Abstract
Introduction
Glucocorticoids (GC) are currently recommended as a bridging therapy in combination with conventional synthetic disease-modifying anti-rheumatic drugs (csDMARD) for the treatment of rheumatoid arthritis (RA) and should be tapered as rapidly as clinically feasible. We aimed to explore potential predictors for GC discontinuation in patients commencing GC with concomitant csDMARD.
Methods
We used data from a longitudinal real-world cohort. RA patients who newly started GC concomitantly with csDMARD were included. All patients were divided into four groups, according to degree of change in disease activity at 3 months from baseline (group 1: worsening or no decrease; group 2: 0–24.9% decrease; group 3: 25.0–49.9% decrease; group 4: ≥ 50.0% decrease). Cox regression was used to estimate hazard risk (HR) with 95% confidence interval (CI).
Results
In total, 124 out of 207 RA patients discontinued GC at the rheumatologist's discretion and 79.1% (91/115) of them successfully stopping GC without flare within 6 months after GC withdrawal. Increasing age (HR 0.99, 95% CI 0.98–1.00, p = 0.043) and concomitant nonsteroidal anti-inflammatory drugs use at GC initiation (HR 0.47, 95% CI 0.25–0.88, p = 0.018) were independently associated with GC withdrawal failure. Moreover, the degrees of disease activity improvement at 3 months significantly predicted the possibility of subsequent GC discontinuation (fully adjusted HR 1.35–1.47, p < 0.01), with 2.38–3.59 times higher in group 4 than group 1. Switching the outcome to successfully stopping GC without short-term flare yielded similar findings.
Conclusions
The degrees of disease activity improvement at 3 months independently predicted the subsequent GC withdrawal. These findings suggest the importance of dynamic treatment strategies with a closer look at disease activity during GC tapering and discontinuation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Glucocorticoids (GC) are currently recommended as a bridging therapy in combination with conventional synthetic disease-modifying anti-rheumatic drugs (csDMARD) and should be tapered as rapidly as clinically feasible for rheumatoid arthritis (RA). |
To date, the risk profiles for failure of GC discontinuation, in a real-life setting, is scarcely reported in RA patients, leaving a huge knowledge gap. |
What was learned from this study? |
In RA patients initiating GC and concomitant csDMARD, the degrees of disease activity improvement at 3 months or week 6 independently predicted the subsequent GC withdrawal. |
Increasing age and concomitant use of nonsteroidal anti-inflammatory drugs at GC initiation were risk factors for GC withdrawal failure. |
These findings suggest the importance of dynamic treatment strategies with a closer look at disease activity and shed light on individualized precision strategy for GC discontinuation. |
Introduction
Since the first identification in 1948, glucocorticoids (GC) have played important roles in the management of rheumatoid arthritis (RA) although some controversy remains [1,2,3,4,5]. This is due to its advantage of a rapid onset of action on one hand and well-documented disease-modifying effects on the other [6, 7]. In daily practice, about half of RA patients received GC therapy in US and Europe [8,9,10]. In developing countries, GC appears to be more universally used because of being cheap, easy to access, and often without a prescription [6]. However, the gradually increasing safety concerns of GC long-term exposure, even at low dose, leads to lot of debates on the GC usage in RA [8,9,10,11,12]. Prolonged use of GC is indeed common in routine practice due to the complicated clinical scenarios and absence of evidence-based tapering protocol.
In the European League Against Rheumatism (EULAR) recommendations for the management of RA, GC has long been recommended as a part of therapy, concomitantly with conventional synthetic disease-modifying anti-rheumatic drug (csDMARD) and should be stopped as rapidly as clinically feasible, ideally within 3–6 months [3, 4]. GC co-therapy with csDMARD is considered a failure if GC cannot be withdrawn within an acceptable time frame, and a biological or targeted synthetic DMARD (b/tsDMARD) should be added [3, 4]. In our previous research, about 60% of patients who newly started GC concomitantly with csDMARD finally discontinued GC during a median follow-up of 38.6 months in real-world setting [13]. This also implies GC withdrawal is not reachable in over one-third of RA patients who received GC co-therapy with csDMARD in day-to-day practice. In this regard, unravelling the risk factors for GC discontinuation failure is urgent and significant. Therefore, we aimed to explore predictors of GC discontinuation in RA patients commencing GC with concomitant csDMARD in real-world practice.
Methods
Study Design and Participants
This study is a retrospective analysis of prospectively collected data from Treat-to-TARget in RA (TARRA) cohort of RA patients. The cohort, first established over a decade ago, is a monocentric longitudinal cohort and has been described in greater detail in our previous research [13,14,15,16,17,18,19]. Briefly, demographics, symptom duration, RA core variables, and treatment details were collected at the first visit. After that, all participants are prospectively followed up and documented at least every 3 months for those in moderate/high diseases activity and every 3–12 months (usually 3–6 months) for those in remission/low disease activity (LDA). Extra follow-up is scheduled besides those at regular intervals to satisfy clinical needs. The treatment decisions at each visit are made at the discretion of attending physicians based on disease activity heading for clinical remission. The TARRA cohort was approved by the Institutional Review Board (IRB) of our hospital and the participants provided informed consent to participate in this study (IRB number 2014-785).
All patients in the TARRA cohort fulfilled the 1987 American College of Rheumatology (ACR) classification criteria [20] or 2010 ACR/EULAR classification criteria for RA [21]. The inclusion criteria included: (1) visited the outpatient clinic between January 2009 and December 2019; (2) initiated GC with concomitant csDMARD therapy at the initial visit to our clinic; (3) had over 1-year follow-up with at least three visits. The exclusion criteria were as follows: (1) GC was used for comorbidities other than RA; (2) having another disease (e.g., polymyalgia rheumatica, systemic lupus erythematosus) or certain condition (e.g., pregnancy, lactation) that might influence GC tapering; (3) concomitant use of b/tsDMARD at the initiation of GC and csDMARD.
Clinical Assessment and Definitions
The data of each eligible participant were collected from the timepoint of commencing GC treatment to December 2020. The collected data included (1) demographics: sex, age; (2) clinical features of RA: disease duration, tender joint count (TJC), swollen joint count (SJC), titers of rheumatoid factor (RF) and anti-cyclic citrullinated peptides (anti-CCP), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), patient’s global assessment (PGA), evaluator’s global assessment (EGA); (3) treatment details at each visit (GC; methotrexate (MTX); leflunomide (LEF); hydroxychloroquine (HCQ); sulfasalazine (SSZ); Tripterygium wilfordii Hook F (TII); nonsteroidal anti-inflammatory drugs (NSAIDs)).
A patient who never received DMARD or was on DMARD treatment for less than 3 months at the initiation of GC was defined as a DMARD-naive patient. Certain inflammatory markers are strongly influenced by GC use, tapering steroids might limit improvement in inflammatory markers. To avoid biases induced by single diseases activity index, the levels of disease activity at each visit was measured by disease activity score based on 28-joint count and ESR (DAS28-ESR) [22], simplified disease activity index (SDAI) [23], and clinical disease activity index (CDAI) [24].
Study Outcomes
Similar study methods have been used in a previous study: https://ard.bmj.com/content/80/8/997 [11]. Patients were categorized into two groups according to whether they discontinued GC during the period of follow-up: discontinued group and continued group. The prescribed GC dosage was checked at each visit and converted to prednisolone (PSL) equivalent dose. The decision of tapering or discontinuing GC was made by the treating rheumatologist. Discontinuation of GC in a patient at discretion of treating physician during follow-up was regarded as GC discontinuation, and discontinuation without disease flare within 6 months after GC withdrawal was regarded as successful discontinuation. Disease flare in this study was defined if one of the following criteria was satisfied after 6 months of GC withdrawal: (1) increasing DAS28 beyond 0.60; (2) GC re-initiation; (3) DMARD added or increment. Adding of any b/tsDMARD for the purpose of facilitating GC tapering during follow-up was regarded as failure of GC discontinuation in the context of csDMARD, and the data before b/tsDMARD initiation were analyzed.
The primary outcome was the predictors for GC discontinuation in RA patients who newly started GC co-therapy with csDMARD. The secondary analysis was conducted for predictors for successful GC discontinuation. Immortal time bias is a critical issue in epidemiological studies because the outcome cannot occur for a certain time span. In this study, RA patients who newly started GC concomitantly with csDMARD were included for the outcomes of GC discontinuation, instead of GC adverse event and immortal time bias therefore is minimized.
Statistical Analysis
Patient characteristics were presented as mean (SD) or median and interquartile range (IQR) depending on the level of resemblance to the normal distribution. Absolute and relative frequencies were reported for categorical variables. Remission rates were measured by aforementioned definitions, reported as percentages with 95% confidence interval (95% CI). The trends of PSL dose, disease activity, and remission rate in discontinued and continued groups were analyzed using generalized estimating equations with an unstructured working correlation matrix and a robust estimation for the covariance matrix. The comparisons of clinical characteristics and treatment profiles between the discontinued group and continued group were analyzed by Student’s t tests for normally distributed continuous variables, Mann–Whitney U tests for skewed continuous variables, and chi-square tests for categorical variables. The log-rank test was used to analyze the differences between the survival curves of patients with different clinical characteristics. Univariate and multivariate analysis with enter method was performed to determine the hazard risk (HR) with 95% CI for predictive factors based on a Cox proportional hazards regression model. Variables with p values of < 0.1 in the univariate analysis, clinically important variables (e.g., age, DAS), and the predictors of GC discontinuation suggested in past reports were included in the multivariate Cox analysis. P values < 0.05 were considered statistically significant. All the analyses were done by SPSS v.20.0.
Results
Baseline Characteristics Between Discontinued and Continued Groups
As we previously presented, 124 out of 207 (59.9%) patients finally discontinued GC at the discretion of treating rheumatologist during a median (IQR) follow-up of 38.6 (20.7–60.3) months. For the 124 patients who discontinued GC, the median time (IQR) to GC cessation was 13.6 (8.0–24.6) months, ranging from 3.1 to 77.6 months. Compared with patients who discontinued GC, patients in the continued group were more frequently treated with concomitant NSAIDs (19.3 vs. 8.9%, p = 0.024) (Tables 1, 2, Supplementary Material Figure S1). Multivariate Cox analysis among age, disease activity, concomitant NSAIDs use, and initiating PSL dose revealed increasing age (HR 0.99, 95% CI 0.98–1.00, p = 0.043) and concomitant NSAIDs usage at GC initiation (HR 0.47, 95% CI 0.25–0.88, p = 0.018) were independent risk factors for of GC discontinuation failure (Table 2).
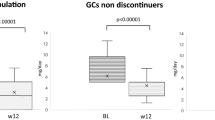
Changes in PSL Daily Dose and Disease Activity Over Course Between Discontinued and Continued Groups
We further compared the changes in PSL dose and disease activity in the first 36 months after GC initiation between the discontinued and continued groups (Fig. 1). At baseline of GC initiation, the median PSL dose and disease activity were well balanced between the two groups. In general, the median PSL dose was significantly decreased with time in either the discontinued or continued group (p < 0.001) (Fig. 1A). Notably, the median PSL dose was significantly lower in the discontinued group than in the continued group as early as month 3 (p < 0.001). In relation to disease control, the median disease activity, measured by DAS28, SDAI, and CDAI, was markedly reduced in the first year and then fluctuated afterwards. Similarly, the median DAS28, SDAI, and CDAI in the discontinued group were significantly lower than that in the continued group at all follow-up time points, including as early as month 3 (Fig. 1B–D).
Change in Disease Activity at Month 3 and Subsequent GC Discontinuation
Considering sophisticated and dynamic aspects of GC discontinuation in real-world practice, we explored whether the reduction in disease activity at month 3 could predict subsequent GC discontinuation. Initially, all patients were divided into four groups according to the levels of disease activity change from baseline to month 3: worsening or no improvement (≤ 0%, group 1), slight improvement (0.1–24.9%, group 2), moderate improvement (25.0–49.9%, group 3) and substantial improvement (≥ 50.0%, group 4). Regarding CDAI, the likelihood of subsequent discontinuation of GC was increased by 48% with increasing one degree of improvement at month 3 (e.g., group 3 vs. group 2) (Table 3). After adjustment for age, baseline DAS, initial PSL dose, NSAIDs use, and PSL dose reduction at month 3, 47% increased likelihood of GC discontinuation was detected with one degree increases of CDAI improvement and patients in group 2, 3 and 4 had 1.77, 1.98 and 3.23 times more likely to discontinue GC respectively, compared with patients in group 1 (p for trend < 0.001). Similar findings were detected in both SDAI and DAS28 changes at month 3 (Table 3).
Change in Disease Activity at Week 6 and Subsequent GC Discontinuation
Of 130 patients with DAS changes document at week 6, we divided them into three groups according to the levels of disease activity change from baseline to week 6: worsening or no improvement (≤ 0%, group 1), slight or moderate improvement (0.1–49.9%, group 2), substantial improvement (≥ 50.0%, group 3). Regarding DAS28, patients in groups 2 and 3 had 2.11 and 2.72 times more likely to discontinue GC respectively, compared with patients in group 1 (p for trend = 0.015) in fully adjusted model (Table 4). Similar trends were observed in terms of SDAI and CDAI although not reaching significance.
Secondary Analysis: Predictors for Successful GC Discontinuation
In 124 patients who stopped GC, clinical data and follow-up information in 6 months after GC cessation were available in 115 patients, including 91 patients with successful GC discontinuation. In the comparison between successful GC discontinuation and continued groups, multivariate Cox analysis showed increasing age with HR of 0.99 (p = 0.048) and concomitant NSAIDs usage at GC initiation with HR 0.529, p = 0.063).
Similarly, all patients were divided into four groups according to the levels of disease activity from baseline to month 3: worsening or no improvement (≤ 0%, group 1), slight improvement (0.1–24.9%, group 2), moderate improvement (25.0–49.9%, group 3) and substantial improvement (≥ 50.0%, group 4). RegradingDAS28, patients in groups 2, 3, and 4 were 2.81, 4.75, and 5.01 times more likely to successfully discontinue GC, compared with patients in group 1 in fully adjusted model (Table 5). Similar findings were detected for CDAI and SDAI regarding the outcome of successful GC discontinuation.
Discussion
GC, a universally used anti-inflammatory and immunosuppressive drug, has been recommended to co-administrate with csDMARD for either early or long-standing RA in current guidelines [2, 3, 6]. Studies of effectiveness and safety of short-term GC co-therapy with csDMARD in RA have demonstrated its unique place in the era of modern rheumatology [5]. To allay both patient and rheumatologist concerns about GC-related adverse effects, it is critical to stop GC as rapidly as clinically feasible after commencing GC with concomitant DMARD and elicit a b/tsDMARD to facilitate GC discontinuation if clinically necessary. In our previous research, about 40% of patients who newly started GC concomitantly with csDMARD failed to discontinue GC in a real-world setting [13]. In Tokyo University Biologics Registry for RA with 80 patients taking a median PSL dose of 5.0 (1.0–10.0) mg/day at bDMARD initiation, higher DAS28 (HR 0.200; p = 0.039) and higher PSL dose (HR 0.748; p = 0.029) at baseline were significantly associated with less frequent GC discontinuation [25]. Most recently, based on protocolized discontinuation of GC in two trials, about 40% of patients experienced loss of disease control despite continuation of csDMARD and a lower DAS both at baseline and stop visit was associated with successful discontinuation in patients with in patients with early RA and undifferentiated arthritis [26]. Risk factors for GC cessation failure in the context of csDMARD, to date, remain completely unknown in real-world setting.
In the present study, we found that increasing age and concomitant NSAIDs usage at GC initiation were significantly related to subsequent failure of GC cessation in the context of csDMARD. Furthermore, the decrement levels of disease activity at month 3 or week 6, but not the baseline levels, strongly predicted the subsequent GC discontinuation. In general, GC should be discontinued as rapidly as clinically feasible when the treatment target is achieved. Accumulative evidence has confirmed that RA patients with increasing age had poor therapeutic response, lower possibility to achieve treatment target (e.g., clinical remission, sustained clinical remission), and consequently decreased chance of GC discontinuation [17, 27, 28]. In addition to GC, NSAIDs are effective in controlling inflammation of RA. There are several possible explanations that could account for the association between concomitant NSAIDs use and low probability of GC discontinuation. On one hand, in clinical scenarios, the combination of GC with NSAIDs is not frequently seen in daily practice. Co-administration of NSAIDs besides GC, to a large extent, indicates the severity of joint and/or systemic inflammation and the treating rheumatologist may be more inclined to control the inflammation more aggressively with prolong treatment period of GC in routine clinical practice. On the other hand, narcotics usage is strictly regulated in China, which is conditionally used for cancer pain in China. By contrast, NSAIDs are easily accessible in daily practice, which is frequently used for the purpose of controlling joint pain. Patients with requirement of GC and NSAIDs combination may be more prone to representing a specific phenotype that comprises predominant pain, fatigue, and unsatisfactory patient-reported outcomes even after adequate control of the inflammation.
In fact, persistent central sensitization and the development of maladaptive pain processing are attributable to the specific phenotype [29]. In addition, even though we adjusted for other factors, potential unmeasured confounders, which are differentially distributed among patients receiving concomitant NSAIDs, may partially explain the link between concomitant NSAIDs therapy and GC discontinuation failure (e.g., the presence of osteoarthritis). Moreover, the decrement levels of disease activity at month 3 and week 6 positively and strongly predicted the subsequent GC discontinuation. These findings shed light on individualized precision strategy for GC discontinuation on one hand, and avoidance of long-term GC exposure and promotion of timely b/tsDMARD initiation for specific patients on the other. According to our findings, advanced therapies of b/tsDMARD may be considered early in patients who fail to reach acceptable disease activity improvements (e.g., < 25%) in the first 3 months of therapy, especially those with advanced age, or concomitant NSAIDs use. Taken together, the findings underline that dynamic treatment strategies with a closer look at disease activity at 6 weeks and 3 months in RA patients is necessary in real-life settings.
We acknowledge the limitations existing in this study. First, single-center design may hamper the generalization of the conclusions to different geographical and ethnic groups. For example, TII was officially approved for the treatment of RA in China. However, this agent is not commonly accessible in other regions. Further prospective cohort studies are warranted to prove the findings in other ethnic groups and regions in the future. Second, the limited sample size of our study warrants further research. Nevertheless, no studies to date are currently available that explore the predictive factors for GC discontinuation in RA patients who newly started GC concomitantly with csDMARD in real-world practice. For the first time, this study attempted to generate knowledge regradingGC discontinuation in the context of csDMARD. Last, despite extensive adjustment for potential confounders performed, residual confounding from these factors, or confounding from other unmeasured factors, cannot be fully ruled out. For example, dermal joint temperature was not assessed in our study, which could quickly and accurately identify individual RA patients at high risk for radiographic damage [30].
Conclusions
In summary, increasing age, concomitant NSAIDs usage, and the decrement levels of disease activity at month 3 or week 6 independently predict the subsequent GC withdrawal. This suggests that dynamic treatment strategies with a closer look at disease activity at 6 weeks and 3 months in RA patients is decidedly warranted to achieve GC discontinuation in a real-life setting.
References
Conn DL. The story behind the use of glucocorticoids in the treatment of rheumatoid arthritis. Semin Arthritis Rheum. 2020;51(1):15–9. https://doi.org/10.1016/j.semarthrit.2020.09.016.
Buttgereit F. Views on glucocorticoid therapy in rheumatology: the age of convergence. Nat Rev Rheumatol. 2020;16(4):239–46. https://doi.org/10.1038/s41584-020-0370-z.
Smolen JS, Landewé RBM, Bijlsma JWJ, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79(6):685–99. https://doi.org/10.1136/annrheumdis-2019-216655.
Smolen JS, Landewé R, Bijlsma J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis. 2017;76(6):960–77. https://doi.org/10.1136/annrheumdis-2016-210715.
Hetland ML, Haavardsholm EA, Rudin A, et al. Active conventional treatment and three different biological treatments in early rheumatoid arthritis: phase IV investigator initiated, randomised, observer blinded clinical trial. BMJ. 2020;371: m4328. https://doi.org/10.1136/bmj.m4328.
Hoes JN, Jacobs JW, Buttgereit F, Bijlsma JW. Current view of glucocorticoid co-therapy with DMARD in rheumatoid arthritis. Nat Rev Rheumatol. 2010;6(12):693–702. https://doi.org/10.1038/nrrheum.2010.179.
Baschant U, Lane NE, Tuckermann J. The multiple facets of glucocorticoid action in rheumatoid arthritis. Nat Rev Rheumatol. 2012;8(11):645–55. https://doi.org/10.1038/nrrheum.2012.166.
Ocon AJ, Reed G, Pappas DA, Curtis JR, Kremer JM. Short-term dose and duration-dependent glucocorticoid risk for cardiovascular events in glucocorticoid-naive patients with rheumatoid arthritis. Ann Rheum Dis. 2021;80(12):1522–1529. https://doi.org/10.1136/annrheumdis-2021-220577.
Roubille C, Coffy A, Rincheval N, et al. Ten-year analysis of the risk of severe outcomes related to low-dose glucocorticoids in early rheumatoid arthritis. Rheumatology (Oxford). 2021;60(8):3738–3746. https://doi.org/10.1093/rheumatology/keaa850.
George MD, Baker JF, Winthrop K, et al. Risk for serious infection with low-dose glucocorticoids in patients with rheumatoid arthritis: a cohort study. Ann Intern Med. 2020;173(11):870–8. https://doi.org/10.7326/M20-1594.
Xie W, Yang X, Ji L, Zhang Z. Incident diabetes associated with hydroxychloroquine, methotrexate, biologics and glucocorticoids in rheumatoid arthritis: a systematic review and meta-analysis. Semin Arthritis Rheum. 2020;50(4):598–607. https://doi.org/10.1016/j.semarthrit.2020.04.005.
Abtahi S, Driessen JHM, Burden AM, et al. Concomitant use of oral glucocorticoids and proton pump inhibitors and risk of osteoporotic fractures among patients with rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis. 2021;80(4):423–431. https://doi.org/10.1136/annrheumdis-2020-218758.
Xie W, Huang H, Li G, et al. Dynamical trajectory of glucocorticoids tapering and discontinuation in patients with rheumatoid arthritis commencing glucocorticoids with csDMARD: a real-world data from 2009 to 2020. Ann Rheum Dis. 2021;80(8):997–1003. https://doi.org/10.1136/annrheumdis-2021-220112.
Xie W, Li G, Huang H, Zhang Z. How to define Boolean low disease activity in rheumatoid arthritis: experience from a large real-world cohort. Rheumatol Ther. 2021;8(1):289–301. https://doi.org/10.1007/s40744-020-00270-z.
Ji L, Xie W, Li G, Zhang Z. Maintenance to target was associated with radiological outcomes in patients with rheumatoid arthritis: a real-world observational cohort study. Clin Rheumatol. 2021;40(4):1307–15. https://doi.org/10.1007/s10067-020-05385-w.
Xie W, Li J, Zhang Z. The impact of different criteria sets on early remission and identifying its predictors in rheumatoid arthritis: results from an observational cohort (2009–2018). Clin Rheumatol. 2020;39(2):381–9. https://doi.org/10.1007/s10067-019-04807-8.
Xie W, Li J, Zhang X, Sun X, Zhang Z. Sustained clinical remission of rheumatoid arthritis and its predictive factors in an unselected adult Chinese population from 2009 to 2018. Int J Rheum Dis. 2019;22(9):1670–8. https://doi.org/10.1111/1756-185X.13651.
Xie W, Li J, Zhang X, Li G, Hao Y, Zhao J, Wang L, Sun X, Fan Y, Zhang Z. Trends in the activity of rheumatoid arthritis as the consequence of treat-to-target strategy: eight-year data from 2009 to 2016. Clin Exp Rheumatol. 2018;36(5):820–8.
Zhang H, Zhang H, Gao D, Xie W, Geng Y, Zhang Z. Overlapping Sjogren’s syndrome reduces the probability of reaching target in rheumatoid arthritis patients: a propensity score matched real-world cohort from 2009 to 2019. Arthritis Res Ther. 2020;22(1):100.
Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315–24. https://doi.org/10.1002/art.1780310302.
Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69(9):1580–8. https://doi.org/10.1136/ard.2010.138461.
Fransen J, Creemers MC, Van Riel PL. Remission in rheumatoid arthritis: agreement of the disease activity score (DAS28) with the ARA preliminary remission criteria. Rheumatology (Oxford). 2004;43(10):1252–5.
Smolen JS, Breedveld FC, Schiff MH, et al. A Simplified Disease Activity Index for rheumatoid arthritis for use in clinical practice. Rheumatology (Oxford). 2003;42(2):244–57.
Aletaha D, Nell VP, Stamm T, et al. Acute phase reactants add little to composite disease activity indices for rheumatoid arthritis: validation of a clinical activity score. Arthritis Res Ther. 2005;7(4):R796–806.
Inoue M, Kanda H, Tateishi S, Fujio K. Factors associated with discontinuation of glucocorticoids after starting biological disease-modifying antirheumatic drugs in rheumatoid arthritis patients. Mod Rheumatol. 2020;30(1):58–63. https://doi.org/10.1080/14397595.2018.1553264.
Maassen JM, Dos Santos SR, Bergstra SA, et al. Glucocorticoid discontinuation in patients with early rheumatoid and undifferentiated arthritis: a post-hoc analysis of the BeSt and IMPROVED studies. Ann Rheum Dis. 2021;80(9):1124–1129. https://doi.org/10.1136/annrheumdis-2021-220403.
Smolen JS, Szumski A, Koenig AS, Jones TV, Marshall L. Predictors of remission with etanercept-methotrexate induction therapy and loss of remission with etanercept maintenance, reduction, or withdrawal in moderately active rheumatoid arthritis: results of the PRESERVE trial. Arthritis Res Ther. 2018;20(1):8. https://doi.org/10.1186/s13075-017-1484-9.
Schipper LG, Fransen J, den Broeder AA, Van Riel PL. Time to achieve remission determines time to be in remission. Arthritis Res Ther. 2010;12(3):R97. https://doi.org/10.1186/ar3027.
Buch MH, Eyre S, McGonagle D. Persistent inflammatory and non-inflammatory mechanisms in refractory rheumatoid arthritis. Nat Rev Rheumatol. 2021;17(1):17–33. https://doi.org/10.1038/s41584-020-00541-7.
Greenwald M, Ball J, Guerrettaz K, Paulus H. Using dermal temperature to identify rheumatoid arthritis patients with radiologic progressive disease in less than one minute. Arthritis Care Res (Hoboken). 2016;68(8):1201–5. https://doi.org/10.1002/acr.22813.
Acknowledgements
The authors would like to thank all the patients and rheumatology nurses who contributed to our study.
Funding
This work and the journal’s Rapid Service Fee were supported by the National Natural Science Foundation of China (Grant Number: 81771740, 81801611, 81971524).
Author Contributions
ZZ conceived of the study, participated in its design and coordination, and critically revised the manuscript. WX had full access to all of the data collection, analysis, interpretation, and drafted the manuscript. HH contributed to the process of data collection. All the authors listed have approved the enclosed manuscript.
Disclosures
Wenhui Xie has nothing to disclose; Hong Huang has nothing to disclose; Zhuoli Zhang has nothing to disclose.
Compliance with Ethics Guidelines
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This retrospective study was approved by the Institutional Review Board (IRB) of the Peking University First Hospital (IRB number 2014-785). The participants provided their written informed consent to participate in this study. Informed consent for publication was obtained from all the patients.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xie, W., Huang, H. & Zhang, Z. Dynamic Characteristics and Predictive Profile of Glucocorticoids Withdrawal in Rheumatoid Arthritis Patients Commencing Glucocorticoids with csDMARD: A Real-World Experience. Rheumatol Ther 10, 405–419 (2023). https://doi.org/10.1007/s40744-022-00527-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-022-00527-9