Abstract
Background
Direct oral anticoagulants are available for patients with atrial fibrillation.
Objective
This study compared adherence and persistence of once-daily (QD) vs twice-daily (BID) direct oral anticoagulants in patients with atrial fibrillation.
Methods
A cohort study was conducted in three databases in the Netherlands, Italy and Germany. Patients with AF starting direct oral anticoagulants after drug approval date were included. The index date was the date of first dispensing. Study patients were restricted to those aged ≥ 18 years, ≥ 1 year database history and ≥ 1 year follow-up. Adherence to treatment was defined as the proportion of days covered ≥ 80% between the index date and the date of last dispensing of the index regimen (i.e. exposure period). The proportion of days covered was also determined during the 12-month follow-up. Persistence was defined as continuous use from index to treatment discontinuation.
Results
In the Netherlands, Italy and Germany, respectively, 6068, 32,260 and 167,445 patients were included. The mean age of the patients was 70, 77 and 74 years, and 31%, 40% and 61% were QD users, all respectively. Among QD/BID users, 93/90%, 88/86% and 77/58%, respectively were adherent during the exposure period. Persistence rates at 1 year in QD/BID users were 60/59%, 13/14% and 46/31%, respectively.
Conclusions
Adherence to treatment was high. In Germany, adherence was markedly higher in QD users compared with BID users. In Italy and the Netherlands, these differences were marginal. Persistence was low in all countries, but discontinuation was temporary. Only in Germany, persistence was markedly lower in BID users vs QD users.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adherence and persistence of direct oral anticoagulants (DOACs) were assessed in patients with atrial fibrillation. A comparison was made between once-daily and twice- daily DOACs. |
Overall, patients with atrial fibrillation were very adherent to their DOAC treatment. |
Patients with atrial fibrillation discontinued often with DOAC treatment. However, discontinuation was mostly temporary. |
1 Introduction
Non-valvular atrial fibrillation (AF) is the most common sustained rhythm disorder. It has long been identified as a significant risk factor for disabling or fatal ischaemic stroke and systemic embolism [1]. The risk of stroke in AF is reduced by antithrombotic therapy, specifically vitamin K antagonists (VKAs, e.g. warfarin) or the direct oral anticoagulants (DOACs) [2, 3].
Based on the results of multiple randomised controlled trials, DOACs are now frequently used to reduce stroke risk in patients with AF [4,5,6]. Favorable risk-benefit profiles of DOACs compared with warfarin have been demonstrated with significant reductions in stroke, intracranial haemorrhage and mortality [7]. Additionally, DOACs compared with VKAs have gained increasing popularity because of no need for routine coagulation testing, improved patient convenience, greater predictability, faster onset of anticoagulation effect, and lower potential for food and drug interactions. Concerns however, have been raised regarding the heightened consequences of poor adherence and persistence to DOACs compared with warfarin [8, 9].
A high degree of adherence to DOACs is essential for reducing the risk of ischaemic stroke and systemic embolism in patients with AF, given the rapid decline in anticoagulation activity when doses are omitted [10]. In real-world settings, suboptimal medication adherence and persistence may attenuate the efficacy and safety estimates derived from randomised controlled trials, accounting for increased adverse outcomes and healthcare costs [11, 12].
Several factors may influence medication adherence and persistence. One factor is the complexity of the medication regimen. The daily dosing frequency is a domain of this complexity. Patients with cardiovascular disease often take multiple medications, including the use of combination products. The simplification of daily dosing frequency may improve drug adherence and persistence in patients with cardiovascular disease [13,14,15].
Direct oral anticoagulants are available as once-daily (QD) or twice-daily (BID) regimens. The QD vs BID dosage regimens have a number of practical implications. There is no guideline for healthcare providers for prescribing a specific DOAC regimen instead of another. Expert opinion recommends a QD dosage regimen DOAC in patients who prefer a low pill burden [16]. Contemporary studies assessing treatment adherence by QD or BID DOAC regimens are few and limited in size [17]. The objective of the present study is to assess, in three large real-life samples of patients with AF, the adherence, persistence and switching patterns of QD vs BID regimens in three different European countries.
2 Methods
2.1 Data Sources
For this study, we used three different databases; healthcare records from the PHARMO Database Network in the Netherlands (7 million residents), the Italian Agenzia regionale di sanità della Toscana database [ARS] (3.7 million residents) and the German Pharmacoepidemiological Research Database [GePaRD] (25 million insurants/insured persons). The databases are described in detail elsewhere [18,19,20]. All three databases contain dispensings from out-patient pharmacies. In GePaRD and ARS, the dispensing is recorded with a national coding system that is linked to the number of pills, and to the Anatomical Therapeutic Chemical (ATC) code of the active principle. In PHARMO, all information is available in the dispensing records. All three databases contain medical diagnostic data recorded during inpatient care, registered in International Classification of Diseases, Ninth Revision codes in ARS and PHARMO and in International Classification of Diseases, Tenth Revision codes in GePaRD and PHARMO. In addition, the PHARMO and GePaRD databases contain medical diagnostic information recorded during outpatient care.
2.2 Study Design and Patient Selection
A retrospective observational cohort study was performed. All patients meeting the inclusion criteria and receiving a DOAC (Table 1 of the Electronic Supplementary Material [ESM]) starting from the approval date by the Committee for Medicinal Products for Human Use for the AF indication (14 April, 2011 for dabigatran, 22 September, 2011 for rivaroxaban, 20 September, 2012 for apixaban and 23 April, 2015 for edoxaban) until the end of database availability (31 December, 2016 in GePaRD, 31 December, 2017 in PHARMO and 31 December, 2018 in ARS) were analysed. The date of first dispensing of a DOAC was defined as the index date. Direct oral anticoagulant use was based on both general practitioner-prescribed and specialist-prescribed DOACs, dispensed from out-patient pharmacies. Patients were followed from the index date to the end of data collection (e.g. patient moved out of catchment area/ended insurance), death or end of database availability, whichever occurred first.
Inclusion criteria: adult patients (≥ 18 years at the index date); at least 1 year of database history at the index date; new users, i.e. no previous DOAC dispensing in the year before the index date, no multiple different DOACs on the index date and no VKA dispensing on the index date; at least 1 year of follow-up after the index date; AF diagnosis ever before the index date (diagnosis codes are included in Table 1 of the ESM). Atrial fibrillation diagnoses were based on general practitioner records (in PHARMO), on outpatient and hospital diagnoses (in GePaRD) and on hospital admissions (in GePaRD and ARS). The QD or BID regimen was defined based on the prescribed dosage regimen in PHARMO; based on the index drug (edoxaban and rivaroxaban: QD; apixaban and dabigatran: BID) in GePaRD and ARS, as the prescribed dosage regimen was unavailable.
2.3 Patient Characteristics
Baseline factors (i.e. sex, age and available follow-up) were determined. Based on out-patient dispensing records, VKA treatment in the year prior to the index date, polypharmacy (i.e. the number of all different pharmacological subgroups [ATC third level] excluding antithrombotic agents [ATC B01A]), and use of lipid-lowering, antihypertensive, antidiabetic and anti-arrhythmic drugs were assessed in the 3 months before the index date (Table 1 of the ESM).
2.4 Adherence and Persistence of DOAC Use
Direct oral anticoagulant dispensings were converted into treatment episodes of uninterrupted use based on the method of Catalan [21]: in the case of gaps between DOAC dispensings, use of the respective DOAC was considered uninterrupted if the gap lasted less than half the preceding dispensing period, with a minimum of 7 days. The end date of an episode was defined as the date of the last dispensing after uninterrupted use (i.e. the duration of this last dispensing, excluding the permissible gap). Patients could have several treatment episodes. In the case of switching of a dosage regimen, the respective DOAC episode was censored (i.e. days of overlap in dispensing of different DOACs were not counted). Switching within a dosage regimen was allowed.
Switching patterns were assessed from the day after the index date until the end of the follow-up based on DOAC treatment episodes. Switching was defined as either a dosage regimen switch or a cluster switch (i.e. to another DOAC with the same dosage regimen). For the assessment of adherence and persistence by dosage regimen, switches within the QD or BID clusters were allowed.
Given the aforementioned method, adherence was defined based on the proportion of days covered (PDC) during the exposure period (i.e. between first and last dispensing within the index dosage regimen). Considering the varying length of follow-up within the study population, the PDC was also determined during the first year of follow-up. Among patients with more than one dispensing, the PDC was calculated as the total days of supply divided by the number of days in the exposure period. The PDC values range from 0 to 1, with higher values indicating better adherence. Adherent patients were defined as those with PDC ≥ 0.8 [22].
Persistence was defined as the time from the index date to the first treatment regimen discontinuation and was based on DOAC treatment episodes. With this definition, persistence did not necessarily mean permanent but also temporary discontinuation.
2.5 Sensitivity Analyses
Several sensitivity analyses were performed to study bias that may result from the different nature of the included databases. First, in Germany and the Netherlands, we adjusted the study population to hospital-diagnosed AF only, to create more comparable study populations. For the Netherlands, this meant a new selection for the AF study patients, as hospital data were not used in the main analyses. In Germany, the source population from the main study was limited to patients with hospital-diagnosed AF. Second, we assessed the impact on persistence of varying permissible gaps between dispensings in the calculation of treatment episodes of uninterrupted DOAC use. We assessed a permissible gap between dispensings of 30 and 90 days (i.e. a treatment episode would be considered as uninterrupted if the duration of the gap was less than 30 or 90 days).
2.6 Subgroup Analyses
As medication adherence and persistence might be influenced by several factors (i.e. age, sex, comorbidities, polypharmacy, CHA2DS2-VASc score), we performed exploratory subgroup analyses of adherence and persistence for age (categorised as age <65, 65–74, ≥75 years), CHA2DS2-VASc (categorised as CHA2DS2-VASc <2, 2–5, >5), sex, co-medication (lipid-modifying and anti-hypertensive drugs), polypharmacy (categorised as <5, 6–7, ≥8) and comorbidities (depression, cancer, ischaemic stroke, chronic heart failure) [8, 23, 24].
2.7 Additional Analyses
We have performed all analyses described in “Statistical analysis” in the InGef database (Institut für angewandte Gesundheitsforschung Berlin GmbH) in Germany as well, to add more data for patients on edoxaban (i.e. most recent approved DOAC) and see whether results were similar in more recent years. The InGef database is an anonymised healthcare claims database with longitudinal data from approximately 8 million German insured members of one of more than 60 German statutory health insurance providers currently contributing data to the database (mainly company or guild health insurances). InGef, data between 2013 and 2018 was used. Atrial fibrillation diagnoses were based on primary and secondary care records.
2.8 Statistical Analysis
Measures of adherence, persistence and switching patterns were compared between QD and BID DOAC users by means of chi-square tests for categorical variables and analysis of variance tests for continuous variables. Persistence over time is presented in a Kaplan–Meier persistence curve, stratified by database and index dosage regimen.
Analyses were performed per database. All data were structured to a study-specific common data model in order to apply identical analytical programmes across databases. All analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) in the Netherlands and Germany. In Italy, R was used for data processing and analyses.
3 Results
Table 1 presents the selection of the study population in the Netherlands, Italy and Germany. In the Netherlands, 1907 patients (31%) used a QD dosage regimen and 4161 patients (69%) used a BID regimen. In Italy, there were 13,017 patients (40%) and 19,243 patients (60%), respectively. In Germany, 102,422 patients (61%) used a QD dosage regimen and 65,023 patients (39%) used a BID regimen.
Table 2 shows that the mean age was 70 years in the Netherlands, 77 years in Italy and 74 years in Germany. Median follow-up (i.e. available database follow-up) was 2.1–2.8 years in all databases.
In all databases, rivaroxaban (the first approved DOAC among the QD group) was the most frequently used drug at the index date (76–99%) among users in the QD group. In the Netherlands and Germany, edoxaban was used by only 1–3% of the patients in the QD group; in Italy, which provided the most recent data, it was used by 24%. In the BID group, dabigatran was the most frequently used drug at the index date (74%) in the Netherlands; in Germany, it was apixaban (63%); in Italy, apixaban and dabigatran were used equally frequently. Patient characteristics were equally distributed between dosage regimen groups. Study populations were slightly different among databases. In the Netherlands, the proportion of male patients was higher, patients were younger, and there was less polypharmacy compared with patients in Germany and Italy. With only hospital-diagnosed patients with AF, Italy had a study population with more severely diseased patients (i.e. older patients and more polypharmacy compared with the other databases). Indeed, sensitivity analyses in the Netherlands and Germany, with only hospital-diagnosed patients with AF, showed an increased frequency of polypharmacy (Table 4 of the ESM vs Table 2).
3.1 Adherence
In the Netherlands, during the first 12 months of treatment, 93% of the QD users was adherent to DOAC treatment. During the total exposure period, 94% of the QD users was adherent to DOAC treatment (Table 3). These proportions were slightly, but significantly lower among BID users. Ninety percent of the BID users was adherent to DOAC treatment during the exposure period. This was 91% of the BID users during the first 12 months of follow-up (p < 0.05). In Italy, 88% of the QD users was adherent to treatment during the exposure period and 89% was adherent to treatment during the first 12 months of follow-up. This was also slightly but significantly lower among BID users (86% during the exposure period and 88% during 12 months of follow-up) [p < 0.05]. In Germany, 77% of the QD users was adherent to treatment during the exposure period and 82% of the QD users was adherent to treatment during 12 months of follow-up. This was significantly lower among BID users (58% during the exposure period and62% during 12 months of follow-up) [p < 0.05]. Sensitivity analyses based on hospital-diagnosed patients with AF only in Germany and PHARMO showed similar adherence results compared to the analyses in the main study (Table 5 of the ESM). Subgroup analyses showed lower adherence rates for BID users among older patients compared with younger patients in Germany. In Germany, during the total exposure period, 50% of BID users aged ≥ 75 years was adherent and 69% of BID users aged < 65 years was adherent. Among QD users, this was 74% and 78%, respectively, which shows that adherence rates were higher and differences between subgroups were smaller among QD users. Furthermore, the exploratory subgroup analyses showed lower adherence rates for BID users among female patients, higher CHA2DS2-VASc score patients compared with male patients and lower CHA2DS2-VASc score patients in Germany, but not in the Netherlands and Italy (Tables 6 and 7 of the ESM).
3.2 Persistence
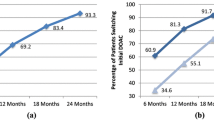
In the Netherlands, 84% of QD users and 83% of BID users had uninterrupted treatment after 3 months of follow-up. After 12 months, this was 60% and 59%, respectively (Table 3). The Kaplan–Meier curves (Fig. 1) show a slightly higher proportion of persistent users in the QD group compared with the BID group from 16 months of follow-up onwards.
In Italy, 45% of the QD users and 43% of the BID users were still using the initial dosage regimen after 3 months of follow-up. After 12 months, this was 13% and 14%, respectively. The Kaplan–Meier curves (Fig. 1) show no difference in the proportion of persistent users among the QD group and BID group during follow-up. Several sensitivity analyses were performed to explain the low persistence rates here. As 86–88% of the patients had a PDC of ≥0.8 and only 43–45% were persistent after 3 months of treatment, we surmised that patients only discontinued temporarily and re-started their treatment after a short period again. Sensitivity analyses using a different definition for treatment episodes showed higher persistence rates. After considering a treatment episode as uninterrupted if the gap between two dispensings was less than 30 days, 23% of the QD users and 25% of the BID users was persistent after 12 months of follow-up. A maximum gap between two dispensings of 90 days showed persistence rates of 69% and 75%, respectively. In this sensitivity analysis, the results were comparable among all three databases (Table 2 of the ESM).
In Germany, 78% of the QD users and 56% of the BID users were still using the initial dosage regimen after 3 months of follow-up. After 12 months, this was 46% and 31%, respectively. Persistence rates at all timepoints were significantly higher among QD users compared with BID users (p < 0.05). The Kaplan–Meier analysis illustrates this difference (Fig. 1). In all countries, the sensitivity analyses showed comparable persistence rates between QD and BID users when a maximum gap of 90 days was allowed between two dispensings. This result was observed especially in Germany. It seems that the effect of a higher persistence rate among QD users disappeared when the allowed gap between dispensings was very long.
Sensitivity analyses based only on hospital-diagnosed patients with AF in Germany and the Netherlands showed similar persistence results. Subgroup analyses showed no large differences in persistence among different subgroups (Tables 2–7 of the ESM).
3.3 Switching Patterns
In all databases, the majority of patients (about 90%) did not switch from one DOAC to another during the follow-up. Among the switchers, the largest part of the patients switched dosage regimens. Only a few patients (< 0.5% of the switchers) switched within the same dosage regimen.
3.4 Additional Analyses
In the InGef database, 55,509 DOAC users were included in the study population, with 28,065 (51%) users with a QD dosage regimen and 27,444 (49%) users with a BID regimen. Because a more recent data cut was used in this analysis, more patients with edoxaban (QD) [i.e. most recent approved DOAC] were included. Compared to the data from GePaRD, the proportion of QD users was lower (51% in InGef vs 61% in GePaRD). Adherence rates were slightly lower among patients in InGef compared with patients in GePaRD; however, the significant difference between QD and BID still existed. Persistence results were consistent with the GePaRD results in this study (Table 8 of the ESM).
4 Discussion
The present study was conducted in 205,773 AF new users of DOACs in the Netherlands, Italy and Germany between 2011 and 2018. To our knowledge, it represents the largest study of its type, being at least one order of magnitude larger than previous studies [17]. Across the three European countries, adherence was significantly lower with BID vs QD regimens, with marginal differences in the Netherlands and Italy, but marked in Germany, where formal nonadherence to BID regimens was reached (i.e. PDC <0.8) [22]. Persistence decreased over time in all countries; it was consistently lower with BID vs QD regimens in Germany, but not in the Netherlands and Italy. Highest adherence and persistence levels were observed in the Netherlands, compared to Italy and Germany.
Some studies investigated DOAC medication adherence and the number of daily doses among patients with AF. High adherence rates with DOAC use were observed and there was a 6.9% difference in favour of QD compared with BID dosing regimens observed among patients with long-term cardiovascular medication use [25,26,27]. In patients with venous thromboembolism (VTE), an approximately 39–61% higher likelihood of being adherent compared with patients on BID dosing regimens was observed [14]. These results are in line with our study on patients with AF, although we observed smaller differences in the Netherlands and Italy. Smaller differences in the Netherlands might be explained by the fact that in general adherence rates were very high. Patients in the Netherlands are regularly seen by their healthcare provider, resulting in a better control of patients who take DOACs. Patients in the Netherlands were also younger and had less polypharmacy, which might have contributed to the higher adherence. Furthermore, the lower adherence in Germany is similar to previous research, where high adherence (medication possession ratio (MPR) ≥0.80) was observed in 61.4% of rivaroxaban users and in 49.5% of dabigatran users [28].
We observed clinically relevant, higher persistence rates among QD users compared with BID users during the entire follow-up in Germany, and no or only marginal differences in the Netherlands and Italy. Koziel et al. assessed patients in the phase III GLORIA-AF registry, and also found similar persistence rates for QD and BID users; the proportion of patients persisting on DOAC therapy for 1 year was 79.5% among those using the QD regimen and 80.6% with the BID regimen [17]. Another study found marginal differences, with 63.6% of patients persisting at 6 months among those using dabigatran (BID) and 68.1% of patients persisting among those using rivaroxaban (QD) [12]. A retrospective analysis from the Danish National Patients Registry found that after 1 year, 85% of dabigatran-treated (BID) patients showed persistence whereas this was 90% for rivaroxaban-treated (QD) patients. However, also among apixaban-treated (BID) patients, 90% showed persistence [29].
Low persistence rates in Italy presumably related to the unique DOAC dispensing rules in Italy, which trigger a signal of non-persistence when using the method of Catalan. According to the method of Catalan, a treatment episode ends regardless of whether the patient refilled DOAC a bit later than the maximum allowed gap or permanently stopped. As the adherence rates were high in Italy, we surmise that interruptions were short and true non-persistence was low.
Sensitivity analyses were performed with a fixed permissible gap between dispensings in all three databases. In previous studies [30], results became more stable after applying a 90-day gap. In our study, after applying sensitivity analyses with a permissible gap of 90 days between the dispensings, the results became more comparable to the other databases as well. One year persistence rates were 69–72% in Italy, which was comparable to the other databases in this analysis.
Medication adherence and persistence are different for some demographic factors (e.g. age, sex and education level), comorbidities, higher polypharmacy, CHA2DS2-VASc score, behavioural factors or patient unawareness of the risks and benefits related to drug use and discontinuation [8, 23, 24].
Polypharmacy and co-medication were equally distributed among the dosage regimen groups. We assessed adherence and persistence among subgroups in exploratory subgroup analyses. Adherence rates were lower in BID users among older patients and comorbid patients, as well as female patients and patients with a higher CHA2DS2-VASc score in Germany, which is in line with the literature [8, 23, 24]. In the Netherlands and Italy, no large differences between subgroups were observed, which might be explained by the smaller study populations in these databases. Persistence did not differ among subgroups. The difference in persistence with DOAC treatment among QD users compared with BID users remained within the subgroups.
Our analyses contributed to the importance of assessing adherence and persistence. A high degree of adherence to DOACs is essential for reducing the risk of ischaemic stroke and systemic embolism in patients with AF, given the rapid decline in anticoagulation activity when doses are omitted [10]. Our analysis demonstrates that a QD regimen can help patients taking DOACs to be more adherent than with BID regimens, as adherence was higher among QD users compared with BID users, especially in Germany. This benefit is observed in older patients, patients with comorbidities, those using multiple drugs and those with a higher CHA2DS2-VASc score in Germany as well.
There is no guideline for healthcare providers for prescribing a specific DOAC regimen instead of another. The choice of the dosing regimen may depend on a clinician’s preference, a patient’s preference, and a patient’s characteristics and as a result it varies case by case. However, suboptimal treatment persistence is a major concern. This is a particular concern for elderly patients with AF, who are at a greater risk of both ischaemic and bleeding events than younger patients [31, 32].
Because a good adherence is associated with better outcomes, QD DOACs may be an appropriate choice for elderly patients, although the treating physician should also be aware of other criteria, such as the patient risk profile, comorbidities and concomitant medications. All these factors must be carefully considered on an individual basis for appropriately matching a DOAC to a particular patient.
A limitation of this study was that the Catalan method for persistence calculation seemed not the right method for Italy; treatment episodes ended after a short period of follow-up and persistence rates became low. However, sensitivity analyses were performed with a longer permissible gap between DOAC dispensings. Another limitation in calculating adherence and persistence with dispensing data is that we never know the real intake of a medicine. We can assume that patients started using the drug at the dispensed day, but we do not know whether a gap of several days means that a patient did not take the drug at separate days or over a period of several days. However, we based our calculations on dispensing dates from the outpatient pharmacies, and when next dispensings were recorded, we can assume that patients continued their medication intake. Furthermore, with the exclusion of patients with less than 1 year of follow-up available, we excluded the patients who died within a year of follow-up. This might have caused selection bias, as more healthy patients were selected in this manner, which may have slightly affected adherence rates. Last, no matching was applied for the potential differences between the QD and BID users. This is a limitation of the study, as potential baseline differences could be addressed with this.
An important strength of our study is that we used data from unselected populations from three different countries. Data were extracted locally and transformed into a common data model. Aggregated data were created on site for each database by using a shared programme. In addition, this study included a large cohort of DOAC users, to our knowledge being at least one order of magnitude larger than previous studies [17]. Healthcare records from multiple settings of care were combined to be able to take many medical factors into account, such as comorbidities and co-medications.
We are working on a follow-up research in which stroke outcomes were included, which was beyond the scope of the current paper. A scientific paper is currently under development. Furthermore, other factors (besides demographic factors, comorbidities and polypharmacy) that might contribute to the proportion of patients with AF not gaining the full benefit of DOAC treatment are eligible patients who were not prescribed a DOAC or patients not filling the first prescription. Future research could focus on assessing these factors.
5 Conclusions
Adherence to treatment was high in all three countries. In Germany, adherence was markedly higher in QD users compared with BID users. In Italy and the Netherlands, these differences were marginal. Persistence was low in all countries, but discontinuation was mostly temporary. In Germany, persistence was markedly lower in BID users vs QD users.
References
Björck S, Palaszewski B, Friberg L, Bergfeldt L. Atrial fibrillation, stroke risk, and warfarin therapy revisited: a population-based study. Stroke. 2013;44(11):3103–8. https://doi.org/10.1161/strokeaha.113.002329.
Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33(21):2719–47. https://doi.org/10.1093/eurheartj/ehs253.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1-76. https://doi.org/10.1016/j.jacc.2014.03.022.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51. https://doi.org/10.1056/NEJMoa0905561.
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92. https://doi.org/10.1056/NEJMoa1107039.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91. https://doi.org/10.1056/NEJMoa1009638.
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–62. https://doi.org/10.1016/s0140-6736(13)62343-0.
Raparelli V, Proietti M, Cangemi R, Lip GY, Lane DA, Basili S. Adherence to oral anticoagulant therapy in patients with atrial fibrillation: focus on non-vitamin K antagonist oral anticoagulants. Thromb Haemost. 2017;117(2):209–18. https://doi.org/10.1160/th16-10-0757.
Forslund T, Wettermark B, Hjemdahl P. Comparison of treatment persistence with different oral anticoagulants in patients with atrial fibrillation. Eur J Clin Pharmacol. 2016;72(3):329–38. https://doi.org/10.1007/s00228-015-1983-z.
Alberts MJ, Peacock WF, Fields LE, Bunz TJ, Nguyen E, Milentijevic D, et al. Association between once- and twice-daily direct oral anticoagulant adherence in nonvalvular atrial fibrillation patients and rates of ischemic stroke. Int J Cardiol. 2016;215:11–3. https://doi.org/10.1016/j.ijcard.2016.03.212.
Deshpande CG, Kogut S, Willey C. Real-world health care costs based on medication adherence and risk of stroke and bleeding in patients treated with novel anticoagulant therapy. J Manag Care Spec Pharm. 2018;24(5):430–9. https://doi.org/10.18553/jmcp.2018.24.5.430.
Jackevicius CA, Tsadok MA, Essebag V, Atzema C, Eisenberg MJ, Tu JV, et al. Early non-persistence with dabigatran and rivaroxaban in patients with atrial fibrillation. Heart. 2017;103(17):1331–8. https://doi.org/10.1136/heartjnl-2016-310672.
Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23(8):1296–310.
Laliberté F, Bookhart BK, Nelson WW, Lefebvre P, Schein JR, Rondeau-Leclaire J, et al. Impact of once-daily versus twice-daily dosing frequency on adherence to chronic medications among patients with venous thromboembolism. Patient. 2013;6(3):213–24. https://doi.org/10.1007/s40271-013-0020-5.
Bae JP, Dobesh PP, Klepser DG, Anderson JD, Zagar AJ, McCollam PL, et al. Adherence and dosing frequency of common medications for cardiovascular patients. Am J Manage Care. 2012;18(3):139–46.
Ageno W, Beyer-Westendorf J, Rubboli A. Once- versus twice-daily direct oral anticoagulants in non-valvular atrial fibrillation. Expert Opin Pharmacother. 2017;18(13):1325–32. https://doi.org/10.1080/14656566.2017.1361405.
Kozieł M, Mazurek M, Teutsch C, Diener HC, Dubner SJ, Halperin JL, et al. Persistence with anticoagulation for atrial fibrillation: report from the GLORIA-AF phase III 1-year follow-up. J Clin Med. 2020;9(6):1969. https://doi.org/10.3390/jcm9061969.
Haug U, Schink T. German Pharmacoepidemiological Research Database (GePaRD). In: Sturkenboom M, Schink T, editors. Databases for pharmacoepidemiological research. Springer Series on Epidemiology and Public Health. New York: Springer; 2020.
Trifirò G, Gini R, Barone-Adesi F, Beghi E, Cantarutti A, Capuano A, et al. The role of European healthcare databases for post-marketing drug effectiveness, safety and value evaluation: where does Italy stand? Drug Saf. 2019;42(3):347–63. https://doi.org/10.1007/s40264-018-0732-5.
Kuiper JG, Bakker M, Penning-van Beest FJA, Herings RMC. Existing data sources for clinical epidemiology: the PHARMO Database Network. Clin Epidemiol. 2020;12:415–22. https://doi.org/10.2147/clep.S247575.
Catalan VLJ. Predictors of long-term persistence on statins in a subsidized clinical population. Value Health. 2000;3(6):417–26. https://doi.org/10.1046/j.1524-4733.2000.36006.x.
Choudhry NK, Shrank WH, Levin RL, Lee JL, Jan SA, Brookhart MA, et al. Measuring concurrent adherence to multiple related medications. Am J Manag Care. 2009;15(7):457–64.
Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother. 2011;9(1):11–23. https://doi.org/10.1016/j.amjopharm.2011.02.004.
Rolnick SJ, Pawloski PA, Hedblom BD, Asche SE, Bruzek RJ. Patient characteristics associated with medication adherence. Clin Med Res. 2013;11(2):54–65. https://doi.org/10.3121/cmr.2013.1113.
Coleman CI, Roberts MS, Sobieraj DM, Lee S, Alam T, Kaur R. Effect of dosing frequency on chronic cardiovascular disease medication adherence. Curr Med Res Opin. 2012;28(5):669–80. https://doi.org/10.1185/03007995.2012.677419.
Vrijens B, Heidbuchel H. Non-vitamin K antagonist oral anticoagulants: considerations on once- vs. twice-daily regimens and their potential impact on medication adherence. Europace. 2015;17(4):514–23. https://doi.org/10.1093/europace/euu311.
Borne RT, O’Donnell C, Turakhia MP, Varosy PD, Jackevicius CA, Marzec LN, et al. Adherence and outcomes to direct oral anticoagulants among patients with atrial fibrillation: findings from the veterans health administration. BMC Cardiovasc Disord. 2017;17(1):236. https://doi.org/10.1186/s12872-017-0671-6.
Beyer-Westendorf J, Ehlken B, Evers T. Real-world persistence and adherence to oral anticoagulation for stroke risk reduction in patients with atrial fibrillation. Europace. 2016;18(8):1150–7. https://doi.org/10.1093/europace/euv421.
Lamberts M, Staerk L, Olesen JB, Fosbøl EL, Hansen ML, Harboe L, et al. Major bleeding complications and persistence with oral anticoagulation in non-valvular atrial fibrillation: contemporary findings in real-life Danish patients. J Am Heart Assoc. 2017;6(2): e004517. https://doi.org/10.1161/jaha.116.004517.
Banerjee A, Benedetto V, Gichuru P, Burnell J, Antoniou S, Schilling RJ, et al. Adherence and persistence to direct oral anticoagulants in atrial fibrillation: a population-based study. Heart. 2020;106(2):119–26. https://doi.org/10.1136/heartjnl-2019-315307.
Cavallari I, Patti G. Efficacy and safety of oral anticoagulation in elderly patients with atrial fibrillation. Anatol J Cardiol. 2018;19(1):67–71. https://doi.org/10.14744/AnatolJCardiol.2017.8256.
Patti G, Cavallari I, Hanon O, De Caterina R. The safety and efficacy of non-vitamin K antagonist oral anticoagulants in atrial fibrillation in the elderly. Int J Cardiol. 2018;265:118–24. https://doi.org/10.1016/j.ijcard.2018.02.066.
Acknowledgements
The authors thank all the healthcare providers contributing information to the PHARMO Database Network, the Italian Agenzia regionale di sanità della Toscana database (ARS) and the German Pharmacoepidemiological Research Database (GePaRD). The authors also thank Dominik Beier and Dirk Enders from the InGef database (Institut für angewandte Gesundheitsforschung Berlin GmbH) in Germany for performing the additional analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Daiichi Sankyo Europe GmbH. The authors had complete autonomy in the process of establishing the protocol, carrying out the analyses, and interpreting the results and the authors retained the full right to publish the results without limitation.
Conflict of interest/competing interests
Elisabeth Smits, Eline Houben, Fernie Penning-van Beest and Ron Herings are employees of the PHARMO Institute for Drug Outcomes Research. This independent research institute performs financially supported studies for government and related healthcare authorities and pharmaceutical companies. Felicita Andreotti, Harry Crijns and Sylvia Haas report personal fees/advisory board fees from Daiichi Sankyo Europe during the conduct of the study. Tania Schink is working at an independent non-profit research institute, the Leibniz Institute for Prevention Research and Epidemiology, BIPS. Unrelated to this study, BIPS occasionally conducts studies financed by the pharmaceutical industry. Almost exclusively, these are post-authorisation safety studies requested by health authorities. The design and conduct of these studies as well as the interpretation and publication are not influenced by the pharmaceutical industry.
Ethics approval
This observational study analysed de-identified data from the PHARMO Database Network; therefore, the study was exempt from ethical review and informed consent was not required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The data in this study are available from the PHARMO Database Network. As restrictions apply to the availability of these data, they are not publicly available. Data can be made available from the PHARMO Database Network upon request.
Code availability
Not applicable.
Author contributions
All authors contributed to the study conception and design. Material preparation and analysis were performed by ES, EH, TS, RG and CB. The first draft of the manuscript was written by ES, FA and EH and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Additional information
Elisabeth Smits and Felicita Andreotti share first authorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Smits, E., Andreotti, F., Houben, E. et al. Adherence and Persistence with Once-Daily vs Twice-Daily Direct Oral Anticoagulants Among Patients with Atrial Fibrillation: Real-World Analyses from the Netherlands, Italy and Germany. Drugs - Real World Outcomes 9, 199–209 (2022). https://doi.org/10.1007/s40801-021-00289-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-021-00289-w