adverse events of the drug). The dataset for this study was extracted from the RWD-DB on October 11, 2020. The inclusion criterion was a definitive diagnosis of RA based on the International Statistical Classification of Disease and Related Health Problems, 10th revision (ICD-10) (Online Resource 2).
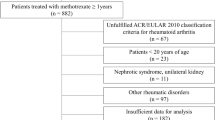
2.3 Study Population
We enrolled patients aged 65 years and older who were newly prescribed GLM between July 1, 2011, and June 30, 2018. Patients newly prescribed GLM were defined as those who had no record of GLM prescription before the index date, which was designated as the first day of prescription. We included patients with a definitive diagnosis of RA (see Online Resource 2) on or before the index date. Severe renal dysfunction (estimated glomerular filtration rate [eGFR], < 30 mL/min) is a contraindication for MTX, so patients were excluded if they had an eGFR of less than 30 mL/min or if eGFR values were unavailable in the 90 days before and after the index date. If multiple values for eGFRs were available, we used only the value from the measurement closest to the index date. The eGFR was calculated by using a previously established equation for the Japanese population: eGFR (mL/min/1.73 m2) = 194 × SCr–1.094 × age–0.287 (× 0.739 for women only), where SCr is serum creatinine [18].
2.4 Study Outcomes
The primary outcome was persistence of GLM treatment. The persistence period was estimated by using the number of prescriptions and the maintenance dosage. For example, if the maintenance dosage was 50 mg and two vials were prescribed, the GLM exposure period was recorded as 8 weeks. An interruption in GLM treatment of more than 60 days was considered as a discontinuation [11, 19].
The secondary outcome was occurrence of serious AEs during GLM exposure. Serious AEs were defined as a definitive diagnosis of malignant neoplasms, demyelinating disease, infectious disease at hospital admission, or acute coronary syndrome at hospital admission [20]. The ICD-10 codes used to identify the serious AEs are listed in Online Resource 3. If patients had repeated serious AEs, we included the first event in the analysis.
2.5 Covariates
As potential covariates, we extracted information on patient demographic characteristics (sex and age at the index date), laboratory test results, comorbidities, drug history, and concomitant drug use. Comorbidities were defined as a definitive diagnosis of hypertension, diabetes, dyslipidemia, or chronic lung disease on or before the index date (see Online Resource 4). Baseline laboratory test results, i.e., results from the period from the index date to 90 days later, were extracted; if multiple tests were conducted during the 90-day period, we used the values from the measurement closest to the index date. The study follow-up period ended on July 31, 2019. Concomitant drugs were extracted in the period from the index date until 90 days after the index date, and drug history was extracted in the period before the index date. The effect of concomitant use of MTX on the persistence of GLM was investigated by dividing the MTX dose into high (≥ 8 mg/week) and low (< 8 mg/week) doses. The study overview is shown in Fig. 1.
2.6 Statistical Analysis
Categorical variables are expressed as number and percentage (%); and continuous variables, as mean and standard deviation (SD) or median and interquartile range (IQR). Results were regarded as statistically significant if p was less than 0.05. We used R version 4.0.3 for Windows (R Foundation for Statistical Computing, Vienna, Austria) for all statistical analyses. We defined a month as 30 days.
The persistence of GLM was compared between three groups classified according to eGFR: high (≥ 90), moderate (≥ 60, < 90), and low (≥ 30, < 60). The thresholds for these renal function severity groups were newly defined in accordance with existing guidance [21]. Kaplan–Meier curves were created to estimate the continuation of drug treatment in each group. Patients were censored at death or at the end of the observation period. The log-rank test was used to test for statistically significant differences between the Kaplan–Meier curves. A sensitivity analysis of the Kaplan–Meier method was performed by using more than 45 days and 90 days as grace periods for GLM continuation. A Cox proportional hazards regression analysis was used to assess the relationship between GLM discontinuation and eGFR, age, sex, maintenance dose of GLM, baseline C-reactive protein (CRP), concomitant use of MTX, concomitant use of non-steroidal anti-inflammatory drugs (NSAIDs), concomitant use of corticosteroids, biologics-naïve patients, and comorbidities.
Cumulative serious AEs were estimated by Kaplan–Meier analysis. When comparing serious AEs, patients were censored at the end of GLM exposure, death, or the end of the study observation period. The log-rank test was used to test for statistically significant differences between the Kaplan–Meier curves. We used the following factors as covariates for the Cox proportional hazards regression analysis: age, sex, maintenance dose of GLM, baseline CRP, concomitant use of MTX, concomitant use of NSAIDs, concomitant use of corticosteroids, new user of biologics, and comorbidities.
2.7 Ethical Approval
The study was approved by the ethics committee of the Research Institute of Healthcare Data Science (https://rihds.org/ethic/) (No RI2020020) and conducted according to the Declaration of Helsinki. Given the anonymous nature of the data, the requirement for informed consent was waived.
3 Results
3.1 Patient Characteristics
In total, 772 patients received GLM during the study period, and of these patients, 423 (male, n = 95; female, n = 328; mean age, 74.7 ± 6.5 years) met the eligibility criteria (Fig. 2). Of the included patients, 85 had high eGFR; 223, moderate eGFR; and 115, low eGFR. The baseline characteristics of the patients are shown in Table 1. The mean duration of GLM treatment was 19.6 ± 20.9 months (median, 10.8; IQR [3.2, 30.3]). Treatment regimens included 50 mg GLM in combination with MTX (n = 229, 54.1%), 100 mg GLM in combination with MTX (n = 28, 6.6%), 50 mg GLM without MTX (n = 99, 23.4%), and 100 mg GLM without MTX (n = 67, 15.8%). Among patients with 1 year or more of GLM exposure, the 1-year changes in eGFR were as follows: high eGFR group, − 15.12 ± 11.75; moderate eGFR group, − 2.90 ± 10.60; and low eGFR group, 0.17 ± 9.01.
3.2 Persistence of GLM
The persistence rate at 6 months after the initial GLM dose was 64.3% (272/423). The 6-month persistence rate stratified by eGFR was 62.4% (53/85) in the high eGFR group, 63.7% (142/223) in the moderate eGFR group, and 67.0% (77/115) in the low eGFR group. The 12- and 36-month persistence rates were 47.1% (40/85) and 17.6% (15/85) in the high eGFR group, 45.7% (102/223) and 20.2% (45/223) in the moderate eGFR group, and 49.6% (57/115) and 18.3% (21/115) in the low eGFR group. Figure 3 shows the Kaplan–Meier curves of drug persistence in the three eGFR groups; there was no significant difference between the groups. The adjusted odds ratio of MTX dose is shown in Online Resource 5. The sensitivity analysis with the two grace periods shows the similarity of the curves in the three eGFR groups (Online Resource 6, 7).
Cox proportional hazards regression analysis revealed that baseline eGFR was not associated with discontinuation in patients with moderate eGFR (hazard ratio [HR], 0.92 [95% CI 0.69–1.23] or low eGFR (HR 0.86 [95% CI 0.60–1.23]). Concomitant MTX and low baseline serum CRP were significantly associated with prolonged persistence of GLM (Table 2).
The results on the effect of concomitant use of MTX on the persistence of GLM suggested that concomitant use of MTX significantly prolonged the persistence of GLM at both high (≥ 8 mg/week) and low (< 8 mg/week) doses of MTX compared with GLM monotherapy (Online Resource 5). Age, sex, and comorbidities were not associated with duration of GLM. The Kaplan–Meier curves comparing GLM alone and GLM with concomitant MTX are shown in Online Resource 8. Receiver operating characteristic curve of C-reactive protein are available in Online Resource 9.
3.3 Adverse Events During GLM Exposure
The incidence rate of serious AEs was 12.87 cases per 100 person-years. Figure 4 shows the cumulative incidence of serious AEs in the eGFR groups. The cumulative incidence of each serious AEs in the eGFR groups are shown in Online Resource 10–12. Cox proportional hazards regression analysis showed no association of the incidence of serious AEs with baseline eGFR (Table 3). The incidence rate of each AE (per 100 person-years) was as follows: malignant neoplasms, 8.06 cases; infectious disease at hospital admission, 4.87 cases; and acute coronary syndrome at hospital admission, 0.33 cases. No patients had demyelinating disease during GLM exposure.
Incidence of serious adverse events and baseline eGFR. The p value was calculated by log rank test. The incidence rate of serious adverse events was 10.7 cases per 100 person-years in patients with high eGFR, 8.6 in those with moderate eGFR, and 10.1 in those with low eGFR. eGFR estimated glomerular filtration rate
4 Discussion
This study showed for the first time that baseline eGFR is not associated with the persistence of GLM and is independent of renal function in elderly patients with RA. Baseline eGFR was also not associated with the incidence of AEs.
The GLM persistence rate at 6 months was 64.3%, which was lower than that reported by previous studies in Japan [11, 22]. By analyzing data in an employee-based health insurance database, Mahlich et al. reported that the GLM persistence rate was 91.9% at 6 months after initial administration [11]. Possible factors that could explain the difference in persistence rates between the study by Mahlich et al. and the present study is that Mahlich et al. enrolled younger patients (mean age = 59.8 years) and excluded patients with fewer than 12 months of follow-up. Previous reports showed that the continuation rate of TNF inhibitors is lower in elderly than in younger patients [6, 7, 10]. To better compare our data with those of Mahlich et al., we recalculated the 6-month persistence rate by including patients with at least 12 months of follow-up and a 3-month washout period before the index date and found a persistence rate of 71.7% (167/233; data not shown). A post-marketing surveillance of GLM reported a persistence rate of 74.7% at 6 months after the first treatment with GLM in elderly patients with RA (> 75 years old) [22]. The differences in persistence rates between previous reports and the present study may be due to the different definitions of target population and persistence and differences in data structure, for example.
The results of this study suggest there is no difference in the safety of GLM treatment in elderly patients with RA with and without renal dysfunction. Impaired renal function is known to result in delayed drug elimination and increased risk of AEs with small molecule compounds such as MTX, which is used as an anchor drug in RA treatment [23, 24]. In contrast, clearance of drugs with larger molecular weights, such as biologics, is not affected by renal function. However, because TNF-α is involved in host defense and tumor growth control, patients with RA who receive TNFi may be at increased risk for infection and malignancy [25]. In addition, uremia due to decreased renal function, which is more common in elderly patients with RA, may likewise decrease the activity of immune cells [26]. Considering the above, there was some concern that TNFi might increase the frequency of AEs, especially in elderly patients with RA and renal dysfunction; however, the present study found no clear increase in the frequency of serious AEs due to decreased renal function.
Sumida et al. divided a population of patients with RA treated with adalimumab, a type of TNFi, into two groups according to the presence or absence of renal dysfunction and examined the proportion of patients who subsequently discontinued or changed their treatment. The researchers found no significant difference between the groups. However, the study was conducted at a single center and in a small sample (39 patients with renal dysfunction and 26 patients without), and the analysis did not focus on the elderly patients [13]. In the current study, we used a larger database to examine the effects of renal dysfunction in more detail and investigated the persistence rate of GLM and frequency of AE in elderly patients with RA. Our results suggest that elderly patients with RA may benefit from GLM regardless of their baseline renal function.
We showed that concomitant use of MTX and GLM was associated with better persistence of GLM treatment and that the proportion of patients treated with concomitant MTX was smaller in the group with low eGFR. Nevertheless, the Kaplan–Meier curves of GLM persistence showed no significant differences between eGFR groups. Previously, concomitant MTX use was shown to improve TNFi persistence in patients with RA [27]. However, it remains unclear whether concomitant MTX use is associated with improved continuation of TNFi therapy in elderly patients [6, 28]. Bechman et al. enrolled 768 elderly patients from a British registry [6]. They reported that the group of patients younger than 75 years old receiving TNFi such as infliximab, etanercept, adalimumab, and certolizumab in combination with MTX had significantly higher persistence rates than those receiving TNFi in monotherapy; however, there was no significant difference in the effect of MTX on the persistence rate in patients aged 75 years and older. The differences in the target patients (e.g., race and definition of elderly) in the study by Bechman et al. and the present study might explain the slight differences in the results.
Our study shows that MTX improves GLM persistence, even at low doses (Table 2 and Online Resource 5). Our analysis was limited to patients with an eGFR of at least 30 mL/min and no contraindication to MTX, but even in these patients, not only the rate of concomitant use of MTX but also the amount used decreased as eGFR decreased (Table 1). Although there are many reasons why MTX is used at low doses in real-world clinical practice, the results of this study suggest that even low doses of MTX can be effective in prolonging the persistence rate of GLM.
Regarding the mechanism by which concomitant use of MTX increases TNFi persistence, previous studies reported that MTX administration reduces the immunogenicity of biologics [29, 30] and that MTX itself may have additive or synergistic antirheumatic effects [31]. Furthermore, studies on GLM showed that concomitant use of MTX alters the pharmacokinetics of GLM and prolongs the duration of antibody persistence [32].
Our Cox proportional hazards regression analysis showed that low baseline CRP also may improve the persistence rate of GLM. This finding suggests that the disease activity of patients at the time of GLM initiation may have an impact on the subsequent GLM persistence rate and that the early suppression of systemic inflammation levels may enable long-term disease control.
This study has some limitations. First, it used a medical database of EMR and claims data, and the database did not include important outcomes such as the disease activity score in 28 joints (DAS28), radiological findings, and reasons for discontinuation (e.g. primary response failure, secondary response failure, or adverse events of the drug). Therefore, it is unclear whether the long persistence of GLM reflected the clinical effectiveness of the drug. Second, the study evaluated EMR data, but we do not know whether patients used the drugs according to their prescription. Therefore, the persistence rate of GLM as measured in this study may be inaccurate; however, this aspect is not expected to have a significant impact on the results because a sensitivity analysis showed similar results for two different grace periods (shown in the Online Resource 6, 7). Last, the database collected data from multiple medical institutions and did not identify when a patient was transferred to a different hospital. Therefore, the persistence of GLM might have been underestimated.
5 Conclusion
The persistence rate of GLM and the frequency of typical adverse events due to GLM exposure in the elderly patients with RA are independent of the degree of renal dysfunction, and concomitant use of MTX and low baseline CRP levels increase the persistence rate of GLM. The finding that also low-dose MTX improves the GLM persistence may be useful information when treating elderly patients with RA in real-world clinical settings, where MTX often is used at lower doses and frequencies of administration; however, further validation in prospective studies is needed.
References
Smolen JS, Aletaha D, McInnes IB. Rheumatoid arthritis. Lancet. 2016;388:2023–38.
Smolen JS, Landewé RBM, Bijlsma JWJ, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79:685–99.
Kameda H, Fujii T, Nakajima A, et al. Japan College of Rheumatology guideline for the use of methotrexate in patients with rheumatoid arthritis. Mod Rheumatol. 2019;29:31–40.
Ma X, Xu S. TNF inhibitor therapy for rheumatoid arthritis. Biomed Rep. 2013;1:177–84.
Rubbert-Roth A, Szabó MZ, Kedves M, et al. Failure of anti-TNF treatment in patients with rheumatoid arthritis: the pros and cons of the early use of alternative biological agents. Autoimmun Rev. 2019;18: 102398.
Bechman K, Oke A, Yates M, et al. Is background methotrexate advantageous in extending TNF inhibitor drug survival in elderly patients with rheumatoid arthritis? An analysis of the British Society for Rheumatology Biologics Register. Rheumatology (Oxford). 2020;59:2563–71.
Jung SM, Lee SW, Song JJ, et al. Drug survival of biologic therapy in elderly patients with rheumatoid arthritis compared with nonelderly patients: results from the Korean College of Rheumatology Biologics Registry. J Clin Rheumatol. 2020;28:e81–8.
Radovits BJ, Kievit W, Fransen J, et al. Influence of age on the outcome of antitumour necrosis factor alpha therapy in rheumatoid arthritis. Ann Rheum Dis. 2009;68:1470–3.
Cho SK, Sung YK, Kim D, et al. Drug retention and safety of TNF inhibitors in elderly patients with rheumatoid arthritis. BMC Musculoskelet Disord. 2016;17:333.
Freitas R, Godinho F, Madeira N, et al. Safety and effectiveness of biologic disease-modifying antirheumatic drugs in older patients with rheumatoid arthritis: a prospective cohort study. Drugs Aging. 2020;37:899–907.
Mahlich J, Sruamsiri R. Persistence with biologic agents for the treatment of rheumatoid arthritis in Japan. Patient Prefer Adherence. 2016;10:1509–19.
Komano Y, Tanaka M, Nanki T, et al. Incidence and risk factors for serious infection in patients with rheumatoid arthritis treated with tumor necrosis factor inhibitors: a report from the Registry of Japanese Rheumatoid Arthritis Patients for Longterm Safety. J Rheumatol. 2011;38(7):1258–64.
Sumida K, Ubara Y, Suwabe T, et al. Adalimumab treatment in patients with rheumatoid arthritis with renal insufficiency. Arthritis Care Res (Hoboken). 2013;65:471–5.
Kawahito Y, Morinobu A, Kaneko Y, et al. Drug Treatment Algorithm and Recommendations from the 2020 update of the Japan College of Rheumatology Clinical Practice Guidelines for the Management of Rheumatoid Arthritis-Secondary Publication. Mod Rheumatol. 2022. https://doi.org/10.1093/mr/roac017.
Tanaka Y, Senoo A, Fujii H, et al. Evaluation of golimumab for the treatment of patients with active rheumatoid arthritis. Expert Opin Drug Metab Toxicol. 2016;12:319–26.
Takeuchi M, Ogura M, Minoura T, et al. Comparative effectiveness of sodium–glucose cotransporter-2 inhibitors versus other classes of glucose-lowering medications on renal outcome in type 2 diabetes. Mayo Clin Proc. 2020;95:265–73.
Fujiwara T, Miyakoshi C, Kanemitsu T, et al. Identification and validation of hemophilia-related outcomes on Japanese electronic medical record database (Hemophilia-REAL V Study). J Blood Med. 2021;12:571–80.
Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Yamairi F, Yano T, Goto T, et al. Dose adjustment of methotrexate administered concomitantly with golimumab for rheumatoid arthritis in Japanese real-world clinical settings. Rheumatol Ther. 2020;7:811–24.
Edwards CJ, Bukowski JF, Burns SM, et al. An analysis of real-world data on the safety of etanercept in older patients with rheumatoid arthritis. Drugs Aging. 2020;37:35–41.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;2013(3):1–150.
Okazaki M, Kobayashi H, Shimizu H, et al. Safety, effectiveness, and treatment persistence of golimumab in elderly patients with rheumatoid arthritis in real-world clinical practice in Japan. Rheumatol Ther. 2018;5:135–48.
Skácelová M, Nekvindová L, Mann H, et al. The beneficial effect of csDMARDs co-medication on drug persistence of first-line TNF inhibitor in rheumatoid arthritis patients: data from Czech ATTRA registry. Rheumatol Int. 2022;42:803–14.
Kanbori M, Suzuka H, Yajima T, et al. Postmarketing surveillance evaluating the safety and effectiveness of golimumab in Japanese patients with rheumatoid arthritis. Mod Rheumatol. 2018;28:66–75.
Dixon W, Silman A. Is there an association between anti-TNF monoclonal antibody therapy in rheumatoid arthritis and risk of malignancy and serious infection? Commentary on the meta-analysis by Bongartz et al. Arthritis Res Ther. 2006;8:111.
Cohen G. Immune dysfunction in uremia 2020. Toxins (Basel). 2020;12:439.
Kristensen LE, Saxne T, Nilsson JA, et al. Impact of concomitant DMARD therapy on adherence to treatment with etanercept and infliximab in rheumatoid arthritis. Results from a six-year observational study in southern Sweden. Arthritis Res Ther. 2006;8:R174.
Zhang J, Xie F, Delzell E, et al. Impact of biologic agents with and without concomitant methotrexate and at reduced doses in older rheumatoid arthritis patients. Arthritis Care Res (Hoboken). 2015;67:624–32.
Krieckaert CL, Nurmohamed MT, Wolbink GJ. Methotrexate reduces immunogenicity in adalimumab treated rheumatoid arthritis patients in a dose dependent manner. Ann Rheum Dis. 2012;71:1914–5.
Jani M, Barton A, Warren RB, et al. The role of DMARDs in reducing the immunogenicity of TNF inhibitors in chronic inflammatory diseases. Rheumatology (Oxford). 2014;53:213–22.
Bendtzen K, Geborek P, Svenson M, et al. Individualized monitoring of drug bioavailability and immunogenicity in rheumatoid arthritis patients treated with the tumor necrosis factor alpha inhibitor infliximab. Arthritis Rheumatol. 2006;54:3782–9.
Zhuang Y, Xu Z, Frederick B, et al. Golimumab pharmacokinetics after repeated subcutaneous and intravenous administrations in patients with rheumatoid arthritis and the effect of concomitant methotrexate: an open-label, randomized study. Clin Ther. 2012;34:77–90.
Acknowledgements
This study was supported by Takashi Fujiwara and Yasuyuki Okumura of Real World Data Co., Ltd, who provided advice on the study concept, statistical analysis, and medical writing. The authors thank the Health, Clinic, and Education Information Evaluation Institute for developing the database for the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Janssen Pharma K.K. (Tokyo, Japan).
Conflict of interest
SY, YI, and JM are employees of Janssen Pharma K.K.
Ethics approval
The study was approved by the ethics committee of the Research Institute of Healthcare Data Science (https://rihds.org/ethic/) (No RI2020020) and conducted according to the Declaration of Helsinki. Given the anonymous nature of the data, the requirement for informed consent was waived.
Consent to participate
Not applicable.
Availability of data and material
The datasets generated and analyzed during the current study are not publicly available.
Author contributions
All authors contributed to the study conception and design. The first draft of the manuscript was written by SY and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Consent for publication
Not applicable.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yokoyama, S., Ishii, Y. & Masuda, J. Persistence and Safety of Golimumab in Elderly Patients with Rheumatoid Arthritis and Renal Dysfunction in a Real-World Setting. Drugs - Real World Outcomes 10, 51–60 (2023). https://doi.org/10.1007/s40801-022-00338-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-022-00338-y