Abstract
Introduction
Gout, a common comorbidity of chronic kidney disease (CKD), is associated with high morbidity and healthcare utilization. However, a large proportion of gout remains undermanaged or untreated which may lead to worse patient outcomes and greater healthcare costs. This study estimates the present and future health and economic burden of controlled and uncontrolled gout in a virtual United States (US) CKD population.
Methods
A validated microsimulation model was used to project the burden of gout in patients with CKD in the USA through 2035. Databases were utilized to build a virtual CKD population of “individuals” with controlled or uncontrolled gout. Modelling assumptions were made on the basis of the literature, which was sparse in some cases. Health and economic outcomes with the current care (baseline) scenario were evaluated, along with potential benefits of urate-lowering intervention scenarios.
Results
The prevalence of comorbid gout and CKD in the USA was projected to increase by 29%, from 7.9 million in 2023 to 9.6 million in 2035 in the baseline scenario. Gout flares, tophi, and comorbidity development were also projected to increase markedly through 2035, with the economic burden of gout in the CKD population subsequently increasing from $38.9 billion in 2023 to $47.3 billion in 2035. An increased use of oral urate-lowering therapies in undermanaged patients, and pegloticase use in patients refractory to oral urate-lowering therapies were also project to result in 744,000 and 353,000 fewer uncontrolled gout cases, respectively, by 2035. Marked reductions in complications and costs ensued.
Conclusions
This study projected a substantial increase in comorbid gout and CKD. However, improved use of urate-lowering interventions could mitigate this growth and reduce the health and economic burdens of gout.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Chronic kidney disease (CKD) and gout are both prevalent and interrelated conditions with significant public health implications. Data on the current health and economic burden of gout in the chronic kidney disease population is sparse. Moreover, the future health and economic burden of comorbid gout and CKD is unknown. |
With both CKD and gout associated with significant healthcare resource use and costs, the study aims to quantify the economic burden imposed by comorbid gout and CKD. This understanding is vital for healthcare planning and resource allocation. Furthermore, future projections allow decision-makers to make more informed policy choices. |
This microsimulation modelling study was performed to quantify health and economic burden of controlled and uncontrolled gout in patients with CKD in the USA and assess the expected benefits of two urate-lowering intervention scenarios: optimal coverage of oral urate-lowering therapies (ULT), and optimal coverage of pegloticase with immunomodulation. |
What was learned from the study? |
The prevalence of gout and CKD are projected to increase in the USA over the next decade and this is driven primarily by population aging and CKD progression. |
As a consequence, the direct and indirect costs associated with gout in patients with CKD are projected to substantially increase, highlighting the urgent need for comprehensive disease management strategies. |
Improvement in gout management could result in lower costs, improved quality of life, and reduced gout symptoms in patients with CKD. |
The findings of the study have important implications for healthcare policy and clinical practice. |
Introduction
Chronic kidney disease (CKD) is a major public health concern with an adult prevalence of 15% in the USA [1]. CKD causes accumulation of fluids and waste in the body, which can lead to numerous complications, including heart disease and stroke. Gout is also a serious public health concern, estimated to affect 41.2 million adults globally, and over 9 million adults in the USA (2007–2016 US prevalence of 3.9%). Gout is characterized by acute episodes of inflammation with joint pain and swelling in reaction to monosodium urate (MSU) crystal deposition in and around the joints [2]. In addition to articular deposits, MSU crystal deposition has been documented in soft tissues and organs, including the kidneys, heart, and arteries [2, 3].
Patients with CKD are at higher risk for developing gout due to reduced renal excretion of serum urate (SU) [4]. Additionally, patients with gout are more susceptible to CKD development and progression [5,6,7]. Because the prevalence of gout is high in those with impaired kidney function (approximately 25% in stage 3–5 CKD) and patients with gout are more likely to develop CKD (approximately 25% have stage 3–5 CKD), both conditions place an increased burden on clinicians and the health system [8,9,10,11]. Gout and hyperuricemia are associated with poorer outcomes in patients with CKD compared to those without gout including higher risks for CKD progression, cardiovascular complications, and all-cause and cardiovascular mortality [7, 12, 13].
CKD is associated with significant healthcare resource use and costs, which were estimated at $150 billion in the USA in 2021 and they are projected to grow further [14]. Gout’s direct and indirect costs have been estimated at over $6 billion [15, 16], but the costs associated with gout within the CKD population remain largely unknown.
The American College of Rheumatology (ACR) gout management guidelines recommend maintaining SU < 6 mg/dL with oral urate-lowering therapies (ULT) in a treat-to-target fashion. For those patients with oral ULT inefficacy/intolerance and ongoing gout symptoms (≥ 2 flares/year or unresolving tophi), treatment with pegloticase, an infused medication indicated for patients who are intolerant of or refractory to oral ULTs, is recommended [17]. Maintaining SU < 6 mg/dL with oral ULTs reduces the incidence of acute flare and decreases the functional impacts of tophi [18, 19]. In patients with CKD, SU and gout control improves clinical outcomes and likely reduces the associated costs of comorbid gout and CKD [20].
This study used a validated microsimulation model [21] to build a virtual US CKD population and quantify the current health, quality of life, and economic impact of gout. Both non-intervention (current trajectory) and urate-lowering intervention scenarios were examined and compared to estimate potential patient and economic benefits of widespread gout management.
Methods
Model Structure and Parameters
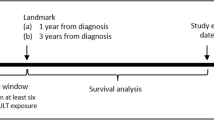
A validated microsimulation model [21] was used to create a virtual CKD population and project the epidemiological and economic burden of comorbid gout and CKD in the USA through 2035. In the start year, 2023, each virtual individual was assigned an age, sex, urinary albumin creatinine ratio (UACR), estimated glomerular filtration rate (eGFR), SU, gout status, baseline disease status (including type 2 diabetes [T2D], hypertension, coronary heart disease [CHD], and stroke) and relative risk of future disease development (termed “complication” here). The microsimulation utilized here comprised population, CKD, gout, complications, and economic modules, as detailed in Fig. 1. Gout and disease status cycled annually, accounting for advancing age and expected decline in eGFR.
Schematic of the microsimulation model. Data sources for each module are shown. CDC Centers for Disease Control and Prevention, NHANES National Health and Nutrition Examination Survey, USRDS United States Renal Data System, CKD chronic kidney disease, AHA American Heart Association, QoL quality of life, eGFR estimated glomerular filtration rate
Population Module
A virtual population of “individuals” in the USA was created using disaggregated data of the following parameters: population estimates by age and sex, population projections, total fertility rate (TFR), mothers’ age at birth, and death risk by age and sex for the USA (Supplementary Materials) [22,23,24]. The virtual population that was created in the microsimulation intentionally matched key characteristics of the US population in 2023. A total population of 200 million “individuals” was created for inclusion in the microsimulation, which was then scaled to match the true size of the US population in 2023, matching the projected population size thereafter.
CKD Module
All 200 million individuals in the full microsimulation were assigned an eGFR and UACR based on age and sex aggregated data that was extracted from the 2018 National Health and Nutrition Examination Survey (NHANES) (Supplementary Materials) [25]. UACR and eGFR values were then used to assign each individual a CKD stage using the Kidney Disease Improving Global Outcomes (KDIGO) classification [26]. This module was derived from the Inside CKD model, which is fully described elsewhere [21].
UACR and eGFR were simulated dynamically across the entire US virtual population, accounting for changes in each parameter as age increased. UACR and eGFR projections through 2035 were made by performing a multinomial logistic regression on the NHANES data. Each year, an individual’s eGFR decreased on the basis of age increase, with the eGFR decline slope determined by the individual’s initial kidney function and comorbidity status (Supplementary Materials). eGFR–age slopes were based on information available in the literature at the time of analysis (Supplementary Materials) [21, 27,28,29,30]. The dynamic year-to-year nature of eGFR and UACR in the microsimulation model allowed individuals without CKD at baseline to develop CKD and for individuals with CKD to advance disease stage each simulation year.
Gout Module
SU level data (mean and standard deviation) were extracted from the NHANES database and grouped by age (20–64, 65+ years), sex, and CKD stage (no CKD, stage 1, stage 2, and stage 3–5) (Supplementary Materials) [25]. SU level was then simulated dynamically across the US virtual population, accounting for advances in age and changes in CKD stage. The probability of having gout based on SU level was also extracted from the NHANES study and grouped by sex and CKD stage (no CKD, stage 1, stage 2, and stage 3–5) (Supplementary Materials). Gout status assignments were reassessed annually, resampling cross-sectionally for every simulation year.
The probabilities of individuals with gout having tophi and experiencing gout flares were also imputed into the model. The probability of a patient with gout experiencing flares and/or tophi was determined using SU levels (Supplement) [31, 32]. Tophi status was then used for classifying gout as tophaceous or non-tophaceous in a given model year (Supplementary Materials). These probabilities were reapplied each year in the microsimulation. Individuals with gout were further classified into having controlled or uncontrolled gout. In line with clinical practice, controlled gout was defined as the absence of tophi and < 2 flares in the simulation year (irrespective of SU levels). Uncontrolled (severe) gout was defined as SU ≥ 6 mg/dL with either ≥ 2 flares per year or the presence of tophi [33].
Comorbidity and Complication Module
Peer-reviewed publications in English through 2022 were identified by literature and Google searches of online databases. Data on complication relative risk, incidence, prevalence, and mortality for individuals with gout and/or hyperuricemia were gathered. The literature supported an independent and statistically significant effect of SU on hypertension, stroke, T2D, and CHD [34,35,36,37].
Virtual individuals were assigned a probability by age and sex of having a comorbidity (hypertension, T2D, CHD, and/or stroke) at simulation start (2023) based on prevalence data. Each subsequent year (2024–2035), individuals were assigned a certain risk of developing an incident gout-associated comorbidity (hypertension, T2D, CHD, and stroke). This risk was determined using incidence statistics by age and sex, and relative risks based on an individual’s SU level (Supplementary Materials). The risk of incident complications increased for each individual with age and SU level [34,35,36,37,38]. Individuals could have had an outcome of death from a comorbidity or any other cause based on known mortality statistics [24, 39, 40].
Health Economics Module
Annual per-patient costs for controlled and uncontrolled gout were assigned to virtual patients each year [41]. The average number of working days lost per year was also calculated on the basis of prior data [42]. Health state utility weights measure quality of life (0 = death, 1 = perfect health) and are typically measured with the EQ-5D questionnaire. Health-related quality of life was calculated for each virtual individual on the basis of their gout and comorbidity statuses (Supplementary Materials) [43].
Baseline and Intervention Scenarios
The non-intervention (“baseline”) scenario used trends of current treatment practices to project health and economic burden through to 2035. Data provided in the literature on current treatment practices were used to assign virtual individuals a probability of being on an oral ULT, depending on their eGFR [44].
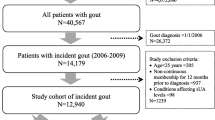
Two urate-lowering intervention scenarios were modelled. The first included oral ULT use in all patients with untreated, uncontrolled gout (oral ULT scenario) and the second included pegloticase and immunomodulator (e.g., methotrexate) co-therapy use in the subset of individuals determined to be refractory to oral ULTs (pegloticase scenario). More specifically, the oral ULT scenario “administered” oral ULT treatment to all individuals with gout, CKD, and an SU ≥ 6 mg/dL who were not receiving an oral ULT in the baseline scenario. On the basis of the literature, those “treated” with an oral ULT were assigned a 48.3% probability of achieving a sustained SU < 6 mg/dL (Fig. 2a) [45]. In the pegloticase scenario, those individuals with uncontrolled gout and CKD, who were on an oral ULT, but did not achieve an SU goal of < 6 mg/dL were “treated” with pegloticase and immunomodulator co-therapy, assigning a 71% probability of achieving a sustained SU < 6 mg/dL (Fig. 2b) [46]. All patients were assumed to be candidates for oral ULT or pegloticase treatment, as described above. Full patient adherence was also assumed, along with no premature medication discontinuation or intolerance. This was done to demonstrate the benefit of widespread improvement in serum urate management. Virtual individuals who did not respond to therapy continued their projected trajectory as if they had not received any urate-lowering intervention (baseline trajectory). In both interventions, individuals who were treatment responders were assumed to have an SU of 5.9 mg/dL through simulation end. This SU level was chosen because the data input into the model, including complication relative risk and the probability of tophi and flares, used an SU of 6 mg/dL as the reference value. Although the literature is not in full agreement on the impact of ULT on cardiovascular events [47], published evidence supports an independent and statistically significant effect of SU on hypertension, stroke, T2D, and CHD. Supportive evidence was used to derive complication risk in all virtual individuals.
Note larger numbers presented in the results have been rounded for brevity.
Ethics Approval
Ethics committee approval was not required for this study as no patient data were used, and all data sources are publicly available. These databases include the NHANES (https://wwwn.cdc.gov/nchs/nhanes/) and USRDS (https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/usrds).
Results
Non-intervention (Baseline) Scenario
The health and economic burden of controlled and uncontrolled gout in CKD was projected to markedly increase between 2023 and 2035, largely due to population aging. This resulted in a large, progressively increasing health and economic burden to patients, healthcare providers, and payers.
The number of people living with CKD was projected to grow by 17.1% between 2023 (51.6 million, 15.4% of the US population) and 2035 (60.5 million, 17.0% of the US population). The number of people living with more advanced CKD (stages 3–5) was projected to increase by 35.8% from 21.5 million (6.4% of the US population) in 2023 to 29.2 million (8.3% of the US population) in 2035 (Fig. 3).
The proportion of patients with CKD living with gout in the USA was also projected to increase, from 15.3% in 2023 to 15.9% in 2035. As a result, the number of patients with comorbid gout and CKD markedly increased over time from 7.9 million adults in 2023 to 9.6 million adults in 2035 (21.8% increase). Uncontrolled gout accounted for 2.7 million gout cases in the adult CKD population in 2023 (34.3% of gout cases in the CKD population). This number was projected to increase to 3.3 million in 2035 (5.4% of the CKD population; Table 1).
The number of flares experienced each year by the comorbid gout-CKD population was projected to increase from 5.0 million flares in 2023 to 6.15 million flares in 2035 (22.2% increase) (Table 2). Further, 1.1 million individuals with gout and CKD (13.8%) were projected to experience ≥ 2 flares/year in 2023, rising to 1.3 million (13.9%) in 2035. Additionally, 80,000 individuals (1.0%) were projected to have ≥ 6 flares/year in 2023, rising to 99,000 individuals (1.0%) in 2035. The number of patients with comorbid gout-CKD with tophacous gout was projected to increase from 2.2 million (27.8%) in 2023 to 2.7 million (27.6%) in 2035.
Gout-associated complications (new-onset comorbidities) were projected to rise markedly between 2023 and 2035 in this virtual CKD population. The simulation predicted 964,100 new cases of CHD, 908,700 new cases of hypertension, 764,600 new cases of T2D, and 441,400 new strokes through 2035.
The annual direct and indirect costs of gout in patients with CKD under the baseline scenario was $38.9 billion in 2023, increasing to $47.3 billion in 2035 (21.8% increase). Over the entire simulation time frame, cumulative cost was $568.1 billion, nearly half of which ($258.7 billion) was associated with uncontrolled gout (Table 3). A large contributor to the indirect costs of uncontrolled gout was the number of working days missed annually, which was projected to rise from 5.0 million days in 2023 to 5.7 million days in 2035 (15.2% increase).
Oral ULT Intervention
“Administering” an oral ULT to all individuals with uncontrolled gout in this virtual CKD population indicated that over half a million uncontrolled gout cases could be avoided. Oral ULT use in all patients was projected to result in approximately 613,000 fewer cases of uncontrolled gout in 2023 and 744,000 fewer cases in 2035. Maintaining SU < 6 mg/dL in this virtual population resulted in a cumulative total of 7.7 million fewer gout flares through 2035 (average of 591,000 fewer flares/year). Further, the number of tophaceous gout cases were substantially reduced with oral ULT intervention (463,000 fewer cases in 2023, 556,000 fewer cases in 2035; Fig. 4).
A projected 118,200 fewer incident complications occurred with oral ULT intervention between 2023 and 2035. During the 13-year period examined, widespread oral ULT intervention resulted in avoidance of 48,300 cases of T2D, 42,605 cases of hypertension, 19,251 strokes, and 8052 cases of CHD (Table 4).
Implementation of oral ULT use in all patients with CKD and uncontrolled gout (oral ULT intervention) also resulted in a notable enhancement in patient quality of life, with a gain of 557,000 QALYs through 2035. Employment absenteeism and presenteeism heavily contributed to the indirect costs of uncontrolled gout. However, with oral ULT intervention, a total of 16.3 million working days were gained (average of 1.3 million working days/year). Through controlling SU levels, subsequently reducing healthcare utilization and increasing productivity, widespread oral ULT use was projected to lead to direct and indirect cost savings of $58.4 billion through 2035 (average savings $4.5 billion/year) in this virtual US CKD population with uncontrolled gout. Accounting for the costs associated with the increasing number of people living with controlled gout, the projected net cost saving was $21.9 billion through 2035 (average savings $1.7 billion/year).
Pegloticase Intervention
Compared to the baseline scenario, “administering” pegloticase with immunomodulation co-therapy in virtual patients with comorbid CKD and uncontrolled gout who were not predicted to respond to an oral ULT indicated that many uncontrolled gout cases could be avoided with this next-line treatment. Pegloticase with immunomodulator co-therapy in patients with refractory gout was projected to result in approximately 292,000 fewer cases of uncontrolled gout in 2023 and 353,000 fewer cases in 2035. Maintaining SU < 6 mg/dL in the expected uncontrolled gout population resulted in a cumulative total of 3.7 million fewer gout flares through 2035 (on average, 281,000 fewer flares/year). The number of tophaceous gout cases was also dramatically reduced in the pegloticase intervention with 222,000 fewer cases in 2023 and 264,000 fewer cases in 2035 (Fig. 4).
Between 2023 and 2035, a projected 53,600 fewer incident complications occurred with pegloticase intervention. During the 13-year period examined, pegloticase with immunomodulator co-therapy resulted in 24,136 cases of T2D, 21,609 cases of hypertension, 7143 strokes, and 706 cases of CHD avoided in patients with CKD and refractory gout, compared to the baseline scenario (Table 4). The number of CHD cases avoided was not statistically significant.
Implementation of pegloticase with immunomodulator co-therapy in all patients with CKD and refractory gout (pegloticase scenario) resulted in a marked improvement in patient quality of life, with a cumulative accrual of 273,000 QALYs through 2035. Through controlling gout in this subpopulation, a total of 7.7 million working days were gained (average of 589,000 working days/year). By controlling gout in patients with CKD who were unable to be effectively managed using oral ULTs, use of pegloticase with immunomodulator co-therapy reduced the direct and indirect costs associated with gout by $27.8 billion through 2035 (average savings of $2.1 billion/year). Accounting for the costs associated with the increased number of patients with controlled gout, $10.4 billion in net savings were projected through 2035 (average savings $798.6 million/year).
Discussion
This study used microsimulation-based modelling to project the future burden of gout in patients with CKD. The microsimulation methods utilized here have been well validated [21] and capture both disease and treatment effect heterogeneity in patients with comorbid gout and CKD at an individual level. Further, our model incorporated epidemiological and treatment findings from multiple sources, including published studies, datasets, clinical trials (MIRROR randomized control trial), and observational data.
Findings of the current analyses suggest that comorbid gout and CKD will become notably more common in the USA over the next 13 years, driven largely by population aging (31% increase in individuals aged 65+) and CKD progression. In addition to patients with gout suffering with chronic pain and impaired quality of life, gout is associated with several cardiometabolic comorbidities including cardiovascular disease, diabetes, and metabolic syndrome [48, 49]. Furthermore, the management of gout-related sequelae, including comorbidities, leads to increasing healthcare costs, including medications, hospitalization, and outpatient services. Therefore, the projected increase in the comorbid gout and CKD population size has important health, quality of life, and economic implications. Finding more effective management strategies to mitigate the impact of gout and its associated sequalae will become more important year after year. Our study suggests that widespread use of ULTs in patients with comorbid gout and CKD could markedly reduce the frequency and severity of gout attacks and improve patient-reported outcomes. Moreover, by “administering” pegloticase to those individuals projected to be refractory to oral ULT, the health and quality of life burdens of uncontrolled gout were further reduced, with accompanying large healthcare cost savings.
This study had several limitations. First, prediction models rely on modelling epidemiological assumptions where evidence is not available in the literature. This can introduce some uncertainty into the results. The methods used here mitigated assumption biases because published literature was used to inform the modelling assumptions and validate the model outputs. For example, the prevalence of hypertension, stroke, T2D, and CHD in the population with gout and CKD were validated against an NHANES analysis [50]. Second, risk of developing complications associated with gout was not always known for a CKD population; therefore, this study used published relative risks based on SU data. Third, all individuals were assumed to be eligible and to remain on medication through the simulation end. However, patients with gout are often not fully adherent to taking ULTs as directed. Fourth, the literature does not have a consistent definition for uncontrolled gout. The current study defined uncontrolled gout as SU > 6 mg/dL with either ≥ 2 flares or ≥ 1 tophus. However, some studies used to determine modelling assumptions had more liberal definitions, including economic studies [41], only requiring SU > 6 mg/dL with ≥ 1 flare in the past year. This discrepancy would have underestimated the current economic projections for uncontrolled gout, and the selected definition for uncontrolled gout was chosen to avoid overestimating the benefits of improved gout control.
Future work could expand this study to focus on specific US states or regions to account for differences in patient demographics to allow policy-makers to target particular populations that have the highest prevalence of gout and CKD. The microsimulation employed in this study, or other models, could incorporate a heritability factor as both gout and hyperuricemia have been repeatedly shown to have a genetic component [51].
Conclusions
This study demonstrates the large current and potential future health and economic burden of gout in a virtual US CKD population. In 2023, an estimated 2.4% of Americans have comorbid gout and CKD, with a shocking $38.9 billion in associated costs. If current gout management trends continue, the prevalence of comorbid gout and CKD is projected to grow by over 20% through 2035, with costs expected to reach nearly $50 billion in 2035. Effective, comprehensive, and thorough SU control was projected to result in sizable improvements in health, quality of life, and healthcare cost savings.
Data Availability
The data sets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
US Centers for Disease Control and Prevention. Chronic kidney disease in the United States, 2021. 2021. https://www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html. Accessed March 2024
Roddy E, Doherty M. Epidemiology of gout. Arthritis Res Ther. 2010;12(6):223.
Centers for Disease Control and Prevention. Gout. 2023. https://www.cdc.gov/arthritis/types/gout.html. Accessed May 2024
Stamp LK, Farquhar H, Pisaniello HL, et al. Management of gout in chronic kidney disease: a G-CAN consensus statement on the research priorities. Nat Rev Rheumatol. 2021;17:633–41.
Li L, Yang C, Zhao Y, Zeng X, Liu F, Fu P. Is hyperuricemia an independent risk factor for new-onset chronic kidney disease?: a systematic review and meta-analysis based on observational cohort studies. BMC Nephrol. 2014;15(1):122.
Jeyaruban A, Hoy W, Cameron A, et al. Hyperuricaemia, gout and allopurinol in the CKD Queensland registry. J Nephrol. 2021;34(3):753–62.
Austin GS, Michelle Elizabeth J, Betina B, et al. Gout and the risk of advanced chronic kidney disease in the UK health system: a national cohort study. BMJ Open. 2019;9(8):e031550.
Krishnan E. Reduced glomerular function and prevalence of gout: NHANES 2009–10. PLoS ONE. 2012. https://doi.org/10.1371/journal.pone.0050046. Accessed May 2024.
Singh JA, Cleveland JD. Gout is associated with a higher risk of chronic renal disease in older adults: a retrospective cohort study of U.S. Medicare population. BMC Nephrol. 2019;20(1):93.
Roughley MJ, Belcher J, Mallen CD, Roddy E. Gout and risk of chronic kidney disease and nephrolithiasis: meta-analysis of observational studies. Arthritis Res Ther. 2015;17(1):90.
Mohammed E, Browne LD, Kumar AUA, Adeeb F, Fraser AD, Stack AG. Prevalence and treatment of gout among patients with chronic kidney disease in the Irish health system: a national study. PLoS ONE. 2019;14(1):e0210487.
Zhang J, Lu X, Li H, Wang S. Serum uric acid and mortality in patients with chronic kidney disease: a systematic review and meta-analysis. Blood Purif. 2021;50(6):758–66.
Kuo CF, See LC, Luo SF, et al. Gout: an independent risk factor for all-cause and cardiovascular mortality. Rheumatology (Oxford). 2010;49(1):141–6.
Mennini FS, et al. Inside CKD: projecting the economic burden of chronic kidney disease using patient-level microsimulation modelling. 2021. https://www.healthlumen.com/wp-content/uploads/2022/06/posb68-inside-ckdispor-eucost-burdenposterrevised-submission-pdf.pdf. Accessed May 2024.
Wertheimer A, Morlock R, Becker MA. A revised estimate of the burden of illness of gout. Curr Ther Res Clin Exp. 2013;75:1–4.
Jackson R, Shiozawa A, Buysman EK, Altan A, Korrer S, Choi H. Flare frequency, healthcare resource utilisation and costs among patients with gout in a managed care setting: a retrospective medical claims-based analysis. BMJ Open. 2015;5(6):e007214.
FitzGerald JD, Dalbeth N, Mikuls T, et al. 2020 American College of Rheumatology guideline for the management of gout. Arthritis Care Res (Hoboken). 2020;72(6):744–60.
Shoji A, Yamanaka H, Kamatani N. A retrospective study of the relationship between serum urate level and recurrent attacks of gouty arthritis: evidence for reduction of recurrent gouty arthritis with antihyperuricemic therapy. Arthritis Rheum. 2004;51(3):321–5.
Perez-Ruiz F, Calabozo M, Pijoan JI, Herrero-Beites AM, Ruibal A. Effect of urate-lowering therapy on the velocity of size reduction of tophi in chronic gout. Arthritis Rheum. 2002;47(4):356–60.
Mitri G, Wittbrodt ET, Turpin RS, Tidwell BA, Schulman KL. Cost comparison of urate-lowering therapies in patients with gout and moderate-to-severe chronic kidney disease. J Manag Care Spec Pharm. 2016;22(4):326–36.
Tangri N, Chadban S, Cabrera C, Retat L, Sánchez JJG. Projecting the epidemiological and economic impact of chronic kidney disease using patient-level microsimulation modelling: rationale and methods of inside CKD. Adv Ther. 2023;40(1):265–81.
United Nations. World Population Prospects 2022. 2022. https://population.un.org/wpp/. Accessed May 2024.
National Vital Statistics Reports. Births: final data for 2020. 2022. https://www.cdc.gov/nchs/data/nvsr/nvsr70/nvsr70-17.pdf. Accessed May 2024.
National Vital Statistics Reports. Deaths: final data for 2019. 2021. https://www.cdc.gov/nchs/data/nvsr/nvsr70/nvsr70-08-508.pdf. Accessed May 2024.
National Health and Nutrition Examination Survey (NHANES). Datasets, and related documentation. NHANES 2017–2018. 2018 https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2017. Accessed May 2024.
Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158(11):825–30.
NHS Digital. Health Survey for England, 2016. 2017. https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/health-survey-for-england-2016. Accessed 29 July 2020.
Boulware LE, Jaar BG, Tarver-Carr ME, Brancati FL, Powe NR. Screening for proteinuria in US adults: a cost-effectiveness analysis. JAMA. 2003;290(23):3101–14.
Khan NA, Ma I, Thompson CR, et al. Kidney function and mortality among patients with left ventricular systolic dysfunction. J Am Soc Nephrol. 2006;17(1):244–53.
Barzilay JI, Davis BR, Pressel SL, et al. The effects of eGFR change on CVD, renal, and mortality outcomes in a hypertensive cohort treated with 3 different antihypertensive medications. Am J Hypertens. 2018;31(5):609–14.
Becker MA, Schumacher HR, Espinoza LR, et al. The urate-lowering efficacy and safety of febuxostat in the treatment of the hyperuricemia of gout: the CONFIRMS trial. Arthritis Res Ther. 2010;12(2):R63.
Khanna PP, Nuki G, Bardin T, et al. Tophi and frequent gout flares are associated with impairments to quality of life, productivity, and increased healthcare resource use: results from a cross-sectional survey. Health Qual Life Outcomes. 2012;10(117):1–11.
Bursill D, Taylor WJ, Terkeltaub R, et al. Gout, Hyperuricaemia and Crystal-Associated Disease Network (G-CAN) consensus statement regarding labels and definitions of disease states of gout. Ann Rheum Dis. 2019;78(11):1592–600.
Grayson PC, Kim SY, LaValley M, Choi HK. Hyperuricemia and incident hypertension: a systematic review and meta-analysis. Arthritis Care Res (Hoboken). 2011;63(1):102–10.
Zhong C, Zhong X, Xu T, Xu T, Zhang Y. Sex-specific relationship between serum uric acid and risk of stroke: a dose-response meta-analysis of prospective studies. J Am Heart Assoc. 2017;6(4):e005042.
Bhole V, Choi JWJ, Kim SW, Vera MD, Choi H. Serum uric acid levels and the risk of type 2 diabetes: a prospective study. Am J Med. 2010;123(10):957–61.
Kim SY, Guevara JP, Kim KM, Choi HK, Heitjan DF, Albert DA. Hyperuricemia and coronary heart disease: a systematic review and meta-analysis. Arthritis Care Res (Hoboken). 2010;62(2):170–80.
Stewart JD, Langlois V, Noone D. Hyperuricemia and hypertension: links and risks. Integr Blood Press Control. 2019;12:43–72.
CDC. Underlying Cause of Death 1999–2020. ICD code I60-I69. 2020. http://wonder.cdc.gov/ucd-icd10.html. Accessed May 2024
National Vital Statistics Reports. Deaths: final data for 2017. 2019. https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_09-508.pdf. Accessed May 2024
Flores NM, Nuevo J, Klein AB, Baumgartner S, Morlock R. The economic burden of uncontrolled gout: how controlling gout reduces cost. J Med Econ. 2019;22(1):1–6.
Jaffe DH, Klein AB, Benis A, et al. Incident gout and chronic kidney disease: healthcare utilization and survival. BMC Rheumatol. 2019;3(1):11.
Wood R, Fermer S, Ramachandran S, Baumgartner S, Morlock R. Patients with gout treated with conventional urate-lowering therapy: association with disease control, health-related quality of life, and work productivity. J Rheumatol. 2016;43(10):1897–903.
Chen-Xu M, Yokose C, Rai SK, Pillinger MH, Choi HK. Contemporary prevalence of gout and hyperuricemia in the United States and decadal trends: the national health and nutrition examination survey 2007–2016. Arthritis Rheumatol. 2019;71(6):991–9.
Becker MA, Fitz-Patrick D, Choi HK, et al. An open-label, 6-month study of allopurinol safety in gout: the LASSO study. Semin Arthritis Rheum. 2015;45(2):174–83.
Botson JK, Saag K, Peterson J, et al. A randomized, placebo-controlled study of methotrexate to increase response rates in patients with uncontrolled gout receiving pegloticase: primary efficacy and safety findings. Arthritis Rheumatol. 2023;75(2):293–304.
National Institute for Health and Care Excellence. Gout: diagnosis and management. Evidence reviews for urate-lowering therapies for the long-term management of gout 2022. https://www.nice.org.uk/guidance/ng219/chapter/Recommendations. Accessed May 2024.
Choi HK, McCormick N, Yokose C. Excess comorbidities in gout: the causal paradigm and pleiotropic approaches to care. Nat Rev Rheumatol. 2022;18(2):97–111.
Thottam GE, Krasnokutsky S, Pillinger MH. Gout and metabolic syndrome: a tangled web. Curr Rheumatol Rep. 2017;19(10):60.
Zhu Y, Pandya BJ, Choi HK. Comorbidities of gout and hyperuricemia in the US general population: NHANES 2007–2008. Am J Med. 2012;125(7):679-87.e1.
Nian YL, You CG. Susceptibility genes of hyperuricemia and gout. Hereditas. 2022;159(1):30.
Acknowledgements
We acknowledge Marek Pietrowski and Michael Xu for model development, John Guzek and Timothy LR Coker for data analysis support, and Markiyan Mitchyn for epidemiological and cost research support.
Funding
This study was funded by Horizon Therapeutics plc (now Amgen, Inc). The journal’s Rapid Service Fee and publication costs were funded by Amgen, Inc.
Author information
Authors and Affiliations
Contributions
Joshua Card-Gowers, Laura Webber, and Lise Retat contributed to the data collection and analysis, microsimulation modelling, and analysis of results. Joshua Card-Gowers wrote the original manuscript draft, and all authors critically reviewed the manuscript. Brian LaMoreaux, Brad A Marder, and Ada Kumar provided medical expertise and critically reviewed study methods and results. Lissa Padnick-Silver provided critical review of study results and medical writing. All authors approved the final submitted version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Joshua Card-Gowers and Laura Webber are employees of HealthLumen Limited, who were commissioned by Horizon (now Amgen, Inc.) to perform simulation modelling and provide medical writing support. Lise Retat was an employee at HealthLumen at the time of this study, and is now employed at AstraZeneca. Brian LaMoreaux, Brad A Marder, Lissa Padnick-Silver, and Ada Kumar are employees of and stockholders in Amgen, Inc. (formerly Horizon Therapeutics).
Ethical Approval
Ethics committee approval was not required for this study as no patient data were used, and all data sources are publicly available. These databases include the NHANES (https://wwwn.cdc.gov/nchs/nhanes/) and USRDS (https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/usrds).
Additional information
Lise Retat’s affiliation has changed since the time of this study.
Prior Presentation: Marder B, et al. 2023. Projected benefits of gout control on the health and economic burden of patients with CKD and uncontrolled gout. FR-PO921. Poster presented at the 2023 annual meeting of the American Society of Nephrology (ASN), November 2–5 (Philadelphia, PA). Card-Gowers J, et al. 2023. Present and Future Health and Economic Burden of Controlled and Uncontrolled Gout in Patients with Chronic Kidney Disease in the United States. Poster presented at the European Congress of Rheumatology (EULAR), May 31–June 3 (Milan, Italy).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Card-Gowers, J., Retat, L., Kumar, A. et al. Projected Health and Economic Burden of Comorbid Gout and Chronic Kidney Disease in a Virtual US Population: A Microsimulation Study. Rheumatol Ther (2024). https://doi.org/10.1007/s40744-024-00681-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40744-024-00681-2