Abstract
Objective
We aimed to investigate the discrepancy in metabolic syndrome (MS) and cardiovascular disease (CVD) between patients with psoriatic arthritis (PsA) and those with rheumatoid arthritis (RA).
Methods
Patients with PsA and RA were enrolled between 1 December 2018 and 31 December 2021. Data on their demographics, height, weight, waist circumference, clinical and laboratory data, and comorbidities were collected. Disease activities of patients with RA and PsA were assessed. Prevalence was estimated by dividing cases (such as MS and CVD) of PsA and RA individually. Propensity score matching and inverse probability of treatment weighting were used for further validation.
Results
Consecutively, 197 patients with PsA and 279 patients with RA were enrolled in this study. Both MS [36.0% versus 23.3%, p = 0.002, OR 1.54 (1.16, 2.05)] and CVD [6.6% versus 1.1%, p = 0.001, OR 6.13 (1.77, 21.25)] were more frequently observed in patients with PsA compared with patients with RA. The frequency of abdominal obesity was also higher in patients with PsA [61.9% versus 33.0%, OR 1.87 (1.53, 2.29), p < 0.001]. After 1:1 propensity score matching for age, sex, smoking history, serum lipids, and disease activity, MS remained more common in 117 patients with PsA than in 117 patients with RA (37.6% versus 23.1%, p = 0.016) These findings remained after the inverse probability of treatment weighting in 196 patients with PsA and 288 patients with RA. A positive linear relationship between MS with disease activity was found in patients with PsA, but not in patients with RA.
Conclusion
Considerable discrepancies in MS and CVD were observed between patients with PsA and those with RA. The greater odds of MS and CVD emphasize the need to pay more attention to metabolic and cardiovascular conditions in patients with PsA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Frequencies of metabolic syndrome (MS) and cardiovascular disease (CVD) have been seldom investigated in Chinese patients with psoriatic arthritis (PsA). |
The discrepancies of MS and CVD have never been directly compared between patients with PsA and those with rheumatoid arthritis (RA) in mainland China. |
What was learned from this study? |
The results of propensity score matching and inverse probability of treatment weighting indicate that MS and CVD are more frequently observed in patients with PsA than in patients with RA, despite the influence of age, sex, smoking history, or disease activity. |
More attention should be paid to metabolic and cardiovascular conditions in patients with PsA that conform to the Treatment Guidelines of Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA). |
Introduction
Rheumatoid arthritis (RA) and psoriatic arthritis (PsA) are both autoimmune diseases characterized by inflammatory arthritis, with a prevalence of 0.5% and 0.1–0.25%, respectively [1, 2]. Extra-articular manifestations, including psoriasis psoriatic nails, uveitis, dactylitis, and enthesitis in PsA and lung disease and vasculitis in RA, can occur and indicate poor prognosis in both diseases [3, 4]
Metabolic syndrome (MS) is marked by the presence of three or more of a group of features, including impaired glucose tolerance or type 2 diabetes mellitus (T2DM), abdominal obesity, dyslipidemia, and hypertension, that are linked to increased risk of cardiovascular disease (CVD) [5]. MS is associated with chronic inflammation. The pro-inflammatory and procoagulant state caused by MS plays an important role in the development of CVD [6]. Previous studies showed an increased risk of MS both in patients with RA and in those with PsA [7, 8]. A meta-analysis of 70 studies showed MS in 14.32–37.83% of patients with RA [7], while a study by Lin et al. showed that 42% of patients with PsA had MS [9]. In addition, the risk of MS in patients with psoriasis was also increased [10]. Therefore, patients with PsA appear to be more likely to have MS than patients with RA. Both MS and inflammation have been confirmed to contribute to the development of cardiovascular disease (CVD) [6]. Compared with the general population, the risk of CVD in patients with inflammatory arthritis such as RA and PsA was markedly elevated [11].
There has been limited investigation into the discrepancy of MS and CVD between RA and PsA. Moreover, no consistent conclusions about the discrepancy of MS and CVD between RA and PsA have been reached. Research by Mok and Labitagan et al. showed the prevalence of MS and CVD in patients with PsA was higher than in patients with RA [12, 13]. However, Cooksey et al. found an opposite phenomenon [14]. Research of Ozkul and Lauper et al. revealed no significant difference in the prevalence of MS and CVD in RA and PsA [15, 16]. Importantly, none of these previous studies had attempted to control for the influence of potential confounding variables, such as age and sex, key risk factors of MS. Therefore, we designed this study with the intention of examining the discrepancy in MS and CVD between patients with RA and those with PsA, using both propensity score matching and inverse probability of treatment weighting.
Methods
Study Design
This is a cross-sectional study carried out in the rheumatology clinic of Peking University First Hospital to observe discrepancies of MS and CVD in patients with PsA and those with RA.
Participants
Consecutive patients with RA and PsA were enrolled in the rheumatology clinic of Peking University First Hospital from 1 December 2018 to 31 December 2021. All patients were over 18 years old. The patients with PsA fulfilled the Classification criteria for Psoriatic Arthritis (CASPAR), and patients with RA satisfied the 2010 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) classification criteria [17]. Patients with malignancy, infection, or rheumatic diseases other than RA or PsA were excluded from the study.
The study was approved by the institutional Research Ethics Committee, and all patients received informed consent for data collection of their medical records.
Clinical Data Collection
The following data were collected: disease duration, height, weight, waist circumference, clinical manifestations, laboratory parameters including erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), fasting blood glucose (FBG), and fasting lipid profiles. Normal ranges of these laboratory tests are presented in Supplementary Table 1. Patient’s and evaluator’s global assessments (PGA/EGA) were documented. Composite disease activity scores, including Clinical Disease Activity Index (CDAI), Simplified Disease Activity Index (SDAI), and Disease Activity Score based on 28-joint count (DAS28) for RA and Disease Activity Index for Psoriatic Arthritis (DAPSA) and Psoriasis Area and Severity Index (PASI) for PsA, were calculated. History of comorbidities including hypertension, T2DM, and cardiovascular and cerebral vascular disease were collected. MS was diagnosed according to the definitions proposed by the International Diabetes Federation (IDF). In detail, the diagnosis of MS requires the presence of at least three of the following five criteria: (1) waist circumference ≥ 85 cm in men and ≥ 80 cm in women; (2) hypertriglyceridemia with triglyceride (TG) > 150 mg/dl (1.7 mmol/L); (3) low high-density lipid, with HDL < 40 mg/dl in men (1.03 mmol/L) and < 50 mg/dl in women (1.3 mmol/L); (4) elevated blood pressure, with systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure ≥ 85 mmHg or treatment of previously diagnosed hypertension (HTN); (5) elevated FBG ≥ 100 mg/dl (5.6 mmol/L) or previously diagnosed type 2 diabetes mellitus (T2DM) [18]. In the present study, patients’ diagnosis of HTN and T2DM and history of cerebral and cardiovascular diseases were based on their self-reports.
The disease activity of PsA was defined by the DAPSA score. The cutoff values of the DAPSA score were proposed as ≤ 4 for remission, > 4 and ≤ 14 for low disease activity (LDA), > 14 and ≤ 28 for moderate disease activity (MDA), and > 28 for high disease activity (HDA) [19]. The disease of RA was defined by the DAS28CRP score. The cutoff values of DAS28CRP were proposed as ≤ 2.6 for remission, > 2.6 and ≤ 3.2 for LDA, > 3.2 and ≤ 5.1 for MDA, and > 5.1 for HDA.
Statistical Analysis
Data are presented as mean (± SD), median (IQR), or proportion (%) as appropriate. Comparisons of continuous variables with normal distribution were performed using Student’s t-test such as age, serum lipid spectrum, body mass index (BMI), and waist circumstance. Other continuous variables with non-normal distribution were evaluated by Mann–Whitney U test. Categorical variables were reported as frequencies and were analyzed by chi-squared test with odds ratio (OR). Pearson’s coefficient was used to describe the correlation between disease activity parameters and the number of MS components. Propensity score matching was used to reduce the influence of bias and confounding variables, including age and sex. These analyses were performed using SPSS version 22.0.
Propensity score matching (PSM) and propensity score-based inverse probability of treatment weighting (IPTW) were used to adjust the covariates including age, gender, smoking history, triglyceride, total cholesterol, and disease activity, to ensure the robustness of our findings. One-to-one nearest-neighbor matching with a caliper of 0.05 was applied. An IPTW model was created using the estimated propensity score as weights. The standardized mean differences (SMDs) were calculated to evaluate the effectiveness of the PSM and IPTW. The PSM and IPTW analyses were performed by RStudio (version 4.1.2).
Results
Demographics and Clinical Characteristics of Patients with PsA and RA
A total of 197 patients with PsA and 279 patients with RA were enrolled in this study. Compared with patients with RA, the patients with PsA were younger (47.9 ± 13.4 versus 50.4 ± 13.1, p = 0.043) with more males [107 (54.3%) versus 43 (15.4%), p < 0.001]. At enrollment, the median disease duration was 4.0 (IQR 8.0) years and 4.2 (IQR 8.3) for PsA and RA, respectively (p = 0.324). The median PASI of patients with PsA was 2.7 (7.0). The median DAPSA for patients with PsA was 12.0 (IQR 16.6). Forty-nine patients with PsA had minimal disease activity. The DAS28ESR/CRP, CDAI, and SDAI for RA were 3.86/3.40, 10.0, and 11.1, respectively (Table 1). The prevalence of moderate to high disease activity in RA was also higher than in PsA [151 (54.1%) versus 85 (43.1%), p = 0.018].
Prevalence of MS and CVD in Patients with RA and PsA
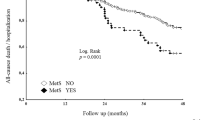
Before matching, MS was more frequently observed in patients with PsA than in those with RA [36.0% versus 23.3%, p = 0.002, OR 1.54 (1.16, 2.05)]. Patients with PsA had a larger mean waist circumference (84.6 ± 10.3 versus 78.6 ± 9.8 cm, p < 0.001) and mean BMI (24.61 ± 3.96 versus 22.93 ± 3.75, p < 0.001), with a higher frequency of abdominal obesity (61.9% versus 33.0%, p < 0.001). Patients with PsA had higher FBG (5.49 ± 0.88 versus 5.31 ± 0.76 mmol/L, p = 0.018) and were more frequently observed with T2DM (14.7% versus 7.9%, p = 0.018). Mean serum TG, total cholesterol (TCHO), and low-density lipoprotein (LDL) were all higher in PsA while mean HDL was lower (all p values < 0.05) (Tables 1 and 2). Considering the statistical differences in age, sex, smoking history, LDL, TCHO, and disease activity, we matched patients with PsA and those with RA by propensity score with a ratio of 1:1. Caliper was set as 0.05 for the nearest-neighbor matching. A total of 117 patients with PsA and 117 patients with RA were eventually selected for further comparison under PSM. The frequency of MS [37.6% versus 23.1%, OR 2.01 (1.44, 3.55), p = 0.016] and abdominal obesity [59.8% versus 32.5%, OR 3.10 1.81, 5.29), p < 0.001] was still higher in patients with PsA than in patients with RA. Similar discrepancies were observed in the IPTW cohorts (Tables 3 and 4).
Patients with PsA were more likely to have CVD than patients with RA [6.6% versus 1.1%, p = 0.001, OR 6.13 (1.77, 21.25)]. Four cases of acute myocardial infarction (AMI) were observed in the PsA group while no AMI cases were observed in the RA group. The prevalence of cerebral vascular diseases was comparable between the two groups [4.6% versus 2.2%, OR 2.12 (0.76, 5.87) p = 0.137] (Table2). These trends did not change after PSM and IPTW (Table 4).
Clinical Features of Metabolically Unhealthy Patients with PsA and RA
In the present study, the most common components of MS seen in metabolically unhealthy patients were abdominal obesity and decreased HDL. Reduced HDL (73.2% versus 93.8%, p = 0.001) was more frequently shown in metabolically unhealthy patients with RA, while statistical significance was found in frequencies of other components of MS (Table 5).
Patients with RA and PsA with MS were older than those without MS (53.7 ± 11.7 versus 44.7 ± 13.2, p < 0.001 and 54.7 ± 9.4 versus 49.1 ± 13.8, p = 0.002, respectively). In the PsA group, composite disease activity scores and several components were higher in patients with MS than in those without. Moreover, we observed a weak linear correlation between the number of MS components and several disease activity indexes, including PGA, EGA, VAS-pain, DAS28, CDAI, SDAI, and DAPSA scores (r = 0.174–0.308, all p value < 0.05). This phenomenon was not found in the RA group (Table 6). In addition, among the extra-articular manifestations of PsA, we observed a higher frequency of eye involvement in patients with PsA who have MS than in patients with PsA who do not have MS (11.2% versus 0.8%, p = 0.001).
Discussion
In our study, we found that MS was more frequently observed in patients with PsA, regardless of the influence of age, sex, and smoking history. The prevalence of increased FBG and abdominal obesity was higher in PsA. Previous studies also demonstrated that patients with PsA tended to have a higher risk of obesity and T2DM compared with patients with RA [4, 20, 21], which contributed to the increased prevalence of MS in PsA. Increased risks of obesity (BMI > 30 kg/m2) and T2DM were shown in patients with RA, PsA, and ankylosing spondylitis in previous studies [22,23,24,25]. In the Chinese population, obesity was also reported more frequently in patients with RA and patients with PsA than in the population without arthritis or psoriasis [26, 27].
Obesity is an important component of MS. MS or obesity itself has been demonstrated to lead to inflammation in patients with inflammatory arthritis, although at a low level [28, 29]. In MS, the imbalance in inflammatory components of adipose tissue, including immune cells, cytokines, and adipocytokines, causes a pro-inflammatory profile [30]. This could increase the risk of developing inflammatory arthritis. Increased BMI was associated with increased risk of developing PsA [31]. However, the relationship between obesity and RA is controversial [32, 33]. These findings may explain the increased risk of MS and obesity in PsA compared with RA.
A downtrend of serum HDL in RA and PsA was reported previously [34, 35]. Serum HDL was shown to be negatively correlated with disease activity in patients with RA [36]. In the present study, more patients with decreased HDL were observed in the RA cohort after IPTW. Interleukin-6 (IL-6) is a significant cytokine involved in the inflammatory process of RA, but not of PsA. IL-6 also affects lipid metabolism by increasing the uptake of cholesterol, which in turn caused a downtrend of HDL [37]. During the treatment of IL-6, decreased uptake and catabolism of lipids caused increased HDL levels [38,39,40]. These findings may explain the relatively larger proportion of decreasing HDL in patients with RA.
In the present study, we observed a weak-to-medium positive correlation between MS and baseline disease activity of patients with PsA. Leite et al. revealed a similar positive linear correlation between disease activity and total body fat in patients with PsA [41]. The weak correlation may be caused by not combining joint and skin lesion together when evaluating disease activity of PsA. This is one limitation of the present study. However, we did not find a similar correlation between disease activity and MS in patients with RA. Some studies have shown RA disease activity to be associated with MS, while others have shown the opposite [42,43,44]. Previous research by Sumarac-Dumanovic examined interleukin-23 (IL-23) and interleukin-17 (IL-17) levels in people with obesity [45]. IL-17 contributes to inflammation in both RA and PsA [46]. The increased levels of IL-23 may contribute more to the inflammation status of PsA than that of RA. We reckon that the increased burden of obesity in patients with PsA could amplify its influence on inflammation, which causes this positive linear relationship between MS and disease activity. The inflammatory axis of IL-23/IL-17 may also contribute to eye inflammation [47], which may explain the relatively higher frequency of uveitis in our patients with PsA who have MS. Further research is needed to understand this difference.
We observed an increased prevalence of CVD in patients with PsA compared with patients with RA, in both unmatched and matched cohorts. Moreover, we observed cases of AMI in patients with PsA but not in patients with RA. Since more cardiovascular risk factors such as obesity and T2DM were observed in patients with PsA, this phenomenon was not hard to explain. The research by Martin-Martinez observed the highest prevalence of cardiovascular events in patients with PsA compared with patients with RA and ankylosing spondylitis [48]. Despite traditional risk factors, psoriasis also independently contributes to the risk of myocardial infarction [49]. These previous findings illustrate that more attention should be paid to the management of CVD, especially in patients with PsA.
As many risk factors of MS and CVD were different between our patients with PsA and those with RA, we used PSM and IPTW to control these covariates, including age, sex, disease activity, smoking history, TCHO, and LDL. The assessment tools of disease activity of RA and PsA were different, and joint counts contribute more to PsA disease activity. After matching, ESR and CRP were still higher in patients with RA in both PSM and IPTW cohorts while the disease activities were comparable. We did not include uric acid as a covariate either since hyperuricemia was a metabolic disorder we wanted to observe. Hyperuricemia is associated with psoriatic arthritis and some metabolic items such as obesity, so it is reasonable to observe an increased proportion of hyperuricemia in patients with PsA after matching.
This present one-center study directly showed the discrepancy of MS and CVD in PsA and RA that few studies have observed before. To our knowledge, this is the first study in mainland China that showed the difference between PsA and RA in the aspect of metabolic disorders in adults. Owing to the increased risk of CVD, CVD risk factors should be screened in patients with PsA and modifiable factors should be managed [50].
We acknowledge the limitation of this study. We recorded the history of hypertension in all enrolled patients, but no quantitative data on blood pressure were collected, making it impossible to analyze the relationship among arthritis type, disease activity, and level of hypertension. We did not record data on HbA1c, which might have affected the diagnosis of MS. Severity of other comorbidities, including CVD and T2DM, was not analyzed either. Moreover, we do not have sufficient data of treatment duration before recruitment and medication adherence to analyze the effect exerted on MS and cardiovascular events by previous therapy. Further research is needed to explore the specific mechanism of MS in these patients and any impact on disease activity with the improvement of MS.
Conclusions
Considerable discrepancies in MS and CVD were observed between patients with PsA and patients with RA. The greater odds of MS and CVD emphasize the need to pay more attention to metabolic and cardiovascular conditions in patients with PsA.
References
FitzGerald O, et al. Psoriatic arthritis. Nat Rev Dis Primers. 2021;7(1):59.
Almutairi KB, et al. The prevalence of rheumatoid arthritis: a systematic review of population-based studies. J Rheumatol. 2021;48(5):669–76.
Conforti A, et al. Beyond the joints, the extra-articular manifestations in rheumatoid arthritis. Autoimmun Rev. 2021;20(2): 102735.
Pittam B, et al. Prevalence of extra-articular manifestations in psoriatic arthritis: a systematic review and meta-analysis. Rheumatology (Oxford). 2020;59(9):2199–206.
Silveira RJ, et al. Metabolic syndrome and cardiovascular diseases: going beyond traditional risk factors. Diabetes Metab Res Rev. 2022;38(3): e3502.
Grandl G, Wolfrum C. Hemostasis, endothelial stress, inflammation, and the metabolic syndrome. Semin Immunopathol. 2018;40(2):215–24.
Hallajzadeh J, et al. Metabolic syndrome and its components among rheumatoid arthritis patients: a comprehensive updated systematic review and meta-analysis. PLoS ONE. 2017;12(3): e0170361.
Karmacharya P, Ogdie A, Eder L. Psoriatic arthritis and the association with cardiometabolic disease: a narrative review. Ther Adv Musculoskelet Dis. 2021. https://doi.org/10.1177/1759720X21998279.
Lin YC, et al. Relationship between metabolic syndrome and carotid intima-media thickness: cross-sectional comparison between psoriasis and psoriatic arthritis. Arthritis Care Res (Hoboken). 2014;66(1):97–103.
Rodriguez-Zuniga M, Garcia-Perdomo HA. Systematic review and meta-analysis of the association between psoriasis and metabolic syndrome. J Am Acad Dermatol. 2017;77(4):657–66 (e8).
Agca R, et al. EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis. 2017;76(1):17–28.
Mok CC, et al. Prevalence of atherosclerotic risk factors and the metabolic syndrome in patients with chronic inflammatory arthritis. Arthritis Care Res (Hoboken). 2011;63(2):195–202.
Labitigan M, et al. Higher rates and clustering of abnormal lipids, obesity, and diabetes mellitus in psoriatic arthritis compared with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2014;66(4):600–7.
Cooksey R, et al. Cardiovascular risk factors predicting cardiac events are different in patients with rheumatoid arthritis, psoriatic arthritis, and psoriasis. Semin Arthritis Rheum. 2018;48(3):367–73.
Ozkul O, et al. Are there any differences among psoriasis, psoriatic arthritis and rheumatoid arthritis in terms of metabolic syndrome and cardiovascular risk factors? Eur J Rheumatol. 2019;6(4):174–8.
Lauper K, et al. Incidence and prevalence of major adverse cardiovascular events in rheumatoid arthritis, psoriatic arthritis, and axial spondyloarthritis. Arthritis Care Res (Hoboken). 2018;70(12):1756–63.
Arnett FC, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315–24.
Alberti KG, Zimmet P, Shaw J. Metabolic syndrome—a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006;23(5):469–80.
Schoels MM, et al. Disease activity in psoriatic arthritis (PsA): defining remission and treatment success using the DAPSA score. Ann Rheum Dis. 2016;75(5):811–8.
Fragoulis GE, et al. Higher depression rates and similar cardiovascular comorbidity in psoriatic arthritis compared with rheumatoid arthritis and diabetes mellitus. Ther Adv Musculoskelet Dis. 2020. https://doi.org/10.1177/1759720X20976975.
Jin Y, et al. Risk of incident type 2 diabetes mellitus among patients with rheumatoid arthritis: a population-based cohort study. Arthritis Care Res (Hoboken). 2020;72(9):1248–56.
Queiro R, et al. Obesity in psoriatic arthritis: comparative prevalence and associated factors. Medicine (Baltimore). 2019;98(28): e16400.
Dar L, et al. Are obesity and rheumatoid arthritis interrelated? Int J Clin Pract. 2018;72(1):e13045.
Jiang P, Li H, Li X. Diabetes mellitus risk factors in rheumatoid arthritis: a systematic review and meta-analysis. Clin Exp Rheumatol. 2015;33(1):115–21.
Queiro R, et al. Prevalence and type II diabetes-associated factors in psoriatic arthritis. Clin Rheumatol. 2018;37(4):1059–64.
Li C, et al. A multicenter study of coronary artery disease and its risk factors in rheumatoid arthritis in China. Beijing Da Xue Xue Bao Yi Xue Ban. 2012;44(2):176–81.
Zhang C, et al. The effect of overweight and obesity on psoriasis patients in Chinese Han population: a hospital-based study. J Eur Acad Dermatol Venereol. 2011;25(1):87–91.
Carrier A. Metabolic syndrome and oxidative stress: a complex relationship. Antioxid Redox Signal. 2017;26(9):429–31.
Rohm TV, et al. Inflammation in obesity, diabetes, and related disorders. Immunity. 2022;55(1):31–55.
Torres S, et al. Adipose tissue inflammation and metabolic syndrome. The proactive role of probiotics. Eur J Nutr. 2019;58(1):27–43.
Green A, et al. Modifiable risk factors and the development of psoriatic arthritis in people with psoriasis. Br J Dermatol. 2020;182(3):714–20.
Ljung L, Rantapaa-Dahlqvist S. Abdominal obesity, gender and the risk of rheumatoid arthritis—a nested case–control study. Arthritis Res Ther. 2016;18(1):277.
Cerhan JR, et al. Blood transfusion, alcohol use, and anthropometric risk factors for rheumatoid arthritis in older women. J Rheumatol. 2002;29(2):246–54.
Pietrzak A, et al. Serum lipid metabolism in psoriasis and psoriatic arthritis—an update. Arch Med Sci. 2019;15(2):369–75.
Robertson J, et al. Changes in lipid levels with inflammation and therapy in RA: a maturing paradigm. Nat Rev Rheumatol. 2013;9(9):513–23.
Ridker PM, et al. Reduction in C-reactive protein and LDL cholesterol and cardiovascular event rates after initiation of rosuvastatin: a prospective study of the JUPITER trial. Lancet. 2009;373(9670):1175–82.
Hashizume M, et al. Overproduced interleukin 6 decreases blood lipid levels via upregulation of very-low-density lipoprotein receptor. Ann Rheum Dis. 2010;69(4):741–6.
Behl T, et al. The Lipid Paradox as a metabolic checkpoint and its therapeutic significance in ameliorating the associated cardiovascular risks in rheumatoid arthritis patients. Int J Mol Sci. 2020;21(24):9505.
Robertson J, et al. Interleukin-6 blockade raises LDL via reduced catabolism rather than via increased synthesis: a cytokine-specific mechanism for cholesterol changes in rheumatoid arthritis. Ann Rheum Dis. 2017;76(11):1949–52.
Gabay C, et al. Comparison of lipid and lipid-associated cardiovascular risk marker changes after treatment with tocilizumab or adalimumab in patients with rheumatoid arthritis. Ann Rheum Dis. 2016;75(10):1806–12.
Leite BF, et al. Higher bodily adiposity, fat intake, and cholesterol serum levels are associated with higher disease activity in psoriatic arthritis patients: is there a link among fat and skin and joint involvement? Lipids Health Dis. 2020;19(1):21.
Sahebari M, et al. Investigation of the association between metabolic syndrome and disease activity in rheumatoid arthritis. ScientificWorldJournal. 2011;11:1195–205.
Kuriya B, et al. Prevalence and characteristics of metabolic syndrome differ in men and women with early rheumatoid arthritis. ACR Open Rheumatol. 2019;1(9):535–41.
Karvounaris SA, et al. Metabolic syndrome is common among middle-to-older aged Mediterranean patients with rheumatoid arthritis and correlates with disease activity: a retrospective, cross-sectional, controlled, study. Ann Rheum Dis. 2007;66(1):28–33.
Sumarac-Dumanovic M, et al. Increased activity of interleukin-23/interleukin-17 proinflammatory axis in obese women. Int J Obes (Lond). 2009;33(1):151–6.
Ruiz DMJ, et al. Critical role of interleukin (IL)-17 in inflammatory and immune disorders: an updated review of the evidence focusing in controversies. Autoimmun Rev. 2020;19(1): 102429.
Bridgewood C, et al. Unexpected connections of the IL-23/IL-17 and IL-4/IL-13 cytokine axes in inflammatory arthritis and enthesitis. Semin Immunol. 2021. https://doi.org/10.1016/j.smim.2021.101520.
Martin-Martinez MA, et al. Cardiovascular mortality and cardiovascular event rates in patients with inflammatory rheumatic diseases in the CARdiovascular in rheuMAtology (CARMA) prospective study-results at 5 years of follow-up. Rheumatology (Oxford). 2020;60(6):2906–15.
Gelfand JM, et al. Risk of myocardial infarction in patients with psoriasis. JAMA. 2006;296(14):1735–41.
Coates LC, et al. Group for research and assessment of psoriasis and psoriatic arthritis (GRAPPA): updated treatment recommendations for psoriatic arthritis 2021. Nat Rev Rheumatol. 2022;18(8):465–79.
Acknowledgements
We thank the participants of the study. This study is based on the contributions of all colleagues in the Rheumatology and Clinical Immunology Department of Peking University First Hospital during the outpatient visits over the past decade.
Funding
This work and the journal’s Rapid Service Fee were supported by the youth clinical research project of Peking University First Hospital (2019CR28) and the National Natural Science Foundation of China (nos. 81771740, 81801611, 81971524). Declaration of 1964 and its later amendments or comparable ethical standards.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article and take responsibility for the integrity of this work. All the authors listed have approved the manuscript.
Author Contributions
Zhuoli Zhang conceived, designed, and coordinated the study and critically revised the manuscript. Borui Li carried out the data collection, analysis, and interpretation, and drafted the manuscript. Borui Li, Hong Huang, Juan Zhao, and Xuerong Deng contributed to the process of data collection.
Disclosures
Borui Li, Hong Huang, Juan Zhao, Xuerong Deng, and Zhuoli Zhang have no conflicts of interest to disclose.
Compliance with Ethics Guidelines
This study was approved by the institutional review board (IRB) of the Peking University First Hospital, and informed consent was obtained from each participant. All procedures performed in studies involving human participants in this study were performed in accordance with the Declaration of Helsinki.
Data Availability
The original datasets used for analysis in the current study can be provided on reasonable request by contacting the corresponding author.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Li, B., Huang, H., Zhao, J. et al. Discrepancy in Metabolic Syndrome between Psoriatic Arthritis and Rheumatoid Arthritis: a Direct Comparison of Two Cohorts in One Center. Rheumatol Ther 10, 135–148 (2023). https://doi.org/10.1007/s40744-022-00502-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-022-00502-4