Abstract
Background
The association of insomnia treatment with medical costs is not well characterized in Japan, despite the high economic burden of insomnia.
Objective
The aim of this study was to investigate the impact of suvorexant, the first dual orexin receptor antagonist, on direct medical costs in insomnia patients.
Patients and Methods
This retrospective cohort study, conducted using a large-scale claims database, included Japanese patients with diagnosed insomnia receiving suvorexant who were treatment naïve or treatment switchers (pre-treated with a different hypnotic and switched to suvorexant). Total medical costs were estimated for 1 year before and after suvorexant initiation; p-values were calculated for the difference in costs.
Results
Of the 1730 patients included, 1116 were treatment naïve and 614 were treatment switchers. Switching to suvorexant did not change the total treatment cost (US$4693–US$4692; p = 0.9964). Although treatment-naïve patients on average incurred US$3259 after suvorexant initiation, much of the additional cost was attributed to drugs other than hypnotics in the outpatient setting (US$332; p < 0.0001). While ~ 10% of the additional medical costs in the outpatient setting were attributable to hypnotics in both groups (treatment naïve: US$106, p < 0.0001; treatment switchers: US$115, p < 0.0001), no difference was observed in the inpatient setting.
Conclusion
Suvorexant as an initial insomnia treatment was associated with higher total medical costs, given the additional burden of initiating treatment and monitoring costs associated with a new insomnia diagnosis. However, despite a switch from another hypnotic, suvorexant did not increase the incremental economic burden. The hypnotic cost remained proportionately low, demonstrating that suvorexant initiation did not raise the cost of insomnia treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Suvorexant, a sleeping pill, when prescribed as the first treatment in patients with an inability to sleep, was associated with higher medical expenses. This was probably because of the additional burden of new treatment and medical care associated with identification of a new disease. |
However, when patients changed their treatment from another sleeping pill to suvorexant, there was no increase in the medical expenses. |
In addition, the cost of sleeping pills made up a small part of the total medical expenses, indicating that suvorexant did not contribute much to the overall treatment cost. |
1 Introduction
Insomnia is the most prevalent of all sleep disorders [1], with a global prevalence estimated at 6% in the general population in 2002 [2]. In Japan, an insomnia diagnosis was reported in 4.9% of the adult population, and 3.4% were receiving insomnia treatment in 2012 [3]. Although insomnia can be an independent disorder or a symptom of another disorder [1], it is frequently associated with multiple comorbidities, including medical and psychiatric disorders [4].
Insomnia is associated with significant direct and indirect costs [5, 6]. In a survey of Japanese workers, Takemura et al. reported that the economic loss due to insomnia and other sleep disorders was approximately US$31.9 billion [7]. Another report that examined the economic burden of insufficient sleep across five different countries predicted annual economic losses between US$88 billion and US$138 billion in Japan [8]. Several studies have indicated that taking treatment for insomnia is more cost effective than not taking treatment for it [9,10,11].
The pharmacological treatment for insomnia includes γ-aminobutyric acid (GABA) receptor agonists (benzodiazepine and non-benzodiazepine hypnotics), melatonin receptor agonists, and orexin receptor antagonists (ORAs) [12]. Jhaveri et al. carried out a predictive model-based analysis involving 88,305 adult patients receiving hypnotics and identified decreased medical costs following insomnia treatment, suggesting that insomnia treatments may result in direct cost savings [13]. Since this study focused on only non-benzodiazepine formulations and a melatonin receptor agonist, the total medical costs associated with the initiation of hypnotics are still unclear.
Suvorexant is the first dual ORA (DORA) approved for the treatment of insomnia in 2014 in Japan and recommended in the 2019 Japanese guidelines for insomnia [14, 15]. It acts by blocking the binding of neuropeptides orexin A and B to their respective orexin receptors, thereby suppressing wakefulness [16]. In a post-marketing surveillance (PMS) study in Japan, suvorexant treatment was generally well tolerated and resulted in improvements in insomnia in 73–74% of patients, based on both physician and patient assessments [17]. This study aimed to investigate the impact of suvorexant monotherapy on direct medical costs and healthcare resource utilization (HCRU) in Japanese patients with insomnia.
2 Methods
2.1 Study Design and Data Source
This retrospective cohort study analyzed an employer-based insurance claims database comprising inpatient, outpatient, and dispensing services data from over 130 domestic payers (through January 31, 2018), provided by the Japan Medical Data Center Inc. (JMDC), to examine pre- and post-suvorexant costs and HCRU. Each patient had a unique identifier and could be followed longitudinally if they were under the same employer-based insurance. Data were standardized by following the International Classification of Diseases, Tenth Revision (ICD-10) codes and the Anatomical Therapeutic Chemical (ATC) classification. JMDC, the largest health insurance claims database in Japan, allows for follow-up despite a change in the treating facility, unlike records from individual institutions where patients may be lost to follow-up.
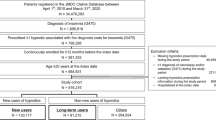
The index period was between December 1, 2014, and January 31, 2017, defined based on the suvorexant launch date in Japan (November 26, 2014). The index date for each patient was defined as the date of the first claim for suvorexant prescription during this period. Comorbidity, cost, and HCRU data were extracted for the pre-index (12 months before the index date) and post-index (12 months after the index date) periods; therefore, the study period was December 1, 2013, through January 31, 2018 (Fig. 1). All claims reported on the index date were included in the post-index period. The study was approved by an independent ethics committee, and the data were fully anonymized by JMDC to ensure data privacy.
2.2 Study Population
Patients with an insomnia diagnosis (ICD-10: G470) who initiated suvorexant monotherapy and who had at least two suvorexant prescriptions during the index period, as a proxy for consistent use of suvorexant, were included in the study. Patients were excluded if they were < 18 years of age at the time of suvorexant initiation; were not enrolled in the insurance claims database for ≥ 12 months before and after their index prescription; had one or more claim for suvorexant before December 1, 2014; or had a prescription claim for any other hypnotic during the post-index period. As suvorexant is contraindicated for narcolepsy [18], patients with one or more claim and an ICD-10 diagnosis for narcolepsy were also excluded. Moreover, suvorexant should be administered with caution in patients with a medical history of narcolepsy [14]. Treatment-naïve patients had no history of hypnotic use during the pre-index period; treatment switchers received hypnotics other than suvorexant during the pre-index period and subsequently switched to suvorexant monotherapy. Patients were evaluated for the presence of comorbidities associated with insomnia, based on > 18 such conditions reported by Kessler et al. [19]. The presence of comorbidities was confirmed at the time of prescribing hypnotics (suvorexant or other hypnotics); patients were counted in the pre- and post-index periods separately for the presence of comorbidities. Treatment costs associated with comorbidities were included in total medical costs, but were not documented separately.
2.3 Outcomes
Direct costs and HCRU in the pre- and post-index periods were analyzed as the primary outcome. Outpatient costs included costs for hypnotics, any other drugs (other than hypnotics), surgeries, or other visits and services in the outpatient setting. Inpatient costs included costs for hypnotics, any other drugs, any surgeries, length of hospitalization, use of intensive care unit (ICU)/high care unit (HCU), or other services in the inpatient settings. Costs associated with drugs (hypnotics and others) were calculated as the cost per dose times the dosage. The cost of drugs and medical treatment was calculated based on the Japanese reimbursement rules using the pricing list of the National Health Insurance, which is determined by the government and applicable to all health insurance associations. The cost of drugs and medical treatment was not adjusted for inflation because inflation rates in Japan were close to zero (inflation rates: 0.8% [2015], − 0.1% [2016], and 0.5% [2017]; source: International Monetary Fund) [20]. Therefore, there was a negligible change in the government-mandated reimbursement rates over the study period. All costs were presented in United States dollars using the 2014 Purchasing Power Parity value in Japan [21], based on the launch date of suvorexant. The costs of hypnotics and other drugs were calculated separately to compare and assess their individual proportions in the total treatment cost.
For HCRU measures, the number of total outpatient encounters (including office visits/laboratory visits/surgery/prescription/any activity that occurred in an outpatient setting) was calculated as the number of distinct days with an outpatient claim. Specific outpatient HCRU measures were presented by the number of distinct days with an outpatient claim for that measure. For inpatient HCRU measures, the number of distinct days with the use of hypnotics or any other drugs, number of surgeries, and the number and length of ICU and HCU stays were calculated.
To minimize the effects of underlying conditions and events that may have contributed to the initiation of insomnia treatment or a change in treatment, hospitalizations that overlapped both the pre- and post-index periods were removed from the post-index time period. Cost and HCRU were accrued only until the day prior to suvorexant initiation to distinguish costs and HCRU originating from encounters that occurred prior to suvorexant initiation.
2.4 Subgroup Analyses
Subgroup analyses were conducted based on patient age (< 55 vs ≥ 55 years) at the index date and treatment adherence, measured by the proportion of days covered (PDC). PDC was calculated as the proportion of the total number of days in the pre- or post-index periods covered by the prescriptions for suvorexant or prior insomnia treatment. In the absence of any consensus on appropriate cutoff values for insomnia treatment, the cutoff values were based on prior adherence studies [22, 23]. Patients were categorized as intermittent users (PDC < 20%), moderate users (PDC 20–79%), or continuous users (PDC ≥ 80%).
2.5 Statistical Analyses
We conducted descriptive statistics to analyze the costs and HCRU, including measures of the central tendency for continuous data (non-missing values, mean, standard deviation [SD]). Differences between pre- and post-index outcomes were evaluated using paired-sample t-tests for continuous measures and the McNemar test for categorical measures. Statistical significance was considered at the p < 0.05 level. In both treatment groups, only patients with hospitalizations were included in the length-of-stay analyses. Statistical significance was not calculated for length of stay in ICU/HCU. Data analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
3 Results
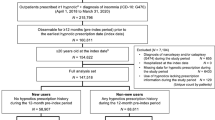
A total of 9277 patients with two or more prescriptions for suvorexant monotherapy were identified during the index period, of whom 1730 were included for analysis; 1116 (64.5%) were treatment naïve and 614 (35.5%) were treatment switchers (Fig. 2).
Patient disposition. Patients who had ≥ 2 prescription claims for suvorexant between December 1, 2014, and January 31, 2017, were evaluated for inclusion. Treatment-naïve patients had no history of other hypnotic drug use during the pre-index period. Treatment switchers had received another hypnotic drug during the pre-index period and subsequently switched to suvorexant monotherapy. ICD-10 International Classification of Diseases, Tenth Revision
3.1 Patient Characteristics
Patient characteristics were similar in the treatment-naïve and treatment-switcher groups (Table 1); most patients were male (61.5% and 56.0%, respectively), with a mean (SD) age of 45.1 (12.6) and 45.0 (12.6) years, respectively. Nearly all patients had an insomnia diagnosis during the study period (98.0% and 98.5%, respectively). Among the treatment switchers, the most frequently prescribed hypnotics (as monotherapy or in combination) prior to suvorexant were zolpidem (31.8%), followed by brotizolam (25.1%) and etizolam (20.2%). Similar characteristics were observed among the 4122 patients excluded from the analyses for hypnotic prescription claims other than suvorexant during the post-index period, suggesting minimal attrition bias.
The most common comorbidity during the pre-index period was diabetes mellitus (26.0%) in the treatment-naïve group and major depression (47.4%) among treatment switchers (Table 2). The most common comorbidity during the post-index period in both groups was major depression (42.0% and 50.5%, respectively). In the treatment-naïve group, all comorbidities (occurring in > 5% of patients) were observed at higher rates in the post-index period. The pre- and post-index comorbidity rates were 20.9% and 42.0% for major depression; 9.7% and 15.1% for anxiety disorders; 26.0% and 31.6% for diabetes; and 16.1% and 21.1% for chronic back/neck pain, respectively. Among treatment switchers, the rates of comorbidities (> 5%) were lower in the post- versus pre-index period, except for major depression (47.4% and 50.5%, respectively), diabetes (33.6% and 34.7%, respectively), hypertension (25.2% and 25.4%, respectively), and osteoarthritis (11.4% and 13.7%, respectively).
3.2 Total Medical Costs
Switching to suvorexant did not change the total costs (US$4693 to US$4692 per year; p = 0.9964) for treatment switchers, whereas treatment-naïve patients on average incurred a higher total cost after (US$3259) versus before (US$2168.9) initiating suvorexant (Table 3). The mean total costs were significantly different by age group and adherence category in treatment-naïve patients (Fig. 3a, b); differences were higher for patients ≥ 55 years old (US$1445; p = 0.0009) versus < 55 years old (US$980; p < 0.001) and for continuous users (US$1447) versus intermittent (US$1047) or moderate users (US$1042; p < 0.0001 for all). The mean total costs were not significantly different among treatment switchers by age group and adherence category.
Mean change in total costs and 95% CI by a age and b adherence categories measured by PDC. There was a significant increase in total costs for both treatment-naïve groups but not for patients who switched treatments. CI confidence interval, PDC proportion of days covered, US United States; *p < 0.005
3.3 Outpatient and Inpatient Costs
The mean overall outpatient costs for both groups were significantly higher during the post-index period compared with the pre-index period (treatment-naïve patients: US$2589.8 and US$1733.0, respectively; treatment switchers: US$3965.6 and US$2996.8, respectively; p < 0.0001 for both) (Table 3). There was a significant difference in the mean outpatient costs for all services in the pre- versus post-index period in both groups, except those associated with surgery and other costs among the treatment switchers (Table 4). The difference in the mean costs associated with hypnotics, accounting for approximately 10% of the additional outpatient costs, was US$105.60 (p < 0.0001) for treatment-naïve patients and US$115.10 (p < 0.0001) for treatment switchers (Table 4).
The mean overall inpatient cost was significantly lower among treatment switchers (Table 3). No significant difference was observed between the pre- and post-index periods in any of the specific inpatient resource uses among treatment-naïve patients. However, the mean inpatient cost for other drugs, surgeries, and other fees was significantly lower among treatment switchers (Table 4).
3.4 Healthcare Resource Utilization
The mean number of outpatient visits was significantly higher in the post-index period than in the pre-index period in both the groups (treatment naïve, 21.5 vs 14.6, p < 0.0001; treatment switchers, 25.6 vs 24.1, p = 0.0375; Table 5). The differences in HCRU between the pre- and post-index periods in the treatment-naïve and treatment-switcher groups are shown in Online Resource A1 (see Electronic Supplementary Material [ESM]).
4 Discussion
Insomnia is the most prevalent sleep disorder and is reportedly associated with increased HCRU and decreased work productivity [5, 6]; however, few studies have evaluated the association of insomnia treatment with direct medical costs and HCRU in Japan. To the best of our knowledge, this was the first study that assessed the direct medical costs associated with an insomnia treatment (suvorexant) in Japan using a large health claims database. The characteristics of the current study cohort were similar to those of the Japanese patients with insomnia in the 2012 National Health and Wellness Survey [3], including the average patient age (44–45 vs 47.9 years), commonly used other hypnotics (zolpidem tartrate, brotizolam, etizolam), and presence of several comorbidities. Almost 65% of users of suvorexant monotherapy in our study were treatment naïve, a proportion similar (approximately 60%) to that reported in the PMS study of suvorexant in patients with insomnia [17].
This study selected >18 insomnia-associated comorbidities, of which 17 were significantly correlated as reported by Kessler et al. [19]. The rate of comorbidities was higher in the post- versus pre-index period in treatment-naïve patients (particularly that of major depression, which almost doubled), while remaining similar among treatment switchers. The rate of comorbidities in the post-index period in treatment-naïve patients was similar to that in the pre-index period in treatment switchers, indicating that these comorbidities were independent of suvorexant initiation. This also suggests that regardless of the choice of hypnotics, comorbidities are associated with insomnia diagnosis. Previous studies have also demonstrated a high burden of comorbidities in patients with insomnia. In a United States (US) database study, the prevalence of depression, anxiety, migraine, and fibromyalgia was approximately two times higher in patients with insomnia than in those without insomnia [4]. Similarly, several studies in Japan have linked insomnia with the development and worsening of depression [24,25,26,27], diabetes, cardiovascular disorders, and hypertension [28].
Literature suggests that initiation of insomnia treatment may result in savings in direct healthcare costs [13]. In the current study, the total cost was significantly higher after suvorexant initiation in treatment-naïve patients. The additional total costs in treatment-naïve patients in our study were incurred irrespective of age or treatment adherence, which was expected given the additional burden of initiating treatment and monitoring costs associated with a new insomnia diagnosis. Previous Japanese studies have estimated a high burden of medical and morbidity costs in Japan due to depression and anxiety [29, 30]. Thus, the additional total costs could also be related to the increased rate of comorbidities, particularly that of major depression, as evident from the higher cost of other drugs in this group. However, the total costs and HCRU in the post-index period in treatment-naïve patients were less than that in the pre-index period among treatment switchers, as expected, because of similar rates of associated comorbidities during the respective study periods in both groups, thus indicating that suvorexant initiation did not add to the insomnia treatment cost. Moreover, hypnotics accounted for only ~ 10% of the total additional costs in the post-index period.
Total direct medical costs have been previously reported to be significantly higher in patients who switch therapy within a year (vs maintainers) [31]. In our study, the total costs did not change in treatment switchers. Comorbid depression or anxiety is reportedly more common among treatment switchers [31]. Similarly, the rate of comorbid depression or anxiety was high among treatment switchers in the post-index period in our study. However, the distribution of comorbidities remained comparable between the pre-index and post-index periods following initiation of suvorexant. Thus, the treatment cost for comorbidities potentially remained similar and may not have impacted the total medical cost. Therefore, our results did not demonstrate any change in the total medical costs among treatment switchers. During the study period, no policy changes such as those for reimbursement or new hypnotics were introduced, which could have impacted the treatment trend of insomnia. Moreover, a single year during the pre-index and post-index period included the same four seasons and, therefore, seasonality is also unlikely to be a confounding factor for the treatment trend. In a previous claims-based US study that investigated direct costs and HCRU among untreated insomnia patients, the key driver of additional costs was inpatient costs [4]. In our study, the outpatient costs were significantly higher and inpatient costs were not significantly different in the post-index periods in both treatment groups. The significant decrease in inpatient costs and HCRU among treatment switchers is indicative of the cost effectiveness of switching to suvorexant. On the contrary, the increased cost and HCRU in treatment-naïve patients could be related to the ≤ 14-day restriction on the duration of suvorexant prescription during the first year of its approval, necessitating frequent visits to the medical site for potentially detailed follow-up for insomnia as well as for comorbidities.
Although the price of suvorexant is higher than that of conventionally used GABA agonist drugs [16], the additional cost of hypnotics accounted for only 10% of the additional total cost. Thus, suvorexant is potentially cost effective in treating insomnia, given its novel mechanism of action. Medication strategies should be carefully planned in Japanese patients with chronic insomnia because of concerns associated with an increased risk of adverse drug reactions (ADRs), such as drug dependence and cognitive impairment, caused by long-term treatment with hypnotics, high dosage, and multiple drug combinations [32]. Moreover, adherence to hypnotics is poor among Japanese patients because of anxiety and concerns associated with their use [32]. Therefore, hypnotics have to be administered taking into account the benefit–risk ratio and patients’ attitudes towards hypnotic use. Suvorexant is a preferred hypnotic for use in psychiatric patients and the elderly because of a relatively safe profile, with no drug dependency or suicidal tendencies observed as ADRs in the PMS study [17]. This was also evident from higher suvorexant versus zolpidem prescriptions in older patients and those with comorbidities in a new-user cohort study [33]. Moreover, the cost outcomes from the current study suggest that switching to suvorexant potentially results in no additional financial or HCRU burden. Thus, suvorexant maintains overall low costs versus conventional alternative hypnotic medications.
Several limitations of this study should be considered while interpreting the results. Study results may be generalized to the Japanese population because data were collected from JMDC, the largest claims database in Japan. However, results need to be interpreted cautiously. Since the JMDC database is derived from employment-based insurance, potentially a small number of elderly patients were included in this analysis, which is likely to underestimate the true number of elderly patients taking suvorexant, and the study population was limited to only those patients who remained with the same insurance association. Furthermore, causality could not be assessed because data on patient characteristics, laboratory tests results, prognosis, reasons for treatment decisions etc. cannot be captured in the JMDC database. This study applied a simple pre–post design and is subject to confounding by indication. Moreover, results were not adjusted for confounding factors. Treatment-naïve patients may have had previously undiagnosed comorbidities in the pre-index period, which could be misinterpreted as cost drivers instead of an effect of limitations of clinical care and/or underreporting, and therefore underdiagnosis of stigma-related conditions such as depression. Statistical tests were performed around the mean, with the assumption that at least some measures were normally distributed. However, because cost data can be right skewed, future studies should focus on methods that better characterize cost data.
5 What is New and Conclusion
The comparison of direct medical costs 1 year before and after the initiation of suvorexant monotherapy in Japanese patients with insomnia suggested that suvorexant as an initial insomnia treatment was associated with higher total medical costs, given the additional burden of initiating treatment and monitoring costs associated with a new insomnia diagnosis. However, despite a switch from a cheaper hypnotic, suvorexant did not increase the incremental economic burden. Moreover, the hypnotic cost remained proportionately low, demonstrating that suvorexant initiation did not add to the insomnia treatment cost. Thus, results from our real-world study demonstrate that novel treatment options, particularly those for insomnia, despite their relatively high cost, may not always increase direct medical costs. Additional research is required to further characterize the real-world clinical and economic benefits of initiating suvorexant among Japanese adults with insomnia.
References
Association AP. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111.
Mishima K, DiBonaventura M, Gross H. The burden of insomnia in Japan. Nat Sci Sleep. 2015;7:1–11.
Wickwire EM, Tom SE, Scharf SM, Vadlamani A, Bulatao IG, Albrecht JS. Untreated insomnia increases all-cause health care utilization and costs among Medicare beneficiaries. Sleep. 2019;42(4):zsz007.
Ozminkowski RJ, Wang S, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep. 2007;30(3):263–73.
Wade AG. The societal costs of insomnia. Neuropsychiatr Dis Treat. 2011;7:1–18.
Takemura S, Ohida T, Kaneda Y, Uchiyama M. Economic evaluation of sleep disorder [Japanese]. Geriatr Med. 2007;45(6):679–85.
Hafner M, Stepanek M, Taylor J, Troxel WM, van Stolk C. Why sleep matters—the economic costs of insufficient sleep: a cross-country comparative analysis. Rand Health Q. 2017;6(4):11.
Scott GW, Scott HM, O’Keeffe KM, Gander PH. Insomnia - treatment pathways, costs and quality of life. Cost Eff Resour Alloc. 2011;9:10.
Watanabe N, Furukawa TA, Shimodera S, et al. Cost-effectiveness of cognitive behavioral therapy for insomnia comorbid with depression: analysis of a randomized controlled trial. Psychiatry Clin Neurosci. 2015;69(6):335–43.
Wickwire EM, Shaya FT, Scharf SM. Health economics of insomnia treatments: the return on investment for a good night’s sleep. Sleep Med Rev. 2016;30:72–82.
Japanese Society of Neurological Therapeutics. Standard neurologic care: insomnia, hypersomnia, and circadian rhythm disorders 2016. https://www.jsnt.gr.jp/guideline/img/fuminkamin.pdf. Accessed 11 Nov 2020.
Jhaveri M, Seal B, Pollack M, Wertz D. Will insomnia treatments produce overall cost savings to commercial managed-care plans? A predictive analysis in the United States. Curr Med Res Opin. 2007;23(6):1431–43.
PMDA. BELSOMRA® (suvorexant) tablets interview form. MSD K.K., Tokyo, Japan. 10th ed (revised December 2021). https://www.info.pmda.go.jp/go/interview/1/170050_1190023F1024_1_010_1F.pdf. Accessed 21 July 2021.
Uchiyama M. Guideline of support actions and treatment for sleep disorders [Japanese]. 3rd ed. Tokyo: Jiho Inc.; 2019.
Rhyne DN, Anderson SL. Suvorexant in insomnia: efficacy, safety and place in therapy. Ther Adv Drug Saf. 2015;6(5):189–95.
Asai Y, Sano H, Miyazaki M, Iwakura M, Maeda Y, Hara M. Suvorexant (Belsomra ® tablets 10, 15, and 20 mg): Japanese drug-use results survey. Drugs R D. 2019;19(1):27–46.
FDA. BELSOMRA® (suvorexant) tablets, for oral use. Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc. Whitehouse station, NJ 08889, USA, 2014. https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/204569s000lbledt.pdf. Accessed 21 July 2021.
Kessler RC, Berglund PA, Coulouvrat C, Fitzgerald T, Hajak G, Roth T, et al. Insomnia, comorbidity, and risk of injury among insured Americans: results from the America Insomnia Survey. Sleep. 2012;35(6):825–34.
IMF DataMapper 2021. International Monetary Fund. Country data: Inflation rate, average consumer prices (Annual percent change). https://www.imf.org/en/Countries/JPN#countrydata. Accessed 20 July 2021.
OECD. Organisation for Economic Co-operation and Development. Stat extracts: PPPs and exchange rates. http://stats.oecd.org/Index.aspx?DatasetCode=SNA_TABLE4. Accessed 11 Mar 2019.
Muntner P, Yun H, Sharma P, Delzell E, Kent ST, Kilgore ML, et al. Ability of low antihypertensive medication adherence to predict statin discontinuation and low statin adherence in patients initiating treatment after a coronary event. Am J Cardiol. 2014;114(6):826–31.
Burden AM, Paterson JM, Gruneir A, Cadarette SM. Adherence to osteoporosis pharmacotherapy is underestimated using days supply values in electronic pharmacy claims data. Pharmacoepidemiol Drug Saf. 2015;24(1):67–74.
Fujieda M, Uchida K, Ikebe S, Kimura A, Kimura M, Watanabe T, et al. Inquiring about insomnia may facilitate diagnosis of depression in the primary care setting. Psychiatry Clin Neurosci. 2017;71(6):383–94.
Koyama F, Yoda T, Hirao T. Insomnia and depression: Japanese hospital workers questionnaire survey. Open Med (Wars). 2017;12:391–8.
Nakajima S, Komada Y, Sasai-Sakuma T, Okajima I, Harada Y, Watanabe K, et al. Higher sleep reactivity and insomnia mutually aggravate depressive symptoms: a cross-sectional epidemiological study in Japan. Sleep Med. 2017;33:130–3.
Nishitani N, Kawasaki Y, Sakakibara H. Insomnia and depression: risk factors for development of depression in male Japanese workers during 2011–2013. Int J Public Health. 2018;63(1):49–55.
Uchiyama M, Inoue Y, Uchimura N, Kawamori R, Kurabayashi M, Kario K, et al. Clinical significance and management of insomnia. Sleep Biol Rhythms. 2011;9(2):63–72.
Sado M, Takechi S, Inagaki A, Fujisawa D, Koreki A, Mimura M, et al. Cost of anxiety disorders in Japan in 2008: a prevalence-based approach. BMC Psychiatry. 2013;13:338.
Sado M, Yamauchi K, Kawakami N, Ono Y, Furukawa TA, Tsuchiya M, et al. Cost of depression among adults in Japan in 2005. Psychiatry Clin Neurosci. 2011;65(5):442–50.
Balkrishnan R, Pollack M, Joish VN, Asche CV, Pawaskar MD, Cziraky MJ. An economic evaluation of therapeutic alteration in the management of insomnia. Curr Med Res Opin. 2009;25(3):663–9.
Working Group of Health and Labour Sciences Research/Japanese Society of Sleep Research. Medical practice guidelines for the appropriate use of sleeping pills and drug withdrawal. http://www.jssr.jp/data/pdf/suiminyaku-guideline.pdf. Accessed 16 Mar 2020.
Pinto CA, Kumar P, Herring WJ, Hyacinthe J, Kumar A, Lakshminarayanan M, et al. Assessment of channeling among initiators of suvorexant compared to other insomnia drugs [ICPE abstract 631]. Pharmacoepidemiol Drug Saf. 2019;28(suppl 2):580–6.
Acknowledgments
Medical writing support was provided by Deepali Garg, MBBS, PGDHA, of Cactus Life Sciences (part of Cactus Communications Pvt. Ltd.) and funded by MSD K.K., Tokyo, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by MSD K.K. (Tokyo, Japan) through a research contract with Market Access, MSD K.K., Tokyo, Japan. The funder participated in study design, interpretation of data, and writing, review, and approving the publication.
Conflicts of interest
M.U. has received research support from Astellas Pharma, Eisai, Meiji Seika Pharma, MSD K.K., Pfizer Japan, Shionogi & Co, Taisho Pharmaceutical, Kao Corporation, and Takeda Pharmaceutical; had a consulting role for Idorsia Pharmaceuticals Japan, Kao Corporation, Taisho Pharmaceutical, and Takeda Pharmaceutical; and has received honoraria for giving lectures and/or contributing text from Astellas Pharma, Eisai, Otsuka Pharmaceutical, Meiji Seika Pharma, MSD K.K., and Takeda Pharmaceutical. K.I. was an employee of the sponsoring company (MSD K.K., Tokyo, Japan) at the time of study conduct. M.A. is an employee of the sponsoring company (MSD K.K., Tokyo, Japan). MSD K.K., Tokyo, Japan manufactures a product for the treatment of insomnia. B.C. and J.Y. are employees of Syneos Health, a healthcare contract research organization. Y.O. has received personal fees from MSD K.K., Otsuka Pharmaceutical, Cando, Japan Medical Data Center, and Japan Medical Research Institute.
Ethics approval
The study was approved by an independent ethics committee, and the data were fully anonymized by Japan Medical Data Center Inc. to ensure data privacy.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Data sharing not applicable—no new data generated, or the article describes entirely theoretical research.
Code availability
Not applicable.
Authors’ contributions
KI, YO, and BC designed the study protocol and methods. BC and JY conducted the statistical analysis and co-wrote the manuscript. MU and YO interpreted the results and served as advisors to guide writing of the manuscript. KI and MA supervised the research.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Uchiyama, M., Ito, K., Okumura, Y. et al. Medical Costs Associated with Insomnia Treatment with Suvorexant Monotherapy in Japan: Results from a Retrospective Cohort Study Using a Large-Scale Claims Database. Drugs - Real World Outcomes 9, 219–229 (2022). https://doi.org/10.1007/s40801-021-00279-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-021-00279-y