Abstract
Background
There is evidence that repetitive administration of levosimendan can improve outcome in chronic heart failure patients.
Objective
The aim of this retrospective study was to investigate the effect of therapy with levosimendan (LEV) additional to standard medical care in patients with symptomatic heart failure (HFrEF = heart failure with reduced ejection fraction) on NYHA class, NT-proBNP values, ejection fraction (EF) and body weight.
Patients and Methods
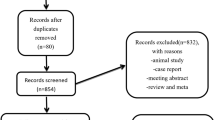
178 participating patients (125 male, 53 female; mean age of 73 ± 13 years) were grouped according to whether LEV was given once (group 1) or repetitively (group 2). In group 2 data were analysed for first treatment with LEV (group 2a) and for the following repetitive LEV treatments (group 2b). The differentiation was required to see if there were different results for the particular groups.
Results
Repetitive dosing was given between two and 11 times, leading to 47 repetitive applications of LEV and a total of 225 (178 once + 47 repetitive) applications. The mean time between the repetitive dosing was 133 days or 4.3 months. LEV in addition to standard medical treatment was associated with reduction of NT-proBNP levels from 9138 to 7051 pg/mL (p < 0.05). The corresponding values in group 2a and group 2b were 8790–4717 pg/mL (p < 0.05) as well as 13,681–7581 pg/mL (p < 0.05). The ejection fraction measured by echocardiography improved from 30 to 38% in group 1, from 31 to 45% in group 2a and from 30 to 35% in group 2b (p < 0.05). Addition of LEV was associated with significant reduction of NYHA class and bodyweight in all groups. No adverse side effects (e.g., rhythm disorder, hypotension, electrolyte disorder) were seen.
Conclusion
LEV may be useful as an additive to standard care of treatment for patients with acute de novo decompensation due to acute heart failure as well as to prevent further deterioration in patients with chronic heart failure disease at high risk for hospitalisation. Intraindividual changes in NT-proBNP levels may be useful in decision-making about the need for additional treatment options in patients with worsening heart failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
LEV-application reduced NYHA class and ejection fraction of the patients. |
Frequently measured NT-proBNP levels can help to evaluate decompensation. |
1 Introduction
Following a remarkable improvement in treatment of heart failure over the last 30 years, a significant reduction in mortality as well as in hospitalisation rate in heart failure patients with reduced ejection fraction (HFrEF) has been observed [1]. However, patients with reduced ejection fraction remain at high risk for hospitalisation or death. It has been documented in several trials that prior heart failure hospitalisation is a strong predictor for cardiovascular death and for further heart failure hospitalisations [2]. The current medical treatment consists of beta-blockers, angiotensin-converting enzyme (ACE)-inhibitors, angiotensin receptor-neprilysin inhibitors (ARNIs), and mineralocorticoid receptor antagonists (MRAs) to improve prognosis [1]. Diuretics are the corner-stone to treat patients with decompensation and fluid overload. Recently, sodium glucose co-transporter 2 (SGLT-2) inhibitors have been added to the treatment options for chronic heart failure patients (ESC 2021) [3]. However, patients with chronic heart failure have a high risk for further worsening of symptoms following fluid overload with signs of congestion, and for further hospitalisations. In this situation optimization of preload and afterload may help reduce symptoms of patients. Treatments with compounds that increase the sympatho-adrenergic activity (beta-agonist, alpha agonist) may stabilize symptoms in the short term, but have been shown to increase mortality [1]. In this situation, levosimendan, a calcium sensitizer, has been demonstrated to beneficially influence symptoms of patients with heart failure [4]. The effect of levosimendan is based on an increase in the sensitivity of myofibrils of the cardiac muscle to calcium by selectively increasing binding to troponin C. Stabilization of the calcium-troponin C complex allows optimized cross-bridge formation, thereby increasing contractility. In addition, levosimendan also modulates ATP-sensitive potassium channels in smooth muscle cells leading to vasodilation and thereby to reduction of preload [4,5,6,7,8,9].
Measurement of N-terminal proBNP sodium peptide (NT-proBNP) has been shown to be a cornerstone for diagnostic risk stratification and follow-up of treatment effects in patients with heart failure [10, 11]. Because of its high negative predictive value, measurement of NT-pro BNP has become an established exclusion parameter for the diagnosis of heart failure [1]. Moreover, NT-proBNP has been used as an inclusion criterion for clinical trials as well as a (bio)marker for the clinical effect of heart failure treatment [12]. More recently, this was demonstrated in the VICTORIA trial to investigate the effect of the sGC-stimulator vericiguat in heart failure patients with recent decompensation episodes [10, 13]. However, many factors such as patient history (gender, body weight, age), renal function, and various treatment mechanisms also influence NT-proBNP levels [14]. A reduction in NT-proBNP level with treatment has been shown to be a marker of lower mortality as well as a lower likelihood of re-hospitalisation for heart failure.
The aim of the present retrospective study was to evaluate the effect of additional therapy with levosimendan in patients hospitalized for symptomatic heart failure for three reasons: (i) acute de novo cardiac decompensation (acute coronary syndrome (ACS), myocarditis, Tako-Tsubo syndrome, tachycardiomyopathy); (ii) because of decompensation of chronic heart failure (dilated cardiomyopathy (DCM), ischaemic cardiomyopathy (ICM)); or (iii) because of a cardio-renal syndrome (Table 1). Patients were grouped according to whether levosimendan was given only once (group 1) or repetitively (group 2). In group 2 data were analysed for first treatment with levosimendan (group 2a) as well as for the following repetitive levosimendan treatments (group 2b). We sought to determine whether the effect of using LEV differed among groups 1, 2a, and 2b.
2 Methods
2.1 Study Design
In this retrospective analysis we estimated the effect of levosimendan in addition to guideline-directed therapy in patients hospitalised for de novo cardiac decompensation because of acute coronary syndrome (n = 64.28%), myocarditis (n = 7.3%), tako-tsubo-syndrome (n = 3.1%) or tachy-cardio-myopathy (n = 13.6%), acute reno-cardiac syndrome (n = 5.2%) or in chronic heart failure patients with repetitive episodes of decompensation due to dilated (n = 50.22%) or ischaemic cardiomyopathy (n = 83.37%) (Table 1). The whole study is a retrospective analysis of the found results, therefore we have no planned treatment intervals with LEV. Still, results can be seen from the results gained in clinical daily routine.
From January 2018 to December 2020 178 consecutive patients (125 male, 53 female; mean age of 73 ± 13 years) were included. In 178 consecutive patients, levosimendan treatment in addition to guideline medication and standard care was studied in a real-world scenario in a primary-care hospital. The effect of levosimendan on NYHA class, NT-proBNP levels, ejection fraction, bodyweight and laboratory baseline parameters was analysed.
NYHA class, NT-pro BNP levels, ejection fraction (echocardiography with Phillips EPIQ 8 using Simpson method), bodyweight and laboratory parameters were measured directly before and after levosimendan treatment as well as before leaving the hospital. The baseline treatment of patients occurred under the determination of the attending physician (coronary intervention in acute coronary syndrome patients, ECMO, treatment with diuretics, use of catecholamines like dobutamine, noradrenaline, suprarenine). In addition to baseline treatment, levosimendan medication was added for 6 hours (0.1 µg/kg body weight/min) and doubled in dosage for the following 18 h.
2.2 Statistical Analysis
Statistical analysis was performed with SPSS Statistics using Student’s t test with a level of significance of p < 0.05. Measurements are given as arrhythmic mean value, standard arrow of the mean (SD), mean value following the 25th as well as the 75th percentile (IQA). Figures are given as boxplots with median values as well as the upper 25th and lower 25th percentile limits.
3 Results
One hundred and seventy-eight patients (125 male, 53 female; mean age 73 ± 13 years) from January 2018 to December 2020 were treated with levosimendan in addition to standard medical care (coronary intervention in acute coronary syndrome patients, ECMO, treatment with diuretics, use of catecholamines like dobutamine, noradrenaline, suprarenine). Eighteen of 178 patients were treated with levosimendan repetitively up to 11 times (group 2). Those ‘outpatients’ gained bodyweight, serious dyspnoea, and an increase in NT-proBNP levels, and thus were scheduled for additional treatment with levosimendan prior to upcoming decompensation. These heart failure patients were hospitalized for the planned levosimendan treatment exclusively (group 2b). There were no defined SOPs for the indication of levosimendan in the treatment scenario. After treatment with OMT, the physician could decide about the option of additional application of levosimendan. The mean time between the repetitive dosing was 133 days, which equates to 4.3 months. Levosimendan was used for repetitive treatment 47 times (group 2). Overall (group 1 + 2) levosimendan treatment was used 225 times (178 + 47). In group 1 in 87 cases, levosimendan was used for treatment of de novo acute cardiac decompensation following acute coronary syndromes (n = 64), myocarditis (n = 7), Tako-Tsubo syndrome (n = 3), tachyarrhythmia episodes (n = 13). Levosimendan was also used in patients with acute decompensation due to chronic heart failure disease for ischaemic cardiomyopathy (n = 83) or dilated cardiomyopathy (n = 50). In five patients levosimendan was used for recompensation following reno-cardiac decompensation (Table 1).
Outpatient medical care of patients consisted of beta-blocker (91%), ACE inhibitor (86%), AT1 antagonist (16%), ARNI (sacubitril/valsartan) (12%), MRA (72%), calcium-channel blocker (23%), loop diuretics (92%) and digitalis (20%) (Table 2). Levosimendan was given as a continuous infusion in a dosage of 0.1 µg/kg/min for 6 h; thereafter dosage was doubled for a further 18 h. No adverse side effects (e.g., rhythm disorder, hypotension, electrolyte disorder) were recognised when levosimendan was added to standard care. In follow-up, 30 days’ survival following the last administration of levosimendan was 83%. In 32 cases treatment of acute cardiac decompensation was performed with one additional catecholamine, in 31 cases with two catecholamines and in four cases with a combination of three catecholamines (dobutamine, noradrenaline, adrenaline). The survival rate was 78%, 11%, 9% and 2% in patients treated with no, one, two or three types of catecholamines, respectively. The survival of patients with repetitive dosing of levosimendan was 100% during follow-up.
Before therapy, in group 1 64% of patients were in NYHA class IV and 35% in NYHA class III. Following treatment 6.8% of patients were at NYHA class IV, 35.6% in NYHA class III and 57.6% in NYHA class II or better (Table 3). The corresponding values for group 2 before first treatment with levosimendan were 47.4% NYHA class IV and 42% NYHA class III. After additional treatment with levosimendan none of the patients (group 2) was in NYHA class IV anymore, 27.8% were in NYHA class III, and 72.2% NYHA class II or better. In the repetitive dosing group (2b) initially 32.6% were NYHA class IV and 65.2% NYHA class III. After treatment, the corresponding values were NYHA class IV 2.2%, NYHA class III 28.9% and NYHA class II or better 68.9% (Table 3).
Thus, additional levosimendan treatment to guideline-directed medication of patients with acute cardiac decompensation was associated with pronounced reduction in NYHA class following first or repetitive treatment. Also, in patients treated with catecholamines, addition of levosimendan was effective in reducing the dosage of catecholamines.
Levosimendan in addition to standard medical treatment was associated with a reduction of NT-proBNP levels from 9138 to 7051 pg/mL (p < 0.05). The corresponding values in group 2a and group 2b were 8790–4717 pg/mL (p < 0.05) as well as 13,681–7581 pg/mL (p < 0.05) (Table 3). Mean values as well as the median are given as boxplots in Fig. 1 and in Table 3. Therapy with levosimendan was associated with a reduction of NT-proBNP levels following initial treatment as well as following repetitive administration of levosimendan.
The ejection fraction measured by echocardiography improved from 30% to 38% in group 1, from 31% to 45% in group 2a, and from 30% to 35% in group 2b (p < 0.05). Figure 2 summarizes the effect of levosimendan on ejection fraction showing that initial treatment as well as repetitive dosing with levosimendan was associated with improved ejection fraction (Table 3).
Guideline-directed treatment of patients with acute cardiac decompensation in addition to levosimendan was effective in lowering bodyweight from 85 kg to 82 kg in group 1 and from 88 kg to 85 kg in group 2a (p < 0.05). The mean difference in bodyweight was– 5 kg in group 1 and −4 kg in group 2 following first dosing. The corresponding value after repetitive administration of levosimendan was − 2 kg (repetitive dosing).
Additional treatment of levosimendan did not affect potassium (4.2 ± 0.6 mmol/L vs. 4.1 ± 0.5 mmol/L), sodium (140 ± 5 mmol/L vs. 140 ± 5 mmol/L) or glomerular filtration rate (GFR) (46.6 ± 22 mL/min vs. 49.6 ± 26 mL/min). This also applies for the clinical parameters heart rate (80 ± 17/min vs. 80 ± 15/min) and blood pressure (117 ± 16 mmHg vs. 122 ± 18 mmHg).
Figure 3 illustrates NT-proBNP levels of one patient with repetitive dosing over the period of 11 applications of levosimendan. The patient had a long history of coronary heart disease and developed ischaemic cardiomyopathy with prominent enlargement of the left ventricle, ejection fraction 18%. This patient was also treated by biventricular pacing because of left bundle block. Following first treatment with levosimendan because of cardiac decompensation with fluid overload, the patient was treated with MitralClip-implantation because of prominent mitral regurgitation (MI IV). In a follow-up clinical situation as well NT-proBNP-levels could be stabilized following repetitive treatments with levosimendan over a period of 35 months. Thus, repeated administration of levosimendan was associated with a positive effect on NYHA class, NT-proBNP levels, and ejection fraction in patients with chronic heart failure and recurrent decompensations.
Effect of repetitive dosing of levosimendan on NT-proBNP levels. NT–proBNP levels are shown before and after levosimendan treatment in a patient with repetitive treatment with levosimendan. The numbers below the plot symbolize the point of measure: the first digit refers to the hospitalisation number, the second digit refers to the measure time during that stay: 1 = before the treatment, 2 = after treatment and 3 = just before dismissal. The red line marks the intervention of mitral-clipping during the first hospitalisation. Levosimendan was effective in lowering NT-proBNP levels each time when given. The high rise in NT-proBNP levels after the first hospitalisation was due to acute kidney failure. The plot shows NT-proBNP levels over a timeline of 35 months. The time intervals are drafted below the legend (a. 6 m = after 6 months, etc.)
4 Discussion
Patients hospitalized because of acute de novo cardiac decompensation as well as patients with chronic heart failure who decompensate repeatedly have a poor prognosis [2]. For patients with reduced ejection fraction (HfrEF), several therapeutic advances promise to delay clinical progression and prolong disease-free survival [1]. Current guidelines recommend a combination of therapy with an ARNI/ACE inhibitor, beta-blocker, MRA and SGLT2-blocker as standard care. For better fluid control and to treat symptoms of congestion, diuretics may be added. These treatment options represent the ‘big five’ in drug treatment for HFrEF [3, 15]. Despite the drug treatment recommended in the guidelines for patients with heart failure, these patients are at high risk of acute decompensation and hospitalisation. Any hospitalisation due to cardiac decompensation limits clinical outcome. In addition, the use of catecholamines to treat patients with acute cardiac decompensation and volume overload further worsens clinical outcomes [1]. Therefore, there is a need for additional treatment options for patients with acute decompensation as well as for patients with chronic heart failure and high risk for decompensation [7, 16].
In 178 consecutive patients hospitalized for acute heart failure due to acute coronary syndrome, myocarditis, Tako-Tsubo syndrome, or tachyarrhythmia, we supplemented standard drug treatment with treatment with levosimendan (Table 1). In 18 patients with chronic heart failure, repeated treatment with levosimendan was given to improve symptoms. In these patients, levosimendan was administered between two and 11 times (47 treatment courses).
The additional administration of levosimendan to standard treatment was associated with an improvement in NYHA class, a reduction in NT-proBNP levels and body weight, and an increase in ejection fraction measured by echocardiography. No significant side effects of levosimendan were observed when added to standard treatment. Levosimendan may be useful as an additive to standard treatment in patients with acute de novo decompensation due to acute heart failure after acute coronary syndrome, and levosimendan may be effective in preventing further deterioration in patients with chronic heart failure at high risk for hospitalisation.
Natriuretic peptide measurements are frequently used to exclude the diagnosis of heart failure because of their high negative predictive value [1]. In addition, NT-proBNP measurement has been used in recent studies to characterize patients with heart failure and to monitor treatment effects [10, 11, 14]. In the present study, NT-proBNP levels were measured before and after treatment with levosimendan in addition to NYHA class, ejection fraction and body weight. Levosimendan was associated with a reduction in NT-proBNP levels and improvement in clinical symptoms in patients with acute decompensation or in patients treated repeatedly with levosimendan for chronic heart failure. NT-proBNP levels have been shown to reflect ventricular wall stress and cardiac filling pressure, which are pathophysiologically associated with symptoms that may lead to worsening heart failure and initiation of hospitalisation for heart failure [17]. Therefore, NT-proBNP levels in addition to clinical status (body weight, dyspnoea) may help to identify patients with chronic heart failure who are at high risk for impending further decompensation. In the present study, these patients were repeatedly treated with levosimendan [7]. This lowered NT-proBNP levels, reduced symptoms, and allowed patients to continue treatment as outpatients. Repeated use of levosimendan has been reported to reduce plasma concentrations of NT-proBNP and the need for hospitalisation for heart failure, and also to improve quality of life [18,19,20]. This may also reduce the cost of treatment [21]. The optimal interval for repeated treatment with levosimendan is still under investigation. In our population, repeated administration occurred at an interval of 4.3 months; in the Leo-Dor study, the interval of repeated treatment was either 2 weeks or every 3 weeks [22].
Patients in our study (group 2b) were treated only if NT-proBNP values or clinical signs were above reference values, indicating impending decompensation. Several measures were used as prognostic information for impending decompensation, such as the scoring system [23], body weight, and measurement of pulmonary ingestion by bioimpedance measurements [24]. In our cohort, plasma NT-proBNP levels were significantly elevated before levosimendan treatment and were decreased after levosimendan treatment. This effect was consistent in both the single-dose group (group 1) and in patients treated repeatedly with levosimendan, both during the first (group 2a) and after repeated use (group 2b). In patients with de novo decompensation of acute heart failure, levosimendan in addition to intravenous medication with one catecholamine (19%), two catecholamine types (19%), and three catecholamine types was also associated with improvement in symptoms, reduction in NT-proBNP levels, and reduced need for catecholamines. Consequently, treatment with levosimendan may contribute to improved outcomes and symptoms by reducing the need for catecholamines.
Therapy-related changes in NT-proBNP levels have been inhomogeneously associated with treatment effects and different clinical outcomes in various chronic heart failure studies [14, 25]. In these studies, NT-proBNP levels may better reflect therapeutic effects and heart failure hospitalisation than effects on mortality or outcome [26, 27]. In individual patients, NT-proBNP levels appear to reflect the treatment effects of medications, predict response to therapy, and also identify the need for more intensive heart failure treatment. The effects of treatment on NT-proBNP levels and outcome have also been investigated in recent studies, such as PARADIGM-AF [25, 28]. Patients treated with sacubitril/valsartan were more likely to have lower NT-proBNP levels than the control group treated with enalapril. Consequently, patients with lower NT-proBNP levels also had a lower risk of subsequent clinical events. Also, in studies measuring the effect of RAA inhibitors, lower NT-proBNP levels were associated with favourable treatment effects and reduced hospitalisations for heart failure [25].
Since decompensation episodes are usually accompanied by an increase in body weight, daily weight monitoring could be useful to monitor the clinical condition of patients with chronic heart failure and also provide information about effective recompensation. In the present study, all patients treated for signs of congestion showed a reduction in body weight. Treatment with the calcium sensitizer levosimendan was associated with an increase in ejection fraction. This has also been demonstrated previously [9, 29]. In the present study, the mean change in ejection fraction was + 7%. This could be the result of the combination of standard treatment and additional use of levosimendan.
The use of levosimendan in the present study was safe, and this is consistent with several studies [7, 16, 22]. Levosimendan had no significant effects on blood markers such as sodium, potassium, creatinine, GFR, haemoglobin, heart rate, or systolic and diastolic blood pressure when administered additively to standard treatment. These parameters were measured immediately before and after the use of levosimendan. It should be noted that no bolus of levosimendan was used in the present study.
4.1 Study Limitations
In this retrospective cohort study, patients with acute de novo or recurrent cardiac decompensation due to a wide range of diseases were studied. Due to the retrospective design, no ethical conflict arose. The patients always received the best possible individual care according to current guidelines and the best state of knowledge. Moreover, due to the retrospective design, the data were derived from a real-life scenario. Levosimendan was administered as needed on an individual basis and not by a predetermined study protocol or schedule. However, due to the lack of a study protocol, documentation for the study of important parameters was sometimes incomplete. This circumstance diminishes the validity and interpretation of the results. Prospective placebo-controlled studies in patients with de novo decompensation and in patients with repeated episodes of decompensation are needed to further elucidate the treatment effect of levosimendan. As evidenced by the high rate of recurrent decompensation episodes in patients with heart failure, there is a need for new treatment options for this patient population and for new prospective studies.
5 Conclusions
In conclusion, there is a need for new treatment options for patients with acute heart failure [30]. Treatment with levosimendan, in addition to guideline-guided heart failure management, can reduce NYHA class, improve ejection fraction, lower NT-proBNP levels and also body weight in patients with acute de novo or recurrent cardiac decompensation. The beneficial effects of levosimendan in a real-world scenario have been demonstrated in a wide range of patients with acute cardiac decompensation after acute coronary syndrome, myocarditis, Tako-Tsubo syndrome, tachyarrhythmic episodes, and in patients with repeated episodes of decompensation due to progression of ischaemic or dilated cardiomyopathy (Table 1).
References
Ponikowski P, Voors AA, Anker SCD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2016;37:2129–200. https://doi.org/10.1093/eurheartj/ehw128.
Nieminen MS, Altenberger J, Ben-Gal T, et al. Repetitive use of levosimendan for treatment of chronic advanced heart failure: clinical evidence, practical considerations, and perspectives: an expert panel consensus. Int J Cardiol. 2014;174(2):360–7. https://doi.org/10.1016/j.ijcard.2014.04.111.
Abdin A, Bauersachs J, Frey N, et al. Timely and individualized heart failure management: need for implementation into the new guidelines. Clin Res Cardiol. 2021;13:1–9. https://doi.org/10.1007/s00392-021-01867-2.
Papp Z, Agostoni P, Alvarez J, et al. Levosimendan efficacy and safety: 20 years of SIMDAX in clinical use. Card Fail Rev. 2020;8(6): e19. https://doi.org/10.15420/cfr.2020.03.eCollection2020Mar.
Reuter H, Schwinger RHG. Calcium handling in human heart failure–abnormalities and target for therapy. Wien Med Wochenschr. 2012;162(13–14):297–301. https://doi.org/10.1007/s10354-012-0117-9.
Farmakis D, Alvarez J, Gal TB, et al. Levosimendan beyond inotrop and acute heart failure: evidence of pleiotropic effects on the heart and other organs: an expert panel position paper. Int J Cardiol. 2016;222:303–12. https://doi.org/10.1016/j.ijcard.2016.07.202.
Gustafsson F, Guarracino F, Schwinger RHG. The inodilator levosimendan as a treatment for acute heart failure in various settings. Eur Heart J Suppl. 2017;19(Suppl C):C2–7. https://doi.org/10.1093/eurheartj/sux001.
Harjola VP, Giannakoulas G, von Lewinski D, et al. Use of levosimendan in acute heart failure. Eur Heart J Suppl. 2018;20(Suppl I):I2–10. https://doi.org/10.1093/eurheartj/suy039.
Najjar E, Stålhberg M, Hage C, et al. Haemodynamic effects of levosimendan in advanced but stable chronic heart failure. ESC Heart Fail. 2018;5(3):302–8.
Ezekowitz JA, O’Connor C, Troughton R, et al. N-terminal pro-B-type natriuretic peptide and clinical outcomes: vericiguat heart failure with reduced ejection fraction study. 2020. Clinical Trial. JACC Heart Fail. 2020;8(11):931–9. https://doi.org/10.1016/j.jchf.2020.08.008.
Januzzi J Jr. Will biomarkers succeed as a surrogate endpoint in heart failure trials? Jacc Heart Fail. 2018;6(7):570–2. https://doi.org/10.1016/j.jchf.2018.02.008.
Packer M, Anker SD, Butler J, et al. Effect of empagliflozin on the clinical stability of patients with heart failure and a reduced ejection fraction. Circulation. 2021;143(4):326–36. https://doi.org/10.1161/CIRCULATIONAHA.120.051783.
Schwinger RHG. Vericiguat—ein neuer Stern in der Herzinsuffizienztherapie? Kompendium Herz-Kreislauf. 2021. https://doi.org/10.1055/a-1281-8902.
Savarese G, Orsini N, Hage C, et al. Utilizing NT-pro-BNP for Eligibility an Enrichment in Trials in HfpEF, HFmrEF an HFrEF. JACC Heart Fail. 2018;6(3):246–56. https://doi.org/10.1016/j.jchf.2017.12.014.
Bauersachs J. Heart failure drug treatment: the fantastic four. Eur Heart J. 2021;42(6):681–3. https://doi.org/10.1093/eurheartj/ehaa1012.
Nieminen MS, Dickstein K, Fonseca C, et al. The patient perspective: quality of life in advanced heart failure with frequent hospitalisations. Int J Cardiol. 2015;191:256–64. https://doi.org/10.1016/j.ijcard.2015.04.235.
Schwinger RHG. Pathophysiology of heart failure. Cardiovasc Diagn Ther. 2021;11(1):263–76. https://doi.org/10.21037/cdt-20-302.
Comin-Colet J, Manito N, Segovia-Cubero J, et al., et al. Efficacy and safety of intermittent intravenous outpatient administration of levosimendan in patients with advanced heart failure: the LION-HEART multicentre randomised trial. Eur J Heart Fail. 2018;20(7):1128–36.
Navarri R, Lunghetti S, Cameli M, et al. Neurohumoral improvement and torsional dynamics in patients with heart failure after treatment with levosimendan. Int J Cardiol Heart Vasc. 2015;7:153–7.
Adamopoulos S, Parissis J, Iliodromitis E, et al. Effects of levosimendan versus dobutamine on inflammatory and apoptotic pathways in acutely decompensated chronic heart failure. Am J Cardiol. 2006;98(1):102–6.
Manito Lorite N, Rubio-Rodrizuez D, González Costello J, et al. Economic analysis of intermittent intravenous outpatient treatment with levosimendan in advanced heart failure in Spain. Rev Esp Cardiol (Engl Ed). 2020;73(5):361–7.
Pölzl G, AllipourBirgani S, Comin-Colet J, et al. Repetitive levosimendan infusions for patients with advanced chronic heart failure in the vulnerable post-discharge period. ESC Heart Fail. 2019;6(1):174–81.
Mo R, Yu LT, Tan HQ, et al. A new scoring system for predicting short-term outcomes in Chinese patients with critically-ill acute decompensated heart failure. BMC Cardiovasc Disord. 2021;21(1):228.
Shavelle DM, Deai AS, Abraham WT, et al. Lower rates of heart failure and all-cause hospitalizations during pulmonary artery pressure-guided therapy for ambulatory heart failure: one-year outcomes from the CardioMEMS post-approval study. Circ Heart Fail. 2020;13(8): e006863.
Vaduganathan M, Claggett B, Packer M, et al. Natriuretic peptides as biomarkers of treatment response in clinical trials of heart failure. JACC Heart Fail. 2018;6(7):564–9. https://doi.org/10.1016/j.jchf.2018.02.007.
Lund LH. Heart failure with “mid-range” ejection fraction-new opportunities. J Card Fail. 2016;22:769–71.
Vedin O, Lam CSP, Koh AS, et al. (2017) Significance of ischemic heart disease in patients with heart failure and preserved, midrange, and reduced ejection fraction: a nationwide cohort study. Circ Heart Fail 10. pii:e003875.
Vaduganathan M, Claggett B, Jhund P, et al. Estimating lifetime benefits of comprehensive disease-modifying pharmacological therapies in patients with heart failure with reduced ejection fraction: a comparative analysis of three randomised controlled trials. Lancet. 2020;396(10244):121–8. https://doi.org/10.1016/S0140-6736(20)30748-0.
Cui D, Liao Y, Li G, et al. Levosimendan can improve the level of B-type natriuretic peptide and the left ventricular ejection fraction of patients with advanced heart failure: a meta-analysis of randomized controlled trials. Am J Cardiovasc Drugs. 2021. PMID: 32462455.
Butler J, Fonarow GC, Zile MR, et al. Developing therapies for heart failure with preserved ejection fraction: current state and future directions. J Am Col Cardiol. 2014;2:97–112.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No financial support was provided for this work.
Conflict of interest
Not applicable for both authors Maximilian Wechsler and Robert H.G. Schwinger.
Ethics approval
Not applicable.
Compliance with ethical guidelines and conflict of interests
The authors Maximilian Wechsler and Robert H.G. Schwinger state that there is no conflict of competing interests. No funds, grants or other support was received. The authors have no conflicts of interest to declare that are relevant to the content of this article. This is a retrospective observation. Ethical approval is not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material (data transparency)
Data sharing is not applicable to this article as no datasets were generated or analysed.
Code availability
Not applicable.
Author contribution
All authors contributed to the study conception and analysis. All authors read and approved the final version.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wechsler, M., Schwinger, R.H.G. Association of Repetitive Dosing of Levosimendan with Reduction of NYHA Class and NT-proBNP Levels in Decompensated Heart Failure: A Retrospective Cohort Study. Drugs - Real World Outcomes 9, 529–537 (2022). https://doi.org/10.1007/s40801-022-00313-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-022-00313-7