Abstract
Introduction
To evaluate the effect of upadacitinib vs. placebo on health-related quality of life (HRQoL) and work productivity in patients with active non-radiographic axial spondyloarthritis (nr-axSpA) enrolled in the SELECT-AXIS 2 phase 3 randomized controlled trial.
Methods
Adult patients with active nr-axSpA and an inadequate response to non-steroidal anti-inflammatory drugs were randomized 1:1 to receive upadacitinib 15 mg once daily or placebo. Mean changes from baseline in measures of HRQoL (Ankylosing Spondylitis QoL [ASQoL], Assessment of SpondyloArthritis international Society Health Index [ASAS HI], Short-Form 36 Physical Component Summary [SF-36 PCS] score) and Work Productivity and Activity Impairment (WPAI) were assessed through 14 weeks based on mixed-effects repeated measures or analysis of covariance models. The proportions of patients with improvements ≥ minimum clinically important differences (MCID) were assessed in HRQoL measures at week 14 using non-responder imputation with multiple imputation.
Results
At week 14, upadacitinib- vs. placebo-treated patients reported greater improvements from baseline in ASQoL and ASAS HI (ranked, P < 0.001) and in SF-36 PCS and WPAI overall work impairment (nominal P < 0.05). Improvements were observed as early as week 2 in ASAS HI. Greater proportions of upadacitinib vs. placebo-treated patients reported improvements ≥ MCID in ASQoL (62.6 vs. 40.9%), ASAS HI (44.8 vs. 28.8%), and SF-36 PCS (69.3 vs. 52.0%), with numbers needed to treat < 10 for all (nominal P ≤ 0.01). Improvements ≥ MCID were consistently observed irrespectively of prior exposure to tumor necrosis factor inhibitors.
Conclusions
Upadacitinib provides clinically meaningful improvements in HRQoL and work productivity in patients with active nr-axSpA.
Clinical Registration Number
NCT04169373, SELECT-AXIS 2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
In addition to reduced mobility and the presence of objective signs and symptoms of inflammation, patients with non-radiographic axial spondyloarthritis (nr-axSpA) frequently experience reduced health-related quality of life (HRQoL) and work productivity. |
This study evaluated the impact of Janus kinase inhibitor, upadacitinib, versus placebo on response rates and clinically meaningful improvements in patient-reported outcomes (PROs) in patients with active nr-axSpA in SELECT-AXIS 2. |
What was learned from the study? |
Upadacitinib improved mean HRQoL and work productivity measures from baseline to week 14 compared to placebo (ASQoL and ASAS HI, ranked, P < 0.001; SF-36 PCS and three of four WPAI domains, nominal P < 0.05). |
Higher proportions of patients achieved clinically meaningful improvements in HRQoL measures, including ASQoL (62.6 vs. 40.9%), ASAS HI (44.8 vs. 28.8%), and SF-36 PCS (69.3 vs. 52.0%) at week 14 with upadacitinib vs. placebo (nominal P ≤ 0.01). |
Improvements in HRQoL occurred as early as week 2 for ASAS HI and week 4 for ASQoL and SF-36 PCS. |
Introduction
Axial spondyloarthritis (axSpA) is a chronic inflammatory condition with manifestations primarily involving the sacroiliac joints (SIJs) and spine [1,2,3]. Axial SpA comprises two subsets of disease, classified as radiographic axSpA (r-axSpA, historically known as ankylosing spondylitis [AS]) and non-radiographic axSpA (nr-axSpA), with r-axSpA or AS presenting with structural damage of the SIJ visible on X-ray and nr-axSpA presenting with no definitive radiographic evidence of SIJ structural damage [2, 4, 5]. Additionally, patients with nr-axSpA compared to AS are more frequently female, have lower levels of inflammation as measured via C-reactive protein (CRP), and have a shorter disease duration [6,7,8].
Inflammatory back pain is a hallmark of both AS and nr-axSpA, frequently contributing to functional impairments and work disability [2, 9, 10]. Patients have rated spinal pain as the most important aspect influencing the burden of axSpA [11]. Additionally, patients with axSpA experience a significant disease burden on their health-related quality of life (HRQoL) and ability to perform daily activities and an increased prevalence of comorbidities contributing to higher healthcare costs [2, 12]. Disease burden in terms of disease activity and impairments in physical activity as well as HRQoL was shown to be similarly affected in nr-axSpA and AS [13].
The goal of treatment includes maximizing HRQoL through control of inflammation, prevention of progressive structural damage, and normalization of function [2, 3, 14,15,16]. The Assessment of SpondyloArthritis international Society (ASAS) and the European Alliance of Associations for Rheumatology (EULAR) now recommend biological disease-modifying antirheumatic drugs (bDMARDs) such as tumor necrosis factor (TNF) inhibitors (TNFis) and interleukin (IL)-17 inhibitors, or Janus kinase (JAK) inhibitors, as treatment in patients with axSpA and persistently high disease activity despite prior use of non-steroidal anti-inflammatory drugs (NSAIDs) [14, 16]. The American College of Rheumatology, Spondylitis Association of America, and Spondyloarthritis Research and Treatment Network recommend a similar treatment approach [15]. Approved treatment options for nr-axSpA are limited and until recently included only TNFis and IL-17 inhibitors, highlighting a need for an oral treatment option for the entire spectrum of axSpA.
Upadacitinib, an oral JAK inhibitor, was recently approved for the treatment of active nr-axSpA in adult patients with objective signs of inflammation in the European Union and the United States, based on data from the SELECT-AXIS 2 study, which evaluated the safety and efficacy of upadacitinib vs. placebo in patients with active nr-axSpA with or without prior exposure to bDMARDs [17]. This analysis evaluated response rates and clinically meaningful improvements in HRQoL and work productivity in patients with active nr-axSpA treated with upadacitinib 15 mg vs. placebo in the SELECT-AXIS 2 trial.
Methods
Study Design and Participants
The study design and primary results through week 14 from the global, multicenter, phase 3 clinical trial SELECT-AXIS 2 were previously reported [17]. Patients in this 52-week randomized, double-blind, parallel-group, placebo-controlled study were randomized 1:1 to receive upadacitinib 15 mg once daily or placebo, followed by a 52-week open-label extension period. The primary endpoint was the ASAS40 response rate at week 14. Here we report improvement in HRQoL and work productivity through 14 weeks in patients with active nr-axSpA enrolled in the SELECT-AXIS 2 trial.
As previously described, eligible patients were adults with a clinical diagnosis of active nr-axSpA, fulfilling the 2009 ASAS classification criteria [5] but not the radiological criterion of the modified New York criteria [18], and an inadequate response or intolerance to ≥ 2 NSAIDs [17]. Included patients had objective signs of inflammation-based magnetic resonance imaging (MRI) of the SIJ or elevated CRP [17]. Patients who were MRI-negative but had elevated CRP were eligible for enrolment. Prior treatment with no more than one bDMARD (TNFi or IL-17 inhibitor) was permitted for at least 20% but no more than 35% of patients who discontinued prior bDMARD due to lack of efficacy (after at least 12 weeks of treatment at an adequate dose) or intolerance (irrespective of treatment duration). Patients who had a lack of efficacy for both a TNFi and IL-17 inhibitor were not eligible for enrolment. In addition, previous exposure to a JAK inhibitor was prohibited.
Compliance with Ethics Guidelines
The SELECT-AXIS 2 trial was conducted in compliance with the International Conference on Harmonization guidelines, local regulations and guidelines governing clinical study conduct, and the ethical principles of the Declaration of Helsinki. As per Good Clinical Practice, the protocol was approved by an ethics committee or institutional review board at all study sites (Supplemental Table S1). All patients provided informed consent before study participation.
Outcomes
This analysis assessed mean change from baseline as well as the proportion of patients reporting clinically meaningful improvements across multiple measures of HRQoL and work productivity.
The mean change from baseline through 14 weeks was assessed for the following measures of HRQoL: Ankylosing Spondylitis Quality of Life (ASQoL) [19], ASAS Health Index (ASAS HI) [20], and Short Form-36 (SF-36) Physical Component Summary (PCS) score [21]; and for work productivity, by the Work Productivity and Activity Impairment (WPAI) Questionnaire [22]. WPAI consists of the following four domains: absenteeism (work missed), presenteeism (reduced work effectiveness), overall work impairment, and activity impairment.
Clinically meaningful improvements were assessed for key patient-reported measures that assess HRQoL and physical function with validated minimum clinically important difference (MCID) thresholds, including ASQoL (MCID ≥ 3-point decrease [2]), ASAS HI (MCID ≥ 3-point decrease [23]), and SF-36 PCS (MCID ≥ 2.5-point increase [24]).
Post-baseline assessments of ASQoL, ASAS-HI, and SF-36 PCS began at week 1, with ASQoL and SF-36 PCS assessed at weeks 1, 4, 8, and 14 and ASAS HI at weeks 1, 2, 4, 8, and 14. Post-baseline assessments for WPAI began at week 14. Mean change from baseline was assessed at each week when assessment data was collected through 14 weeks. Clinically meaningful improvements ≥ MCID were assessed at week 14. WPAI absenteeism, presenteeism, and overall work impairment domains were assessed in patients employed at baseline, while activity impairment was assessed in all patients.
Statistical Analyses
Analyses were conducted in the full analysis set, which included all randomized patients who received at least one dose of study drug. Baseline characteristics are summarized with descriptive statistics using means and standard deviation for continuous endpoints and frequency (n) and percentages for categorical endpoints. For ranked endpoints (mean change from baseline to week 14 in ASQoL and ASAS HI), results were obtained via sequential multiple testing procedure controlling the overall type I error rate of all primary and multiplicity-adjusted secondary endpoints at the significance level of 0.05. Other outcomes were not multiplicity adjusted and all other reported P values were nominal.
Mean change from baseline to week 14 along with 95% confidence intervals (CIs) and nominal P values were based on mixed-effects repeated measures model (MMRM) analysis, including stratification factors of treatment, visit, and treatment-by-visit interaction as fixed factors and baseline value as a covariate for all patient-reported outcomes (PROs) except WPAI. MRI and screening high-sensitivity CRP (hsCRP) status were also included in the model as main stratification factors. All observed patient data were included in the MMRM. For WPAI, within-group mean change from baseline and 95% CI and between-group least squares mean, 95% CI, and nominal P value for each visit were based on an analysis of covariance model, including treatment and baseline value as a covariate; MRI and screening hsCRP status were also included in the model.
The number and percentage of patients with improvements in each PRO ≥ MCID are summarized at week 14. Comparisons of the proportion of patients achieving MCID were made between upadacitinib and the placebo group using the Cochran–Mantel–Haenszel test (CMH). The point estimate and 95% CIs estimated using normal approximation and nominal P values for the treatment comparisons are presented. The number needed to treat (NNT), defined as the number of patients who need to receive treatment to achieve one additional ‘responder’ on a PRO of interest vs. placebo, was calculated. Specifically, NNTs for each PRO with an MCID were calculated as follows: 1/ (MCID response rate in the treatment group—MCID response rate in the placebo group), and the NNTs per MCID response were compared between upadacitinib and placebo using the CMH test at week 14. For all MCID analyses, missing data were reported using non-responder imputation (NRI) incorporating multiple imputation (MI) to handle missing data due to COVID-19 or NRI if there were no missing data due to COVID-19. The number of responders was based on the total number of patients and MI-aggregated response rates.
The proportion of patients who achieved Ankylosing Spondylitis Disease Activity Score (ASDAS) inactive disease (ASDAS CRP < 1.3) at week 14 among those who achieved MCID for ASAS HI, ASQoL, and SF-36 PCS, separately, at week 14 was calculated for the full analysis set. MCID and NNT analyses were repeated in a post hoc subgroup analysis of patients stratified by prior TNFi status. Patients were categorized as TNFi-naïve if they had no prior exposure to TNFis, and patients who had prior exposure, including either intolerance or lack of efficacy to TNFis were categorized as TNFi-IR at baseline.
Results
Several key baseline characteristics were previously reported for the SELECT-AXIS 2 study [17]. A total of 313 patients with active nr-axSpA were included in the analysis, of whom 156 and 157 were randomized to upadacitinib or placebo, respectively. Most patients were female (58.5%), with a mean age of approximately 42 years. Baseline impairments were observed in patient-reported measures of HRQoL, as indicated by the high scores in ASAS HI and ASQoL and low scores in SF-36 PCS (Table 1). Baseline scores in WPAI overall work impairment (mean scores: 60.4 placebo and 54.6 upadacitinib 15 mg) indicate a loss in work productivity in these patients. Overall, baseline characteristics and PRO scores were balanced across treatment groups (Table 1).
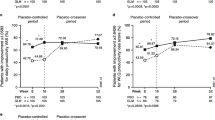
Significant improvements in mean change from baseline to week 14 were reported with upadacitinib 15 mg compared with placebo across key ranked secondary endpoints ASQoL and ASAS HI (P < 0.001); improvements from baseline in SF-36 PCS were also greater with upadacitinib compared to placebo (nominal P < 0.001) (Fig. 1). Improvements from baseline with upadacitinib 15 mg differentiated from placebo as early as week 2 for ASAS HI and week 4 for ASQoL and SF-36 PCS and continued to week 14 (Fig. 1). Furthermore, improvement in mean change from baseline to week 14 across WPAI domains of presenteeism, overall work impairment, and activity impairment was greater with upadacitinib 15 mg compared with placebo (nominal P < 0.05); however, improvement in absenteeism was similar between treatment groups (nominal P = 0.3387) (Fig. 2).
Change from baseline through week 14 in A ASQoL, B ASAS HI, and C SF-36 PCS (MMRM). *Nominal P value ≤ 0.05; **nominal P value ≤ 0.01; ***nominal P value ≤ 0.001. aSignificant after multiplicity adjustment. MMRM analysis included treatment, visit, and treatment-by-visit interaction as fixed factors and baseline value as covariate. Stratification factor hsCRP level (≤ ULN vs. > ULN) was also included in the model. ASAS HI Assessment of SpondyloArthritis international Society Health Index, ASQoL Ankylosing Spondylitis Quality of Life, CI confidence interval, hsCRP high-sensitivity C-reactive protein, MMRM mixed-effect model for repeated measures, PBO placebo, PCS Physical Component Summary, SF-36 36-Item Short Form Health Survey, ULN upper limit of normal, UPA upadacitinib
Mean change (95% CI) from baseline in WPAI at week 14. *Nominal P value ≤ 0.05; **nominal P value ≤ 0.01. aIncludes patients currently employed. Within-group mean and 95% CI and between-group mean, 95% CI, and nominal P value for each visit are based on analysis of covariance model including treatment and main stratification factors MRI and screening hsCRP status (MRI + /hsCRP > ULN, MRI + /hsCRP ≤ ULN, and MRI–/hsCRP > ULN) as fixed factors and baseline value as covariate for all WPAI domains. CI confidence interval, hsCRP high-sensitivity C-reactive protein, MRI magnetic resonance imaging, PBO placebo, ULN upper limit of normal, UPA upadacitinib, WPAI Work Productivity and Activity Impairment
At week 14, a higher proportion of patients reported clinically meaningful improvements ≥ MCID with upadacitinib 15 mg compared with placebo in key PRO measures of ASQoL (62.6 vs. 40.9%; nominal P ≤ 0.001), ASAS HI (44.8 vs. 28.8%; nominal P ≤ 0.01), and SF-36 PCS (69.3 vs. 52.0%; nominal P ≤ 0.01) (Fig. 3). The NNTs were < 10, ranging from 4.6 to 6.2 for all PROs assessed, suggesting a clinically relevant difference [25] in measures of HRQoL (Fig. 3).
Proportion of patients reporting improvements ≥ MCID and NNTs in PROs at week 14 (NRI-MI). **Nominal P ≤ 0.01 and ***nominal P ≤ 0.001 versus placebo. NRI-MI is non-responder imputation (NRI) incorporating multiple imputation (MI) to handle missing data due to COVID-19. MCID definitions: ≥ 3 points decrease (ASAS HI and ASQoL) and ≥ 2.5-point increase (SF-36 PCS). ASAS HI Assessment of SpondyloArthritis international Society Health Index, ASQoL Ankylosing Spondylitis Quality of Life, MCID minimal clinically important difference, NNT number needed to treat, PBO placebo, PCS Physical Component Summary, PRO patient-reported outcome, SF-36 36-Item Short Form Health Survey, UPA upadacitinib
Clinically Meaningful Improvements in PROs by TNF Exposure Status
The subgroup analysis included 226 patients who were TNFi-naïve (n = 114 for placebo and n = 112 for upadacitinib) and 87 patients who were TNFi-IR (n = 43 for placebo and n = 44 for upadacitinib). Patients who had prior exposure to both mechanisms of action (i.e., protocol deviations) are not excluded here; this includes 3 patients randomized to placebo in the TNFi-IR subgroup who also had prior exposure to IL-17 inhibitors. The TNFi-naïve subgroup included 16 patients with prior exposure to IL-17 inhibitors only. In patients who were TNFi-naïve, a greater proportion of patients treated with upadacitinib 15 mg vs. placebo reported achieving clinically meaningful improvements in ASQoL (64.0 vs. 38.7%; nominal P ≤ 0.001), ASAS HI (46.4 vs. 27.3%; nominal P ≤ 0.01), and SF-36 PCS (70.4 vs. 54.1%; nominal P ≤ 0.01) (Supplementary Fig. S1A). Consistent with the full analysis set and TNFi-naïve population, patients with prior exposure to TNFis at baseline reported a numerically higher proportion of patients achieving clinically meaningful improvements in ASQoL (59.1 vs. 46.5%; nominal P = 0.2216), ASAS HI (40.9 vs. 32.6%; nominal P = 0.4166), and SF-36 PCS (66.7 vs. 46.5%; nominal P < 0.05) with upadacitinib 15 mg treatment at week 14 compared with placebo (Supplemental Fig. S1B). Most NNTs were < 10, ranging from 4.0 to 6.1 for all PROs assessed in the TNFi-naïve patients and from 4.8 to 12.0 in the TNFi-IR patients, suggesting a clinically relevant difference in most measures of HRQoL regardless of prior treatment status [25].
Achievement of Inactive Disease Among Those who Achieved Clinically Meaningful Improvement in PROs
A higher proportion of patients treated with upadacitinib 15 mg compared with placebo achieved ASDAS inactive disease among those who achieved clinically meaningful improvements in ASQoL (21.5 vs. 9.4%; nominal P < 0.05), ASAS HI (28.6 vs. 11.1%; nominal P < 0.05), and SF-36 PCS (20.3 vs. 8.6%; nominal P < 0.05) (Supplementary Fig. S2). The percentage of patients who achieved ASDAS inactive disease overall, without consideration for MCID achievement, was 14.1 vs. 5.2% for upadacitinib- vs. placebo-treated patients, respectively [17].
Discussion
The burden of disease in patients with active nr-axSpA is high, with a detrimental impact on pain, physical function, HRQoL, loss of work productivity, and limits to daily activities [2, 26, 27]. The SELECT-AXIS 2 trial is the first to investigate a JAK inhibitor for the treatment of active nr-axSpA. In this study, improvements from baseline were significantly greater in active nr-axSpA patients treated with upadacitinib vs. placebo at week 14 in key measures of HRQoL, ASQoL, and ASAS HI. Additionally, as previously reported, improvements from baseline were also demonstrated to be greater with upadacitinib vs. placebo at week 14 in total and nocturnal back pain and function as assessed by Bath Ankylosing Spondylitis Functional Index (BASFI) [17]. Clinically meaningful improvements were observed in greater proportions of patients treated with upadacitinib vs. placebo across ASQoL, ASAS HI, and SF-36 PCS, with NNTs meeting the clinically meaningful threshold of < 10 [25]. Results were consistent among patients who were TNFi-naïve and those who previously failed TNFi treatment, with NNTs < 10 for most PROs, suggesting upadacitinib may be a beneficial treatment in patients refractory to bDMARDs.
Notably, improvements in HRQoL occurred rapidly in patients treated with upadacitinib vs. placebo. Specifically, improvements in disease-specific and general HRQoL, as measured by ASQoL, ASAS HI, and SF-36 PCS, occurred as early as weeks 2–4; as previously reported, improvements in patient-reported measures of pain and physical function (BASFI) also occurred as early as weeks 2–4 [17]. These rapid improvements from the patient perspective are aligned with treatment goals of reaching early status of inactive disease, normalization of function, and improvement in HRQoL [16].
Furthermore, positive improvements in pain, as well as physical function and general HRQoL as measured by SF-36 PCS and ASAS HI, were consistent with previous studies with IL-17 inhibitors [28, 29]. Results were also consistent with studies with TNFi treatments in nr-axSpA [30,31,32]. Importantly, in the current study, comparable or better outcomes were observed in measures of HRQoL irrespective of prior TNFi exposure status, providing additional evidence for upadacitinib as a potential treatment option in patients with active nr-axSpA, including patients with inadequate response to prior advanced therapies.
Several studies have demonstrated that improvements in PROs are associated with improved clinical measures of disease activity and symptoms, which is critical in axSpA given the high disease burden [28, 30, 33,34,35]. A significantly greater proportion of patients with active nr-axSpA treated with upadacitinib vs. placebo achieved the primary endpoint of ASAS40 at week 14 as well as the threshold of ASDAS inactive disease [17]. Although the current study did not assess a statistical correlation between patients who achieved ASDAS inactive disease and PRO outcomes, improvements in measures of HRQoL were observed through week 14 in nr-axSpA patients treated with upadacitinib. Additionally, among patients who achieved improvements in HRQoL ≥ MCID, the percentage who achieved ASDAS inactive disease with upadacitinib treatment ranged from 20 to 28%, which was numerically higher than the proportion of patients who achieved ASDAS inactive disease for the overall population (reported as 15% with upadacitinib) [17]. Given the correlation between PROs and provider-assessed disease activity and symptoms, future studies may be warranted to characterize this relationship in patients with active nr-axSpA treated with upadacitinib. The high placebo responses observed in AS studies [36] also suggest that measuring patients’ perception of symptom improvement is important to better differentiate treatment effects.
In addition to PROs assessing HRQoL, we also evaluated the impact of upadacitinib treatment on patients’ ability to work. Guidelines recommend that work productivity loss be considered in treatment decisions as it is associated with the indirect economic burden of axSpA [14]. Furthermore, compared to patients with AS, patients with nr-axSpA reported greater impacts of disease on presenteeism and overall activity impairment [2]. Greater improvements from baseline to week 14 in patients treated with upadacitinib vs. placebo were observed in the WPAI domains of presenteeism, overall work impairment, and activity impairment, suggesting that upadacitinib may improve patients’ work productivity and ability to perform daily activities. These improvements are encouraging, given that ability to work is influenced by multiple dimensions.
There are strengths and limitations to this current analysis. Strengths include the randomized study design, which mitigates bias that may arise due to unobservable differences between cohorts, as well as the use of validated PROs to assess improvements in patients’ perception of their symptoms. Limitations including small sample size may result in imprecise estimates and limit the ability to make causal inferences, particularly in subgroup analyses. The number of patients exposed to IL-17 inhibitors was small; therefore, no analysis was conducted assessing outcomes specifically in this population. Future real-word studies are required to confirm the generalizability of these results as patients enrolled in clinical trials may differ from patients in the general population. Furthermore, data here are provided for up to 14 weeks; therefore, long-term follow-up is needed to confirm the durability of PRO improvements. Future studies may also be warranted to characterize the relationship between PROs and the achievement of improved clinical signs and symptoms.
Conclusions
Upadacitinib provides rapid and clinically meaningful improvements in HRQoL as assessed by ASQoL, ASAS HI, and SF-36 PCS, as well as work productivity, in patients with active nr-axSpA. Furthermore, clinically important improvements in HRQoL were consistently observed regardless of prior treatment with TNFis, thus providing further evidence substantiating the overarching benefit of upadacitinib in patients with active nr-axSpA. These findings, together with previously reported efficacy and safety in patients with active AS [37], provide further evidence for the benefit of upadacitinib across all active axSpA patients.
References
Garcia-Montoya L, Gul H, Emery P. Recent advances in ankylosing spondylitis: understanding the disease and management. F1000Res. 2018;7(F1000 Faculty Rev):1512
Richard N, Haroon N, Tomlinson GA, et al. FRI0208 Ankylosing spondylitis quality of life: defining minimal clinically important change. Ann Rheum Dis. 2018;77(Suppl 2):645.
Sieper J, Poddubnyy D. Axial spondyloarthritis. Lancet. 2017;390(10089):73–84.
Baraliakos X, Braun J. Non-radiographic axial spondyloarthritis and ankylosing spondylitis: what are the similarities and differences? RMD Open. 2015;1(Suppl 1): e000053.
Rudwaleit M, van der Heijde D, Landewé R, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68(6):777–83.
Poddubnyy D, Sieper J. Similarities and differences between nonradiographic and radiographic axial spondyloarthritis: a clinical, epidemiological and therapeutic assessment. Curr Opin Rheumatol. 2014;26(4):377–83.
López-Medina C, Ramiro S, van der Heijde D, et al. Characteristics and burden of disease in patients with radiographic and non-radiographic axial spondyloarthritis: a comparison by systematic literature review and meta-analysis. RMD Open. 2019;5(2): e001108.
Robinson PC, Sengupta R, Siebert S. Non-radiographic axial spondyloarthritis (nr-axSpA): advances in classification, imaging and therapy. Rheumatol Ther. 2019;6(2):165–77.
Nikiphorou E, Ramiro S, van der Heijde D, et al. Association of comorbidities in spondyloarthritis with poor function, work disability, and quality of life: results from the Assessment of SpondyloArthritis International Society Comorbidities in Spondyloarthritis Study. Arthritis Care Res (Hoboken). 2018;70(8):1257–62.
Mease PJ, Heijde DV, Karki C, et al. Characterization of patients with ankylosing spondylitis and nonradiographic axial spondyloarthritis in the US-Based Corrona Registry. Arthritis Care Res (Hoboken). 2018;70(11):1661–70.
Kiltz U, Essers I, Hiligsmann M, et al. Which aspects of health are most important for patients with spondyloarthritis? A Best Worst Scaling based on the ASAS Health Index. Rheumatology (Oxford). 2016;55(10):1771–6.
Walsh JA, Song X, Kim G, Park Y. Healthcare utilization and direct costs in patients with ankylosing spondylitis using a large US administrative claims database. Rheumatol Ther. 2018;5(2):463–74.
Kiltz U, Baraliakos X, Karakostas P, et al. Do patients with non-radiographic axial spondylarthritis differ from patients with ankylosing spondylitis? Arthritis Care Res (Hoboken). 2012;64(9):1415–22.
van der Heijde D, Ramiro S, Landewé R, et al. 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis. 2017;76(6):978–91.
Ward MM, Deodhar A, Gensler LS, et al. 2019 update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network recommendations for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritis. Arthritis Care Res. 2019;71(10):1285–99.
Ramiro S, Nikiphorou E, Sepriano A et al. ASAS-EULAR recommendations for the management of axial spondyloarthritis: 2022 update. Ann Rheum Dis 2023;82(1):19–34.
Deodhar A, Van den Bosch F, Poddubnyy D, et al. Upadacitinib for the treatment of active non-radiographic axial spondyloarthritis (SELECT-AXIS 2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2022;400(10349):369–79.
van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984;27(4):361–8.
Doward LC, Spoorenberg A, Cook SA, et al. Development of the ASQoL: a quality of life instrument specific to ankylosing spondylitis. Ann Rheum Dis. 2003;62(1):20–6.
Kiltz U, van der Heijde D, Boonen A, et al. Development of a health index in patients with ankylosing spondylitis (ASAS HI): final result of a global initiative based on the ICF guided by ASAS. Ann Rheum Dis. 2015;74(5):830–5.
Braun J, Brandt J, Listing J, et al. Treatment of active ankylosing spondylitis with infliximab: a randomised controlled multicentre trial. Lancet. 2002;359(9313):1187–93.
Reilly MC, Gooch KL, Wong RL, Kupper H, van der Heijde D. Validity, reliability and responsiveness of the Work Productivity and Activity Impairment Questionnaire in ankylosing spondylitis. Rheumatology (Oxford). 2010;49(4):812–9.
Kiltz U, van der Heijde D, Boonen A, et al. Measurement properties of the ASAS Health Index: results of a global study in patients with axial and peripheral spondyloarthritis. Ann Rheum Dis. 2018;77(9):1311–7.
Strand V, Boers M, Idzerda L, et al. It’s good to feel better but it’s better to feel good and even better to feel good as soon as possible for as long as possible. Response criteria and the importance of change at OMERACT 10. J Rheumatol. 2011;38(8):1720–7.
Siwek J, Newman DH. Introducing medicine by the numbers: A collaboration of The NNT Group and AFP. Am Fam Physician. 2015;91(7):434–5.
Strand V, Singh JA. Patient burden of axial spondyloarthritis. J Clin Rheumatol. 2017;23(7):383–91.
Kishimoto M, Ono K, Fukui S, et al. Clinical characteristics of non-radiographic versus radiographic axial spondyloarthritis in Asia and non-radiographic axial spondyloarthritis in other regions: results of the cross-sectional ASAS-COMOSPA study. RMD Open. 2021;7(3): e001752.
Deodhar A, Mease P, Rahman P, et al. Ixekizumab improves patient-reported outcomes in non-radiographic axial spondyloarthritis: results from the Coast-X trial. Rheumatol Ther. 2021;8(1):135–50.
Walsh JA, Magrey MN, Baraliakos X, et al. Improvement of functioning and health with ixekizumab in the treatment of active nonradiographic axial spondyloarthritis in a 52-week, randomized, controlled trial. Arthritis Care Res (Hoboken). 2022;74(3):451–60.
van der Heijde D, Joshi A, Pangan AL, et al. ASAS40 and ASDAS clinical responses in the ABILITY-1 clinical trial translate to meaningful improvements in physical function, health-related quality of life and work productivity in patients with non-radiographic axial spondyloarthritis. Rheumatology (Oxford). 2016;55(1):80–8.
Sieper J, Kivitz A, van Tubergen A, et al. Long-term maintenance of improvements in patient-reported outcomes with certolizumab pegol in patients with axial spondyloarthritis, including ankylosing spondylitis and non-radiographic axial spondyloarthritis: 96-week results of the RAPID-axSpA study. Value Health. 2014;17(7):A385–6.
Sieper J, van der Heijde D, Dougados M, et al. A randomized, double-blind, placebo-controlled, sixteen-week study of subcutaneous golimumab in patients with active nonradiographic axial spondyloarthritis. Arthritis Rheumatol. 2015;67(10):2702–12.
Mease P, Walsh JA, Baraliakos X, et al. Translating improvements with ixekizumab in clinical trial outcomes into clinical practice: ASAS40, pain, fatigue, and sleep in ankylosing spondylitis. Rheumatol Ther. 2019;6(3):435–50.
Stebbings SM, Treharne GJ, Jenks K, Highton J. Fatigue in patients with spondyloarthritis associates with disease activity, quality of life and inflammatory bowel symptoms. Clin Rheumatol. 2014;33(10):1467–74.
Dougados M, van der Heijde D, Tsai WC, et al. Relationship between disease activity status or clinical response and patient-reported outcomes in patients with non-radiographic axial spondyloarthritis: 104-week results from the randomized controlled EMBARK study. Health Qual Life Outcomes. 2020;18(1):4.
van der Heijde D, Cheng-Chung Wei J, Dougados M, et al. Ixekizumab, an interleukin-17A antagonist in the treatment of ankylosing spondylitis or radiographic axial spondyloarthritis in patients previously untreated with biological disease-modifying anti-rheumatic drugs (COAST-V): 16 week results of a phase 3 randomised, double-blind, active-controlled and placebo-controlled trial. Lancet. 2018;392(10163):2441–51.
van der Heijde D, Baraliakos X, Sieper J, et al. Efficacy and safety of upadacitinib for active ankylosing spondylitis refractory to biological therapy: a double-blind, randomised, placebo-controlled phase 3 trial. Ann Rheum Dis. 2022;81(11):1515–23.
Acknowledgements
We thank the participants of the study.
Funding
This work was supported by AbbVie, including the Rapid Service Fee. AbbVie sponsored the study and participated in the interpretation of data, review, and approval of the manuscript. All authors contributed to the development of the manuscript and maintained control over the final content. No honoraria or payments were made for authorship.
Author Contributions
All authors (Uta Kiltz, Mitsumasa Kishimoto, Jessica A. Walsh, Percival Sampaio-Barros, Manish Mittal, Christopher D. Saffore, Peter Wung, Fabiana Ganz, Ana Biljan, Denis Poddubnyy) contributed to the conception and design of the research, interpretation of the data, and writing and critical revision of the manuscript; agreed to be fully accountable for ensuring the integrity and accuracy of the work; and read and approved the final manuscript.
Medical Writing, Editorial, and Other Assistance
Medical writing assistance was provided by Brandy Menges, PhD, of Fishawack Facilitate Ltd., part of Fishawack Health, and was funded by AbbVie Inc., North Chicago, IL.
Disclosures
Uta Kiltz: received grant and research support and consultancy fees from AbbVie, Amgen, Biocad, Biogen, Chugai, Eli Lilly, Fresenius, Gilead, Grünenthal, GSK, Hexal, Janssen, MSD, Novartis, onkowoessen.de, Pfizer, Roche, UCB, and Viatris. Mitsumasa Kishimoto: Consulting fees and/or honoraria from AbbVie, Amgen, Asahi-Kasei Pharma, Astellas, Ayumi Pharma, BMS, Celgene, Chugai, Daiichi-Sankyo, Eisai, Eli Lilly, Gilead, Janssen, Novartis, Ono Pharma, Pfizer, Tanabe-Mitsubishi, and UCB Pharma. Jessica A Walsh: Consultant: UBC, Lilly, Janssen, Novartis, Pfizer, Amgen, AbbVie. Grants: AbbVie, Pfizer, and Merck. Percival Sampaio-Barros: received speaker and/or consultancy fees from AbbVie, Janssen, Lilly, Novartis, Pfizer, and UCB. Manish Mittal, Christopher D Saffore, Peter Wung, Fabiana Ganz, and Ana Biljan are employees of AbbVie and may hold stock or stock options. Denis Poddubnyy: Research support from: AbbVie, Eli Lilly, MSD, Novartis, Pfizer; consulting fees from: AbbVie, Biocad, Eli Lilly, Galapagos, Gilead, GlaxoSmithKline, Janssen, MSD, Moonlake, Novartis, Pfizer, Samsung Bioepis, and UCB; speaker fees from: AbbVie, Bristol Myers Squibb, Eli Lilly, Janssen, MSD, Medscape, Novartis, Peervoice, Pfizer, and UCB.
Compliance with Ethics Guidelines
The SELECT-AXIS 2 trial was conducted in compliance with the International Conference on Harmonization guidelines, local regulations and guidelines governing clinical study conduct, and the ethical principles of the Declaration of Helsinki. As per Good Clinical Practice, the protocol was approved by an ethics committee or institutional review board at all study sites. All patients provided informed consent before study participation.
Data Availability
AbbVie is committed to responsible data sharing regarding the clinical trials we sponsor. This includes access to anonymized, individual, and trial-level data (analysis data sets), as well as other information (e.g., protocols, clinical study reports, or analysis plans), as long as the trials are not part of an ongoing or planned regulatory submission. This includes requests for clinical trial data for unlicensed products and indications. These clinical trial data can be requested by any qualified researchers who engage in rigorous, independent, scientific research, and will be provided following review and approval of a research proposal, Statistical Analysis Plan (SAP), and execution of a Data Sharing Agreement (DSA). Data requests can be submitted at any time after approval in the United States and Europe and after acceptance of this manuscript for publication. The data will be accessible for 12 months, with possible extensions considered. For more information on the process or to submit a request, visit the following link: https://www.abbvie.com/our-science/clinical-trials/clinical-trials-data-and-information-sharing/data-and-information-sharing-with-qualified-researchers.html.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kiltz, U., Kishimoto, M., Walsh, J.A. et al. Effect of Upadacitinib on Quality of Life and Work Productivity in Active Non-radiographic Axial Spondyloarthritis: Results From Randomized Phase 3 Trial SELECT-AXIS 2. Rheumatol Ther 10, 887–899 (2023). https://doi.org/10.1007/s40744-023-00550-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-023-00550-4