Abstract
Introduction
To evaluate the effect of guselkumab on work productivity and nonwork daily activity impairment and general health status through 2 years in patients who were biologic-naïve with active psoriatic arthritis (PsA) in the phase 3 DISCOVER-2 clinical trial.
Methods
Adult patients with PsA were randomized to subcutaneous injections of guselkumab 100 mg every 4 weeks (Q4W); at weeks 0, 4, then every 8 weeks (Q8W); or placebo (through week 24 with crossover to guselkumab Q4W). Work productivity and nonwork daily activity impairment were assessed using the Work Productivity and Activity Impairment Questionnaire for PsA (WPAI-PsA) and patient-reported general health status using the EuroQol 5-Dimension 5-Level (EQ-5D-5L) Index and EQ-Visual Analog Scale (EQ-VAS). Least-squares (LS) mean changes from baseline in WPAI-PsA domains and EQ-5D-5L/EQ-VAS were assessed through week 100. Changes in employment status were utilized to estimate potential indirect savings from improved work productivity.
Results
Of 739 randomized patients, 738 had available baseline data for the analyses (Q4W 245; Q8W 248; placebo 245). At week 24, greater improvements in work productivity, nonwork daily activity, and EQ-5D-5L/EQ-VAS were observed in the Q4W and Q8W groups versus the placebo group. At week 100, LS mean reductions in work productivity impairment (− 23.8% to − 28.0%) and nonwork daily activity impairment (– 26.6% to − 29.2%) and improvements in EQ-5D-5L/EQ-VAS (0.14 to 0.15/21.2 to 25.0) were maintained in patients receiving guselkumab. Among patients employed at baseline, 12.1–16.4% were not employed at week 100, and 20.0–25.3% shifted from not employed at baseline to employed at week 100. Potential yearly indirect cost savings (USD) from improved work productivity at week 100 ranged from $16,529 to $19,409.
Conclusion
Patients with active PsA treated with guselkumab demonstrated reduced impairment in work productivity and nonwork daily activity, together with improvement in general health status and substantial potential cost savings, over a 2-year period.
Trial Registration
Clinicaltrials.gov identifier: NCT03158285.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The efficacy and safety of guselkumab for psoriatic arthritis (PsA) have been previously demonstrated in phase 3 trials. Treatment with guselkumab 100 mg every 4 or 8 weeks (Q4W/Q8W) in patients with active PsA was associated with reduced impairment in work productivity and nonwork daily activity and enhanced overall patient health-related quality of life through 1 year. Durability of treatment effect on quality of life is important for patients. |
The objective of these analyses was to evaluate the effect of guselkumab on work productivity and nonwork daily activity impairment and general health status through 2 years in patients with active PsA (biologic-naïve) in the DISCOVER-2 clinical trial. |
What was learned from the study? |
Reductions in impairment of work productivity and nonwork daily activity and improved general health status were maintained through up to 2 years of treatment with guselkumab Q4W/Q8W in patients with active PsA who were biologic-naïve. Improvements in work productivity were estimated to result in substantial yearly indirect work productivity-related cost savings. |
Reducing the signs and symptoms of PsA through inhibition of the interluekin-23p19 subunit with guselkumab may result in improvements in health-related quality of life through lessening the impact of PsA on work productivity, nonwork daily activity, and general health status. |
Introduction
Psoriatic arthritis (PsA) is a chronic inflammatory disease that can lead to substantial impairment in physical function and a high degree of disability [1,2,3], reflecting symptomatology across a variety of affected domains, such as skin, joints, and entheses, as well as systemic features, including fatigue, reduced cognitive function, and low mood. Structural damage in patients with PsA is further linked to physical functional impairment, which can be irreversible [4]. Consequently, patients with PsA often report impairments in work productivity and nonwork daily activity and reduced general health-related quality of life (HRQoL) compared with the general population [3, 5,6,7]. Globally, an estimated 20–50% of patients with PsA are unemployed, and 16–39% report some degree of work disability [6,7,8]. A recent retrospective analysis demonstrated that patients with PsA frequently bear substantial costs related to nonrecreational work absences, sick leaves, and short-term work disability in the USA [9]. Furthermore, patients with PsA tend to experience impairments in work productivity, nonwork daily activity, and HRQoL as well as work-related costs that are, on average, greater in patients with PsA than in those with cutaneous psoriasis alone [6, 9, 10].
Guselkumab, a high-affinity, fully human, interleukin-23 p19-subunit inhibitor, was the first selective agent in its class approved by the US Food and Drug Administration to treat adults with active PsA [11, 12]. The efficacy and safety of guselkumab in patients with PsA despite standard therapies was established in the pivotal phase 3 DISCOVER-1 (1 year; patients who were biologic-naïve and biologic-experienced) and DISCOVER-2 (2 years; patients who were biologic-naïve) studies [13, 14]. In both studies, at week 24, patients who received subcutaneous guselkumab 100 mg every 4 or 8 weeks (Q4W/Q8W) demonstrated significantly greater improvements across PsA domains compared with those receiving placebo [15]. In addition, guselkumab Q4W was associated with significantly less progression of structural damage up to week 24 compared with placebo [14]. Robust improvements were maintained in the patients treated with guselkumab through 1 year in DISCOVER-1 and 2 years in DISCOVER-2 [16,17,18].
In DISCOVER-2, patients receiving guselkumab, regardless of dosing regimen, reported reduced work productivity loss and nonwork daily activity impairment, as well as improved general health status through 1 year [19, 20]. Understanding the durability of the effects of guselkumab on these outcomes is important for patients with PsA and their health care providers. Thus, we further evaluated the long-term effects of guselkumab therapy on work productivity and nonwork daily activity impairment; employment; and general health status through 2 years in the DISCOVER-2 trial.
Methods
Patients and Study Design
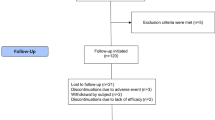
DISCOVER-2 (Clinicaltrials.gov identifier: NCT03158285) was a phase 3, randomized, double-blind, placebo-controlled trial. Study design details and full inclusion/exclusion criteria have been previously reported [14]. Eligible patients were aged ≥ 18 years and biologic-naïve and met the classification criteria for PsA (CASPAR) [21]. Study participants had active disease (≥ 5 swollen and ≥ 5 tender joints and C-reactive protein [CRP] ≥ 0.6 mg/dL) despite prior therapy with conventional systemic disease-modifying antirheumatic drugs (csDMARDs), apremilast, or nonsteroidal anti-inflammatory drugs [14]. Patients were randomized (1:1:1) to receive subcutaneous guselkumab 100 mg Q4W; guselkumab 100 mg at weeks 0, 4, and then Q8W; or placebo. Randomization was stratified by the most recent high-sensitivity serum CRP value before randomization (< 2.0 vs. ≥ 2.0 mg/dL) and by baseline csDMARD use (yes vs. no). At week 24, patients randomized to placebo crossed over to receive subcutaneous guselkumab 100 mg Q4W. Concomitant use of selected nonbiologic therapies was permitted at stable doses.
This study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines. All patients provided written informed consent, and the protocol was approved by local institutional review boards or ethics committees (for several US sites, Sterling Institutional Review Board approval number: 5910C) (Electronic Supplementary Material [ESM] Table S1).
Assessments
Work productivity, nonwork daily activity impairment, and employment status at weeks 0, 16, 24, 52, and 100 were assessed using the Work Productivity and Activity Impairment Questionnaire for PsA (WPAI-PsA), a validated instrument that evaluates the impact of PsA on patients’ ability to work (among patients working at baseline) and perform daily nonwork activities (among all patients) during the previous 7 days [22, 23]. Four scores are derived from the questionnaire: percentage of work time missed (absenteeism), percentage of reduced productivity while at work (presenteeism), an overall work productivity impairment score that combines absenteeism and presenteeism, and percentage of impairment in activities performed outside of work.
Changes in employment status for all patients and potential indirect savings from improved overall work productivity for employed patients also were assessed. The latter were estimated by multiplying the Organization for Economic Co-operation and Development (OECD)-reported average wages for 2020 for Europe (including France, Germany, Italy, Spain, and the UK), the USA, and Japan [24] by the percentage change from baseline in WPAI-PsA overall work productivity impairment at weeks 24 and 100 for each treatment group. Note that all values are presented in US dollars (USD).
General health status was evaluated using the patient-reported EuroQol 5-Dimension 5-Level (EQ-5D-5L) Index and EuroQol Visual Analog Scale (EQ-VAS) [25], administered at weeks 0, 16, 24, 52, and 100. Patients completed the EQ-5D-5L questionnaire by rating each of five dimensions (mobility, self-care, ability to perform usual activities, pain/discomfort, and anxiety/depression) as one of five levels of difficulty (no, slight, moderate, severe, or extreme problems) [26]. The individual dimension scores were converted into a single summary index score on a scale of 0 (death) to 1 (perfect health) [26, 27]. The questionnaire also includes the EQ-VAS, on which patients rated their daily health status from 0 (worst imaginable) to 100 (best imaginable). EQ-5D-5L value sets are country-specific; the current analyses utilized a US-based value set.
Statistical Analyses
Change From Baseline in WPAI-PsA and EQ-5D-5L/EQ-VAS
As previously reported [19], least-squares (LS) mean changes from baseline in WPAI-PsA domains were determined using an analysis of covariance model that included all available data at each time point. LS means and 95% confidence intervals were calculated as the average of all multiple imputation datasets at weeks 24, 52 and 100. Changes in absenteeism, presenteeism, and overall work productivity impairment were assessed in patients employed at baseline who had post-baseline values. Changes in nonwork daily activity impairment were assessed in all patients who had post-baseline values. The proportions of patients who achieved the minimum clinically important difference (MCID) in work productivity (15% improvement) [23] and nonwork daily activity impairment (20% improvement) [23] were determined among patients with ≥ 15% impairment and ≥ 20% impairment, respectively, at baseline.
LS mean changes from baseline in EQ-5D-5L Index and EQ-VAS scores by visit were estimated using a mixed-effects model for repeated measures (MMRM) that included all available data at each time point. The minimal important differences (MIDs) for the EQ-5D-5L Index and EQ-VAS (i.e., statistically-derived minimum values) were defined as one-half the standard deviation (SD) of the baseline score [28]. The proportions of patients who achieved the MID for each measure were determined at weeks 16, 24, 52, and 100.
Analyses used observed data, except for the treatment effect on the EQ-5D-5L Index, as previously described [20]. Briefly, for analyses of changes in EQ-5D-5L, treatment failure rules were applied through week 24, and missing data (for patients who had not discontinued the study) after week 24 were imputed as 0 or nonresponse; no imputation was performed for patients who had discontinued the study.
The significance level of all statistical tests reported for WPAI-PsA and general health status outcomes were based on α = 0.05 (2-tailed) through week 24 [19, 20]; no treatment group comparisons were performed thereafter. Statistical analyses were performed using the SAS, version 9.4 statistical package (SAS Institute, Cary, NC, USA) and R-studio version 1.3.1056 ® Foundation for Statistical Computing, Vienna, Austria).
Changes From Baseline in Employment
Changes in employment status over the trial period were assessed post hoc by analyzing shifts in patient-reported employment status by treatment group from baseline through week 100. All patients were included in these analyses and were grouped by employment status (employed or unemployed) at baseline.
Results
Patients
A total of 739 patients were randomized and treated in DISCOVER-2 [14]; 652 (88.2%) patients completed study treatment through 2 years [18]. These data were collected from July 2017 through December 2020. Baseline demographic and disease characteristics related to work/employment and HRQoL have been previously described and are summarized in ESM Table S2 and ESM Table S3 [14, 19, 20]. At baseline (N = 739), the mean age was 46 years, 98% were white, and slightly less than half (47.5%) were female. At baseline, patients had moderately to highly active disease (mean [SD] swollen joint count: 12.3 [7.2]; tender joint count: 21.3 [12.9]; patient pain score: 6.3 [1.9]; median CRP: 1.2 mg/dL).
Although 64.4% of patients were actively employed at baseline, meaningful impairment was observed in most of the WPAI-PsA domains, including an overall mean (SD) percentage of presenteeism of 48.3% (24.7), work productivity impairment of 51.4% (25.9), and percentage of nonwork daily activity impairment of 55.5% (22.8). Overall, the mean (SD) percentage of absenteeism at baseline due to PsA was 11.2% (22.7) and ranged from 8.4% to 14.5% across the treatment groups. In addition, among patients actively employed at baseline (N = 475), 38.7% reported missed work time due to PsA, and nearly all reported impairment while working (presenteeism: 93.6%) as well as impairments in overall work productivity (93.9%) and nonwork daily activity (97.8%). Moderate impairment in general health status at baseline also was evident from a mean (SD) EQ-5D-5L Index score of 0.6 (0.1) and EQ-VAS score of 44.6 (19.7), both of which were below the US population norms of 0.9 and 79.3, respectively [29].
Effects of Guselkumab on Work Productivity and Nonwork Daily Activity Impairment
Change From Baseline in WPAI-PsA
Reductions in work productivity loss and nonwork daily activity impairment in patients treated with guselkumab were previously reported through 1 year in DISCOVER-2 [19]. Patients randomized to guselkumab demonstrated significantly greater improvements in work productivity and nonwork daily activity impairment versus patients receiving placebo through week 24 in both the Q4W and Q8W groups, and improvements were maintained through week 52 (Fig. 1). In both guselkumab groups, continued LS mean improvements from baseline in presenteeism and work productivity (among patients employed at baseline) were observed at week 100 (presenteeism: Q4W − 26.3%, Q8W −28.0%; work productivity impairment: Q4W − 23.8%, Q8W − 28.0%) (Fig. 1). Similar results were observed for reductions in nonwork daily activity impairment (all patients; employed and not employed), with significantly greater LS mean changes in the guselkumab groups (Q4W: − 20.5%, Q8W − 21.2%) compared with placebo (− 9.9%) at week 24, with maintenance of effect through 1 year in guselkumab-randomized patients (Fig. 1). At week 100, LS mean reductions in nonwork daily activity impairment were − 29.2% in the Q4W group and − 28.0% in the Q8W group (Fig. 1). Among placebo→Q4W patients, LS mean reductions in presenteeism, work productivity impairment, and nonwork daily activity impairment approached those of the guselkumab groups at week 52 (Fig. 1) and further improved at week 100: −24.2%, −24.1%, and −26.6%, respectively. Among 184 patients overall who reported missing work at baseline due to PsA, LS mean changes in absenteeism were stable over time and ranged from − 1.8% to − 4.2% at week 100 across treatment groups (Fig. 1).
Least-squares mean change from baseline through week 100 in WPAI-PsA absenteeism (a), presenteeism (b), work productivity loss (c), and nonwork daily activity impairment (d). Absenteeism = work time missed; presenteeism = reduced productivity while at work. LS mean changes from baseline in WPAI-PsA domains were calculated for each multiple imputation dataset using an analysis of covariance; reported LS mean = average of all multiple imputation datasets.. Patients receiving PBO crossed over to GUS 100 mg Q4W at week 24. Asterisk indicates a significant difference at *p < 0.04. GUS guselkumab, LS least-squares, PBO placebo, Q4W every 4 weeks, Q8W every 8 weeks, WPAI-PsA Work Productivity and Activity Impairment Questionnaire for Psoriatic Arthritis
Among patients with ≥ 15% work productivity impairment at baseline (89.5%, 394/440), 57.5–58.5% (week 16) and 60.0–67.2% (week 24) of patients in the guselkumab groups achieved the MCID (≥ 15%) versus 46.6% and 53.4%, respectively, in the placebo group (Fig. 2). In the Q4W and Q8W groups, response rates were maintained through week 52 (Fig. 2) and were increased at week 100 (Q4W: 76.9%; Q8W: 77.3%) (Fig. 2). Among patients with nonwork daily activity impairment ≥ 20% at baseline (95.0%, 701/738), response rates for MCID at weeks 16 and 24 were significantly greater in both guselkumab groups (55.1–62.1%) versus placebo (40.9–41.7%; p ≤ 0.002 for both time points) (Fig. 2). Among guselkumab-randomized patients, response rates were maintained through week 52 [19] and increased to 76.8% and 74.5% in the Q4W and Q8W groups, respectively, at week 100 (Fig. 2). The response rates for achieving the MCID in work productivity impairment and nonwork daily impairment among placebo→Q4W patients at week 52 and week 100 were consistent with those of the guselkumab groups (Fig. 2).
Proportions of patients who achieved MCID improvements from baseline in WPAI-PsA work productivity loss (≥ 15%) (a) and nonwork daily activity impairment (≥ 20%) (b) through week 100. GUS guselkumab, MCID minimum clinically important difference, PBO placebo, Q4W every 4 weeks, Q8W every 8 weeks, WPAI-PsA Work Productivity and Activity Impairment Questionnaire for Psoriatic Arthritis
Change From Baseline in Employment
Changes in employment status were previously reported through 1 year of DISCOVER-2 [19]. Among patients who were not employed at baseline (35.6%, 263/738), 13.0% (n = 12) and 12.4% (n = 12) of patients in the guselkumab Q4W and Q8W groups, respectively, and 8.1% (n = 6) of those in the placebo group reported active employment at week 16. At week 52 (when all patients were receiving guselkumab), 25.6% (n = 22) of patients in the guselkumab Q4W group, 23.1% (n = 21) of those in the guselkumab Q8W group, and 17.1% (n = 12) of those in the placebo→Q4W group reported active employment at week 52 (Fig. 3); additionally, 24.1% (n = 20), 25.3% (n = 22), and 20.0% (n = 13), respectively, of those who were not employed at baseline reported active employment at week 100.
Employment status through week 100 for patients who were not employed at baseline (a) and those who were employed at baseline (b). Patients with missing data among those not employed at baseline per treatment group are: GUS 100 mg Q4W: W16, 3.3%; W24, 2.2%; W52, 1.2%; GUS 100 mg Q8W: W16, 1.0%; W24, 2.1%; PBO→GUS 100 mg Q4W (W24-100): W16, 1.4%; W24, 1.4%. Patients with missing data among those employed at baseline per treatment group are: GUS 100 mg Q4W: W16, 1.3%; W24, 2.0%; GUS 100 mg Q8W: W16, 2.6%; W24, 2.0%; PBO→GUS 100 mg Q4W (W24–100): W24, 1.2%. GUS guselkumab, PBO placebo, Q4W every 4 weeks, Q8W every 8 weeks, W week
At baseline, 64.4% (475/738) of patients reported being employed. Of these, the proportions of patients whose status in employment shifted to ‘not employed’ were numerically smaller in the guselkumab Q4W and Q8W groups versus the placebo group at week 16 (5.2% [n = 8], 6.0% [n = 9], and 9.4% [n = 16], respectively) and week 24 (6.5% [n = 10], 3.3% [n = 5], and 10.5% [n = 18], respectively). At week 52, (when all patients were receiving guselkumab), 8.3% (n = 12) in the guselkumab Q4W group, 8.4% (n = 12) in the guselkumab Q8W group, and 13.8% (n = 22) in the placebo→Q4W group who were employed at baseline reported not being employed at week 52 (Fig. 3); 16.1% (n = 22), 12.4% (n = 17), and 16.1% (n = 24), respectively, reported not being employed at week 100. Most patients who were employed at baseline reported active employment at the time points assessed through week 100 (83.9% to 87.6%) (Fig. 3).
Cost Analyses
Cost analyses through 1 year [19] suggested that annualized monetized employment-related productivity gains associated with guselkumab treatment of PsA could result in significant indirect and employer-related economic benefits. Potential yearly indirect cost savings from improved overall work productivity at week 24 in Europe, the USA, and Japan were similar between the guselkumab groups and nearly twofold greater than in patients treated with placebo (Fig. 4). At week 100, potential yearly cost savings in the USA were generally consistent across guselkumab treatment groups: Q4W, US$16,529; Q8W, US$19,409; and placebo→Q4W group, US$16,716 (Fig. 4).
Effects of Guselkumab on General Health Status
Change From Baseline in EQ-5D-5L Index and EQ-VAS Scores
Improvements in general health status through 1 year in patients treated with guselkumab were previously reported [20]. Patients randomized to guselkumab had greater LS mean improvements compared with placebo in both the EQ-5D-5L Index and EQ-VAS scores at week 16, the earliest post-baseline assessment, which further improved in both guselkumab groups at week 24 (Fig. 5). LS mean changes from baseline in both scores in the guselkumab groups were maintained through week 100 (EQ-5D-5L: 0.15 in both groups; EQ-VAS: Q4W, 25.0; Q8W, 24.6) (Fig. 5). In the placebo→Q4W group, mean changes in these scores at week 52 and at week 100 were similar to those of the Q4W and Q8W groups (Fig. 5).
LS mean change from baseline through week 100 in EQ-5D-5L Index (a) and EQ-VAS (b). LS mean changes from baseline in the EQ-5D-5L Index and EQ-VAS scores by visit were estimated using mixed-effects model for repeated measures (MMRM). Patients receiving PBO crossed over to GUS 100 mg Q4W at week 24. Asterisk indicates nominal p-value < 0.0001 versus PBO. EQ-5D-5L EuroQol 5-Dimension 5-Level Index, EQ-VAS EuroQol Visual Analog Scale, GUS guselkumab, LS least-squares, PBO placebo, Q4W every 4 weeks, Q8W every 8 weeks
At week 24, 56.0% of patients treated with guselkumab achieved an improvement in the EQ-5D-5L Index ≥ the established MID (0.1), compared with 43.4% in the placebo group (Fig. 6). At week 52, > 65% of all patients (including those in the placebo→Q4W group) achieved the MID, and response rates ranged from 66.1% to 71.8% at week 100 (Fig. 6).
Proportions of patients who achieved improvements in the EQ-5D-5L Index (a) and EQ-VAS (b) greater than or equal to the MIDs through week 100. EQ-5D-5L EuroQol 5-Dimension 5-Level, EQ-VAS EuroQol Visual Analog Scale, GUS guselkumab, MIDs minimal important differences, PBO placebo, Q4W every 4 weeks, Q8W every 8 weeks
Similar results were observed for the proportions of patients achieving the established MID (9.86) in the EQ-VAS through week 100 (Fig. 6). At week 24, approximately 63% of patients treated with guselkumab achieved the MID compared with 44.4% of patients receiving placebo. Across treatment groups, response rates ranged from 67.1% to 73.8% at week 52 and from 72.8% to 77.5% at week 100 (Fig. 6).
Discussion
The majority of DISCOVER-2 participants presented with substantial impairment of work productivity, nonwork daily activity, and general health status at baseline, consistent with previous analyses of patients with PsA [7,8,9, 30]. Unemployment and work productivity loss in patients with PsA represent significant patient, employer, and societal burdens [7, 30]. Importantly, treatment goals for patients with PsA include optimization of functional status [31], which may lead to improvements in work and nonwork daily productivity and general health status.
As previously reported, improvements (reduced impairment) from baseline at W24 were greater in guselkumab-treated versus placebo-treated patients for presenteeism (Q4W group: − 20.1%; Q8W group: − 19.6%; placebo group: − 10.5%), work productivity (Q4W: − 20.1%; Q8W: − 19.2%; placebo: − 10.6%), and nonwork activity (Q4W: − 20.5%; Q8W: − 21.2%; placebo: − 9.9%) [19]. Similarly, greater LS mean improvements from baseline at W24 in the Q4W/Q8W versus placebo groups were observed for EQ-5D-5L (both 0.12 vs. 0.05) and EQ-VAS (18.2/18.4 vs. 6.8) [20]. Approximately 73% of patients treated with guselkumab in DISCOVER-2, including those who crossed over from placebo at week 24, achieved meaningful improvements in work productivity and nonwork daily activity at week 100. Likewise, 66.1–71.8% and 72.8–77.5% of patients treated with guselkumab achieved MIDs in the EQ-5D-5L and EQ-VAS, respectively, at week 100. Employment rates remained generally stable through 2 years in patients employed at baseline (≥ 84%). Although the majority of patients randomized to guselkumab who were employed at baseline continued to be employed at 2 years, 14.2% reported not being employed at week 100; among patients not employed at baseline, 24.7% reported being employed at week 100. The long-term improvements in work productivity and overall health status observed among patients with PsA receiving guselkumab were also associated with potential indirect and employer-related economic benefits.
Current treatment recommendations from the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) are generally tailored to address the six disease domains for PsA: peripheral arthritis, axial disease, enthesitis, dactylitis, and skin/nail disease [31]. Previous research from a large US real-world registry has shown that patients with multiple active PsA domains had, on average, worse overall health status and greater impairments in work productivity compared with those with a single active PsA domain [32,33,34,35]. A more recent analysis demonstrated that the presence of enthesitis, dactylitis, and peripheral joint involvement was associated with poorer overall health status and greater impairments in work productivity [36]. Additionally, a higher body surface area affected by psoriasis was associated with work productivity impairment [36]. In previous analyses assessing the relationships between PsA disease characteristics and WPAI domains at baseline in DISCOVER-2, higher CRP level and greater patient-reported fatigue and pain were positively associated with the degree of impairment assessed by each of the four WPAI domains [19]. Additionally, more extensive skin disease (as assessed by the Psoriasis Area and Severity Index [PASI]) and the presence of enthesitis were associated with presenteeism, work productivity loss, and nonwork daily activity impairment; the presence of dactylitis was associated with presenteeism; and tender joint count was positively associated with nonwork daily activity impairment. Through 2 years of DISCOVER-2, 62–70% of patients treated with guselkumab achieved enthesitis resolution, 72–83% achieved dactylitis resolution, and 53–59% achieved clear skin [18]. Furthermore, approximately 40% of patients who received guselkumab achieved minimal disease activity [18], indicating high levels of response across several PsA domains. Although reasons for changes related to work productivity/nonwork daily activity and employment status were not captured in DISCOVER-2, sustained improvements across PsA domains may have contributed to the improvements related to productivity and employment reported here in patients treated with guselkumab.
Substantial improvements in absenteeism were not observed in any of the treatment groups at any time point through 2 years in the current analyses. In part, this may reflect the minority (< 12%) of DISCOVER-2 patients reporting work time missed due to PsA (absenteeism) at baseline [19], which is consistent with prior reports [23, 37]. These findings, which illustrate that patients with PsA may come to work despite having substantially more productivity impairments at work than recognized by simply assessing absenteeism, are supported by the high proportion (approx. 94%) of patients who were actively employed at baseline and reported work impairment.
Limitations of this study include: enrollment of participants with moderately to highly active PsA who had not received prior biologic therapy, and slightly more than half of the study population was male; therefore, these results may not be generalizable to all patients. Additionally, most participants in DISCOVER-2 were White, limiting the applicability of these findings in patients of racial minority groups who are more likely to experience greater PsA disease burden, including ability to work [38]. In addition, the lack of requirements for minimal levels of impairment in work productivity/nonwork daily activity or general health status for inclusion in DISCOVER-2 may limit the ability to assess improvements in this study population, and information regarding specific job responsibilities and work environments was not captured in this study. Also, a patient’s decision to participate in a clinical study may be influenced by the type of job or the number of hours spent working each week. Relative to clinical efficacy results from DISCOVER-2, the placebo response was relatively high in the current analyses related to work productivity and employment. It should be noted that these outcomes may be influenced by many factors other than disease activity, such as age, macroeconomics, and lifestyle choice, as well as the type of employment and the country and context in which a patient’s work is performed. It is unknown whether patients who were not working did so specifically because of their PsA; although we note that this would mitigate against the size of effect observed. Of note, this study was ongoing at the beginning of the COVID-19 pandemic, which may have affected work productivity and employment-related assessments for some patients (4 participants did not complete study procedures due to the pandemic). Although clinically meaningful improvements for WPAI-PsA have been validated [23], improvements greater than the MID values for the EQ-5D-5L and EQ-VAS [28] have not been confirmed as clinically meaningful. These instruments are also limited by the lack of inclusion of key factors that may influence HRQoL in the EQ-5D-5L [39] (e.g., fatigue and pain) and potential ambiguity in how respondents interpret the EQ-VAS labels [40].
Conclusions
DISCOVER-2 was a relatively large phase 3 study with strong patient retention through 2 years, which allowed for a robust dataset for long-term (up to 2 years) follow-up. Among patients with active PsA who were biologic-naïve, these post hoc analyses demonstrated that both guselkumab dosing regimens led to meaningful improvements in work productivity, nonwork daily activity impairment, and general health status, and these outcomes were sustained through 2 years. Furthermore, rates of employment increased in patients treated with guselkumab who were not employed at baseline and observed improvements in work productivity were estimated to result in substantial yearly indirect work productivity-related cost savings.
Data Availability
The data sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinical-trials/transparency. As noted on this site, requests for access to the trial data can be submitted through Yale Open Data Access (YODA) Project site at http://yoda.yale.edu.
References
Mease PJ, Gladman DD, Papp KA, et al. Prevalence of rheumatologist-diagnosed psoriatic arthritis in patients with psoriasis in European/North American dermatology clinics. J Am Acad Dermatol. 2013;69:729–35.
Ritchlin CT, Colbert RA, Gladman DD. Psoriatic arthritis. N Engl J Med. 2017;376:957–70.
Lee S, Mendelsohn A, Sarnes E. The burden of psoriatic arthritis: a literature review from a global health systems perspective. P T. 2010;35:680–9.
Kerschbaumer A, Baker D, Smolen JS, Aletaha D. The effects of structural damage on functional disability in psoriatic arthritis. Ann Rheum Dis. 2017;76:2038–45.
Husni ME, Merola JF, Davin S. The psychosocial burden of psoriatic arthritis. Semin Arthritis Rheum. 2017;47:351–60.
Tillett W, de Vries C, McHugh NJ. Work disability in psoriatic arthritis: a systematic review. Rheumatology (Oxford). 2012;51:275–83.
Bojke L, Spackman E, Hinde S, Helliwell P. Capturing all of the costs in NICE appraisals: the impact of inflammatory rheumatic diseases on productivity. Rheumatology (Oxford). 2012;51:210–5.
Tillett W, Shaddick G, Askari A, et al. Factors influencing work disability in psoriatic arthritis: first results from a large UK multicentre study. Rheumatology (Oxford). 2015;54:157–62.
Orbai AM, Reddy SM, Dennis N, et al. Work absenteeism and disability associated with psoriasis and psoriatic arthritis in the USA—a retrospective study of claims data from 2009 to 2020. Clin Rheumatol. 2021;40:4933–42.
Rosen CF, Mussani F, Chandran V, Eder L, Thavaneswaran A, Gladman DD. Patients with psoriatic arthritis have worse quality of life than those with psoriasis alone. Rheumatology (Oxford). 2012;51:571–6.
Janssen Biotech, Inc. Tremfya (guselkumab). Package insert. 2020. https://www.janssenlabels.com/package-insert/product-monograph/prescribing-information/TREMFYA-pi.pdf. Accessed 21 Dec 2023.
Boehncke W-H, Brembilla NC, Nissen MJ. Guselkumab: the first selective IL-23 inhibitor for active psoriatic arthritis in adults. Expert Rev Clin Immunol. 2021;17:5–13.
Deodhar A, Helliwell PS, Boehncke W-H, et al. Guselkumab in patients with active psoriatic arthritis who were biologic-naïve or had previously received TNFα inhibitor treatment (DISCOVER-1): a double-blind, randomised, placebo-controlled phase 3 trial. Lancet. 2020;395:1115–25.
Mease PJ, Rahman P, Gottlieb AB, et al. Guselkumab in biologic-naïve patients with active psoriatic arthritis (DISCOVER-2): a double-blind, randomised, placebo-controlled phase 3 trial. Lancet. 2020;395:1126–36.
Coates LC, Ritchlin CT, Gossec L, et al. Guselkumab provides sustained domain-specific and comprehensive efficacy using composite indices in patients with active psoriatic arthritis. Rheumatology (Oxford). 2023;62:606–16.
Ritchlin CT, Helliwell PS, Boehncke W-H, et al. Guselkumab, an inhibitor of the IL-23p19 subunit, provides sustained improvement in signs and symptoms of active psoriatic arthritis: 1 year results of a phase III randomised study of patients who were biologic-naïve or TNFα inhibitor-experienced. RMD Open. 2021;7: e001457.
McInnes IB, Rahman P, Gottlieb AB, et al. Efficacy and safety of guselkumab, an interleukin-23p19-specific monoclonal antibody, through one year in biologic-naïve patients with psoriatic arthritis. Arthritis Rheumatol. 2021;73:604–16.
McInnes IB, Rahman P, Gottlieb AB, et al. Long-term efficacy and safety of guselkumab, a monoclonal antibody specific to the p19 subunit of interleukin-23, through two years: results from a phase III, randomized, double-blind, placebo-controlled study conducted in biologic-naïve patients with active psoriatic arthritis. Arthritis Rheumatol. 2022;74:475–85.
Curtis JR, McInnes IB, Rahman P, et al. The effect of guselkumab on work productivity in biologic-naïve patients with active psoriatic arthritis through week 52 of the phase 3, randomized, placebo-controlled DISCOVER-2 trial. Adv Ther. 2022;39:4613–31.
Curtis JR, McInnes IB, Rahman P, et al. The effect of guselkumab on general health state in biologic-naïve patients with active psoriatic arthritis through week 52 of the phase 3, randomized, placebo-controlled DISCOVER-2 trial. Adv Ther. 2022;39:4632–44.
Taylor W, Gladman DD, Helliwell P, et al. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum. 2006;54:2665–73.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–65.
Tillett W, Lin C-Y, Zbrozek A, Trevelin Sprabery A, Birt J. A threshold of meaning for work disability improvement in psoriatic arthritis measured by the work productivity and activity impairment questionnaire. Rheumatol Ther. 2019;6:379–91.
Organization for Economic Co-operation and Development (OECD). Average wages (indicator). 2020. https://data.oecd.org/earnwage/average-wages.htm. Accessed 18 Nov 2021.
The EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
van Hout B, Janssen MF, Feng YS, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15:708–15.
Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care. 2005;43:203–20.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–92.
Janssen MF, Szende A, Cabases J, Ramos-Goñi JM, Vilagut G, König HH. Population norms for the EQ-5D-3L: a cross-country analysis of population surveys for 20 countries. Eur J Health Econ. 2019;20:205–16.
Kawalec P, Malinowski KP. The indirect costs of psoriatic arthritis: systematic review and meta-analysis. Expert Rev Pharmacoecon Outcomes Res. 2015;15:125–32.
Coates LC, Soriano ER, Corp N, et al. Group for research and assessment of psoriasis and psoriatic arthritis (GRAPPA): updated treatment recommendations for psoriatic arthritis 2021. Nat Rev Rheumatol. 2022;18:465–79.
Ogdie A, Hur P, Liu M, et al. Effect of multidomain disease presentations on patients with psoriatic arthritis in the Corrona Psoriatic Arthritis/Spondyloarthritis Registry. J Rheumatol. 2021;48:698–706.
Mease PJ, Karki C, Palmer JB, et al. Clinical characteristics, disease activity, and patient-reported outcomes in psoriatic arthritis patients with dactylitis or enthesitis: results from the Corrona Psoriatic Arthritis/Spondyloarthritis Registry. Arthritis Care Res (Hoboken). 2017;69:1692–9.
Mease PJ, Palmer JB, Liu M, et al. Influence of axial involvement on clinical characteristics of psoriatic arthritis: analysis from the Corrona Psoriatic Arthritis/Spondyloarthritis Registry. J Rheumatol. 2018;45:1389–96.
Mease PJ, Liu M, Rebello S, et al. Disease characteristics, quality of life, and work productivity by enthesitis site: real-world data from the US Corrona Psoriatic Arthritis/Spondyloarthritis Registry. J Rheumatol. 2021;48:367–75.
Walsh JA, Ogdie A, Michaud K, et al. Impact of key manifestations of psoriatic arthritis on patient quality of life, functional status, and work productivity: findings from a real-world study in the United States and Europe. Joint Bone Spine. 2023;90: 105534.
Tillett W, Lin C-Y, Trevelin Sprabery A, Birt JA, Kavanaugh A. Clinically meaningful improvement in work productivity loss in active psoriatic arthritis: post-hoc analysis of SPIRIT-P1 and SPIRIT-P2 trials. Clin Exp Rheumatol. 2020;38:1227–30.
Navarro-Millán I, Kerr G, Carter J, Simone L, Nelson M. Racial/ethnic differences in psoriatic arthritis patient responses regarding disease burden, treatment, and communication with care team [abstract]. Arthritis Rheumatol. 2023;75(suppl 9). https://acrabstracts.org/abstract/racial-ethnic-differences-in-psoriatic-arthritis-patient-responses-regarding-disease-burden-treatment-and-communication-with-care-team/. Accessed 6 Dec 2023.
Efthymiadou O, Mossman J, Kanavos P. Health related quality of life aspects not captured by EQ-5D-5L: Results from an international survey of patients. Health Policy. 2019;123:159–65.
Feng Y, Parkin D, Devlin NJ. Assessing the performance of the EQ-VAS in the NHS PROMs programme. Qual Life Res. 2014;23:977–89.
Acknowledgements
Medical Writing, Editorial, and Other Assistance.
Medical writing support was provided by Teresa Tartaglione, PharmD, of Certara Synchrogenix (funded by Janssen Scientific Affairs, LLC) and Rebecca Clemente, PhD, of Janssen Scientific Affairs, LLC, under the direction of the authors in accordance with Good Publication Practice guidelines (Ann Intern Med. 2022; https://doi.org/10.7326/M22-1460). The authors thank Cynthia Guzzo, MD (consultant funded by Janssen Scientific Affairs, LLC) for substantive manuscript review.
Authorship.
Authors who were employees of the sponsor were involved in designing the study and collecting and analyzing the data. All authors revised the manuscript for important intellectual content and approved the manuscript for submission.
Funding
The DISCOVER-2 study and the journal’s Rapid Service Fee were supported by Janssen Research & Development, LLC, Spring House, PA, USA. Medical writing support for the manuscript was funded by Janssen Scientific Affairs, LLC, Horsham, PA, USA.
Author information
Authors and Affiliations
Contributions
Study concept and design: Jeffrey R. Curtis, Iain B. McInnes, Proton Rahman, Dafna D. Gladman, Steven Peterson, Alexa P. Kollmeier, Chenglong Han, May Shawi, William Tillett, Philip J. Mease. Acquisition of data: Steven Peterson, Feifei Yang, Alexa P. Kollmeier. Statistical analysis: Feifei Yang. Interpretation, revision, approval: Jeffrey R. Curtis, Iain B. McInnes, Proton Rahman, Dafna D. Gladman, Steven Peterson, Feifei Yang, Oluwakayode Adejoro, Alexa P. Kollmeier, Natalie J. Shiff, Chenglong Han, May Shawi, William Tillett, Philip J. Mease.
Corresponding author
Ethics declarations
Conflict of Interest
Jeffrey R. Curtis received grant/research support from AbbVie, Amgen, Bristol Myers Squibb, CorEvitas, Eli Lilly, Janssen, Myriad, Novartis, Pfizer, Sanofi, and UCB; and consulting fees from AbbVie, Amgen, Bristol Myers Squibb, CorEvitas, Eli Lilly, Janssen, Myriad, Novartis, Pfizer, Sanofi, and UCB. Iain B. McInnes received consultant fees from AbbVie, Amgen, Astra Zeneca, Bristol Myers Squibb, Cabaletta, Compugen, Eli Lilly, Gilead, Glaxo Smith Kline, Janssen, Novartis, Pfizer, Roche, Sanofi, and UCB; grant/research support from Amgen, Astra Zeneca, Bristol Myers Squibb, Eli Lilly, Glaxo Smith Kline, Janssen, Novartis, Roche, and UCB; and is a shareholder for Causeway Therapeutics and Evelo Compugen. Proton Rahman received consulting fees from AbbVie, Amgen, Bristol Myers Squibb, Celgene, Eli Lilly, Janssen, Merck, Novartis, Pfizer, and UCB; meeting attendance/travel support from Janssen; and research grants from Janssen and Novartis. Dafna D. Gladman received grant support from AbbVie, Amgen, Bristol Myers Squibb, Celgene, Eli Lilly, Janssen, Novartis, Pfizer, and UCB; and consulting fees from AbbVie, Amgen, Bristol Myers Squibb, Celgene, Eli Lilly, Galapagos, Gilead, Janssen, Novartis, Pfizer, and UCB. Steven Peterson, Oluwakayode Adejoro, and Chenglong Han are employees of Janssen Global Services, LLC, and own stock in Johnson & Johnson. Feifei Yang was an employee of Janssen Global Services, LLC, at the time this work was performed, and owns stock in Johnson & Johnson. Alexa P. Kollmeier and May Shawi are an employees of Janssen Research & Development, LLC, and own stock in Johnson & Johnson. Natalie J. Shiff is an employee of Janssen Scientific Affairs, LLC, and owns stock in AbbVie, Gilead, Iovance, Jazz Pharmaceuticals, Johnson & Johnson, Novavax, and Viatris. William Tillett received consultant fees from AbbVie, Amgen, Eli Lilly, Janssen, Merck Sharp & Dohme, Novartis, Ono-Pharma, Pfizer, and UCB; grant/research support from AbbVie, Amgen, Eli Lilly, Janssen, Pfizer, and UCB; and speaker fees from AbbVie, Amgen, Eli Lilly, Janssen, Merck, Novartis, Pfizer, and UCB. Philip J. Mease has received research grants from AbbVie, Acelyrin, Amgen, Bristol Myers Squibb, Eli Lilly, Janssen, Novartis, Pfizer, SUN Pharma, and UCB; consulting fees from AbbVie, Acelyrin, Aclaris, Amgen, Boehringer Ingelheim, Bristol Myers Squibb, Eli Lilly, Galapagos, Gilead, GlaxoSmithKline, Immagene, Janssen, Moonlake Pharma, Novartis, Pfizer, SUN Pharma, UCB, Ventyx, and Xinthera; and speaker fees from AbbVie, Amgen, Eli Lilly, Janssen, Novartis, Pfizer, and UCB.
Ethical Approval
This study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines. All patients provided written informed consent, and the protocol was approved by local institutional review boards or ethics committees at each site (for several United States sites, Sterling Institutional Review Board approval number: 5910C) (Supplementary Materials Table S1). All patients provided written informed consent.
Additional information
Prior Presentation: These data have been presented in part at ACR Convergence, November 10–14, 2022 in Philadelphia, PA. Arthritis Rheumatol. 2022; 74 (suppl 9).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Curtis, J.R., McInnes, I.B., Rahman, P. et al. Work Productivity and General Health Through 2 Years of Guselkumab Treatment in a Phase 3 Randomized Trial of Patients With Active Psoriatic Arthritis. Rheumatol Ther 11, 425–441 (2024). https://doi.org/10.1007/s40744-024-00642-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-024-00642-9