Abstract
Introduction
This article aims to describe malignancies in patients with rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), or non-radiographic axial spondyloarthritis (nr-axSpA) treated with upadacitinib (UPA) or active comparators.
Methods
This integrated safety analysis includes data from 11 phase 3 UPA trials across RA (6 trials), PsA (2 trials), AS (2 trials; one phase 2b/3), and nr-axSpA (1 trial). Treatment-emergent adverse events (TEAEs) were summarized for RA (pooled UPA 15 mg [UPA15], pooled UPA 30 mg [UPA30], adalimumab 40 mg [ADA], methotrexate monotherapy [MTX]), PsA (pooled UPA15, pooled UPA30, ADA), AS (pooled UPA15), and nr-axSpA (UPA15). TEAEs were reported as exposure-adjusted event rates (events/100 patient-years).
Results
Median treatment duration ranged from 1.0 to 4.0 years (with a maximum of 6.6 years in RA). Across treatments and indications, rates of malignancy excluding nonmelanoma skin cancer (NMSC) ranged from 0.2 to 1.1, while NMSC ranged from 0.0 to 1.4. In RA, rates of malignancy excluding NMSC were generally similar between UPA15, UPA30, ADA, and MTX (breast and lung cancer were the most common). In RA and PsA, Kaplan–Meier analyses revealed no differences in event onset of malignancy excluding NMSC with UPA15 versus UPA30 over time. In RA, NMSC rates were higher with UPA30 than UPA15; both UPA15 and UPA30 were higher than ADA and MTX. In PsA, rates of malignancy excluding NMSC and NMSC were generally similar between UPA15, UPA30, and ADA. In AS and nr-axSpA, malignancies were reported infrequently. Few events of lymphoma were reported across the clinical programs.
Conclusion
Rates of malignancy excluding NMSC were generally similar between UPA15, UPA30, ADA, and MTX and were consistent across RA, PsA, AS, and nr-axSpA. A dose-dependent increased rate of NMSC was observed with UPA in RA.
Trial Registration
ClinicaTrials.gov identifier: NCT02706873, NCT02675426, NCT02629159, NCT02706951, NCT02706847, NCT03086343, NCT03104400, NCT03104374, NCT03178487, and NCT04169373.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
As a result of the safety concerns raised in ORAL Surveillance, a post-authorization safety study with the Janus kinase (JAK) inhibitor tofacitinib, further characterization of the safety profile of JAK inhibitors is needed across the rheumatic diseases and in the context of active comparators to help clinicians and patients make informed treatment decisions. |
The objective of this integrated safety analysis is to describe events of malignancy in patients with rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), or non-radiographic axial spondyloarthritis (nr-axSpA) treated with the JAK inhibitor upadacitinib from the SELECT clinical trials in the context of active comparators adalimumab (RA and PsA) and methotrexate (RA). |
What was learned from the study? |
Event rates of malignancy excluding nonmelanoma skin cancer (NMSC) were generally similar between upadacitinib 15 mg (the approved dose for RA, PsA, AS, and nr-axSpA), upadacitinib 30 mg, adalimumab, and methotrexate, and were consistent across RA, PsA, AS, and nr-axSpA. |
In RA, there was a dose-dependent increase in NMSC, with rates being higher with upadacitinib 30 mg treatment than upadacitinib 15 mg; rates of NMSC were higher with both upadacitinib doses versus adalimumab and methotrexate. |
This analysis provides important safety information on malignancies with upadacitinib treatment across RA, PsA, AS, and nr-axSpA, which can help inform treatment decisions to improve patient care. |
Introduction
Rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), and non-radiographic axial spondyloarthritis (nr-axSpA) are chronic immune-mediated inflammatory diseases. An increased risk of malignancy has been associated with chronic inflammation, as well as with the use of immunosuppressive and immunomodulatory therapies [2,3,4,5,6]. It is well established that patients with RA have an increased risk of malignancies compared to the general population [3, 7], while the risk of malignancies in patients with PsA [8,9,10], AS [10, 11], or nr-axSpA is not as clear.
Data from ORAL Surveillance, a post-authorization safety study, demonstrated an increased risk of malignancy and major adverse cardiovascular events (MACE) in patients with RA ≥ 50 years of age with at least one additional cardiovascular risk factor treated with tofacitinib (a Janus kinase [JAK] inhibitor targeting JAK1, JAK2, and JAK3 subtypes over tyrosine kinase 2 [TYK2]) versus tumor necrosis factor (TNF) inhibitors [12, 13]. As a result of the safety concerns raised in ORAL Surveillance, further characterization of the safety profile of JAK inhibitors is needed across the rheumatic diseases and in the context of active comparators to help clinicians and patients make informed treatment decisions.
Upadacitinib is an oral JAK inhibitor engineered for greater selectivity for JAK1 versus JAK2, JAK3, and TYK2, with demonstrated efficacy across many inflammatory diseases, including RA [14,15,16,17,18,19], PsA [20, 21], AS [22, 23], and nr-axSpA [24]. For this integrated safety analysis, our objective is to describe events of malignancy in patients with RA, PsA, AS, or nr-axSpA treated with upadacitinib from the SELECT clinical trials in the context of active comparators adalimumab (RA and PsA) and methotrexate (RA).
Methods
Patients and Studies
This integrated safety analysis includes data (cutoff 15 Aug 2022) from 11 phase 3 upadacitinib trials in adults (≥ 18 years of age) across RA (6 trials), PsA (2 trials), AS (2 trials; one phase 2b/3), and nr-axSpA (1 trial) from the SELECT clinical program. Patients with a history of any malignancy, except for successfully treated nonmelanoma skin cancer (NMSC) or localized carcinoma in situ of the cervix, were excluded from participating in these studies. Methodological details for the SELECT clinical trials in RA [14,15,16,17,18,19], PsA [20, 21], AS [22, 23], and nr-axSpA [24] have been published previously. A brief overview of each trial is provided in the Supplementary Material (Supplementary Tables 1 and 2).
All studies were conducted in accordance with the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) guidelines, applicable regulations governing clinical trial conduct, and the Declaration of Helsinki 1964 and its later amendments. The trial protocols were approved by an independent ethics committee (IEC)/institutional review board (IRB) at each study site per Good Clinical Practice (GCP). All patients provided written informed consent prior to screening.
Treatments
Patients were treated with upadacitinib 15 mg (approved dose) once daily in the RA, PsA, AS, and nr-axSpA studies, and upadacitinib 30 mg once daily in the RA and PsA studies. Active comparators for this analysis included methotrexate monotherapy in RA (up to 5 years from the SELECT-EARLY study) and adalimumab 40 mg every other week in RA (up to 7 years from the SELECT-COMPARE study) and PsA (up to 5 years from the SELECT-PsA 1 study). Within each trial, patients initially randomized to placebo were switched to upadacitinib treatment at the end of the double-blind placebo-controlled period. Since upadacitinib 15 mg is the approved dose for RA and PsA, patients on upadacitinib 30 mg were switched to upadacitinib 15 mg in the ongoing studies. An overview of each clinical trial is provided in Supplementary Tables 1 and 2.
Safety Assessments
Treatment-emergent adverse events (TEAEs) of malignancy were defined as an adverse event (AE) with onset on or after the first dose and ≤ 30 days after the last dose of upadacitinib 15 mg, upadacitinib 30 mg, or methotrexate, or ≤ 70 days after the last dose of adalimumab. AEs were coded using the Medical Dictionary for Regulatory Activities (MedDRA). Malignancy data were retrieved using the standardized MedDRA Query (SMQ) or company MedDRA Query (CMQ) search criteria. All malignancy events, with corresponding information from the treating clinician, were reviewed by safety physicians employed by the sponsor but were not formally adjudicated by an independent committee. Study protocols required that patients developing a malignancy other than localized NMSC or carcinoma in situ of the cervix discontinue from study drug. For this analysis, TEAEs are summarized for RA (pooled upadacitinib 15 mg, pooled upadacitinib 30 mg, adalimumab [SELECT-COMPARE study only], and methotrexate [SELECT-EARLY study only]), PsA (pooled upadacitinib 15 mg, pooled upadacitinib 30 mg, and adalimumab [SELECT-PsA 1 study only]), AS (pooled upadacitinib 15 mg), and nr-axSpA (upadacitinib 15 mg). In the RA program, four of the six studies evaluated both doses of upadacitinib (15 mg and 30 mg); additional sub-analyses comparing upadacitinib 15 mg versus upadacitinib 30 mg were conducted with pooled data from only these four studies.
Statistical Analysis
In this post hoc analysis, TEAE data are reported as exposure-adjusted adverse event rates (EAERs; events/100 patient-years [E/100 PY]), or as exposure-adjusted incidence rates (EAIRs; n/100 PY) in the Supplementary Material, with 95% confidence intervals (CIs) calculated using the exact method for the Poisson mean. For EAERs, exposure time was calculated as the total study drug duration for all events, including multiple events in a single patient, which are shown in the numerator. For EAIRs, exposure time was calculated as the time to the first event in patients who experienced an event; any patient experiencing one or more events was counted once in the numerator. In patients who did not experience an event, exposure time was censored on the day of the patient’s last known assessment or the cutoff date of database lock, whichever occurred first. The age-gender adjusted standard incidence ratio (SIR) was calculated for RA, as there was a sufficient number of events, using the Surveillance, Epidemiology, and End Results (SEER) database for the general population. The SIR was not calculated for PsA, AS, or nr-axSpA because of the low number of malignancy events. Times to first event of malignancy excluding NMSC or NMSC with upadacitinib 15 mg and upadacitinib 30 mg treatment were estimated using Kaplan–Meier analysis for RA (studies with both upadacitinib doses) and PsA. Hazard ratios were generated using univariable Cox proportion hazards regression models for time from first dose of upadacitinib 15 mg to the first events of malignancy excluding NMSC or NMSC to assess the impact of known risk factors on malignancy rates in RA and PsA. Multivariable analysis was not possible because of low numbers of malignancy events. Kaplan–Meier analyses and univariable regression models were not generated for lymphoma in RA or PsA, or for malignancy excluding NMSC, NMSC, or lymphoma in AS or nr-axSpA, because of the low number or absence of malignancy events reported.
Results
Patients and Exposure
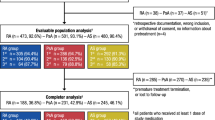
Across RA (N = 5306), PsA (N = 2257), AS (N = 596), and nr-axSpA (N = 286), a total of 4998 patients (14,472.1 PY) received at least one dose of upadacitinib 15 mg, 2125 patients (5110.8 PY) received at least one dose of upadacitinib 30 mg, 1008 patients (2719.6 PY) received at least one dose of adalimumab, and 314 patients (865.1 PY) received at least one dose of methotrexate. In RA, the median treatment duration was 4.0 years (range 1 day–6.6 years) for upadacitinib 15 mg, 3.2 years (range 1 day–5.1 years) for upadacitinib 30 mg, 2.2 years (range 1 day–6.6 years) for adalimumab, and 2.6 years (range 1 day–5.4 years) for methotrexate. In PsA, the median treatment duration was 2.9 years (range 1 day–5.0 years) for upadacitinib 15 mg, 2.4 years (range 1 day–4.3 years) for upadacitinib 30 mg, and 3.1 years (range 1 day–4.8 years) for adalimumab. In AS, the median treatment duration was 1.7 years (range 1 day–3.8 years) for upadacitinib 15 mg. For the nr-axSpA study, the median treatment duration was 1.0 years (range 1 day–2.2 years) for upadacitinib 15 mg.
Baseline demographic data stratified by occurrence of malignancy during the studies (no malignancy, malignancy excluding NMSC, or NMSC) for the RA, PsA, AS, and nr-axSpA patient populations are shown in Supplementary Material Table 3. Within each indication and treatment group, patients with an event of malignancy excluding NMSC or NMSC were slightly older and typically reported higher tobacco/nicotine use and alcohol use at baseline than patients with no malignancy event. Despite exclusion criteria, a small number of patients with previous malignancy were inadvertently enrolled in the studies across RA, PsA, AS, and nr-axSpA (as shown in Supplementary Material Table 3).
TEAEs of Malignancy
For all RA studies, EAERs (E/100 PY [95% CI]) of malignancy excluding NMSC were generally similar between upadacitinib 15 mg (0.8 [0.6, 0.9]), upadacitinib 30 mg (1.1 [0.8, 1.6]), adalimumab (0.8 [0.4, 1.3]), and methotrexate (0.9 [0.4, 1.8]) (Fig. 1a). The age-gender adjusted SIR (95% CI) for malignancy excluding NMSC was 0.98 (0.79, 1.20) in patients treated with upadacitinib 15 mg and 1.18 (0.88, 1.55) in patients treated with upadacitinib 30 mg. The most common types of malignancy excluding NMSC in RA were lung cancer and breast cancer (Table 1). No events of breast cancer were reported in men. Across all treatments in RA, 94.4% (17 of 18 events) of lung cancer events were reported in current or former smokers. Lymphoma was infrequent in RA (upadacitinib 15 mg: < 0.1 [0.0, 0.1]; upadacitinib 30 mg: < 0.1 [0.0, 0.2]; adalimumab: 0.2 [0.0, 0.6]; methotrexate: 0.0 [0.0, 0.4]) (Fig. 1a). One case of suspected lymphoma in a patient treated with upadacitinib 15 mg was of abnormal lymphocyte morphology which became normal in subsequent testing. Rates of NMSC were numerically higher with upadacitinib 30 mg (1.4 [1.0, 1.8]) than upadacitinib 15 mg (0.5 [0.4, 0.6]) and were higher with both doses of upadacitinib compared to adalimumab (0.1 [0.0, 0.5]) or methotrexate (0.0 [0.0, 0.4]). The most common types of NMSC were cutaneous squamous cell carcinoma and basal cell carcinoma, which occurred at similar rates (Table 1). Similar findings as above for rates of malignancy excluding NMSC (upadacitinib 15 mg: 0.9 [0.6, 1.2]; upadacitinib 30 mg: 1.1 [0.8, 1.6]), lymphoma (upadacitinib 15 mg: < 0.1 [0.0, 0.2]; upadacitinib 30 mg: < 0.1 [0.0, 0.2]), and NMSC (upadacitinib 15 mg: 0.5 [0.3, 0.8]; upadacitinib 30 mg: 1.4 [1.0, 1.8]) were observed when RA studies including both doses of upadacitinib were evaluated (Fig. 1b), and in the SELECT-COMPARE study, where upadacitinib 15 mg (malignancy excluding NMSC: 0.6 [0.4, 0.8]; lymphoma: 0.0 [0.0, 0.1]; NMSC: 0.5 [0.3, 0.7]) and adalimumab (malignancy excluding NMSC: 0.8 [0.4, 1.3]; lymphoma 0.2 [0.0, 0.6]; NMSC: 0.1 [0.0, 0.5]) were directly compared (Fig. 1c).
Event rates per 100 patient-years for TEAEs of malignancy in patients treated with UPA across RA (a–c), PsA (d, e), AS (f), and nr-axSpA (g). †Cases of abnormal lymphocyte morphology are included (upadacitinib 15 mg: RA [1], PsA [3], AS [1], and nr-axSpA [1]), as this preferred term is included in the Malignant Lymphoma Standardized MedDRA Queries but were not confirmed to be true lymphomas. ADA adalimumab, AS ankylosing spondylitis, CI confidence interval, E event, EAER exposure-adjusted event rate, EOW every other week, MTX methotrexate, NMSC nonmelanoma skin cancer, nr-axSpA non-radiographic axial spondyloarthritis, PsA psoriatic arthritis, PY patient-years, QD once daily, RA rheumatoid arthritis, TEAE treatment-emergent adverse events, UPA upadacitinib
In PsA, rates of malignancy excluding NMSC were generally similar between upadacitinib 15 mg (0.7 [0.4, 1.1]), upadacitinib 30 mg (0.8 [0.5, 1.3]), and adalimumab (0.4 [0.1, 1.0]). The most common types of malignancy excluding NMSC were colorectal cancer and melanoma (Table 1). Three events of suspected lymphoma were reported in PsA (0.1 [0.0, 0.4]) with upadacitinib 15 mg treatment; however, all three cases were of abnormal lymphocyte morphology and were not confirmed to be true lymphomas (lymphocyte morphology returned to normal in subsequent testing) (Fig. 1d). Rates of NMSC were similar between upadacitinib 15 mg (0.9 [0.6, 1.4]) and upadacitinib 30 mg (0.8 [0.5, 1.3]), but were numerically lower with adalimumab (0.2 [0.0, 0.6]) (Fig. 1d). The most common type of NMSC was basal cell carcinoma (Table 1). Similar findings as above for rates of malignancy excluding NMSC, lymphoma, and NMSC were observed in the SELECT-PsA 1 study, where upadacitinib 15 mg (0.6 [0.3, 1.0], < 0.1 [0.0, 0.3], and 0.8 [0.4, 1.3], respectively), upadacitinib 30 mg (0.7 [0.3, 1.3], 0.0 [0.0, 0.3], and 0.6 [0.3, 1.2], respectively), and adalimumab (0.4 [0.1, 1.0], 0.0 [0.0, 0.3], and 0.2 [0.0, 0.6], respectively) were directly compared (Fig. 1e). Across both AS studies, two events each of malignancy excluding NMSC and NMSC (both 0.2 [0.0, 0.8]) were reported with upadacitinib 15 mg (Fig. 1f). In the nr-axSpA study, one event each of malignancy excluding NMSC and NMSC (both 0.3 [0.0, 1.7]) were reported (Fig. 1g). One event each of abnormal lymphocyte morphology (classified under lymphoma) was reported in the AS (0.1 [0.0, 0.6]) and nr-axSpA (0.3 [0.0, 1.7]) studies and were not confirmed to be true lymphomas (morphology returned to normal in subsequent testing). TEAEs of malignancy, as well as details about the types of malignancy observed, are presented as EAIRs in Supplementary Material Tables 4 and 5, respectively.
Timing of Malignancy Events
When TEAEs were stratified by length of exposure to upadacitinib, 0 to ≤ 12 months or > 12 months, no differences were observed in time to malignancy events in RA, PsA, AS, or nr-axSpA (Fig. 2). TEAEs stratified by length of exposure to upadacitinib as EAIRs are presented in Supplementary Material Table 6. In RA studies with both upadacitinib doses evaluated, Kaplan–Meier analysis revealed no clear pattern in timing of event onset of malignancy excluding NMSC (Supplementary Material Fig. 1A) or NMSC (Supplementary Material Fig. 2A) in patients treated with upadacitinib 15 mg or upadacitinib 30 mg up to 60 months. Similarly, in PsA, no patterns in timing of event onset of malignancy excluding NMSC (Supplementary Material Fig. 1B) or NMSC (Supplementary Material Fig. 2B) were observed with upadacitinib 15 mg or upadacitinib 30 mg up to 42 months.
Event rates per 100 patient-years for TEAEs of malignancy in RA (a), PsA (b), AS (c), and nr-axSpA (d) by length of UPA exposure. †Cases of abnormal lymphocyte morphology are included (upadacitinib 15 mg: RA [1], PsA [3], AS [1], and nr-axSpA [1]), as this preferred term is included in the Malignant Lymphoma Standardized MedDRA Queries but were not confirmed to be true lymphomas. ADA adalimumab, AS ankylosing spondylitis, CI confidence interval, E event, EAER exposure-adjusted event rate, EOW every other week, MTX methotrexate, NMSC nonmelanoma skin cancer, nr-axSpA non-radiographic axial spondyloarthritis, PsA psoriatic arthritis, PY patient-years, QD once daily, RA rheumatoid arthritis, TEAE treatment-emergent adverse events, UPA upadacitinib
Risk Factors for Malignancy Events
In the univariable regression model for all RA studies, being older (≥ 65 years of age), being male, consuming alcohol, and residing in the USA (compared to Europe and/or outside the USA) were associated with an increased risk of malignancy excluding NMSC in patients treated with upadacitinib 15 mg (Fig. 3a). In PsA, being older and male were associated with an increased risk of malignancy excluding NMSC with upadacitinib 15 mg treatment (Fig. 3b). Similarly, factors associated with an increased risk of NMSC in patients with RA treated with upadacitinib 15 mg included being older, male, and residing in the USA (Fig. 4a). In PsA, being older, having a higher body mass index (BMI; particularly ≥ 30 kg/m2), and residing in the USA were associated with an increased risk of NMSC in patients treated with upadacitinib 15 mg (Fig. 4b).
Risk factors for malignancy excluding NMSC in RA (a) and PsA (b) with UPA 15 mg. Hazard ratios were generated using univariable Cox proportional hazards regression models for time from first dose of UPA 15 mg to first event of malignancy excluding NMSC in RA and PsA. *P < 0.05; **P < 0.01; ***P < 0.001. BMI body mass index, CI confidence interval, CRP C-reactive protein, HR hazard ratio, NE not estimable (due to zero events), NMSC nonmelanoma skin cancer, PsA psoriatic arthritis, QD once daily, RA rheumatoid arthritis, ULN upper limit of normal, UPA upadacitinib
Risk factors for NMSC in RA (a) and PsA (b) with UPA 15 mg. Hazard ratios were generated using univariable Cox proportional hazards regression models for time from first dose of UPA 15 mg to first event of NMSC in RA and PsA. *P < 0.05; **P < 0.01; ***P < 0.001. BMI body mass index, CI confidence interval, CRP C-reactive protein, HR hazard ratio, NE not estimable (due to zero events), NMSC nonmelanoma skin cancer, PsA psoriatic arthritis, QD once daily, RA rheumatoid arthritis, ULN upper limit of normal, UPA upadacitinib.
Discussion
A recent analysis of ORAL Surveillance data found an increased risk of both malignancy (excluding NMSC) and NMSC in at-risk patients with RA treated with the JAK inhibitor tofacitinib versus TNF inhibitors [13]. Although the risks of lung cancer and lymphoma are known to be higher in patients with RA compared to the general population [7], treatment with tofacitinib in patients of ≥ 50 years of age with at least one additional cardiovascular risk factor led to higher rates of lung cancer and lymphoma compared to treatment with TNF inhibitors. In contrast to the findings from ORAL Surveillance, published real-world data from the observational, cohort, claims-based STAR-RA study of tofacitinib versus TNF inhibitors [25], as well as data from the CorEvitas (formerly Corrona) real-world registry comparing tofacitinib and biological disease-modifying antirheumatic drugs (bDMARDs) [26], did not find an increased risk of malignancy with JAK inhibitor treatment in patients with RA. However, when similar inclusion criteria to ORAL Surveillance were applied (i.e., ≥ 50 years of age and at least one risk factor for cardiovascular disease), tofacitinib was associated with a numerically increased risk of malignancies [25]. An analysis by the ARTIS group of patients with RA or PsA in clinical practice found no evidence of an increased risk of malignancy excluding NMSC with JAK inhibitors (baricitinib and tofacitinib) compared to TNF inhibitors, while the risk of NMSC was elevated in patients receiving JAK inhibitor treatment [27]. A previous study on natural killer (NK) cells from 16 patients with RA treated with tofacitinib or baricitinib demonstrated altered phenotype and function ex vivo and in vitro, which may impact the NK cell-mediated antitumor response [28]. Given these mixed results, it is important to understand whether the findings from ORAL Surveillance can be generalized to other JAK inhibitors and other rheumatic diseases, as well as assess the safety of a JAK inhibitor versus a conventional synthetic disease-modifying antirheumatic drug (csDMARD) comparator (i.e., methotrexate in the RA SELECT-EARLY trial).
For this integrated safety analysis of upadacitinib across 11 phase 3 trials (1 AS phase 2b/3 study) in RA (5306 patients), PsA (2257 patients), AS (596 patients), and nr-axSpA (286 patients), nearly 20,000 total PYs of exposure data and up to a maximum of 6.6 years of treatment duration data for upadacitinib are described. In the integrated RA data, the overall rate of malignancy excluding NMSC was generally similar across upadacitinib 15 mg, upadacitinib 30 mg, adalimumab, and methotrexate. In the SELECT-COMPARE RA study, where both upadacitinib 15 mg (the approved dose) and adalimumab were evaluated, no increase in the rate of malignancy excluding NMSC was observed. Similarly, in a recent post hoc analysis of the SELECT-COMPARE study, the rate of malignancy excluding NMSC in at-risk patients with RA (≥ 50 years old with at least one cardiovascular risk factor) was generally similar between upadacitinib 15 mg and adalimumab [29]. Furthermore, the current analysis of PsA data also demonstrated similar results to that observed in RA, where the rates of malignancy excluding NMSC were generally similar between upadacitinib 15 mg or 30 mg and adalimumab.
As demonstrated previously [30], NMSC was reported more frequently with upadacitinib 30 mg versus upadacitinib 15 mg in RA, and rates were higher with both doses of upadacitinib than the active comparators adalimumab or methotrexate. While the rates of NMSC were also higher with upadacitinib compared to adalimumab in PsA, no meaningful dose relationship was observed for upadacitinib in the PsA studies. On the basis of the overall data, an increased risk of NMSC has been assessed to be causally related to upadacitinib therapy and has been added to the upadacitinib label; periodic skin examination is recommended for all patients, particularly in those with risk factors for skin cancer [31, 32]. Other JAK inhibitors, such as tofacitinib [33] and baricitinib [34], also report an increased risk of NMSC in their prescribing information.
The rates of basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (SCC) in the SELECT trials were largely similar within each treatment and indication. Published literature shows variability in the prevalence of these malignancies in the general population [35], which can be influenced by many factors including age, sex, and geographic region (i.e., latitude and subsequent sun exposure), as well as the methods used to calculate the incidence rate. Some publications support similar rates for both BCC and SCC [35, 36], as observed in this analysis, while others report a higher prevalence of BCC compared to SCC [37,38,39]. Of relevance to this study, immunosuppression has been linked to a greater incidence of NMSC, with reversal of the BCC to SCC ratio [40]. Additionally, patients who reported an adverse event of NMSC in the SELECT trials were older in age (range 50–66 years old), which has been associated with a more equal ratio of BCC to SCC compared to younger patients [36, 41].
Overall, no differences in the time to malignancy events were observed in RA, PsA, AS, or nr-axSpA. In addition, Kaplan–Meier analysis showed no clear pattern in the timing of event onset of malignancy excluding NMSC or NMSC between the two upadacitinib doses in RA or PsA. Univariable regression modeling revealed that being older and in the USA (compared to Europe and/or outside the USA) were common risk factors for malignancy excluding NMSC and NMSC in patients with RA or PsA treated with upadacitinib 15 mg. Additionally, being male (RA and PsA) and consuming alcohol (RA) were associated with an increased risk of malignancy excluding NMSC, while being male (RA) and having a higher BMI (PsA) were associated with an increased risk of NMSC in patients treated with upadacitinib 15 mg. ORAL Surveillance also found an increased risk of malignancy in patients with RA in North America (including the USA, Puerto Rico, and Canada), regardless of baseline atherosclerotic cardiovascular disease risk score, compared to the rest of the world [13]. A study of patients with PsA (age- and sex-matched to non-PsA comparators) also reported that higher age was a predisposing risk factor for malignancy, but opposite to our findings, being female was also identified as a risk factor [42]. In the general population, being older [43], being male [44], consuming alcohol [45], and having a higher BMI/obesity [45, 46] have been associated with an increased risk of cancer, which is consistent with the findings reported here for patients with RA or PsA treated with upadacitinib.
Limitations of this integrated safety analysis include the lack of a placebo control arm for comparative analysis, and the reduced sample size and limited length of exposure in AS and nr-axSpA compared to RA or PsA. Active comparators (adalimumab or methotrexate) were only assessed in one or two studies, with smaller drug exposure compared to upadacitinib, which makes the interpretation of these data more limited. Comparisons between the SELECT trials and ORAL Surveillance should be treated with caution because of differences in study design, in particular the lack of an enriched, at-risk patient population (≥ 50 years of age with at least one additional cardiovascular risk factor) in the SELECT trials or this post hoc analysis. In addition, these data were gathered from controlled clinical trials, which may not be entirely reflective of data gathered in real-world clinical practice or typical cancer screening practices that occur in routine care settings. Findings from the univariable regression models to assess the impact of known risk factors on the incidence of malignancy excluding NMSC and NMSC in RA and PsA should be interpreted with caution because of the low rates of malignancy reported in these studies. Further evaluation with longer-term exposure to upadacitinib, which may allow for the use of more sophisticated multivariable modeling, is required to make firmer conclusions regarding risk factors for malignancy with upadacitinib treatment.
Conclusion
Event rates of malignancy excluding NMSC were generally similar between upadacitinib 15 mg (the approved dose for RA, PsA, AS, and nr-axSpA), upadacitinib 30 mg, adalimumab, and methotrexate, and were consistent across RA, PsA, AS, and nr-axSpA. In RA, there was a dose-dependent increase in NMSC, with rates being higher with upadacitinib 30 mg treatment than upadacitinib 15 mg. In addition, rates of NMSC were higher with both upadacitinib doses versus adalimumab and methotrexate. This analysis provides important safety information on malignancies with upadacitinib treatment across RA, PsA, AS, and nr-axSpA, which can help inform treatment decisions to improve patient care.
Data Availability
AbbVie is committed to responsible data sharing regarding the clinical trials we sponsor. This includes access to anonymized, individual, and trial-level data (analysis data sets), as well as other information (e.g., protocols, clinical study reports, or analysis plans), as long as the trials are not part of an ongoing or planned regulatory submission. This includes requests for clinical trial data for unlicensed products and indications. These clinical trial data can be requested by any qualified researchers who engage in rigorous, independent, scientific research, and will be provided following review and approval of a research proposal, Statistical Analysis Plan (SAP), and execution of a Data Sharing Agreement (DSA). Data requests can be submitted at any time after approval in the USA and Europe and after acceptance of this manuscript for publication. The data will be accessible for 12 months, with possible extensions considered. For more information on the process or to submit a request, visit the following link: https://vivli.org/ourmember/abbvie/ then select “Home”.
References
Rubbert-Roth A, Kakehasi A, Takeuchi T, et al. Malignancy in the upadacitinib clinical trial programs for rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis [abstract]. Arthritis Rheumatol. 2022;74(suppl 9).
Franks AL, Slansky JE. Multiple associations between a broad spectrum of autoimmune diseases, chronic inflammatory diseases and cancer. Anticancer Res. 2012;32:1119–36.
Thomas E, Brewster DH, Black RJ, Macfarlane GJ. Risk of malignancy among patients with rheumatic conditions. Int J Cancer. 2000;88:497–502.
Bongartz T, Sutton AJ, Sweeting MJ, Buchan I, Matteson EL, Montori V. Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA. 2006;295:2275–85.
Krathen MS, Gottlieb AB, Mease PJ. Pharmacologic immunomodulation and cutaneous malignancy in rheumatoid arthritis, psoriasis, and psoriatic arthritis. J Rheumatol. 2010;37:2205–15.
Szekanecz Z, Szekanecz É, Bakó G, Shoenfeld Y. Malignancies in autoimmune rheumatic diseases—a mini-review. Gerontology. 2010;57:3–10.
Simon TA, Thompson A, Gandhi KK, Hochberg MC, Suissa S. Incidence of malignancy in adult patients with rheumatoid arthritis: a meta-analysis. Arthritis Res Ther. 2015;17:212.
Campanholo CB, Maharaj AB, Corp N, et al. Management of psoriatic arthritis in patients with comorbidities: an updated literature review informing the 2021 GRAPPA treatment recommendations. J Rheumatol. 2023;50(3):426–32.
Hagberg KW, Li L, Peng M, Paris M, Shah K, Jick SS. Rates of cancers and opportunistic infections in patients with psoriatic arthritis compared with patients without psoriatic arthritis. J Clin Rheumatol. 2016;22:241–7.
Karmacharya P, Shahukhal R, Ogdie A. Risk of malignancy in spondyloarthritis a systematic review. Rheum Dis Clin N Am. 2020;46:463–511.
Bittar M, Merjanah S, Alkilany R, Magrey M. Malignancy in ankylosing spondylitis: a cross-sectional analysis of a large population database. BMC Rheumatol. 2022;6:44.
Ytterberg SR, Bhatt DL, Mikuls TR, et al. Cardiovascular and cancer risk with tofacitinib in rheumatoid arthritis. New Engl J Med. 2022;386:316–26.
Curtis JR, Yamaoka K, Chen Y-H, et al. Malignancy risk with tofacitinib versus TNF inhibitors in rheumatoid arthritis: results from the open-label, randomised controlled ORAL Surveillance trial. Ann Rheum Dis. 2022;82:1–13.
Smolen JS, Pangan AL, Emery P, et al. Upadacitinib as monotherapy in patients with active rheumatoid arthritis and inadequate response to methotrexate (SELECT-MONOTHERAPY): a randomised, placebo-controlled, double-blind phase 3 study. Lancet. 2019;393:2303–11.
Genovese MC, Fleischmann R, Combe B, et al. Safety and efficacy of upadacitinib in patients with active rheumatoid arthritis refractory to biologic disease-modifying anti-rheumatic drugs (SELECT-BEYOND): a double-blind, randomised controlled phase 3 trial. Lancet. 2018;391:2513–24.
Rubbert-Roth A, Enejosa J, Pangan AL, et al. Trial of upadacitinib or abatacept in rheumatoid arthritis. N Engl J Med. 2020;383:1511–21.
van Vollenhoven R, Takeuchi T, Pangan AL, et al. Efficacy and safety of upadacitinib monotherapy in methotrexate-naive patients with moderately-to-severely active rheumatoid arthritis (SELECT-EARLY): a multicenter, multi-country, randomized, double-blind, active comparator-controlled trial. Arthritis Rheumatol. 2020;72:1607–20.
Burmester GR, Kremer JM, Van den Bosch F, et al. Safety and efficacy of upadacitinib in patients with rheumatoid arthritis and inadequate response to conventional synthetic disease-modifying anti-rheumatic drugs (SELECT-NEXT): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2018;391:2503–12.
Fleischmann R, Pangan AL, Song IH, et al. Upadacitinib versus placebo or adalimumab in patients with rheumatoid arthritis and an inadequate response to methotrexate: results of a phase III, double-blind, randomized controlled trial. Arthritis Rheumatol. 2019;71:1788–800.
McInnes IB, Anderson JK, Magrey M, et al. Trial of upadacitinib and adalimumab for psoriatic arthritis. N Engl J Med. 2021;384:1227–39.
Mease PJ, Lertratanakul A, Anderson JK, et al. Upadacitinib for psoriatic arthritis refractory to biologics: SELECT-PsA 2. Ann Rheum Dis. 2020;80:312–20.
van der Heijde D, Song IH, Pangan AL, et al. Efficacy and safety of upadacitinib in patients with active ankylosing spondylitis (SELECT-AXIS 1): a multicentre, randomised, double-blind, placebo-controlled, phase 2/3 trial. Lancet. 2019;394:2108–17.
van der Heijde D, Baraliakos X, Sieper J, et al. Efficacy and safety of upadacitinib for active ankylosing spondylitis refractory to biological therapy: a double-blind, randomised, placebo-controlled phase 3 trial. Ann Rheum Dis. 2022;81(11):1515–23.
Deodhar A, Van den Bosch F, Poddubnyy D, et al. Upadacitinib for the treatment of active non-radiographic axial spondyloarthritis (SELECT-AXIS 2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2022;400:369–79.
Khosrow-Khavar F, Desai RJ, Lee H, Lee SB, Kim SC. Tofacitinib and risk of malignancy: results from the safety of tofacitinib in routine care patients with rheumatoid arthritis (STAR-RA) study. Arthritis Rheumatol. 2022;74:1648–59.
Kremer JM, Bingham CO, Cappelli LC, et al. Postapproval comparative safety study of tofacitinib and biological disease-modifying antirheumatic drugs: 5-year results from a United States-based rheumatoid arthritis registry. Acr Open Rheumatology. 2021;3(3):173–84.
Huss V, Bower H, Hellgren K, Frisell T, Askling J. Cancer risks with JAKi and biological disease-modifying antirheumatic drugs in patients with rheumatoid arthritis or psoriatic arthritis: a national real-world cohort study. Ann Rheum Dis. 2023;82(7):911–19.
Meudec L, Richebé P, Pascaud J, Mariette X, Nocturne G. Janus kinase inhibitors alter NK cell phenotypes and inhibit their antitumour capacity. Rheumatology. 2022;62:2855–63.
Fleischmann R, Curtis JR, Charles-Schoeman C, et al. Safety profile of upadacitinib in patients at risk of cardiovascular disease: integrated post hoc analysis of the SELECT phase III rheumatoid arthritis clinical programme. Ann Rheum Dis. 2023;82(9):1130–41.
Cohen SB, van Vollenhoven RF, Winthrop KL, et al. Safety profile of upadacitinib in rheumatoid arthritis: integrated analysis from the SELECT phase III clinical programme. Ann Rheum Dis. 2021;3:304–11.
AbbVie. RINVOQ® (upadacitinib) [Prescribing Information]. https://www.rxabbvie.com/pdf/rinvoq_pi.pdf. Accessed 2023 Jul 25.
Nash P, Kerschbaumer A, Dörner T, et al. Points to consider for the treatment of immune-mediated inflammatory diseases with Janus kinase inhibitors: a consensus statement. Ann Rheum Dis. 2021;80:71–87.
Pfizer. XELJANZ® (tofacitinib) [Prescribing Information]. https://labeling.pfizer.com/ShowLabeling.aspx?id=959. Accessed 2023 Jul 25.
Lilly. OLUMIANT® (baricitinib) [Prescribing Information]. https://uspl.lilly.com/olumiant/olumiant.html#pi. Accessed 2023 Jul 25.
Jiyad Z, Marquart L, Green AC. A call to standardize the BCC:SCC ratio. Br J Dermatol. 2021;184:545–545.
Chahal HS, Rieger KE, Sarin KY. Incidence ratio of basal cell carcinoma to squamous cell carcinoma equalizes with age. J Am Acad Dermatol. 2017;76:353–4.
Muzic JG, Schmitt AR, Wright AC, et al. Incidence and trends of basal cell carcinoma and cutaneous squamous cell carcinoma a population-based study in Olmsted county, Minnesota, 2000 to 2010. Mayo Clin Proc. 2017;92:890–8.
Nagarajan P, Asgari MM, Green AC, et al. Keratinocyte carcinomas: current concepts and future research priorities. Clin Cancer Res. 2019;25:2379–91.
Jones OT, Ranmuthu CKI, Hall PN, Funston G, Walter FM. Recognising skin cancer in primary care. Adv Ther. 2020;37:603–16.
Griffin LL, Ali FR, Lear JT. Non-melanoma skin cancer. Clin Med. 2016;16:62–5.
Pandeya N, Olsen CM, Whiteman DC. The incidence and multiplicity rates of keratinocyte cancers in Australia. Méd J Aust. 2017;207:339–43.
Wilton KM, Crowson CS, Matteson EL. Malignancy incidence in patients with psoriatic arthritis: a comparison cohort-based incidence study. Clin Rheumatol. 2016;35:2603–7.
Fane M, Weeraratna AT. How the ageing microenvironment influences tumour progression. Nat Rev Cancer. 2020;20:89–106.
Oberyszyn TM. Non-melanoma skin cancer: Importance of gender, immunosuppressive status and vitamin D. Cancer Lett. 2008;261:127–36.
Lewandowska AM, Rudzki M, Rudzki S, Lewandowski T, Laskowska B. Environmental risk factors for cancer—review paper. Ann Agric Environ Med. 2018;26:1–7.
Pergola GD, Silvestris F. Obesity as a major risk factor for cancer. J Obes. 2013;2013: 291546.
Acknowledgements
AbbVie and the authors thank the patients, study sites, and investigators who participated in these clinical trials
Writing, Editorial, and Other Assistance.
Medical writing support was provided by Monica R.P. Elmore, PhD, of AbbVie. Editorial support was provided by Angela T. Hadsell of AbbVie.
Author Contributions.
Andrea Rubbert-Roth, Hannah Palac, Derek Coombs, Jianzhong Liu, Samuel I. Anyanwu, Ralph Lippe, and Jeffrey R. Curtis participated in the design of the study. Andrea Rubbert-Roth participated in the acquisition of data. Hannah Palac and Derek Coombs participated in the analysis of data. All authors (Andrea Rubbert-Roth, Adriana M. Kakehasi, Tsutomu Takeuchi, Marc Schmalzing, Hannah Palac, Derek Coombs, Jianzhong Liu, Samuel I. Anyanwu, Ralph Lippe, and Jeffrey R. Curtis) participated in the interpretation of data and contributed to the drafting and critical revision of the manuscript for important intellectual content. All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. No honoraria or payments were made for authorship.
Funding
AbbVie funded these trials (NCT02706873, NCT02675426, NCT02629159, NCT02706951, NCT02706847, NCT03086343, NCT03104400, NCT03104374, NCT03178487, and NCT04169373) and participated in the study design, research, analysis, data collection, interpretation of data, reviewing, and approval of the publication. AbbVie funded the journal’s Rapid Service Fee.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Financial arrangements of the authors with companies whose products may be related to the present manuscript are listed, as declared by the authors. Andrea Rubbert-Roth: Received honoraria for lectures and consulting from AbbVie, Amgen, BMS, Eli Lilly, Gilead, Janssen, MSD, Novartis, Pfizer, Roche, Sanofi, and UCB. Adriana M. Kakehasi: Served as a consultant or member of a speaker’s bureau for, and has received grant/research support from, AbbVie, Amgen, Fresenius Klabi, Janssen, Eli Lilly, Pfizer, Organon, Sandoz, and UCB. Tsutomu Takeuchi: Grant/research support from AbbVie and Eisai; consulting fees from AbbVie, Astellas Pharma, Eli Lilly Japan, and Gilead Sciences; speaker/honoraria from AbbVie, Astellas Pharma, Eisai, Eli Lilly Japan, Gilead Sciences, and Pfizer Japan. Marc Schmalzing: Compensation for consulting from Chugai/Roche, Hexal/Sandoz, Gilead, AbbVie, Janssen-Cilag, Boehringer/Ingelheim, onkowissen.de, EUSA-Pharma, Novartis, AstraZeneca, Amgen, Medac, Lilly, and Galapagos; speaker’s fees from Novartis, AbbVie, AstraZeneca, Chugai/Roche, Janssen-Cilag, Gilead, Boehringer/Ingelheim, Mylan, Galapagos, and EUSA-Pharma; travel grants from Chugai/Roche, Boehringer/Ingelheim, Celgene, Medac, UCB, Mylan, and Galapagos. Hannah Palac: Employee of AbbVie and may hold stock or stock options. Derek Coombs: Employee of AbbVie and may hold stock or stock options. Jianzhong Liu: Employee of AbbVie at time of study and has since retired. May hold stock or stock options in Abbvie. Samuel I. Anyanwu: Employee of AbbVie and may hold stock or stock options. Ralph Lippe: Employee of AbbVie and may hold stock or stock options. Jeffrey R. Curtis: Research grants from AbbVie, Amgen, Bristol Myers Squibb, CorEvitas, Janssen, Labcorp, Lilly, Novartis, Pfizer, Sanofi/Regeneron, and UCB; consulting fees from AbbVie, Amgen, Bristol Myers Squibb, CorEvitas, Janssen, Labcorp, Lilly, Novartis, Pfizer, Sanofi/Regeneron, and UCB.
Ethical Approval
All studies were conducted in accordance with the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) guidelines, applicable regulations governing clinical trial conduct, and the Declaration of Helsinki 1964 and its later amendments. The trial protocols were approved by an independent ethics committee (IEC)/institutional review board (IRB) at each study site per Good Clinical Practice (GCP). All patients provided written informed consent prior to screening.
Additional information
Jianzhong Liu: at AbbVie Inc. during time of study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Rubbert-Roth, A., Kakehasi, A.M., Takeuchi, T. et al. Malignancy in the Upadacitinib Clinical Trials for Rheumatoid Arthritis, Psoriatic Arthritis, Ankylosing Spondylitis, and Non-radiographic Axial Spondyloarthritis. Rheumatol Ther 11, 97–112 (2024). https://doi.org/10.1007/s40744-023-00621-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-023-00621-6