Abstract
Background
Atrial fibrillation (AF) is a major risk factor for the development of stroke and silent cerebral infarct (SCI). Additionally, AF is independently associated with neurological disorders, including cognitive impairment and dementia. Although oral anticoagulants (OACs) are used to reduce the risk of development of stroke and SCI in patients with AF, it is unclear whether OACs reduce the risk of dementia.
Objective
This study aimed to investigate the association between OAC use and dementia in relatively young patients with AF. Moreover, the impact of medication adherence on the association between OAC use and the risk of dementia was examined.
Patients and Methods
This retrospective cohort study was conducted using a large claims database—Japan Medical Data Center, Inc. (JMDC)—from which newly diagnosed patients with AF younger than 75 years of age were identified. We analyzed medication adherence using the medication possession ratio (MPR). The dementia risk was compared between the OAC and non-OAC groups using Cox proportional hazards regression analysis and the Kaplan–Meier method after propensity score matching. Similarly, the MPR-classified and non-OAC groups were also compared.
Results
OAC administration was not associated with the risk of dementia in the entire cohort (hazard ratio [HR] 0.66, 95% confidence interval [CI] 0.40–1.08; p = 0.098); however, OAC administration in patients with an MPR ≥90% was significantly associated with a lower risk of dementia (HR 0.45, 95% CI 0.25–0.81; p = 0.008). Meanwhile, direct OAC (DOAC) and warfarin (WF) administration was not associated with the risk of dementia regardless of MPR. Kaplan–Meier analysis revealed a significant difference in the incidence of dementia between the MPR ≥ 90% OAC and non-OAC groups (log-rank test: p = 0.006). However, no difference was observed in the incidence of dementia between the MPR ≥ 90% WF and non-OAC groups, or between the MPR ≥ 90% DOAC and non-OAC groups.
Conclusions
OAC administration was not associated with the risk of dementia in relatively young patients with AF; however, when limited to patients with an MPR ≥ 90%, OAC administration reduced the risk of dementia. Our results suggest that the association between OAC use and dementia should be evaluated while considering medication adherence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Oral anticoagulant (OAC) administration did not reduce the risk of dementia in patients with nonvalvular atrial fibrillation younger than 75 years of age. |
OAC administration reduced the risk of dementia in patients with an MPR ≥ 90%. |
In the separate analyses of direct OACs and warfarin, administration in patients with an MPR ≥ 90% did not reduce the risk of dementia. |
1 Introduction
The prevalence of atrial fibrillation (AF) in Japan is approximately 0.6% [1], and the number of patients with AF is increasing not only in Japan but also worldwide [2]. Recent studies have suggested that AF is independently associated with neurological disorders, including cognitive impairment and dementia, even after adjusting for previous ischemic stroke [3, 4]. Furthermore, AF has been reported to be associated with an increased risk of mild cognitive impairment and dementia, even among patients who had not experienced an overt stroke [5,6,7]. The aforementioned reports suggest that additional mechanisms other than stroke may be involved in the association between AF and dementia. Accordingly, nerve cell damage due to silent cerebral infarct (SCI), reduced cerebral blood flow, and chronic cerebral hypoperfusion due to complicated heart failure and irregular heartbeat have been presumed to be some of the mechanisms for the development of dementia.
A number of retrospective studies have reported that oral anticoagulants (OACs) reduce the development of stroke or SCI and subsequently reduce the risk of dementia or cognitive impairment in patients with AF [8,9,10]. However, no randomized controlled trial (RCT) has investigated the association between anticoagulant therapy and cognitive decline or dementia in patients with AF. Although RCT remains the gold standard for determining therapeutic efficacy, it would be difficult and unethical to investigate the risk of dementia in patients with AF. By contrast, a study using real-world data (RWD) may be invaluable. Studies using RWD such as registry, claims, prescription, and electronic healthcare record databases can provide valuable information about practice patterns and patient characteristics in actual clinical settings [11], if appropriately designed.
Dementia reduces the quality of life of caregivers, such as family members, as well as the patient. Because dementia is not completely curable, the onset of dementia in young patients is expected to require a longer duration of caregiving than that in older patients. Although it is generally known that older people are at a higher risk of dementia, some studies have reported that younger patients (aged < 70 years) with AF are at a greater risk of dementia than older patients [4, 12]. Therefore, further study is needed to clarify the association between the risk of dementia and OAC use in relatively young patients with AF.
Patient adherence and persistence to drug therapy are known to affect treatment effectiveness. Some observational studies reported that stroke reduction following direct OAC (DOAC) treatment in patients with AF is dependent on adherence and persistence in the real-world setting. Ozaki et al. reported that suboptimal adherence and persistence to DOACs were common in patients with AF, with one in three patients adhering to their DOAC < 80% of the time, which was associated with poor clinical outcomes in nonadherent patients [13]. Moreover, Obamiro et al. reported that approximately 50% of patients taking OACs had poor adherence to their therapy [14]. The association between OAC use and dementia risk should be investigated considering medication adherence, but few studies have considered adherence.
Therefore, this study aimed to investigate the association between OAC use and the risk of dementia in patients with nonvalvular AF. Additionally, we hypothesized that adherence to medication may be a significant protective factor for dementia in patients with nonvalvular AF who received OACs.
2 Methods
2.1 Study Design
A retrospective cohort study was conducted to investigate the association between OAC use and dementia using a large claims database constructed by the Japan Medical Data Center, Inc. (JMDC), one of the database vendors in Japan [15].
2.2 Data Source
The JMDC claims database includes approximately 6 million insured individuals (approximately 5% of the population), consisting primarily of health insurance association members and their families (aged < 75 years). The JMDC database provides information on monthly claims (inpatient, outpatient, and dispensing) received from multiple health insurance associations. This information includes encrypted personal identifiers, age, sex, treatment, International Classification of Diseases 10th revision (ICD-10) codes, and standardized disease classification codes developed by the Medical Information System Development Center. The database also provides data about the name, dose, and number of days for which the drugs were prescribed and/or dispensed. All prescribed drugs are coded according to the Anatomical Therapeutic Chemical classification based on the European Pharmaceutical Market Research Association, with the ingredient and product names also being provided. Given that all claims are collected by the health insurance association, the same patient’s claims are linked even when they visit multiple medical institutions. Additionally, all personal names and identification numbers from the JMDC claims database were replaced by a univocal numerical code. Therefore, obtaining informed consent was not required in this study. This study was approved by the Ethics Committee of Kindai University School of Pharmacy (approval numbers: 17-112).
2.3 Study Population
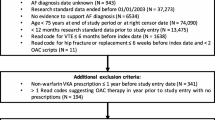
All patients who were diagnosed with AF between April 2010 and April 2019 were extracted from the JMDC claims database. To exclude prevalent cases of AF, the analysis was restricted to patients who were first diagnosed in April 2011 or later (after a run-in period of 12 months). Likewise, the analysis was restricted to OAC users who received their first prescription in April 2011 or later. Patients with incident AF and OAC users aged > 18 years were included in the study. For this study, patients included in the database were followed up until April 2019; therefore, they had different follow-up periods. Patients who did not have at least 6 months of follow-up after their AF diagnosis and at least 12 months of database history (pre-index period) before their AF diagnosis were excluded from the analysis. Additionally, patients who were prescribed OACs within 12 months before the diagnosis of AF and patients who were diagnosed with dementia prior to the diagnosis of AF were excluded from the analysis. Patients diagnosed with atrial flutter and valvular AF, who were identified using standardized disease classification codes (4273009 and 8846941), were excluded from the analysis because such diseases have not been approved as indications for DOACs in Japan. Patients with incomplete medical treatment data were excluded from the analysis. The ICD-10 code I48 was used to identify patients with AF. ICD-10 codes generally have high sensitivity and specificity [16]. The cohort study design is presented in Fig. 1.
Patients were then divided into two groups, the OAC and non-OAC groups, with the former being further divided into the warfarin (WF) and DOAC groups according to the type of OAC initially prescribed. Patients who were prescribed both WF and DOACs on the same day during the follow-up period were treated as censored cases. In total, 17 patients received both WF and DOAC prescriptions on the start date, but in these patients, both treatments were prescribed only on this date. Therefore, these patients were included in the continuously prescribed medications group. Patients were followed from the date of the first AF diagnosis to any of the following events, whichever occurred first: diagnosis of dementia defined by the ICD-10 codes F00–F03 and G30–G31, OAC discontinuation or change, and the end of the study period. A medication was deemed discontinued when the prescription intervals exceeded 3 months or when the medication was switched to another OAC. Deceased patients were considered as censor cases. The non-OAC group was followed from AF diagnosis to the diagnosis of dementia or the end of the study period. The ICD-10 codes F00–F03 and G30–G31 defined the following dementias: dementia in Alzheimer’s disease, vascular dementia, dementia in other diseases classified elsewhere, unspecified dementia, Alzheimer’s disease, other degenerative diseases of the nervous system, not elsewhere classified. Patient characteristics were determined from the database during the baseline period, i.e., 12 months prior to AF diagnosis. The patient selection flowchart is presented in Fig. 2.
2.4 Adherence
The medication possession ratio (MPR), which was calculated as the total duration of supply (days) of the prescribed drug divided by the number of days from the first prescription date to the end date of the last prescription, was used as an indicator of medication adherence (“Appendix 1”). The MPR reflected whether anticoagulants were prescribed or dispensed but not whether patients actually took them. Although the MPR cannot directly evaluate adherence, there are days when patients with an MPR < 100% cannot take the medication because OACs cannot be purchased without a prescription in Japan. Although this is not a direct indicator of compliance, we considered it an indirect indicator. Patients with an MPR of 0 were categorized into the non-OAC group.
2.5 Variables for Propensity Score Matching
Propensity score matching was performed to balance confounding factors between the OAC and non-OAC groups. Factors associated with the development of dementia, (age; sex; comorbidities; diagnosis of stroke, systemic emboli, or transient ischemic attack; cancer; ischemic stroke; intracerebral hemorrhage; other intracranial bleed; myocardial infarction; peripheral artery disease; vascular disease; heart failure; any valvular disease; hypertension; diabetes; renal disease; liver disease; bleeding; venous thromboembolism; hypothyroidism; osteoarthritis; chronic obstructive pulmonary disease; alcohol index; pneumonia; thyrotoxicosis; Parkinson’s disease; and prescription of an antiplatelet agent, angiotensin-converting enzyme inhibitor or angiotensin-receptor blocker, diuretic, statin, nitrates, β-blocker, antiarrhythmic drug class 1 or 3, digoxin) were included as covariates for calculating propensity scores. The comorbidities were used the ICD-10 codes defined by Friberg and Rosenqvist [9]. We extracted from the database the covariates of the diagnoses and prescriptions within 12 months prior to the first diagnosis of AF. Individual propensity scores for the probability of OAC treatment were calculated using logistic regression, after which 1:1 propensity score-matched pairs were created by matching the OAC and non-OAC groups. A caliper of 0.2 on logit-transformed scores was used for propensity score matching. Differences in baseline characteristics between the OAC and non-OAC groups were evaluated using standardized differences. A standardized difference of <0.10 was used to indicate good balance between groups for a given covariate. Additionally, the 1:1 propensity score-matched pairs were created by matching the non-OAC group with the DOAC, WF group, and with the OAC, DOAC, or WF groups of patients with MPRs of ≥ 60%, ≥ 70%, ≥ 80%, and ≥ 90%.
2.6 Statistical Analysis
The incidence of dementia in the non-OAC group was compared with those in the OAC, DOAC, or WF groups, as well as with those in groups of patients with MPRs of ≥ 60%, ≥ 70%, ≥ 80%, and ≥ 90%. Crude incidence rates were expressed as rates per 1000 person-years. The 95% confidence interval (CI) of incidence rates was calculated using the Clopper–Pearson method. The incidence of dementia was compared between the OAC and non-OAC groups after propensity score matching, and the Cox proportional hazards regression model was used to estimate the risk of dementia for the OAC, DOAC, and WF groups. Similarly, the risk of dementia for the OAC, DOAC, and WF groups of patients with MPRs of ≥ 60%, ≥ 70%, ≥ 80%, and ≥ 90% was also estimated. We used the univariate Cox proportional hazards models to obtain the unadjusted hazard ratio (HR) for each group. The Kaplan–Meier method was performed to compare the incidence of dementia between the propensity score-matched OAC, DOAC, and WF groups and the non-OAC group using the log-rank test. Additionally, the Cox proportional hazards regression model and Kaplan–Meier method were used to investigate the risk of stroke between the MPR ≥ 90% OAC group and the non-OACs group.
Data extraction and management were performed using Visual Mining Studio software (version 8.0; Mathematical Systems, Inc., Tokyo, Japan). All analyses were conducted using JMP® version 14.2 (SAS Institute Inc., Cary, NC, USA), and a p-value of < 0.05 indicated statistical significance. Bonferroni’s correction was applied to the analyses of the association between dementia and OAC use.
3 Results
3.1 Patient Characteristics
The JMDC claims database included 26,526 patients with AF, of whom 8564 patients were excluded from the analysis. Ultimately, 17,962 patients who satisfied the selection criteria were included in the study. Among the included patients, 7895 (44.0%) were prescribed OACs (Fig. 2), with 6962 and 933 having been prescribed DOACs and WF, respectively. The baseline patient characteristics of the OAC and non-OAC groups are presented in Table 1. The mean ages of the OAC and non-OAC groups were 56.9 and 51.4 years, respectively. After propensity score matching, 5587 patients were selected from the OAC and non-OAC groups (Table 1); 5211 matched patients were selected from the DOAC and non-OAC groups (Table 2); and 873 matched patients were selected from the WF and non-OAC groups (Table 3). Sufficiently balanced cohorts were generated with a standardized difference of < 0.10 for almost all covariates. Additionally, sufficient balanced cohorts were generated using propensity score matching during the analysis of the OAC, DOAC, and WF groups limited to patients with MPRs of ≥ 60%, ≥ 70%, ≥ 80%, and ≥ 90%.
3.2 Outcomes
The number of events, follow-up duration, and incidence rates for dementia are summarized in Table 4. After propensity score matching, the crude incidence of dementia per 1000 person-years was 2.76 and 4.00 in the OAC and non-OAC groups, respectively, with the MPR ≥ 90% OAC group having the lowest crude incidence per 1000 person-years at 1.97. After analyzing the DOAC group, our findings showed a 3.14 and 3.69 crude incidence of dementia per 1000 person-years in the DOAC and non-OAC groups, respectively, with the MPR ≥ 90% DOAC group having the lowest crude incidence per 1000 person-years at 2.75. After analyzing the WF group, our findings showed a 3.69 and 5.47 crude incidence of dementia per 1000 person-years in the WF and non-OAC groups, respectively, with the MPR ≥ 90% WF group having a crude incidence per 1000 person-years of 3.32. Results of OAC and DOAC analyses showed that the groups with MPR ≥ 90% had the lowest crude incidences per 1000 person-years.
Table 4 details the results of Cox proportional hazards analysis. Although OAC administration was not associated with a lower risk of dementia (HR 0.66, 95% CI 0.40–1.08; p = 0.098), OAC administration in patients with MPR ≥90% was significantly associated with a lower risk of dementia (HR 0.45, 95% CI 0.25–0.81; p = 0.008). The DOAC (HR 0.80, 95% CI 0.48–1.34; p = 0.393) and WF (HR 0.68, 95% CI 0.23–1.98; p = 0.475) groups were not associated with the risk of dementia. Consequently, neither DOAC nor WF administration reduced the risk of dementia regardless of MPR. Additionally, no significant difference was found in the risk of dementia between OAC administration in patients with an MPR ≥ 90% and those with an MPR < 90%, between DOAC administration in patients with an MPR ≥ 90% and those with an MPR < 90%, and between WF administration in patients with an MPR ≥ 90% and those with an MPR < 90% (Table 5).
Figure 3 shows the Kaplan–Meier curves for the incidence of dementia in the MPR ≥ 90% OAC, DOAC, and WF groups. Accordingly, differences in the incidences of dementia were observed between the MPR ≥ 90% OAC and non-OAC groups (log-rank test: p = 0.006). Meanwhile, no difference in the incidence of dementia was noted between the MPR ≥ 90% DOAC and non-OAC groups (log-rank test: p = 0.250) and between the MPR ≥ 90% WF and non-OAC groups (log-rank test: p = 0.346).
In an additional analysis for stroke risk, OAC administration carried a significantly higher risk of stroke in the MPR ≥90% group than in the non-OAC group (HR 1.16, 95% CI 1.08–1.26; p < 0.001) (Table 6). Furthermore, OAC administration was linked to a significantly higher cumulative incidence of stroke in the MPR ≥ 90% group than in the non-OAC group (log-rank test: p < 0.001) (Fig. 4).
4 Discussion
The current study revealed that administration of OACs, be it DOAC or WF, did not reduce the risk of dementia in patients with nonvalvular AF. However, OAC administration with an adherence of MPR ≥ 90% reduced the risk of dementia among the same patients, suggesting that medication adherence may be a significant protective factor for dementia in patients with AF receiving OACs. In this study, MPR was used as the total duration of supply (days) of the prescribed drug divided by the number of days from the first prescription date to the end date of the last prescription. MPR is a commonly used calculation in health research and is supported by the International Society for Pharmaceutical and Outcomes Research [17,18,19].
In the separate analyses of DOAC and WF, administration in patients with an MPR ≥ 90% did not reduce the risk of dementia. Consequently, our study could not detect any difference in the effects of DOAC and WF on dementia prevention. Therefore, whether differences exist in the effects of WF and DOACs on dementia remains unclear. Indeed, several contradictory reports have been published on the association between OAC administration and the risk of dementia. Some studies reported that DOAC users had a lower risk of dementia than WF users [20, 21]. In contrast, studies in Sweden [9, 22], the UK [23], and Korea [7] showed that OACs, including DOACs and WF, reduced the risk of dementia. Among the aforementioned studies, the Sweden study alone accounted for adherence to medication [9, 22]. Therefore, it cannot be denied that the presence or absence of medication adherence consideration may affect the results.
Anticoagulant therapy with WF requires dose adjustment based on the prothrombin time-international normalized ratio (PT-INR) to ensure sufficient efficacy and to prevent adverse effects, including bleeding. Additionally, the time in therapeutic range (TTR) has been used to evaluate the quality of WF therapy. A study reported that patients with a high TTR had a lower risk of dementia [24]. Although PT-INR or TTR would be a relevant parameter for assessing adherence, these laboratory data were not included in the JMDC database.
The current study found fewer incident WF users than incident DOAC users. Notably, DOACs are easier to use than WF because the former does not require PT-INR measurements and have fewer interactions with drugs and food. Several recent treatment guidelines have recommended the use of DOACs instead of WF for anticoagulant therapy in patients with nonvalvular AF [25,26,27,28]. Meanwhile, a study in Japan showed that WF users had higher CHADS2 (congestive heart failure, hypertension, 75 years of age or older, diabetes mellitus, and previous stroke or transient ischemic attack) and HAS-BLED (hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile international normalized ratio, elderly (> 65 years), drugs/alcohol concomitantly) scores and several other comorbidities compared with DOAC users [29]. In Japan, WF is likely used more than DOACs in patients with severe AF. Therefore, the difference in dementia risk between WF and DOAC use in patients with AF needs to be carefully studied.
Aging is a significant risk factor for the development of dementia. In the study, the OAC and non-OAC groups had crude incidences of dementia of 2.76 and 4.00 per 1000 person-years, respectively, which were lower than previously reported data [7, 9, 22, 23]. The JMDC database contains claims data for relatively young working patients and their families collected from multiple health insurance associations. Consequently, the aforementioned database, which includes patients aged 0–75 years, demonstrated that the OAC and non-OAC groups had mean ages of 56.9 ± 9.5 and 51.4 ± 11.7 years, respectively. Conversely, Friberg and Rosenqvist [9] reported that the OAC and non-OAC groups had mean ages of 73.7 and 75.7 years, respectively, with Mongkhon et al. [23] reporting mean ages of 73.3 and 72.9 years, respectively, for the same groups. Although Kim et al. [7] did not provide patient background data for the OAC and non-OAC groups, the mean age of patients with AF included in their study was 70.7 years. The lower incidence of dementia obtained in this study than in previous studies may be attributable to our relatively young study population. Our study revealed that OAC therapy with high adherence reduced the risk of dementia even in relatively young patients, who had a lower risk of dementia.
One hypothesis suggests that effective anticoagulant therapy maintains cognitive function in patients with AF by reducing the risks of stroke and SCI. Indeed, a number of retrospective studies reported that OACs reduced the development of stroke or SCI and subsequently reduced the risk of dementia or cognitive impairment in patients with AF [8,9,10]. However, the study revealed that OAC administration was linked to a significantly higher risk of stroke in the MPR ≥ 90% group than in the non-OAC group, suggesting that OAC administration reduced the risk of dementia in patients with an MPR ≥ 90% regardless of the history of stroke. It is assumed that the patients with an MPR ≥ 90% may have a high risk of stroke. The increased risk of stroke associated with OAC administration in patients with an MPR ≥ 90% may be attributable to indication bias. Furthermore, it seemed paradoxical that the MPR ≥ 90% OAC group is associated with an increased risk of stroke, but a reduced risk of dementia. It is hypothesized that high adherence to OAC therapy in patients with a high risk of stroke contributes to the reduced risk of dementia by additional mechanisms other than stroke. Further studies are needed to evaluate this hypothesis.
The current study has several limitations worth considering when interpreting our results. First, MPR was used as an indirect indicator of adherence to anticoagulants. The study determined whether anticoagulants were prescribed or dispensed but not whether patients actually took them. Furthermore, the time-dependent variance of MPR was not considered in the study. Therefore, it remains unclear whether MPR can accurately determine adherence to anticoagulant therapy. Second, the study was performed using a claims database as secondary data. We note that the diagnosis stated in the claim could have been listed to justify the health insurance claim or that the diagnosis of AF or dementia using ICD-10 codes may be higher than that reported because of subclinical events. Although some studies reported that ICD-10 codes generally have high sensitivity and specificity [16, 30], it remains unclear whether ICD-10 code I48 accurately identifies AF in the JMDC claims database. Nevertheless, the JMDC claims database used in this study includes approximately 6 million insured individuals in Japan (approximately 5% of the population). Third, given that our study population comprised relatively young working adults and their family members, while patients aged > 75 years were not included, the results presented herein may not be applicable to all populations. Fourth, most patients were followed for approximately 2 years. This follow-up may not be sufficient to identify the full risk or benefit to OAC over a longer course. Lastly, the WF group was significantly smaller than the DOAC group. As a result, the HR estimates may be inaccurate owing to the limited sample size of subjects using WF.
5 Conclusion
This retrospective cohort study demonstrated that OAC use did not affect the risk of dementia among relatively young patients with AF. However, OAC administration reduced the risk of dementia in patients with an MPR ≥ 90%. Therefore, the association between OAC administration and dementia should be evaluated while considering medication adherence. Further studies are needed to investigate the differences between the effects of DOACs and WF on dementia.
References
JCS Joint Working Group. Guidelines for pharmacotherapy of atrial fibrillation (JCS 2013). Circ J. 2014;78:1997–2021. https://doi.org/10.1253/circj.CJ-66-0092.
Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–25. https://doi.org/10.1161/CIRCULATIONAHA.105.595140.
Aldrugh S, Sardana M, Henninger N, Saczynski JS, McManus DD. Atrial fibrillation, cognition and dementia: a review. J Cardiovasc Electrophysiol. 2017;28:958–65. https://doi.org/10.1111/jce.13261.
Bunch TJ, Weiss JP, Crandall BG, May HT, Bair TL, Osborn JS, et al. Atrial fibrillation is independently associated with senile, vascular, and Alzheimer’s dementia. Heart Rhythm. 2010;7:433–7. https://doi.org/10.1016/j.hrthm.2009.12.004.
Ott A, Breteler MM, de Bruyne MC, van Harskamp F, Grobbee DE, Hofman A. Atrial fibrillation and dementia in a population-based study. The Rotterdam Study. Stroke. 1997;28:316–21. https://doi.org/10.1161/01.STR.28.2.316.
Santangeli P, Di Biase L, Bai R, Mohanty S, Pump A, Cereceda Brantes M, et al. Atrial fibrillation and the risk of incident dementia: a meta-analysis. Heart Rhythm. 2012;9:1761–8. https://doi.org/10.1016/j.hrthm.2012.07.026.
Kim D, Yang PS, Yu HT, Kim TH, Jang E, Sung JH, et al. Risk of dementia in stroke-free patients diagnosed with atrial fibrillation: data from a population-based cohort. Eur Heart J. 2019;40:2313–23. https://doi.org/10.1093/eurheartj/ehz386.
Ding M, Fratiglioni L, Johnell K, Santoni G, Fastbom J, Ljungman P, et al. Atrial fibrillation, antithrombotic treatment, and cognitive aging: A population-based study. Neurology. 2018;91:e1732–40. https://doi.org/10.1212/WNL.0000000000006456.
Friberg L, Rosenqvist M. Less dementia with oral anticoagulation in atrial fibrillation. Eur Heart J. 2018;39:453–60. https://doi.org/10.1093/eurheartj/ehx579.
Mongkhon P, Naser AY, Fanning L, Tse G, Lau WCY, Wong ICK, et al. Oral anticoagulants and risk of dementia: A systematic review and meta-analysis of observational studies and randomized controlled trials. Neurosci Biobehav Rev. 2019;96:1–9. https://doi.org/10.1016/j.neubiorev.2018.10.025.
Ligthelm RJ, Borzi V, Gumprecht J, Kawamori R, Wenying Y, Valensi P. Importance of observational studies in clinical practice. Clin Ther. 2007;29:1284–92. https://doi.org/10.1016/j.clinthera.2007.07.004.
de Bruijn RF, Heeringa J, Wolters FJ, Franco OH, Stricker BH, Hofman A, et al. Association between atrial fibrillation and dementia in the general population. JAMA Neurol. 2015;72:1288–94. https://doi.org/10.1001/jamaneurol.2015.2161.
Ozaki AF, Choi AS, Le QT, Ko DT, Han JK, Park SS, et al. Real-world adherence and persistence to direct oral anticoagulants in patients with atrial fibrillation: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2020;13: e005969. https://doi.org/10.1161/CIRCOUTCOMES.119.005969.
Obamiro KO, Chalmers L, Lee K, Bereznicki BJ, Bereznicki LR. Adherence to oral anticoagulants in atrial fibrillation: an australian survey. J Cardiovasc Pharmacol Ther. 2018;23:337–43. https://doi.org/10.1177/1074248418770201.
Kimura S, Sato T, Ikeda S, Noda M, Nakayama T. Development of a database of health insurance claims: standardization of disease classifications and anonymous record linkage. J Epidemiol. 2010;20:413–9. https://doi.org/10.2188/jea.JE20090066.
Kokotailo RA, Hill MD. Coding of stroke and stroke risk factors using international classification of diseases, revisions 9 and 10. Stroke. 2005;36:1776–81. https://doi.org/10.1161/01.STR.0000174293.17959.a1.
Hess LM, Raebel MA, Conner DA, Malone DC. Measurement of adherence in pharmacy administrative databases: a proposal for standard definitions and preferred measures. Ann Pharmacother. 2006;40:1280–8. https://doi.org/10.1345/aph.1H018.
Halpern R, Agarwal S, Dembek C, Borton L, Lopez-Bresnahan M. Comparison of adherence and persistence among multiple sclerosis patients treated with disease-modifying therapies: a retrospective administrative claims analysis. Patient Prefer Adherence. 2011;5:73–84. https://doi.org/10.2147/PPA.S15702.
Sedjo RL, Cox ER. Lowering copayments: impact of simvastatin patent expiration on patient adherence. Am J Manag Care. 2008;14:813–8.
Chen N, Lutsey PL, MacLehose RF, Claxton JS, Norby FL, Chamberlain AM, et al. Association of oral anticoagulant type with risk of dementia among patients with nonvalvular atrial fibrillation. J Am Heart Assoc. 2018;7: e009561. https://doi.org/10.1161/JAHA.118.009561.
Jacobs V, May HT, Bair TL, Crandall BG, Cutler MJ, Day JD, et al. Long-term population-based cerebral ischemic event and cognitive outcomes of direct oral anticoagulants compared with warfarin among long-term anticoagulated patients for atrial fibrillation. Am J Cardiol. 2016;118:210–4. https://doi.org/10.1016/j.amjcard.2016.04.039.
Friberg L, Andersson T, Rosenqvist M. Less dementia and stroke in low-risk patients with atrial fibrillation taking oral anticoagulation. Eur Heart J. 2019;40:2327–35. https://doi.org/10.1093/eurheartj/ehz304.
Mongkhon P, Fanning L, Lau WCY, Tse G, Lau KK, Wei L, et al. Oral anticoagulant and reduced risk of dementia in patients with atrial fibrillation: A population-based cohort study. Heart Rhythm. 2020;17:706–13. https://doi.org/10.1016/j.hrthm.2020.01.007.
Madhavan M, Hu TY, Gersh BJ, Roger VL, Killian J, Weston SA, et al. Efficacy of warfarin anticoagulation and incident dementia in a community-based cohort of atrial fibrillation. Mayo Clin Proc. 2018;93:145–54. https://doi.org/10.1016/j.mayocp.2017.09.021.
Chiang CE, Okumura K, Zhang S, Chao TF, Siu CW, Wei Lim T, et al. 2017 consensus of the Asia Pacific Heart Rhythm Society on stroke prevention in atrial fibrillation. J Arrhythm. 2017;33:345–67. https://doi.org/10.1016/j.joa.2017.05.004.
Lip GYH, Banerjee A, Boriani G, Chiang CE, Fargo R, Freedman B, et al. Antithrombotic therapy for atrial fibrillation: CHEST guideline and expert panel report. Chest. 2018;154:1121–201. https://doi.org/10.1016/j.chest.2018.07.040.
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation. 2019;140:e125–51. https://doi.org/10.1161/CIR.0000000000000665.
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;42:373–498. https://doi.org/10.1093/eurheartj/ehaa612.
Yamashita Y, Uozumi R, Hamatani Y, Esato M, Chun YH, Tsuji H, et al. Current status and outcomes of direct oral anticoagulant use in real-world atrial fibrillation patients- fushimi AF registry. Circ J. 2017;81:1278–85. https://doi.org/10.1253/circj.CJ-16-1337.
Yagi N, Suzuki S, Nagai K, Tanaka T, Nagahama T, Arita T, et al. Current status of oral anticoagulant adherence in Japanese patients with atrial fibrillation: a claims database analysis. J Cardiol. 2021;78:150–6. https://doi.org/10.1016/j.jjcc.2021.02.007.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by JSPS KAKENHI (grant numbers: JP16K09084, JP18K06805 and JP19K16461) in Japan.
Conflicts of interest
Yuika Komatsu, Satoshi Yokoyama, Kouichi Hosomi, and Mitsutaka Takada declare they have no conflicts of interest.
Ethics approval
This study was approved by the Ethics Committee of Kindai University School of Pharmacy (approval number: 17-112).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Informed consent
Informed consent was not required for this study since all personal names and identification numbers from the JMDC claims database were replaced by a univocal numerical code.
Data availability
The data that support the findings of this study are available at https://www.jmdc.co.jp/, with the permission from JMDC, Inc. Restrictions apply to the availability of these data, which were used under license for this study.
Code availability
Not applicable.
Author Contributions
All authors contributed to the study conception and design. Material preparation and data collection and analysis were performed by YK, SY, and KH. The draft of the manuscript was written by YK and MT. All authors commented on previous versions of the manuscript and read and approved the final manuscript.
Permission to Reproduce Material from Other Sources
Not applicable.
Appendix 1
Appendix 1
MPR
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Komatsu, Y., Yokoyama, S., Hosomi, K. et al. Impact of Medication Adherence on the Association Between Oral Anticoagulant Use and Risk of Dementia: A Retrospective Cohort Study using the Japanese Claims Database. Drugs - Real World Outcomes 9, 437–449 (2022). https://doi.org/10.1007/s40801-022-00311-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-022-00311-9