Abstract
Purpose of Review
The rise of the pediatric obesity pandemic over the past 40 years has sharpened focus on the management of obesity, hypertension, and lipid abnormalities in children. Multiple studies demonstrate that these risk factors track from childhood into adulthood predisposing individuals to premature atherosclerotic cardiovascular disease and putting them at risk for early morbidity and mortality.
Recent Findings
Importantly, obesity, hypertension, and lipid problems are individual risk factors that can occur independently. Multiple studies have shown that each risk factor causes target organ damage in children. Intensive and focused lifestyle modifications can improve a child’s subclinical disease and decrease the risk for future morbidity.
Summary
Childhood offers a unique opportunity at primordial and primary prevention of atherosclerotic cardiovascular disease. Clinicians must focus on targeting these highly prevalent conditions and applying lifestyle modification and then pharmacologic or surgical therapies as needed.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Benjamin J, Muntner S, Alonso W, et al. Heart Disease and Stroke Statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–66 This article summarizes the most up-to-date statistics regarding heart disease and stroke and the cardiovascular risk factors that contribute to each.
Roth GA, Johnson CO, Abate KH, et al. The burden of cardiovascular diseases among US States, 1990–2016. JAMA Cardiol. 3:375–89 This article summarizes the national burden of cardiovascular disease in the United States, revealing disparities among age, sex, and geography. It also summarizes drivers of change in cardiovascular disease morbidity.
Fryar CD, Chen T-C, Li X (2012) Prevalence of uncontrolled risk factors for cardiovascular disease: United States, 1999–2010. NCHS Data Brief 1–8.
Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJL, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors (mortality effects of risk factors in the US). PLoS Med. 2009;6:e1000058.
•• Whelton K, Carey M, Aronow S, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138:e426–83 This is the most recent clinical practice guideline for the management of high blood pressure in adults.
•• Whelton PK, Williams B, Hope K, et al. (2018) The 2018 European Society of Cardiology/European Society of Hypertension and 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines: more similar than different. In: JAMA. Totowa, NJ: Humana Press: Imprint: Humana, pp. 1749–7. This editorial compares the most recent American and European clinical practice guidelines on the management of high blood pressure in adults.
Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–98.
Expert Panel On Integrated Guidelines FOR Cardiovascular Health And Risk Reduction In Children And Adolescents. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(Suppl 5):S213–56.
Enos WF, Holmes RH, Beyer J. Coronary disease among United States soldiers killed in action in Korea; preliminary report. J Am Med Assoc. 1953;152:1090–3.
McNamara JJ, Molot MA, Stremple JF, Cutting RT. Coronary artery disease in combat casualties in Vietnam. JAMA. 1971;216:1185–7.
Strong JP, Malcom GT, Mcmahan CA, Tracy RE, Newman WP III, Herderick EE, et al. Prevalence and extent of atherosclerosis in adolescents and young adults: implications for prevention from the pathobiological determinants of atherosclerosis in youth study. JAMA. 1999;281:727–35.
Berenson GS, Srinivasan SR, Bao W, Newman WP, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338:1650–6.
Mcmahan CA, Gidding SS, Malcom GT, Schreiner PJ, Strong JP, Tracy RE, et al. Comparison of coronary heart disease risk factors in autopsied young adults from the PDAY Study with living young adults from the CARDIA study. Cardiovasc Pathol. 2007;16:151–8.
May AL, Kuklina EV, Yoon PW. Prevalence of cardiovascular disease risk factors among US adolescents, 1999–2008. Pediatrics. 2012;129:1035–41.
Ebbeling CB, Leidig MM, Feldman HA, Lovesky MM, Ludwig DS. Effects of a low–glycemic load vs low-fat diet in obese young adults: a randomized trial. JAMA. 2007;297:2092–102.
Jacobson MS, Tomopoulos S, Williams CL, Arden MR, Deckelbaum RJ, Starc TJ. Normal growth in high-risk hyperlipidemic children and adolescents with dietary intervention. Prev Med. 1998;27:775–80.
Farpour-Lambert NJ, Aggoun Y, Marchand LM, Martin XE, Herrmann FR, Beghetti M. Physical activity reduces systemic blood pressure and improves early markers of atherosclerosis in pre-pubertal obese children. J Am Coll Cardiol. 2009;54:2396–406.
Kelly S, Barlow E, Rao H, Inge L, Hayman M, Steinberger J, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128:1689–712.
Frederick CB, Snellman K, Putnam RD. Increasing socioeconomic disparities in adolescent obesity. Proc Natl Acad Sci U S A. 2014;111:1338–42.
Ogden CL, Lamb MM, Carroll MD, Flegal KM (2010) Obesity and socioeconomic status in children and adolescents: United States, 2005–2008. NCHS Data Brief. Number 51. National Center for Health Statistics.
Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev. 2016;17:95–107.
• Sharma V, Coleman S, Nixon J, Sharples L, Hamilton-Shield J, Rutter H, et al. A systematic review and meta-analysis estimating the population prevalence of comorbidities in children and adolescents aged 5 to 18 years. Obes Rev. 2019;20:1341–9 This systematic review searches 5 databases up to 2018 for the population prevalence of obesity-associated comorbidities in children and adolescents.
Cote AT, Harris KC, Panagiotopoulos C, Sandor GGS, Devlin AM. Childhood obesity and cardiovascular dysfunction. J Am Coll Cardiol. 2013;62:1309–19.
Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150:12–17.e2.
Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2011;35:891–8.
Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–93.
• Lindberg L, Danielsson P, Persson M, Hagman E, Marcus C (2017) Childhood obesity increases risk of premature death in young adulthood—a prospective cohort study Louise Lindberg. Eur J Public Health. https://doi.org/10.1093/eurpub/ckx189.254. This article summarizes the findings of a Swedish cohort showing that obese children had an increased incidence of premature death in early adulthood compared with the general population.
•• Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, et al. Pediatric obesity-assessment, treatment, and prevention: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2017;102:709–57 This article summarizes the Endocrine Society’s most recent clinical practice guideline for the assessment, treatment and prevention of childhood obesity.
Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120:S164–92.
Gray JS, Filigno SS, Santos M, Ward WL, Davis AM. The status of billing and reimbursement in pediatric obesity treatment programs. J Behav Health Serv Res. 2013;40:378–85.
Strauss RS, Pollack HA. Social marginalization of overweight children. Arch Pediatr Adolesc Med. 2003;157:746–52.
Perrin EM, Finkle JP, Benjamin JT. Obesity prevention and the primary care pediatrician’s office. Curr Opin Pediatr. 2007;19:354–61.
Caprio S, Daniels SR, Drewnowski A, Kaufman FR, Palinkas LA, Rosenbloom AL, et al. Influence of race, ethnicity, and culture on childhood obesity: implications for prevention and treatment. Diabetes Care. 2008;31:2211–21.
•• Grossman DC, Bibbins-Domingo K, Curry SJ, et al. Screening for obesity in children and adolescents: US Preventive Services Task Force Recommendation Statement. JAMA. 2017;317:2417–26 This article from the USPTF recommends that all children 6 years and older be screened for obesity and referred for comprehensive intensive behavioral therapy to improve their weight status.
•• Hall KD, Ayuketah A, Brychta R, et al. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab. 2019;30:67–77.e3 In this study, two groups of patients were given either an ultra-processed or unprocessed diet. Even when the diets were matched for calories and macronutrients those eating an ultra-processed diet gained more weight.
Epstein LH, Roemmich JN, Raynor HA. Behavioral therapy in the treatment of pediatric obesity. Pediatr Clin. 2001;48:981–93.
Wang Y, Cai L, Wu Y, et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev Off J Int Assoc Study Obes. 2015;16:547–65.
August GP, Caprio S, Fennoy I, Freemark M, Kaufman FR, Lustig RH, et al. Prevention and treatment of pediatric obesity: an Endocrine Society Clinical Practice Guideline based on expert opinion. J Clin Endocrinol Metab. 2008;93:4576–99.
Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. The relationship between parent and child self-reported adherence and weight loss. Obes Res. 2005;13:1089–96.
Dhaliwal J, Nosworthy NMI, Holt NL, Zwaigenbaum L, Avis JLS, Rasquinha A, et al. Attrition and the management of pediatric obesity: an integrative review. Child Obes Print. 2014;10:461–73.
Hall KD. The complicated relation between resting energy expenditure and maintenance of lost weight. Am J Clin Nutr. 2018;108:652–3.
• Swinburn BA, Kraak VI, Allender S, et al. The global syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. Lancet. 2019;393:791–846 This article explains how the obesity epidemic is actually part of a worldwide syndemic and describes how toxic food environments contribute to furthering obesity.
Sherafat-Kazemzadeh R, Yanovski SZ, Yanovski JA. Pharmacotherapy for childhood obesity: present and future prospects. Int J Obes. 2013;37:1–15.
Chanoine J-P, Hampl S, Jensen C, Boldrin M, Hauptman J. Effect of orlistat on weight and body composition in obese adolescents: a randomized controlled trial. JAMA. 2005;293:2873–83.
Crinò A, Fintini D, Bocchini S, Grugni G. Obesity management in Prader-Willi syndrome: current perspectives. Diabetes Metab Syndr Obes Targets Ther. 2018;11:579–93.
Pratt JSA, Lenders CM, Dionne EA, et al. Best practice updates for pediatric/adolescent weight loss surgery. Obesity. 2009;17:901–10.
Olbers T, Gronowitz E, Werling M, et al. Two-year outcome of laparoscopic Roux-en-Y gastric bypass in adolescents with severe obesity: results from a Swedish Nationwide Study (AMOS). Int J Obes. 2012;36:1388–95.
• Heymsfield S, Aronne LJ, Eneli I, Kumar RB, Michalsky M, Walker E, et al. Clinical perspectives on obesity treatment: challenges, gaps, and promising opportunities. NAM Perspect. 2018. https://doi.org/10.31478/201809b This article summarizes the challenges and treatment gaps in the management of obesity including the role of pharmacotherapy, bariatric surgery and policy change.
World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. Albany: World Health Organization; 2009.
Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet Lond Engl. 2014;383:1899–911.
Blumenthal S, Epps RP, Heavenrich R, et al. Report of the task force on blood pressure control in children. Pediatrics. 1977;59(I–II):797–820.
•• Flynn JT, Kaelber DC, Baker-Smith CM, et al. (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. https://doi.org/10.1542/peds.2017-1904. This article summarizes the most recent clinical practice guideline for the management of high blood pressure in children.
Din-Dzietham R, Liu Y, Bielo M-V, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488–96.
Dobson CP, Eide M, Nylund CM. Hypertension prevalence, cardiac complications, and antihypertensive medication use in children. J Pediatr. 2015;167:92–97.e1.
• Zachariah JP, Wang Y, Penny DJ, Baranowski T. Relation between lead exposure and trends in blood pressure in children. Am J Cardiol. 2018;122:1890–5 This article shows that the recent decline in pediatric blood pressure during the rise of pediatric obesity may be attributable to declining lead exposure.
•• Sharma A, Metzger D, Rodd C (2018) Prevalence and severity of high blood pressure among children based on the 2017 American Academy of Pediatrics Guidelines. JAMA Pediatr. 557. This article assesses the consequences of the new clinical practice guideline for high blood pressure in children. The article reveals that with the new definitions an additional 5.8% of children would be diagnosed as having high blood pressure.
Muntner P, He J, Cutler JA, Wildman RP, Whelton PK. Trends in blood pressure among children and adolescents. JAMA. 2004;291:2107–13.
Shi Y, de Groh M, Morrison H (2012) Increasing blood pressure and its associated factors in Canadian children and adolescents from the Canadian Health Measures Survey. BMC Public Health 12:388.
Falkner B, Gidding SS, Portman R, Rosner B. Blood pressure variability and classification of prehypertension and hypertension in adolescence. Pediatrics. 2008;122:238–42.
• Cheung EL, Bell CS, Samuel JP, Poffenbarger T, Redwine KM, Samuels JA (2017) Race and obesity in adolescent hypertension. Pediatrics. https://doi.org/10.1542/peds.2016-1433. This article shows how the prevalence of adolescent hypertension varies among race and ethnicities.
Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta–regression analysis. Circulation. 2008;117:3171–80.
Gray L, Lee I-M, Sesso HD, Batty GD. Blood pressure in early adulthood, hypertension in middle age, and future cardiovascular disease mortality: HAHS (Harvard Alumni Health Study). J Am Coll Cardiol. 2011;58:2396–403.
Sundström J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ. 2011. https://doi.org/10.1136/bmj.d643.
Kelly RK, Thomson R, Smith KJ, Dwyer T, Venn A, Magnussen CG. Factors affecting tracking of blood pressure from childhood to adulthood: the childhood determinants of adult health study. J Pediatr. 2015;167:1422–1428.e2.
Flynn T, Daniels R, Hayman L, Maahs M, Mccrindle W, Mitsnefes P, et al. Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension. 2014;63:1116–35.
Stergiou GS, Giovas PP, Kollias A, Rarra VC, Papagiannis J, Georgakopoulos D, et al. Relationship of home blood pressure with target-organ damage in children and adolescents. Hypertens Res. 2011;34:640–4.
Sorof M, Cardwell J, Franco J, Portman J. Ambulatory blood pressure and left ventricular mass index in hypertensive children. Hypertens J Am Heart Assoc. 2002;39:903–8.
Stabouli S, Kotsis V, Papamichael C, Constantopoulos A, Zakopoulos N. Adolescent obesity is associated with high ambulatory blood pressure and increased carotid intimal-medial thickness. J Pediatr. 2005;147:651–6.
Lande B, Carson L, Roy C, Meagher C. Effects of childhood primary hypertension on carotid intima media thickness: a matched controlled study. Hypertension. 2006;48:40–4.
Zhu H, Yan W, Ge D, Treiber FA, Harshfield GA, Kapuku G, et al. Cardiovascular characteristics in American youth with prehypertension. Am J Hypertens. 2007;20:1051–7.
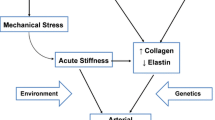
Kulsum-Mecci N, Goss C, Kozel BA, Garbutt JM, Schechtman KB, Dharnidharka VR. Effects of obesity and hypertension on pulse wave velocity in children. J Clin Hypertens. 2017;19:221–6.
Aggoun Y, Farpour-Lambert NJ, Marchand LM, Golay E, Maggio ABR, Beghetti M. Impaired endothelial and smooth muscle functions and arterial stiffness appear before puberty in obese children and are associated with elevated ambulatory blood pressure. Eur Heart J. 2008;29:792–9.
Lovibond K, Jowett S, Barton P, et al. Cost-effectiveness of options for the diagnosis of high blood pressure in primary care: a modeling study. Lancet Lond Engl. 2011;378:1219–30.
Swartz SJ, Srivaths PR, Croix B, Feig DI. Cost-effectiveness of ambulatory blood pressure monitoring in the initial evaluation of hypertension in children. Pediatrics. 2008;122:1177–81.
Gupta-Malhotra M, Banker A, Shete S, Hashmi SS, Tyson JE, Barratt MS, et al. Essential hypertension vs. secondary hypertension among children. Am J Hypertens. 2015;28:73–80.
Dennison BA. Bright futures and NHLBI integrated pediatric cardiovascular health guidelines. Pediatr Ann. 2012;41:e31–6.
Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–24.
• Siervo M, Lara J, Chowdhury S, Ashor A, Oggioni C, Mathers JC (2015) Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta-analysis. 80:1–15. This systematic review summarizes the beneficial effect of the DASH diet on blood pressure, overweight and obesity in adolescence.
Paula Bricarello L, Poltronieri F, Fernandes R, Retondario A, de Moraes Trindade EBS, de Vasconcelos F d AG. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on blood pressure, overweight and obesity in adolescents: a systematic review. Clin Nutr ESPEN. 2018;28:1–11.
Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10.
Kelley GA, Kelley KS, Tran ZV. The effects of exercise on resting blood pressure in children and adolescents: a meta-analysis of randomized controlled trials. Prev Cardiol. 2003;6:8–16.
Leary SD, Ness AR, Davey SG, Calum M, Kevin D, Blair SN, et al. Physical activity and blood pressure in childhood. Hypertension. 2008;51:92–8.
Steinberger R, Daniels R, Hagberg S, et al. Cardiovascular health promotion in children: challenges and opportunities for 2020 and beyond: a scientific statement from the American Heart Association. Circulation. 2016;134:e236–55.
PAG Midcourse Report: Strategies to increase physical activity among youth | health.gov. https://health.gov/our-work/physical-activity/previous-guidelines/2013-midcourse-report. Accessed 7 Feb 2020.
Messerli FH, Sripal B, Stevo J. Risk/benefit assessment of β-blockers and diuretics precludes their use for first-line therapy in hypertension. Circulation. 2008;117:2706–15.
Ferguson M, Flynn J. Treatment of pediatric hypertension: lessons learned from recent clinical trials. Curr Cardiovasc Risk Rep. 2014;8:1–7.
Ferguson M, Flynn J. Rational use of antihypertensive medications in children. Pediatr Nephrol. 2014;29:979–88.
Relation of Serum Lipoprotein Levels and Systolic Blood Pressure to Early Atherosclerosis | NEJM. https://www.nejm.org/doi/full/10.1056/nejm198601163140302. Accessed 15 Dec 2019.
Schrott HG, Bucher KA, Clarke WR, Lauer RM. The Muscatine hyperlipidemia family study program. Prog Clin Biol Res. 1979;32:619–46.
Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: the Muscatine study. Circulation. 2001;104:2815–9.
Raitakari OT, Juonala M, Kähönen M, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA. 2003;290:2277–83.
Juhola J, Magnussen CG, Viikari JSA, et al. Tracking of serum lipid levels, blood pressure, and body mass index from childhood to adulthood: the cardiovascular risk in Young Finns Study. J Pediatr. 2011;159:584–90.
•• Duell PB, Gidding SS, Andersen RL, et al. Longitudinal low density lipoprotein cholesterol goal achievement and cardiovascular outcomes among adult patients with familial hypercholesterolemia: The CASCADE FH registry. Atherosclerosis. 2019;289:85–93 This article reports on an American cohort of patients with FH and shows that with aggressive therapy, the LDL-c in FH patients can be reduced to near normal levels.
•• Pérez de Isla L, Alonso R, Mata N, et al. Predicting cardiovascular events in familial hypercholesterolemia: the SAFEHEART Registry (Spanish Familial Hypercholesterolemia Cohort Study). Circulation. 2017;135:2133–44 This article reports on a Spanish cohort of patients with FH and describes the development of a risk prediction equation for ASCVD events unique to this population.
•• Masana L, Zamora A, Plana N, et al. (2019) Incidence of cardiovascular disease in patients with familial hypercholesterolemia phenotype: analysis of 5 years follow-up of real-world data from more than 1.5 million patients. J Clin Med. https://doi.org/10.3390/jcm8071080. This article compares the incidence of ASCVD events in patients with FH to those with normal lipid profiles. The hazard ratio for ASCVD and coronary heart disease in patients with FH were 7.1 and 16.7 respectively.
Urbina EM, Williams RV, Alpert BS, et al. Noninvasive assessment of subclinical atherosclerosis in children and adolescents. Hypertension. 2009;54:919–50.
•• Perak AM, Ning H, Kit BK, de Ferranti SD, Van Horn LV, Wilkins JT, et al. Trends in levels of lipids and apolipoprotein B in US youths aged 6 to 19 years, 1999–2016. JAMA. 2019;321:1895–905 This article summarizes the most recent NHANES data on the incidence of lipid disorders in children and adolescents.
Bansal N, Tejtel K. Race/ethnic differences in dyslipidemia patterns in youth. J Clin Lipidol. 2019;13:e43.
Zachariah J (2016) Lipid screening in youth. MDText.com, Inc.
Goldberg AC, Hopkins PN, Toth PP, et al. Familial hypercholesterolemia: screening, diagnosis and management of pediatric and adult patients. J Clin Lipidol. 2011;5:S1–8.
• Akioyamen LE, Genest J, Shan SD, Reel RL, Albaum JM, Chu A, Tu JV (2017) Estimating the prevalence of heterozygous familial hypercholesterolaemia: a systematic review and meta-analysis. BMJ Open. https://doi.org/10.1136/bmjopen-2017-016461. This systematic review pooled data from > 2.5 million people to estimate the prevalence of FH to be ~1/250 individuals.
(1992) National Cholesterol Education Program (NCEP): highlights of the report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Pediatrics 89:495–501.
Daniels SR, Greer FR, Committee on Nutrition. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008;122:198–208.
Haney EM, Huffman LH, Bougatsos C, Freeman M, Steiner RD, Nelson HD. Screening and treatment for lipid disorders in children and adolescents: systematic evidence review for the US Preventive Services Task Force. Pediatrics. 2007;120:e189–214.
Ritchie SK, Murphy EC-S, Ice C, Cottrell LA, Minor V, Elliott E, et al. Universal versus targeted blood cholesterol screening among youth: the CARDIAC Project. Pediatrics. 2010;126:260–5.
Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Screening for lipid disorders in children and adolescents: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;316:625–33.
Zachariah JP, Mcneal CJ, Copeland LA, et al. Temporal trends in lipid screening and therapy among youth from 2002 to 2012. J Clin Lipidol. 2015;9:S77–87.
McNeal C, Zachariah J, Gregory S, Cassidy-Bushrow A, Wilson D, Tom J, et al. Identifying and reducing barriers to improve lipid screening in youth. Curr Cardiovasc Risk Rep. 2014;8:1–7.
Silverman MG, Ference BA, Im K, Wiviott SD, Giugliano RP, Grundy SM, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA. 2016;316:1289–97.
•• Luirink IK, Wiegman A, Kusters DM, Hof MH, Groothoff JW, de Groot E, et al. 20-year follow-up of statins in children with familial hypercholesterolemia. N Engl J Med. 2019;381:1547–56 This article shows that initiation of statin therapy in patients with FH starting in childhood slowed measures of subclinical atherosclerosis and reduced their risk of ASCVD in adulthood.
Ference BA, Yoo W, Alesh I, Mahajan N, Mirowska KK, Mewada A, et al. Effect of long-term exposure to lower low-density lipoprotein cholesterol beginning early in life on the risk of coronary heart disease: a Mendelian randomization analysis. J Am Coll Cardiol. 2012;60:2631–9.
Zachariah JP, Chan J, Mendelson MM, Regh T, Griggs S, Johnson PK, et al. Adolescent dyslipidemia and standardized lifestyle modification: benchmarking real-world practice. J Am Coll Cardiol. 2016;68:2122–3.
Linda Van H, Eva O, Bruce AB, et al. A summary of results of the dietary intervention study in children (DISC): lessons learned. Prog Cardiovasc Nurs. 2003;18:28–41.
Clinical Practice Guideline for Multicomponent Behavioral Treatment of Obesity and Overweight in Children and Adolescents. 109.
Nordestgaard BG, Chapman MJ, Humphries SE, et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart J. 2013;34:3478–3490a.
• EAS Familial Hypercholesterolaemia Studies Collaboration, Vallejo-Vaz AJ, De Marco M, et al. Overview of the current status of familial hypercholesterolaemia care in over 60 countries - The EAS Familial Hypercholesterolaemia Studies Collaboration (FHSC). Atherosclerosis. 2018;277:234–55 This article summarizes the diagnosis and management strategies for FH across nearly 70 countries. Management varies widely with overall suboptimal diagnosis and under-treatment.
• Vuorio A, Kuoppala J, Kovanen PT, Humphries SE, Tonstad S, Wiegman A, Drogari E, Ramaswami U (2017) Statins for children with familial hypercholesterolemia. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD006401.pub4. This systematic review assesses the effectiveness and safety of statins for the treatment of FH in children. Briefly, statins are effective with no significant safety issues.
• Joyce NR, Zachariah JP, Eaton CB, Trivedi AN, Wellenius GA. Statin use and the risk of type 2 diabetes mellitus in children and adolescents. Acad Pediatr. 2017;17:515–22 This article shows how statin use in obese children without a lipid disorder can increase their risk of developing type 2 diabetes.
Funding
This work was supported by National Heart, Lung, and Blood Institute R01 HL148217 (JPZ).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Scott Leopold declares that he has no conflict of interest.
Justin P. Zachariah declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiology/CT Surgery
Rights and permissions
About this article
Cite this article
Leopold, S., Zachariah, J.P. Pediatric Obesity, Hypertension, Lipids. Curr Treat Options Peds 6, 62–77 (2020). https://doi.org/10.1007/s40746-020-00188-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-020-00188-2