Abstract
Background
Acute anterior uveitis (AAU) affects up to 40% of patients with axial spondyloarthritis (axSpA). An effective treatment for patients with axSpA that reduces the risk of AAU flares while also targeting axial symptoms is therefore highly desirable. Tumor necrosis factor inhibitors (TNFis) have been shown effective for treatment of axSpA and AAU occurrence, with guidelines conditionally recommending treating patients with axSpA and associated AAU with TNFi monoclonal antibodies. To date, most available data on the impact of TNFis on AAU in axSpA are from observational, open-label studies without parallel comparator arms. However, there is a growing body of evidence describing the impact of the TNFi certolizumab pegol (CZP) on the incidence of axSpA-associated AAU.
Objective
Our objective was to collate data pertaining to the impact of CZP in axSpA-associated AAU in patients across the full axSpA spectrum.
Methods
Data were obtained from four industry-supported phase 3 and 4 clinical trials (C-VIEW, C-axSpAnd, C-OPTIMISE, and RAPID-axSpA). To supplement these data, a targeted literature review was performed through searches of MEDLINE, Embase, and reference lists.
Results
Available data from 1467 patients from the C-VIEW, C-axSpAnd, C-OPTIMISE, and RAPID-axSpA trials show CZP to be effective in AAU in patients across the full axSpA spectrum, reducing AAU flares when compared with placebo or pretreatment period. No differences in AAU outcomes were reported when stratified by axSpA subgroup age or sex. The targeted literature review identified six further studies of CZP in spondyloarthritis-associated AAU, only one of which was specific to axSpA.
Conclusion
CZP was effective in reducing AAU incidence in clinical trials with patients with axSpA. The targeted literature review, however, highlighted that there remains a paucity of data beyond these trials. Data from comparative studies would further enhance the body of evidence on the effects of CZP in patients with axSpA who develop AAU.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Acute anterior uveitis (AAU) affects up to 40% of patients with axial spondyloarthritis (axSpA). |
This study collates data pertaining to the impact of the tumor necrosis factor inhibitor certolizumab pegol (CZP) in axSpA-associated AAU in patients across the full axSpA spectrum. |
CZP was effective in reducing AAU incidence in studies with axSpA patients, reducing AAU flares when compared with placebo or pretreatment period. |
No differences in AAU outcomes were reported when stratified by axSpA subgroup, age, or sex. |
Outside of industry-supported clinical trials, however, there remains a paucity of data regarding the effectiveness of CZP in axSpA-associated AAU. |
Digital Features
This article is published with digital features, including a graphical abstract, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.20490063.
Introduction
Axial spondyloarthritis (axSpA) is a chronic inflammatory disease characterized by involvement of the axial and peripheral skeleton. The disease comprises two subpopulations: those with radiographic axSpA (r-axSpA; ankylosing spondylitis, AS) and those with nonradiographic axSpA (nr-axSpA), with the difference determined by the presence or absence of radiographic sacroiliitis fulfilling the modified New York criteria [1, 2]. Although primarily a musculoskeletal condition, extramusculoskeletal manifestations (EMMs) such as acute anterior uveitis (AAU), psoriasis, and inflammatory bowel disease are important and common systemic features of axSpA that further contribute to the disease burden [3].
AAU, defined as a noninfectious, acute inflammation of the anterior uveal tract and adjacent structures, is the most common EMM in axSpA and affects up to 40% of patients [4, 5]. The onset of AAU symptoms is sudden and includes ocular pain, photophobia, and blurred vision. AAU flares can be recurrent and unpredictable, with variable remission periods spanning from weeks to years [6]. Treatment for AAU with local corticosteroids and mydriatics is often effective, but delayed or inadequate treatment can cause blindness [7, 8]. An efficacious treatment for patients with axSpA that reduces the risk of AAU flares while also targeting axSpA symptoms is, therefore, highly desirable; the importance of treating AAU associated with axSpA has been emphasized in the 2019 American College of Rheumatology (ACR)–Spondylitis Association of America (SAA)–Spondyloarthritis Research and Treatment Network (SPARTAN) and the 2016 ASAS–European League Against Rheumatism (EULAR) guidelines [9, 10].
Biologic disease-modifying antirheumatic drugs (bDMARDs)—especially tumor necrosis factor inhibitors (TNFis)—have been proven effective for the treatment of axSpA. Indeed, the 2016 ASAS–EULAR guidelines recommend bDMARDs for patients with axSpA who failed to respond to conventional treatments, and highlight the initiation of TNFi therapy over other biologics owing to more extensive experience and clinical data [10].
TNFis, especially monoclonal antibodies, have also been shown effective against AAU recurrence, with several studies demonstrating their effectiveness in r-axSpA-related AAU [11,12,13,14,15,16,17,18]. The ACR–SAA–SPARTAN guidelines conditionally recommend treating patients with axSpA and associated AAU with TNFi monoclonal antibodies [9]. Adalimumab is currently the sole TNFi to have received US Food and Drug Administration (FDA) approval for the treatment of uveitis in adults. However treatment is indicated only for intermediate uveitis, posterior uveitis, and panuveitis, and does not extend to AAU. Additionally, data pertaining to the impact of TNFis on AAU in axSpA are mostly from observational, open-label studies with historical controls and r-axSpA (rather than nr-axSpA) populations [11, 15,16,17].
Certolizumab pegol (CZP) is a PEGylated Fc-free TNFi, indicated for the treatment of adult patients with active axSpA by several regulatory authorities, and is the only FDA-approved TNFi for both r-axSpA and nr-axSpA [19, 20]. Previous studies have shown CZP to be safe and efficacious for axial symptoms of axSpA; with these studies comes a growing body of evidence describing the impact of CZP on the incidence of axSpA-associated AAU [21,22,23,24,25,26,27].
The purpose of this narrative review is to summarize the evidence within the current literature for the effect of CZP treatment on AAU in both subpopulations of patients with axSpA (r- and nr-axSpA), supported by data from four phase 3 or 4 clinical trials. Data are also supplemented by a targeted literature review of studies in patients with axSpA and AAU who received CZP.
Patients and Methods
Study Populations
Data in this review have been obtained from one phase 4 and three phase 3 industry-supported, interventional, clinical studies that assessed CZP in axSpA-associated AAU as primary, secondary, or post-hoc outcomes: C-VIEW (NCT03020992), C-axSpAnd (NCT02552212), C-OPTIMISE (NCT02505542), and RAPID-axSpA (NCT01087762, Table 1). Detailed study design and methods have been described previously—data included in this review include both data taken from the original study publications, and data on file [19, 21,22,23,24,25,26,27].
C-VIEW
C-VIEW was a 104-week (96 weeks plus 8-week safety follow-up), open-label, multicenter phase 4 study. Eligible patients had high axSpA disease activity at baseline (defined as a Bath Ankylosing Spondylitis Disease Activity Index [BASDAI] score ≥ 4 and spinal pain [BASDAI item 2] ≥ 4) and were at high risk for recurrent AAU flares (a history of recurrent AAU [two or more AAU flares in total; one or more flares in the year prior to baseline]). The primary efficacy outcome was the AAU flare event rate—assessed by counting distinct episodes of AAU flares—during 96 weeks CZP versus 2 years pre-baseline. Patients were requested to contact their ophthalmologist when they suspected an AAU flare at any time during the study. Patients received CZP 400 mg at weeks 0, 2, and 4, then 200 mg every 2 weeks to week 96 [24, 25].
C-axSpAnd
C-axSpAnd was a 3-year, multicenter phase 3 study including a 52-week double-blind, placebo-controlled period reporting uveitis data as a secondary outcome. Adults (n = 317) with nr-axSpA fulfilling the Assessment of SpondyloArthritis international Society (ASAS) classification criteria and with objective signs of inflammation (C-reactive protein [CRP] ≥ upper limit of normal [CRP+] and/or evidence of sacroiliitis on MRI [MRI+]) were randomized 1:1 to placebo (PBO) or CZP (400 mg at weeks 0, 2, and 4, then 200 mg every 2 weeks [Q2W]) for 52 weeks. AAU outcomes included the number of patients reporting AAU flares as recorded on EMM and adverse event forms [27].
C-OPTIMISE
C-OPTIMISE was a two-part, multicenter phase 3 study in adults with early active axSpA (radiographic or nonradiographic) where AAU data were reported as a secondary outcome. During the 48-week open-label induction period, patients received CZP 200 mg every 2 weeks (Q2W). At week 48, patients in sustained remission (Ankylosing Spondylitis Disease Activity Score [ASDAS] < 1.3 at weeks 32/36 and 48) were randomized to receive double-blind CZP 200 mg Q2W (full maintenance dose), CZP 200 mg every 4 weeks (Q4W; reduced maintenance dose) or placebo (withdrawal) for a further 48 weeks. AAU outcomes included the number of patients reporting AAU flares as recorded on EMM and adverse event forms, and were stratified by history of uveitis at baseline [22, 23].
RAPID-axSpA
RAPID-axSpA was a double-blind and placebo-controlled to week 24, dose-blind to week 48, and open-label to week 204 phase 3 study. In this multicenter study in adults with active axSpA (radiographic or nonradiographic), patients were randomized to CZP or placebo; placebo patients entering the dose-blind phase were rerandomized to CZP. AAU outcomes included number of patients reporting AAU flares and were recorded on EMM or adverse event forms. Events were stratified by history of uveitis at baseline, and rates were reported per 100 patient-years [21, 26].
Targeted Literature Review
To capture any data on CZP in axSpA-associated AAU beyond the C-VIEW, C-axSpAnd, C-OPTIMISE, and RAPID-axSpA studies, a targeted literature search was performed on 19 July 2021, in the Ovid MEDLINE and Embase databases. Search terms included “axial spondyloarthritis,” “spondylarthropathies,” [“certolizumab pegol” OR “CZP”], [“uveitis” OR “iritis” OR “AU” or “AAU”]; the full search strategy is outlined in Supplementary Table S1. A supplementary search of the bibliographies of relevant review articles identified through the database searches was also performed.
To be eligible, studies had to be in English and report AAU outcomes in adults with axSpA who had received CZP. Review articles, conference abstracts where data had subsequently been reported in a full manuscript, and abstracts and manuscripts pertaining to the clinical studies detailed above were excluded.
Results
Study Populations
Across the phase 3 and 4 clinical studies reporting on the impact of CZP in axSpA-associated AAU, data have been reported for 1467 patients (Fig. 1). Baseline characteristics for patients included in the phase 3/4 clinical studies are provided in Table 2. These studies confirmed the safety and efficacy profile of CZP in both r-axSpA and nr-axSpA populations; data pertaining to the treatment of axial symptoms in axSpA are reported in the original publications [21,22,23,24,25,26,27].
AAU Flare Incidence and Event Rate and Duration
Across all studies, CZP led to a reduction in the number of patients reporting AAU flares compared with placebo or the pretreatment period (Table 3, Supplementary Fig. 1), with larger reductions in AAU flares observed in groups receiving a continuous maintenance dose of CZP (200 mg Q2W), compared with those who had a dose reduction (200 mg Q4W). During the C-OPTIMISE double-blind period, 6/104 (5.8%) patients experienced an AAU flare in the placebo group. This compares to the 3/105 (2.9%) of patients who experienced an AAU flare in the group receiving 200 mg CZP Q4W; in the group receiving the full maintenance dose, no flares were reported (data on file). In C-axSpAnd, where all patients had nr-axSpA, 4/159 (2.5%) patients receiving CZP 200 mg Q2W reported an AAU flare by week 52 compared with 8/158 (5.1%) of those in the placebo group [27].
Data pertaining to AAU flare event rate have also been reported [24, 25]. In C-VIEW, the adjusted event rate was 1.87 in the pretreatment period compared with 0.34 in the 96-week treatment period (Fig. 2). This represents an 82% reduction (rate ratio 0.18, 95% confidence interval [95% CI] 0.12–0.28) and is noteworthy since patients were selected on the basis of criteria that predicted the highest recurrence risk of AAU (both prior history of AAU and human leukocyte antigen B27 [HLA-B27] positivity) [25].
AAU flares event rate per 96 weeks stratified by disease diagnosis, sex, and age. All data from C-VIEW [25]. “Pre-Study Historical”: week—104 to baseline; “On-study CZP”: baseline to week 96. CI confidence interval, CZP certolizumab pegol, nr-axSpA nonradiographic axSpA, r-axSpA radiographic axSpA
AAU flare event rate data—assessed by counting distinct episodes of AAU flares—for CZP versus placebo were reported in RAPID-axSpA, where the rate of uveitis flares to week 24 was lower in patients treated with CZP (3.0 per 100 patient‐years; 95% CI 0.6–8.8; 200 mg Q2W or 400 mg Q4W) compared with placebo (10.3 per 100 patient‐years; 95% CI 2.8–26.3). Furthermore, data pertaining to the long‐term incidence of uveitis—collected to week 96 of the RAPID‐axSpA trial—suggested that the overall rate of AAU flares remained similar at weeks 48 and 96 of CZP treatment compared with that observed over 24 weeks of CZP treatment (4.9 per 100 patient‐years at week 48 [95% CI 2.5–8.6] and 4.9 per 100 patient‐years at week 96 [95% CI 3.2–7.4]) [21].
The final measure of the impact of CZP on AAU in patients with axSpA reported in the literature is flare duration, defined as total days of active AAU per patient. In C-VIEW, 18/89 patients (20%) experienced AAU flares during the 96-week treatment period: for these patients, the mean (SD) duration of total days active inflammation per patient was 97.3 (66.7) days in the 2-year prebaseline period, compared with 74.4 (55.3) days during 96 weeks of CZP treatment (mean reduction of 22.9 days) [25].
AAU Outcomes Stratified by History of AAU at Baseline
AAU flares are often recurrent in patients with axSpA, yet effective treatments for relapsing AAU are limited [28]. All patients enrolled in the C-VIEW trial had at least one AAU flare in the 104-week prestudy period, with 53/89 patients (59.6%) experiencing two or more AAU flares. Over the 96-week CZP treatment period, the proportion of patients experiencing two or more flares was reduced to 11.2% (10/89); 9.0% of patients (8/89) experienced a single flare, whilst 79.8% of patients (71/89) had no AAU flares while receiving CZP [25]. Similar AAU outcomes were reported in C-OPTIMISE and RAPID-axSpA (Table 4). Of those with a history of AAU at baseline, patients who received CZP reported no AAU flares compared with 4/17 (23.5%) of those who received placebo at week 96 in C-OPTIMISE (data on file); comparably, at week 24 in RAPID-axspA, 3/38 (7.9%) patients with a history of AAU who received CZP reported flares, compared with 4/31 (12.9%) of those in the placebo group [21, 22].
Comparator data are limited for patients without a history of AAU at baseline, although no patients in this group reported AAU flares in RAPID-axSpA (with either CZP or placebo treatment) [21].
AAU Outcomes by Disease Classification
AAU is known to have a greater prevalence in patients with r-axSpA compared with nr-axSpA: as many as 40% of patients with r-axSpA will experience at least one AAU flare during the course of their disease. A lower prevalence has been reported for patients with nr-axSpA, but data are more limited [29,30,31,32]. Across the C-VIEW, C-axSpAnd, C-OPTIMISE, and RAPID-axSpA studies, AAU data are reported for 806 patients with nr-axSpA. Data from C-axSpAnd—where all 317 enrolled patients had nr-axSpA—show CZP to be effective at reducing the number of patients reporting AAU flares when compared with placebo [CZP 200 mg Q2W: n = 4 (2.5%); placebo: n = 8 (5.1%); Table 3] [27].
Furthermore, no significant differences in AAU flare event rate data between nr-axSpA (n = 13) and r-axSpA (n = 76) subpopulations were reported in C-VIEW (Fig. 2)—after 96 weeks of receiving CZP, both groups achieved an 82% reduction in AAU flare event rate [25]. C-OPTIMISE and RAPID-axSpA also included patients with both nr-axSpA (C-OPTIMISE: n = 329; RAPID-axSpA: n = 147) and r-axSpA (C-OPTIMISE: n = 407; RAPID-axSpA: n = 178); AAU outcome data specific to patients with nr-axSpA from these trials are not available, however, as data were pooled with those from the r-axSpA subpopulations [21,22,23, 26].
AAU Outcomes Stratified by Sex and Age
The efficacy of TNFis has been observed to be lower in females with axSpA compared with males for subjective outcome measures [33], but little has been reported on sex differences in the treatment of AAU. In C-VIEW, the male and female subgroups achieved reductions in AAU flare event rate of 85% and 76%, respectively: the AAU flare event rate was reduced from 1.89 to 0.28 per 96 weeks (rate ratio 0.15; 95% CI 0.08–0.27) in male patients (n = 56), compared with a reduction of 1.86–0.44 (rate ratio 0.24; 95% CI 0.12–0.46) in female patients (n = 33; Fig. 2) [25]. No significant differences have been reported for the impact of age on the effectiveness of CZP in AAU associated axSpA, although data are limited to a small subgroup analysis performed in C-VIEW where AAU flare event rates were reported for patients older or younger than 45 years (Fig. 2).
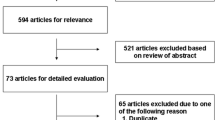
Targeted Literature Review
We performed a targeted literature search of the Ovid MEDLINE and Embase databases to identify data on the effects of CZP in axSpA-associated AAU beyond the RAPID-axSpA, C-OPTIMISE, C-axSpAnd, and C-VIEW studies. After deduplication, the electronic database search identified 80 records; 25 were included for full-text review, of which 2 publications fulfilled the eligibility criteria and were included. The supplementary search of excluded review article bibliographies identified four further publications, giving a total of six (Supplementary Fig. 2) [34,35,36,37,38,39]. However, of these six included studies, only one was specific to CZP in axSpA-associated AAU—an observational, multicenter, retrospective study in 13 patients with SpA (8 axSpA) with refractory uveitis, who had received CZP for at least 6 months [34]. The results of this study suggest that CZP provides a benefit to patients with uveitis associated with SpA refractory to previous TNFi treatment: improvements (although not quantified) were observed in both SpA activity and visual acuity. The remaining five studies included a very low number of patients from several subpopulations across the SpA disease spectrum, including psoriatic spondylitis and inflammatory bowel disease-associated spondyloarthritis. As the study populations comprised patients who are not the topic of this review, it is difficult to draw any conclusions on the efficacy of CZP in uveitis specifically associated with axial SpA from these studies.
Discussion
AAU is the most frequent extramusculoskeletal manifestation of axSpA and can represent a significant clinical burden; the management of AAU therefore represents an important aspect of axSpA disease treatment. Some observational data suggest that conventional synthetic DMARDs (csDMARDs) such as sulfasalazine could have potential in the management of highly recurrent AAU [4, 6]. Data demonstrating the impact of CZP treatment on the incidence of AAU are available for 1467 patients across the C-VIEW, C-axSpAnd, C-OPTIMISE, and RAPID-axSpA clinical trials and show CZP to be effective in patients with axSpA-associated AAU across the full axSpA spectrum, including both r- and nr-axSpA. In these trials, concomitant use of csDMARDs was comparable across CZP and placebo groups; greater improvements in AAU symptoms in groups receiving CZP compared with placebo cannot be ascribed to differing rates of csDMARD administration [21,22,23,24,25,26,27].
Our targeted literature review highlighted that, outside of the industry-supported phase 3 and 4 clinical studies—and similar to other biologics for the treatment of axSpA—there remains a paucity of data that are specific to CZP in axSpA and related AAU. Those few studies that are available have a limited number of patients and are predominantly case reports. In our analysis, the earliest report of CZP use in a patient with AAU associated with r-axSpA was from a single retrospective case series of seven patients with uveitis, one of whom had anterior uveitis and r-axSpA [35]. After CZP commencement, rapid ocular quiescence and improvement in axial symptoms were achieved in the patient with r-axSpA and maintained until 6 months of follow-up. However, the patient also had relapsing polychondritis, and so was excluded from our analysis.
This review demonstrates that subsequent data beyond the industry-supported clinical trials are still limited and highlights data from C-VIEW, C-axSpAnd, C-OPTIMISE, and RAPID-axSpA trials as the most robust and consistent pertaining to the efficacy of CZP on axSpA-associated AAU. C-VIEW was the first study to assess AAU flares as a primary outcome in a population of patients with axSpA who were at a high risk of AAU (both HLA-B27 positive and with a history of AUU). One limitation of C-VIEW was the open-label study design without a parallel control group. A placebo control, however, was considered unethical owing to enrolling patients at a high risk of developing recurrent AAU and with high axSpA disease activity at baseline. While the within-patient historical control in C-VIEW offered a good solution, the availability of data from comparative studies would further enhance the body of evidence on the effects of CZP in patients with axSpA and associated AAU.
AAU is known to have a greater prevalence in patients with r-axSpA than in those with nr-axSpA: one 2016 study performed a pooled meta-analysis comprising 2236 patients and reported a difference in the pooled prevalence of history of uveitis between patients with r-axSpA (23%) and those with nr-axSpA (16%) [31]. The increased incidence of AAU with axSpA disease duration is likely to contribute to this difference; the prevalence of AAU in axSpA has been shown to reach over 50% in patients with r-axSpA with a disease duration ≥ 30 years [40]. An alternative explanation for these differences in prevalence is HLA-B27 positivity being lower in nr-axSpA populations: a key genetic marker for axSpA, HLA-B27 has been associated with a substantially increased risk (2.6- to 4.2-fold) of developing AAU [41]. Patients with HLA-B27-positive axSpA also often have more frequent and severe episodes of AAU than those who are HLA-B27 negative [3].
To date, there has been a paucity of data specific to the effect of biologics in nr-axSpA and AAU, with most studies specific to r-axSpA populations. Studies report that about 10–40% of patients with nr-axSpA progress to r-axSpA over a period of 2–10 years, though there remains some debate on whether nr-axSpA should be seen as an early form of r-axSpA, or as two distinct conditions [42,43,44]. This review collates AAU outcome data for 806 patients with nr-axSpA, with the C-axSpAnd study being the first to incorporate a 52-week placebo-controlled time period to investigate the efficacy of an anti-TNF agent in a population of nr-axSpA patients and report the impact of CZP on axSpA disease activity and AAU flare rates.
Other reported subgroup analyses (age greater or less than 45 years; sex) found no significant differences between groups, although the sample sizes were too small to be sufficiently powered to draw conclusions by subgroup [25]. To our knowledge, these are the only data in the literature pertaining to CZP efficacy in axSpA-associated AAU stratified by age or sex.
Conclusion
The management of AAU manifestation is an important aspect of axSpA disease treatment. Data showing CZP to be effective in AAU in patients through the full axSpA spectrum, including both r-axSpA and nr-axSpA, are available for 1467 patients across the C-VIEW, C-axSpAnd, C-OPTIMISE, and RAPID-axSpA clinical trials. Outside of these studies, however, there remains a paucity of data that are specific to CZP in axSpA and related AAU.
References
Robinson PC, van der Linden S, Khan MA, Taylor WJ. Axial spondyloarthritis: concept, construct, classification and implications for therapy. Nat Rev Rheumatol. 2021;17(2):109–18.
van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984;27(4):361–8.
Carron P, Van Praet L, Jacques P, Elewaut D, Van den Bosch F. Therapy for spondyloarthritis: the role of extra-articular manifestations (eye, skin). Rheum Dis Clin N Am. 2012;38(3):583–600.
Biggioggero M, Crotti C, Becciolini A, Miserocchi E, Favalli EG. The management of acute anterior uveitis complicating spondyloarthritis: present and future. Biomed Res Int. 2018;2018:9460187.
Martin TM, Smith JR, Rosenbaum JT. Anterior uveitis: current concepts of pathogenesis and interactions with the spondyloarthropathies. Curr Opin Rheumatol. 2002;14(4):337–41.
Bacchiega ABS, Balbi GGM, Ochtrop MLG, de Andrade FA, Levy RA, Baraliakos X. Ocular involvement in patients with spondyloarthritis. Rheumatology (Oxford). 2017;56(12):2060–7.
Gutteridge IF, Hall AJ. Acute anterior uveitis in primary care. Clin Exp Optom. 2007;90(2):70–82.
O’Rourke M, Haroon M, Alfarasy S, Ramasamy P, FitzGerald O, Murphy CC. The effect of anterior uveitis and previously undiagnosed spondyloarthritis: results from the DUET cohort. J Rheumatol. 2017;44(9):1347–54.
Ward MM, Deodhar A, Gensler LS, Dubreuil M, Yu D, Khan MA, et al. 2019 update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritis. Arthritis Care Res (Hoboken). 2019;71(10):1285–99.
van der Heijde D, Ramiro S, Landewé R, Baraliakos X, Van den Bosch F, Sepriano A, et al. 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis. 2017;76(6):978–91.
Guignard S, Gossec L, Salliot C, Ruyssen-Witrand A, Luc M, Duclos M, et al. Efficacy of tumour necrosis factor blockers in reducing uveitis flares in patients with spondylarthropathy: a retrospective study. Ann Rheum Dis. 2006;65(12):1631–4.
Braun J, Baraliakos X, Listing J, Sieper J. Decreased incidence of anterior uveitis in patients with ankylosing spondylitis treated with the anti-tumor necrosis factor agents infliximab and etanercept. Arthritis Rheum. 2005;52(8):2447–51.
Lie E, Lindström U, Zverkova-Sandström T, Olsen IC, Forsblad-d’Elia H, Askling J, et al. Tumour necrosis factor inhibitor treatment and occurrence of anterior uveitis in ankylosing spondylitis: results from the Swedish biologics register. Ann Rheum Dis. 2017;76(9):1515–21.
Calvo-Río V, Blanco R, Santos-Gómez M, Rubio-Romero E, Cordero-Coma M, Gallego-Flores A, et al. Golimumab in refractory uveitis related to spondyloarthritis. Multicenter study of 15 patients. Semin Arthritis Rheum. 2016;46(1):95–101.
van Denderen JC, Visman IM, Nurmohamed MT, Suttorp-Schulten MS, van der Horst-Bruinsma IE. Adalimumab significantly reduces the recurrence rate of anterior uveitis in patients with ankylosing spondylitis. J Rheumatol. 2014;41(9):1843–8.
van Bentum RE, Heslinga SC, Nurmohamed MT, Gerards AH, Griep EN, Koehorst C, et al. Reduced occurrence rate of acute anterior uveitis in ankylosing spondylitis treated with golimumab—the GO-EASY study. J Rheumatol. 2019;46(2):153–9.
Rudwaleit M, Rødevand E, Holck P, Vanhoof J, Kron M, Kary S, et al. Adalimumab effectively reduces the rate of anterior uveitis flares in patients with active ankylosing spondylitis: results of a prospective open-label study. Ann Rheum Dis. 2009;68(5):696–701.
Lindström U, Bengtsson K, Olofsson T, Di Giuseppe D, Glintborg B, Forsblad-d’Elia H, et al. Anterior uveitis in patients with spondyloarthritis treated with secukinumab or tumour necrosis factor inhibitors in routine care: does the choice of biological therapy matter? Ann Rheum Dis. 2021;80(11):1445–52.
Landewé R, Braun J, Deodhar A, Dougados M, Maksymowych WP, Mease PJ, et al. Efficacy of certolizumab pegol on signs and symptoms of axial spondyloarthritis including ankylosing spondylitis: 24-week results of a double-blind randomised placebo-controlled phase 3 study. Ann Rheum Dis. 2014;73(1):39–47.
CIMZIA (certolizumab pegol). Product information. Smyrna: UCB Inc; 2019.
Rudwaleit M, Rosenbaum JT, Landewé R, Marzo-Ortega H, Sieper J, van der Heijde D, et al. Observed incidence of uveitis following certolizumab pegol treatment in patients with axial spondyloarthritis. Arthritis Care Res (Hoboken). 2016;68(6):838–44.
Landewé RB, van der Heijde D, Dougados M, Baraliakos X, Van den Bosch FE, Gaffney K, et al. Maintenance of clinical remission in early axial spondyloarthritis following certolizumab pegol dose reduction. Ann Rheum Dis. 2020;79(7):920–8.
Landewé R, van der Heijde D, Dougados M, Baraliakos X, Van den Bosch F, Gaffney K, et al. Induction of sustained clinical remission in early axial spondyloarthritis following certolizumab pegol treatment: 48-week outcomes from C-OPTIMISE. Rheumatol Ther. 2020;7(3):581–99.
van der Horst-Bruinsma I, van Bentum R, Verbraak FD, Rath T, Rosenbaum JT, Misterska-Skora M, et al. The impact of certolizumab pegol treatment on the incidence of anterior uveitis flares in patients with axial spondyloarthritis: 48-week interim results from C-VIEW. RMD Open. 2020;6(1):e001161.
van der Horst-Bruinsma IE, van Bentum RE, Verbraak FD, Deodhar A, Rath T, Hoepken B, et al. Reduction of anterior uveitis flares in patients with axial spondyloarthritis on certolizumab pegol treatment: final 2-year results from the multicenter phase IV C-VIEW study. Ther Adv Musculoskelet Dis. 2021;13:1759720x211003803.
van der Heijde D, Dougados M, Landewé R, Sieper J, Maksymowych WP, Rudwaleit M, et al. Sustained efficacy, safety and patient-reported outcomes of certolizumab pegol in axial spondyloarthritis: 4-year outcomes from RAPID-axSpA. Rheumatology (Oxford). 2017;56(9):1498–509.
Deodhar A, Gensler LS, Kay J, Maksymowych WP, Haroon N, Landewé R, et al. A fifty-two-week, randomized, placebo-controlled trial of certolizumab pegol in nonradiographic axial spondyloarthritis. Arthritis Rheumatol. 2019;71(7):1101–11.
Rademacher J, Poddubnyy D, Pleyer U. Uveitis in spondyloarthritis. Ther Adv Musculoskelet Dis. 2020;12:1759720x20951733.
Rosenbaum JT, Smith JR. Anti-TNF therapy for eye involvement in spondyloarthropathy. Clin Exp Rheumatol. 2002;20(6 Suppl 28):S143–5.
Frantz C, Portier A, Etcheto A, Monnet D, Brezin A, Roure F, et al. Acute anterior uveitis in spondyloarthritis: a monocentric study of 301 patients. Clin Exp Rheumatol. 2019;37(1):26–31.
de Winter JJ, van Mens LJ, van der Heijde D, Landewé R, Baeten DL. Prevalence of peripheral and extra-articular disease in ankylosing spondylitis versus non-radiographic axial spondyloarthritis: a meta-analysis. Arthritis Res Ther. 2016;18(1):196.
Zeboulon N, Dougados M, Gossec L. Prevalence and characteristics of uveitis in the spondyloarthropathies: a systematic literature review. Ann Rheum Dis. 2008;67(7):955–9.
Wright GC, Kaine J, Deodhar A. Understanding differences between men and women with axial spondyloarthritis. Semin Arthritis Rheum. 2020;50(4):687–94.
Hernández M, Mesquida M, Llorens V, Maza MSDL, Blanco R, Calvo V, et al. THU0381 certolizumab pegol is effective in uveitis associated to spondyloarthritis refractory to other tumour necrosis factor inhibitors. Ann Rheum Dis. 2017;76(Suppl 2):350.
Llorenç V, Mesquida M, Sainz-de-la-Maza M, Blanco R, Calvo V, Maíz O, et al. Certolizumab pegol, a new anti-TNF-α in the armamentarium against ocular inflammation. Ocul Immunol Inflamm. 2016;24(2):167–72.
Fabiani C, Vitale A, Rigante D, Emmi G, Lopalco G, Sota J, et al. Efficacy of anti-tumour necrosis factor-α monoclonal antibodies in patients with non-infectious anterior uveitis. Clin Exp Rheumatol. 2019;37(2):301–5.
Tosi GM, Sota J, Vitale A, Rigante D, Emmi G, Lopalco G, et al. Efficacy and safety of certolizumab pegol and golimumab in the treatment of non-infectious uveitis. Clin Exp Rheumatol. 2019;37(4):680–3.
Prieto-Peña D, Calderón-Goercke M, Adán A, Chamorro-López L, Maíz-Alonso O, De Dios-Jiménez Aberásturi JR, et al. Efficacy and safety of certolizumab pegol in pregnant women with uveitis. Recommendations on the management with immunosuppressive and biologic therapies in uveitis during pregnancy. Clin Exp Rheumatol. 2021;39(1):105–14.
Martín-Varillas JCRV, Sanchez-Bilbao L, Gonzalez-Mazon I, Torre I, García Martos A, Sánchez Andrade A, García Aparicio A, De Dios J, Urriticoechea A, Maiz Alonso O, Veroz R, García Valle A, Rodriguez Montero S, Miguelez R, Jovani V, Hernandez Garfella M, Conesa A, Martinez Gonzalez O, Rubio Muñoz P, Peña Sainz-Pardo E, González-Gay M, Blanco R. Treatment with certolizumab pegol in refractory uveitis secondary to immune-mediated inflammatory diseases multicenter study of 39 patients [abstract]. Arthritis Rheumatol. 2020;79:384–5.
Robinson PC, Claushuis TA, Cortes A, Martin TM, Evans DM, Leo P, et al. Genetic dissection of acute anterior uveitis reveals similarities and differences in associations observed with ankylosing spondylitis. Arthritis Rheumatol. 2015;67(1):140–51.
Lim CSE, Sengupta R, Gaffney K. The clinical utility of human leucocyte antigen B27 in axial spondyloarthritis. Rheumatology (Oxford). 2018;57(6):959–68.
Baraliakos X, Braun J. Non-radiographic axial spondyloarthritis and ankylosing spondylitis: what are the similarities and differences? RMD Open. 2015;1(Suppl 1): e000053.
Robinson PC, Wordsworth BP, Reveille JD, Brown MA. Axial spondyloarthritis: a new disease entity, not necessarily early ankylosing spondylitis. Ann Rheum Dis. 2013;72(2):162–4.
Protopopov M, Poddubnyy D. Radiographic progression in non-radiographic axial spondyloarthritis. Expert Rev Clin Immunol. 2018;14(6):525–33.
Acknowledgements
The authors acknowledge Simone E. Auteri, MSc EMS PhD, UCB Pharma, Milan, Italy for publication coordination and Jane Spingardi, DPhil, from Costello Medical, UK, for medical writing and editorial assistance based on the authors’ input and direction.
Funding
This manuscript, the graphical abstract, and the journal’s Rapid Service Fee were sponsored by UCB Pharma.
Medical Writing and Editorial Assistance
Support for third-party writing assistance for this article, provided by Jane Spingardi, DPhil, Costello Medical, UK, was funded by UCB Pharma in accordance with Good Publication Practice (GPP3) guidelines http://www.ismpp.org/gpp3.
Author Contributions
Substantial contributions to study conception and design: I.E.v.d.H.B., P.C.R., E.G.F., F.D.V., M.K., T.K., L.B., B.H., A.D.; substantial contributions to analysis and interpretation of the data: I.E.v.d.H.B., P.C.R., E.G.F., F.D.V., M.K., T.K., L.B., B.H., A.D.; drafting the article or revising it critically for important intellectual content: I.E.v.d.H.B., P.C.R., E.G.F., F.D.V., M.K., T.K., L.B., B.H., A.D.; final approval of the version of the article to be published: I.E.v.d.H.B., P.C.R., E.G.F., F.D.V., M.K., T.K., L.B., B.H., A.D.
Disclosures
Irene E. van der Horst-Bruinsma: honoraria/consulting fees/research grants from AbbVie, BMS, MSD, Novartis, Pfizer, and UCB Pharma. Philip C. Robinson: personal fees from AbbVie, Atom Biosciences, Eli Lilly, Gilead, Janssen, Novartis, Roche, Pfizer, and UCB Pharma; meeting attendance support from Bristol Myers Squibb, Lilly, Pfizer, and Roche; grant funding from Janssen, Novartis and UCB Pharma. Ennio G. Favalli: honoraria/consulting fees from AbbVie, Bristol Myers Squibb, Celltrion, Eli Lilly, Galapagos, Janssen, MSD, Novartis, Pfizer, Roche, Sandoz, Janssen, and UCB Pharma. Frank D. Verbraak: consulting fees/research grants from Bayer, Novartis, IDxDR, UCB Pharma. Mindy Kim, Thomas Kumke, Lars Bauer, and Bengt Hoepken: employees and stockholders of UCB Pharma. Atul Deodhar: speaker for Janssen, Novartis Pfizer, and UCB Pharma; consulting fees from AbbVie, Amgen, Aurinia, Bristol Myers Squibb, Celgene, Eli Lilly, GSK, Janssen, MoonLake, Novartis, Pfizer, and UCB Pharma; research grants from AbbVie, Bristol Myers Squibb, Celgene, Eli Lilly, GSK, Novartis, Pfizer, and UCB Pharma.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
van der Horst-Bruinsma, I.E., Robinson, P.C., Favalli, E.G. et al. Certolizumab Pegol Treatment in Patients with Axial-Spondyloarthritis-Associated Acute Anterior Uveitis: a Narrative Review. Rheumatol Ther 9, 1481–1497 (2022). https://doi.org/10.1007/s40744-022-00486-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-022-00486-1