Abstract
Neuroimaging techniques such as head computed tomography (CT) are frequently used to guide neurosurgical and neurocritical care of civilian and military patients with severe traumatic brain injury (sTBI). Although less widely available, brain magnetic resonance imaging (MRI) enhances detection of traumatic axonal injury and therefore improves the accuracy of outcome prediction for patients with sTBI. Nevertheless, over the past several years, emerging evidence has revealed that conventional MRI also has limitations as a prognostic tool in sTBI. Thus, there is growing interest in the development of advanced imaging techniques to guide prognostication and therapeutic decision-making. These advanced imaging techniques enable measurement of the brain’s structural and functional connectivity, as well as its perfusion, metabolism, and responses to stimuli. In this review, we discuss the clinical applications and limitations of head CT and conventional MRI, as well as evidence demonstrating that advanced imaging techniques may improve the accuracy of prognostication for patients with sTBI.
Similar content being viewed by others
Introduction
Neuroimaging tools such as head computed tomography (CT) and brain magnetic resonance imaging (MRI) are critical to acute decision-making and long-term prognostication for the tens of thousands of civilians who experience a severe traumatic brain injury (sTBI) in the USA each year [1], as well as the thousands of military personnel who have experienced a sTBI since the start of the wars in Afghanistan and Iraq [2]. However, both head CT and conventional brain MRI have limitations as prognostic tools, which has led to growing interest in the development of advanced imaging techniques to improve the accuracy of prognostication for patients with sTBI. This review aims to provide an overview of how head CT and conventional MRI are currently used in the clinical care of patients with sTBI, as well as a summary of recent advances in structural and functional neuroimaging techniques that have the potential for future integration into clinical practice. Evidence demonstrating the potential prognostic utility of each advanced imaging technique is discussed, with consideration of the feasibility of clinical implementation. Furthermore, the recommendations of the Federal Interagency Initiative on Common Data Elements [3, 4] and the Brain Trauma Foundation [5] pertaining to each imaging technique are presented, wherever applicable. For the purpose of this review, we consider conventional MRI to include sequences that are widely available on clinical scanners, which include T2-weighted fluid-attenuated inversion recovery (T2-FLAIR), gradient-recalled echo (GRE), and diffusion-weighted imaging (DWI).
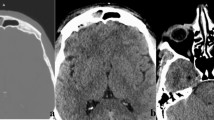
Head Computed Tomography
Head computed tomography (CT) continues to be the preferred technique for acute diagnostic evaluation of patients with sTBI because of its accessibility, speed of acquisition, and its ability to detect skull fractures and large intracranial hemorrhages that require urgent neurosurgical intervention. Furthermore, CT findings are routinely used to guide decision-making about intracranial pressure (ICP) monitoring [5]. CT grading systems, such as the Marshall CT classification [6] and Rotterdam CT score [7], have been developed to assess the severity of intracranial injury. Although early head CT is rarely used for long-term prognostication, elements of both the Marshall and the Rotterdam CT grading systems have been incorporated into prognostic models, such as the International Mission for Prognosis and Analysis of Clinical Trials in TBI (IMPACT) [8, 9] and the Medical Research Council (MRC) CRASH [10] models.
After the initial diagnostic evaluation in the Emergency Department is completed, head CT is routinely used for follow-up imaging of sTBI patients admitted to the intensive care unit (ICU). There are no consensus guidelines regarding the frequency or total number of repeat head CTs that should be performed, and hence, decisions about follow-up imaging are typically made on an individualized basis. The Brain Trauma Foundation Guidelines suggest that head CT data should be used in conjunction with the clinical examination and ICP data to guide therapeutic decision-making [11], but thresholds for ICP and examination changes that should trigger a repeat head CT have not been precisely defined. In the Common Data Element Guidelines for TBI, a neurologic decline, or “neuroworsening,” is defined as (1) a decrease in Glasgow Coma Scale (GCS) motor score ≥2 points compared with previous examination, (2) a new loss of pupillary reactivity, development of pupillary asymmetry ≥2 mm, or (3) deterioration in neurological status sufficient to warrant immediate medical or surgical intervention [12]. Such neuroworsening may be considered an appropriate threshold for triggering a repeat head CT scan to assess for development of new lesions and/or evolution of previously observed lesions causing new mass effect.
It remains uncertain whether neuroimaging provides additional or similar information as continuous neuromonitoring utilizing invasive probes [13–19] or noninvasive cerebral hemodynamic and electrophysiologic methods [20–23]. While a detailed discussion of the latter methods is outside the scope of this review, multiple imaging studies have sought to assess how imaging may facilitate detection of edema, tissue shifts, and herniation in order to guide management. Chesnut et al. [24] examined the relative utility of brain imaging and clinical examination (ICE) with or without the addition of invasive intracranial pressure monitoring (PM). Imaging was recommended to occur at least three times: at baseline, at 48 h, and at 5–7 days following injury. The ICE standard alone had no significant difference from PM added to the ICE standard, either in a composite primary clinical outcome or in secondary outcomes including mortality at 14 days, mortality at 6 months, and Glasgow Outcome Scale-Extended scores at 6 months. These results raised the possibility that screening for secondary injury with neuroimaging provides a benefit not augmented by PM. While the follow-up rate of ascertaining the primary clinical outcome measures was excellent, generalizing the results to routine practice is not possible given several limitations: the low rate of acute enrollment, variable expertise with PM strategies in the Bolivian and Ecuadorian study sites, uncertain access to post-discharge acute rehabilitation, and disparities in the treatment allocation within each allocation group. Examples of treatment disparities between groups reflect differences in the treatment protocols for each group: ICE with PM patients received a higher rate of high-dose barbiturates (24 vs. 13 %), a higher rate of neuromuscular blockade (11 vs. 5 %), and lower rate of hypertonic saline (58 vs. 72 %) than patients receiving ICE alone. Some of these differences in pharmacologic strategies relate to the prescribed order of therapy in each treatment group.
In addition to the use of CT for the detection of cerebral edema and tissue shifts, CT angiography has enabled the diagnosis of cerebral vasospasm following TBI. This phenomenon has been documented with a variety of imaging tools including Doppler ultrasonography, digital subtraction angiography, Xenon CT, CT angiography, and MR angiography [25–30]. Traumatic vasospasm is observed in patients with and without traumatic subarachnoid hemorrhage and in both closed and penetrating injuries [27]. The prevalence in patients with moderate-to-severe TBI has ranged from 27 to 68 % [31]. While vasospasm occurs with increasing frequency in patients with severe or widespread injury, it has been not definitively demonstrated to be a pathogenic mediator of poor outcome, although it may respond to hemodynamic or catheter-based interventions [25, 32].
Conventional Magnetic Resonance Imaging
Conventional MRI is often not feasible during the acute stage of sTBI because of lack of access, prolonged data acquisition time, or clinical factors that preclude MRI (e.g. raised ICP or penetrating injury with a metallic object). Nevertheless, conventional MRI utilizing T2-FLAIR, GRE, DWI, and derived apparent diffusion coefficient (ADC) maps provides better detection of traumatic axonal injury (TAI) than does CT [33–36]. Given that TAI is the most devastating subtype of traumatic injury from a prognostic standpoint [37], conventional MRI is a more useful prognostic tool than is CT [33, 38–40]. White matter ADC is particularly useful for predicting outcomes, with a recent study demonstrating that ADC values in the whole-brain white matter and in the corpus callosum correlate with functional outcome in sTBI patients at hospital discharge [41]. Of note, in contrast to ischemic stroke, diffusion restriction (bright signal on DWI and dark signal on ADC) is often not associated with irreversible, cytotoxic edema in sTBI. Rather, this radiologic finding may be caused by transient, reversible intracellular edema in patients with sTBI. Indeed, there are reports of neurological recovery in sTBI patients despite evidence of extensive TAI-related diffusion restriction [42, 43]. These observations are consistent with animal studies showing that TAI may be reversible when shear-strain forces do not cause acute, primary axotomy [44]. Thus, the term “cytotoxic edema” should be used with caution when describing TAI-related diffusion restriction, since these lesions may not lead to secondary axotomy or neuronal death. Moreover, the potential reversibility of TAI-related signal abnormalities on DWI/ADC suggests a longer window for therapeutic intervention in sTBI as compared to ischemic stroke.
It has long been recognized that the shear-strain forces that transiently injure or permanently sever axons in TAI also cause disruption of the brain’s microvasculature, resulting in extravasation of blood [45]. Whereas CT studies in the 1990s found that microhemorrhages, also known as traumatic microbleeds (TMBs), are associated with approximately 20 % of radiologically apparent TAI lesions [46], the application of the GRE sequence subsequently demonstrated that up to 80 % of TAI lesions may be associated with TMBs [36, 47]. The pathophysiological link between vessel disruption and axonal injury suggests that the presence of TAI can be inferred when a TMB is present. Even if evidence of axonal pathology (i.e., signal change on T2 FLAIR or DWI) is not identified, the presence of a TMB is considered in the Common Data Element Guidelines as sufficient evidence of hemorrhagic TAI [3]. Supporting this assumption are studies showing that the total number of TMBs correlates with admission GCS score [47–49], duration of post-traumatic unconsciousness [48, 50], and neurological recovery [48, 50]. Yet, while GRE identification of TMBs has been correlated with acute TBI severity and outcomes, prior studies have not consistently demonstrated that GRE predicts long-term outcomes [36, 47, 50–52]. These results highlight the need for advanced imaging techniques that are more sensitive for detection of both hemorrhagic and non-hemorrhagic TAI and thus potentially more useful for prognosis.
Motivation for Advanced Imaging Techniques in Prognostication
Recovery of consciousness, communication, and functional independence is possible in both civilian [38, 43, 53–55] and military [56] patients after sTBI. Indeed, recent evidence from the US Department of Veterans Affairs “Emerging Consciousness” Program and the Traumatic Brain Injury Model Systems suggests that a majority of patients with sTBI ultimately recover consciousness [54, 57, 58]. Thus, it is critical to identify patients with sTBI who have the potential for a meaningful functional improvement.
Further motivating the application of advanced imaging techniques to prognostication in patients with sTBI are data demonstrating that bedside neurological examinations are often inaccurate for patients with traumatic disorders of consciousness (DOC). A misdiagnosis rate of up to 43 % has been reported in cases of consensus-based diagnosis of post-traumatic vegetative state (VS) [59–61] when compared to a standardized neurobehavioral evaluation with the Coma Recovery Scale-Revised [62]. This concerning statistic may be related to fluctuations in arousal or deficits in visual, auditory, motor, or language function that limit a patient’s ability to demonstrate purposeful behavior [61]. The high misdiagnosis rate in patients with traumatic DOC has significant implications for prognosis, since patients in post-traumatic minimally conscious state (MCS) have greater potential for functional recovery than those in post-traumatic VS [63, 64].
Given the prognostic limitations of CT and MRI, as well as the risk of misdiagnosing a patient’s level of consciousness using a standard bedside neurological examination, interest has grown in recent years in developing advanced neuroimaging techniques to more accurately determine the brain’s structural connectivity, functional activity, and, hence, potential for recovery. In the next section of this review, we provide an overview of recent advances in structural and functional neuroimaging techniques that are relevant to diagnosing states of consciousness and predicting outcomes in patients with sTBI. We highlight the potential clinical utility of advanced techniques such as susceptibility-weighted imaging (SWI), diffusion tensor imaging (DTI), diffusion tensor tractography (DTT), stimulus-based functional MRI (fMRI), resting-state fMRI (rs-fMRI), arterial spin-labeled (ASL) perfusion MRI, positron emission tomography (PET), and magnetic resonance spectroscopy (MRI) and discuss future directions for further study. The methodological principles of each advanced imaging technique are briefly introduced, but a detailed discussion of advanced imaging methods is beyond the scope of this review and can be found elsewhere [65, 66].
Advanced Imaging Techniques
Susceptibility-Weighted Imaging
SWI significantly enhances the detection of blood products beyond the level of detection provided by GRE. This increased sensitivity for blood is enabled by advances in both data acquisition and data post-processing [67]. Specifically, SWI combines data regarding both the magnitude and the phase of the blood products’ susceptibility effects within the magnetic field to produce an image with enhanced signal contrast. Accordingly, SWI detects more foci of hemorrhagic TAI than GRE does [48, 49, 68]. Furthermore, initial studies suggest that the total number and volume of TMBs detected by SWI correlate with functional outcomes after TBI [48], whereas earlier GRE studies did not consistently demonstrate such a correlation [36, 47, 51, 52]. The reason(s) for SWI’s increased predictive value remains unclear. SWI is particularly sensitive for detecting TMBs in the brainstem [48, 68], a region in which unilateral and bilateral lesions are associated with odds ratios of 8 and 182, respectively, for poor outcome on the Glasgow Outcome Scale-Extended [38]. It is thus possible that SWI improves the accuracy of prognostication by identifying hemorrhagic TAI in regions where lesions are particularly predictive of outcomes.
An important methodological consideration in interpreting SWI data in patients with sTBI is the magnetic field strength at which the SWI data are acquired. Hemorrhagic TAI is more readily detected at 3 T as compared to 1.5 T [69] due to increased sensitivity to susceptibility effects at higher field strengths. In addition, the spatial resolution of the SWI data (i.e., voxel size) may influence the number of TMBs that are detected [70]. Thus, SWI data obtained from different patients or longitudinally in a single patient can only be compared when magnetic field strength and imaging acquisition parameters are the same. SWI has already been implemented into routine clinical practice in many centers and is currently listed as a Tier 1 sequence in the Common Data Element guidelines [3]. We recommend the use of SWI at 3 T, whenever available, to assess the burden of hemorrhagic TAI in patients with sTBI.
Diffusion Tensor Imaging
Whereas DWI measures the mean diffusivity of water, DTI characterizes the directional diffusion of water within the brain [71]. This directionality can be quantified using a unitless scalar called fractional anisotropy (FA), where 0 is defined as completely non-directional (i.e., isotropic) diffusion and 1 is defined as completely directional (i.e., anisotropic) diffusion. The aspect of FA measurements that is of particular relevance to sTBI is its ability to detect structural changes in the white matter axons that are susceptible to TAI. Low FA in the white matter has been correlated with histopathological evidence of TAI in experimental animal models [72, 73]. In addition, low FA in white matter regions that are known to be susceptible to TAI (e.g., corpus callosum and internal capsules) is associated with a broad range of neurological deficits in patients with sTBI [74–83]. Moreover, FA in specific white matter bundles correlates with neurocognitive functions that are associated with those bundles.
The emerging evidence that FA provides a valid, clinically relevant assessment of white matter integrity suggests that clinical implementation of DTI may be approaching. Indeed, DTI is currently listed in Tier 2 of the recommended protocols in the Common Data Elements guidelines [3]. Yet, clinical translation of DTI is currently limited by several methodological factors. For example, both the imaging hardware (i.e., the MRI scanner) and software (i.e., the DTI sequence) may affect the measurement of directional diffusion. Thus, the prognostic utility of DTI-based FA measurements is still being debated, pending harmonization of methods within and across institutions. At the present time, the Common Data Element Guidelines provide recommendations for DTI sequences that can be performed on both 1.5- and 3-T MRI scanners [3].
Diffusion Tensor Tractography
Diffusion tensor tractography (DTT) enables three-dimensional analysis of white matter connectivity. The principle upon which tractography is based is that as long as the primary diffusion directions of the tensors in adjacent voxels are coherent, these tensors can be reconstructed as a fiber tract. A fiber tract can therefore be conceptualized as a “streamline” of connected vectors along a single deterministic path, hence the term “deterministic streamline tractography” [84]. Fiber tracts are typically calculated by manually tracing or automatically segmenting a white matter region, such as the corpus callosum, and then using this ROI as a “seed” for the generation of three-dimensional fiber tracts passing through it. Another tractography technique developed by Behrens and colleagues called probabilistic tractography [85] aims to account for the inherent uncertainty in fiber tract direction at each voxel. As opposed to the deterministic tractography model, which creates a single streamline passing through adjacent voxels, the probabilistic tractography model generates a distribution of all possible streamlines that may pass through these voxels. Regardless of which methodology is being used, it is important to emphasize that tractography is an inferential technique in which white matter tracts are reconstructed on the basis of water diffusion measurements. The number of fiber tracts that is calculated in any tractography analysis is significantly affected by data acquisition parameters, such as the spatial resolution (i.e., voxel size) and angular resolution (i.e., number of directional diffusion measurements). Although studies have begun to validate tractography with “gold standard” histopathology data [86, 87], DTT results should always be interpreted with caution given the inherent limitations of the technique [88, 89].
The application of DTT to the study of sTBI is based on the ability of tractography to identify alterations in white matter connectivity, as well as changes in the mean FA, number of fiber tracts, average tract length, and total volume of a white matter bundle. Wang and colleagues found that early DTT (mean day 7) identified fiber tract damage in the corpus callosum, fornix, and cerebral peduncle projections in 12 patients with sTBI as compared to age- and gender-matched controls [90]. Furthermore, mean FA, fiber number, and fiber length in subregions of the corpus callosum correlated with TBI patients’ functional outcome scores on the Glasgow Outcome Scale-Extended at a mean follow-up of 8 months. A subsequent longitudinal study involving 28 patients with mild-to-severe TBI demonstrated that DTT identifies structural connectivity changes between the acute (days 0–9) and chronic (6–14 months) periods and that DTT measurements of structural connectivity in both the acute and chronic periods predicted neurocognitive test results [91]. Newcombe and colleagues provided additional support for the utility of DTT as a diagnostic and prognostic tool in TBI by showing that patients in post-traumatic VS have a different pattern of white matter injury than patients in post-anoxic VS [92]. Specifically, DTT demonstrated preferential damage of brainstem fiber tracts, a finding that is consistent with histopathological and biomechanical studies showing that the brainstem is susceptible to rotational shear-strain forces in sTBI [37, 93–95]. Similarly, DTT studies of moderate and severe TBI patients indicate that the corpus callosum, which is also known to be susceptible to shear-strain forces in TAI [37], undergoes volume loss, shortening of fiber tracts, a decrease in mean FA, and a decline in total tract number in the subacute and chronic stages of injury [76, 96, 97]. Finally, a recent study of 52 patients with DOC (32 sTBI) by Fernandez-Espejo and colleagues demonstrated that DTT-based measurements of connectivity within the default mode network (DMN), a brain network believed to be involved in self-awareness, correlated with patients’ level of consciousness on behavioral testing [98••] (see resting-state fMRI section below for additional DMN studies in sTBI). This DTT analysis suggests that structural connectivity data may provide critical information about the brain’s potential for conscious awareness in patients with traumatic DOC.
Stimulus-Based Functional Magnetic Resonance Imaging
For the purpose of predicting outcomes in patients with sTBI, the most commonly used stimulus-based fMRI technique relies upon the blood-oxygen-level-dependent (BOLD) signal. This BOLD signal is considered a surrogate for cerebral blood flow and, hence, neuronal metabolic activity, as long as the brain’s activation-flow coupling response is intact. Notably, multiple types of intracranial pathology in patients with sTBI, such as elevated ICP and peri-contusional edema, may disrupt the coupling between neuronal activation and cerebral blood flow, and thus, stimulus-based BOLD fMRI results must be analyzed with careful consideration of this potential confounder, as well as other confounders like sedation and patient motion.
BOLD stimulus-based fMRI analyses are typically performed using a block design, in which stimuli are presented in discreet epochs (often 16 s to 1 min), with the BOLD signal during the stimulus blocks (“on”) compared to the BOLD signal during a control-block (“off”), such as a rest period. Brain “activation maps” are then derived from regions with statistically significant differences in the BOLD signal between on and off periods and may be complementary to data derived from similar electroencephalography (EEG) paradigms [99, 100••]. In a recent study of 44 patients with DOC, 28 of whom experienced a sTBI, Forgacs and colleagues demonstrated that the four subjects (three with sTBI) who were able to demonstrate command following during an fMRI motor imagery task (i.e., “covert” command following) also had evidence of normal or near-normal background organization on the EEG while awake, as well as spindles while asleep [100••]. Furthermore, all four subjects demonstrated relative preservation of cortical metabolic activity when studied with (18F)-fluorodeoxygluose (FDG) PET. These correlative fMRI-EEG-PET findings suggest that stimulus-based fMRI results may indeed reflect the brain’s functional capacity for cognition, albeit in a covert manner when injury to motor pathways limits the patient’s capacity for self-expression at the bedside.
In considering data from fMRI studies in patients with sTBI, it is important to recognize that most studies have been performed in the subacute-to-chronic stage of injury, as opposed to the acute stage when prognostic data are potentially of greater value to the clinician and family. This limitation reflects the difficulty of acquiring fMRI data in the acute stage of sTBI, since intracranial hypertension, hemodynamic instability, motor restlessness, and a variety of other clinical factors may preclude acute fMRI. Nevertheless, the potential clinical utility of fMRI has been suggested by studies showing that abnormal brain activation patterns detected by fMRI correlate with a broad range of neurocognitive and functional deficits in patients with sTBI, including memory impairment [82, 101] and motor dysfunction [102]. For patients with traumatic DOC, fMRI has also challenged classical concepts about the diagnosis of consciousness. In one of several groundbreaking studies, a 23-year-old woman in a traumatic VS was asked to perform motor and spatial imagery tasks (imagining playing tennis or walking through her house) while undergoing BOLD fMRI [103]. The BOLD activation patterns in the patient were similar to those observed in healthy controls, despite the absence of any behavioral evidence of awareness of self or environment on detailed neurological examination.
The suggestion that fMRI may reveal cognitive processing that is undetectable on bedside examination has been reproduced in patients with MCS and VS using a variety of motor imagery, spatial imagery, language, and visual fMRI paradigms [92, 104–116, 117••, 118, 119] (Table 1). Monti and colleagues found that five of 54 patients with DOC (23 in VS and 31 in MCS; 33 with sTBI) had brain activation patterns during command-following paradigms involving motor and spatial imagery that were similar to controls (all five patients had traumatic DOC). One subject in traumatic MCS answered questions while in the MRI scanner by linking the two imagery tasks described above to “yes” and “no” answers [117••]. Collectively, these studies suggest that stimulus-based fMRI may provide evidence of conscious awareness that evades detection on bedside examination. In addition, the potential prognostic utility of these fMRI paradigms was shown in a recent study in which language-related fMRI activation correlated with behavioral recovery 6 months after the fMRI scan [104]. Although the fMRI data for the 41 patients (22 VS, 19 MCS; 11 TBI) were acquired in the subacute-to-chronic stages of recovery (2 to 122 months), the correlation between fMRI data and subsequent behavioral outcomes suggests that acute fMRI may provide similar prognostic utility.
Resting-State Functional Magnetic Resonance Imaging
Rs-fMRI is based on the principle that spontaneous fluctuations in brain activity are temporally correlated in functionally related brain regions. Identification of resting correlations in brain activity has led to the concept of “resting-state networks,” whose activity is higher at rest and lower during active tasks. The resting-state network that has received the most attention in patients recovering from sTBI is the DMN [122–125], which is believed to play an essential role in self-awareness, along with other internally directed cognitive processes. DMN connectivity is altered in patients recovering from sTBI [126–132] (Table 2), and longitudinal increases in DMN connectivity have been correlated with functional recovery [127]. Furthermore, the severity of DMN dysfunction may predict neurocognitive task performance [126, 128, 129]. Moreover, functional connectivity of cortical nodes within the DMN, as measured by rs-fMRI, correlates with the structural injury of white matter pathways connecting these nodes, as measured by DTI [126, 128, 129]. These correlative rs-fMRI/DTI findings suggest that functional connectivity measurements may be firmly rooted in structural neuroanatomy, a finding that is supported by studies of healthy control subjects [135, 136]. Perhaps most notably, the strength of functional connectivity within the DMN, as determined by rs-fMRI, has been to shown to correlate with the level of consciousness after severe brain injury [131].
Arterial Spin-Labeled Perfusion Magnetic Resonance Imaging
ASL perfusion MRI utilizes a radiofrequency pulse to label water protons in blood flowing through the carotid arteries. Inverting the spins of protons in this “endogenous bolus” provides an indirect measure of the cerebral blood flow as these spins dissipate in the distal cerebrovasculature. Unlike the BOLD signal, ASL perfusion maps provide a direct measurement of arterial blood flow that can theoretically be quantified in absolute units of cc/100 g/min if one has knowledge of the longitudinal relaxation rate of blood and tissue, as well as the labeling efficiency and arterial transit delays. The ASL signal should therefore correlate directly with neuronal activity as long as cerebrovascular autoregulation and activation-flow-coupling mechanisms are intact [137].
ASL perfusion imaging studies have revealed alterations in resting cerebral blood flow (CBF) in patients recovering from sTBI. In the chronic stage of moderate-to-severe TBI, global CBF may be reduced, as well as regional perfusion in the thalamus, posterior cingulate cortex, and frontal cortex [138]. Reductions in thalamic perfusion correlate with thalamic atrophy, suggesting that ASL perfusion measurements may be based upon the functional capacity of injured neurons. Furthermore, a correlation has been observed between decreased resting CBF and altered brain activation during an ASL fMRI working memory task [139]. These findings suggest that ASL measurements of resting CBF may be used to elucidate the brain’s functional potential for recovery.
Neuroimaging Correlates of Brain Metabolism
Positron Emission Tomography
In sTBI patients, FDG PET enables calculation of regional cerebral metabolic rate of glucose (CMRG) utilization. An early FDG PET study demonstrated “hyperglycolysis,” an increase in cerebral glucose utilization in all six patients with acute sTBI for whom the cerebral metabolic rate of oxygen could also be measured. Another five patients were found to have localized areas of hyperglycolysis near mass lesions [140]. These neuroimaging findings complement cerebral microdialysis studies in sTBI, which similarly suggest hyperglycolysis in the form of persistently low extracellular glucose in association with poor outcome without associated ischemia [141••].
FDG PET has also been utilized in the subacute-to-chronic phase of sTBI to predict outcomes in patients with traumatic DOC. A recent study by Bruno and colleagues demonstrated that MCS patients overall demonstrated reduced thalamic, caudate, and cortical metabolism; within the MCS group, patients characterized as “MCS+” (intelligible verbalization, yes/no responses, and/or command following) could be discriminated from patients characterized as “MCS−” (localization to noxious stimuli and/or visual pursuit of a stimulus) by the presence of increased left-hemispheric cortical metabolism, particularly in language, premotor, supplementary motor, and sensorimotor cortices [142]. Quantitative FDG PET to quantify CMRG using a standard arterial input based on healthy control patients demonstrated 82 % accuracy for distinguishing between patients in VS and MCS. This study also demonstrated that VS patients are likely to progress to MCS when CMRG threshold exceeded 45 % of normal [143]. A recent validation study by Stender and colleague showed similar utility for FDG PET in predicting outcomes in patients with DOC on the Glasgow Outcome Scale-Extended, with prognostic accuracy that was superior to that of concomitantly acquired stimulus-based fMRI data [141••].
Imaging Biomarkers of Seizures, Status Epilepticus, and Cortical Spreading Depolarization
Electrophysiologic mechanisms of injury frequently seen in sTBI, such as seizures, status epilepticus, and cortical spreading depolarizations (CSD), have only yielded indirect neuroimaging signatures. Nonconvulsive seizures may occur in over 20 % of sTBI patients undergoing EEG. These findings may affect cerebral metabolism as seen by increased FDG PET avidity in individual patients [100••] or as restricted diffusion along the cortical ribbon or thalamus [144]. sTBI patients diagnosed with status epilepticus have significantly greater hippocampal atrophy at follow-up compared to patients without status epilepticus (21 vs. 12 % atrophy) [100••].
CSD, unique from seizures, are prolonged neuronal depolarizations, which occur at a near 50 % rate in patients with sTBI. CSD are considered electrophysiologically akin to migraine, but in the setting of brain injury, they result in significant metabolic exhaustion and are accompanied by brain tissue hypoxia. CSD are associated with a more than doubling in the rate of poor clinical outcomes (60 vs. 26 %), and CSD clusters may result in regional isoelectric cortical activity, which was associated with universally poor outcomes in a case series of 53 monitored patients [145]. To date, however, CSD detection has relied mostly on invasive electrophysiology, limiting the feasibility of clinical trials targeting this biomarker. MRI-based penumbral perfusion-diffusion measurements during experimental paradigms to provoke CSD in animals have revealed ADC and CBF decrements of 20 and 40 %, respectively [134]. Other methods such as repeated DWI [146] or parenchymal spin-lock fMRI [147] may reflect pathogenic signatures, providing future directions toward identifying a neuroimaging biomarker of CSD.
Magnetic Resonance Spectroscopy
Proton MRS provides regional metabolic information complementary to repeated focal measures via cerebral microdialysis. While N-acetylaspartate (NAA), creatine, phosphocreatine, choline, inositol, and glucose are typically broadly decreased on MRS acutely after TBI [120], lactate levels are variable, potentially related to temporal differences between acute and subacute findings or due to the presence of nearby structural pathology. Within regions of cerebral contusion after sTBI, lactate may be either unchanged or elevated, whereas lactate is normal in regions without structural pathology on MRI [40, 120]. Another explanation for this variability may be that cerebral microdialysis measures cerebral lactate, often in association with a non-ischemic “glycolytic” pattern: elevated pyruvate, preserved brain tissue oxygenation, and normal CT perfusion measures of CBF [148]. Experimental animal models of TBI have raised yet another possible explanation; (13)-C-labeled glucose, lactate, and acetate administration has demonstrated metabolic uncoupling between glia and neurons, a phenomenon in which lactate uptake by neurons becomes impaired after injury while lactate production by glial cells persists [143]. From a prognostic standpoint, MRS may also reveal lesions that are undetectable to conventional MRI methods, thus providing the potential for improved accuracy of outcome prediction [78, 149]. At the present time, MRS is included in Tier 2 of the Common Data Elements Guidelines for TBI [3, 4].
Clinical Implementation of Advanced Imaging Techniques: Feasibility Considerations
Currently, stimulus-based fMRI has the most data supporting its use as a tool for detecting evidence of conscious awareness, which has significant prognostic relevance given that patients in post-traumatic MCS have greater potential for recovery than patients in post-traumatic VS. However, the administration of sedative medications during the acute stage of sTBI can alter a patient’s ability to respond to an imagery task or auditory stimulus [150], and therefore, stimulus-based fMRI may not be feasible in the acute setting. Similarly, sedating medications may confound PET-based assessments of cerebral metabolic activity. In contrast, rs-fMRI may be used to investigate resting-state networks across the spectrum of states of consciousness, throughout each stage of the sleep-wake cycle and even during anesthesia [151–153], although interpretation of the results may be confounded by altered metabolic status. A major advantage of ASL is its ability to provide direct repeated measurements of global and/or regional CBF before and after administration of a therapy. Thus, ASL may ultimately be used to detect individualized responses to stimulant medications [154]. Ultimately, the multimodal integration of task-based fMRI, rs-fMRI, PET, and ASL perfusion MRI is likely to provide the highest prognostic yield, since each technique provides potentially unique information about the functional status of the injured brain and its potential for recovery (Fig. 1). The optimal timing of performing these techniques requires a careful assessment of patient safety, as ICP may increase in the supine position, and invasive monitors may cause artifacts.
Task-based fMRI, resting-state fMRI, and arterial spin-labeled (ASL) perfusion MRI data from a 23-year-old woman scanned 146 days (5 months) after severe traumatic brain injury caused by a motor vehicle accident. At the time of the scan, the patient was in a minimally conscious state. In a, activation within the left (arrow) > right hemispheric peri-Sylvian language networks is observed during a passive language stimulus (spoken narrative). FMRI data processing was carried out using FMRI Expert Analysis Tool (FEAT) Version 5.98, part of FSL (FMRIB’s Software Library, www.fmrib.ox.ac.uk/fsl), and the color scalar bar indicates the Z scores. In b, an independent component resting-state fMRI analysis reveals that the posterior cingulate/precuneus region of the default mode network (arrow) retains partial functional connectivity with the inferior parietal lobules (arrowheads), but connectivity with the medial prefrontal cortex (asterisk) has been disrupted. Independent component analysis was carried out using probabilistic independent component analysis [66] as implemented in Multivariate Exploratory Linear Decomposition into Independent Components (MELODIC) Version 3.10, part of FSL. The color scalar bar indicates the thresholded independent component (IC) map, with yellow-red colors indicating positive correlations and blue colors indicating negative correlations (anticorrelations). In c, an ASL perfusion-weighted imaging (PWI) map using pulsed ASL demonstrates cerebral perfusion in the posterior cingulate/precuneus region (arrow) and thalami (arrowheads). The color scalar bar indicates relative cerebral perfusion. Reproduced from Edlow, Giacino, and Wu [66]
With regard to the feasibility of advanced structural imaging techniques such as DTI and DTT, it should be noted that acute sTBI may cause variable effects on FA due to intracellular and/or extracellular edema. By contrast, FA tends to more predictably decline in the subacute and chronic stages of sTBI [52, 75, 77–79, 155, 156]. For this reason, DTI and DTT may provide more prognostically relevant information once acute edema associated with sTBI has resolved. The optimal timing for acquisition of MRS data is currently also a matter of debate. Ultimately, clinicians must balance the goal of obtaining imaging data early enough to guide diagnosis, prognosis, and therapeutic decision-making with the goal of acquiring the data late enough that acute confounders are minimized.
Future Directions
Although major advances have occurred in the past few years in elucidating the structural and functional basis for recovery of awareness in patients with sTBI, current understanding about recovery of arousal (wakefulness) lags far behind. Arousal is critical to recovery of consciousness, since without arousal, awareness is not possible. The current lack of understanding about the mechanisms that enable recovery of arousal in patients with traumatic DOC can be explained by the inability of conventional imaging tools to map the complex neuroanatomic connectivity of the ascending reticular activating system (ARAS), an arousal network that connects nuclei in the brainstem to diencephalic, forebrain, and cortical targets. Indeed, the neuroanatomic connectivity of the human ARAS has only recently been mapped in preliminary ex vivo and in vivo tractography studies [55, 157, 158]. Rs-fMRI measurements of brainstem connectivity are also methodologically challenging to perform, although recent studies suggest that it may be possible in the near future to map the functional connectivity of brainstem networks that mediate arousal [159]. Delineating the structural and functional integrity of the ARAS is fundamentally important to predicting recovery after sTBI, because the human ARAS network appears to contain redundant circuitry that may enable recovery of arousal when some, but not all components of the network are disrupted [160]. Hence, it should be emphasized that the presence of brainstem TAI, or “grade 3 DAI,” does not invariably portend a poor outcome [43, 55].
Conclusions
The cardinal utility of neuroimaging in sTBI is to provide structural and function information about the brain’s potential for recovery, both to help clinicians tailor treatment to pathophysiologic phenotypes and to guide prognostication. Advanced imaging may provide a gateway to informing the timing and appropriateness of decompressive craniectomy, hemodynamic treatment of brain edema or vasospasm, and administration of therapies aimed at promoting recovery of consciousness in patients with traumatic DOC. Future clinical implementation of advanced imaging techniques will depend upon the establishment of standardized methods that are reproducible across centers and validated in clinical trials testing specific interventions.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Faul M, Xu L, Wald MM, et al. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002-2006. Atlanta: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010.
(DVBIC) DaVBIC. Defense Medical Surveillance System (DMSS) and Theater Medical Data Store (TMDS). (Numbers for 2000 - 2014 Q2). http://dvbic.dcoe.mil/dod-worldwide-numbers-tbi, 2014.
Haacke EM, Duhaime AC, Gean AD, et al. Common data elements in radiologic imaging of traumatic brain injury. J Magn Reson Imaging. 2010;32:516–43.
Duhaime AC, Gean AD, Haacke EM, et al. Common data elements in radiologic imaging of traumatic brain injury. Arch Phys Med Rehabil. 2010;91:1661–6.
Brain Trauma F, American Association of Neurological S, Congress of Neurological S, et al. Guidelines for the management of severe traumatic brain injury. VI. Indications for intracranial pressure monitoring. J Neurotrauma. 2007;24 Suppl 1:S37–44.
Marshall LF, Marshall SB, Klauber MR, et al. A new classification of head injury based on computerized tomography. J Neurosurg. 1991;75:S14–20.
Maas AI, Hukkelhoven CW, Marshall LF, et al. Prediction of outcome in traumatic brain injury with computed tomographic characteristics: a comparison between the computed tomographic classification and combinations of computed tomographic predictors. Neurosurgery. 2005;57:1173–82. discussion -82.
Murray GD, Butcher I, McHugh GS, et al. Multivariable prognostic analysis in traumatic brain injury: results from the IMPACT study. J Neurotrauma. 2007;24:329–37.
Steyerberg EW, Mushkudiani N, Perel P, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008;5:e165. discussion e.
Perel P, Arango M, Clayton T, et al. Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ. 2008;336:425–9.
Brain Trauma F, American Association of Neurological S, Congress of Neurological S, et al. Guidelines for the management of severe traumatic brain injury. VIII. Intracranial pressure thresholds. J Neurotrauma. 2007;24 Suppl 1:S55–8.
Hicks R, Giacino J, Harrison-Felix C, et al. Progress in developing common data elements for traumatic brain injury research: version two—the end of the beginning. J Neurotrauma. 2013;30:1852–61.
Lazaridis C, Andrews CM. Brain tissue oxygenation, lactate-pyruvate ratio, and cerebrovascular pressure reactivity monitoring in severe traumatic brain injury: systematic review and viewpoint. Neurocrit Care. 2014;21:345–55.
Martini RP, Deem S, Treggiari MM. Targeting brain tissue oxygenation in traumatic brain injury. Respir Care. 2013;58:162–72.
Green JA, Pellegrini DC, Vanderkolk WE, et al. Goal directed brain tissue oxygen monitoring versus conventional management in traumatic brain injury: an analysis of in hospital recovery. Neurocrit Care. 2013;18:20–5.
Rosenthal G, Sanchez-Mejia RO, Phan N, et al. Incorporating a parenchymal thermal diffusion cerebral blood flow probe in bedside assessment of cerebral autoregulation and vasoreactivity in patients with severe traumatic brain injury. J Neurosurg. 2011;114:62–70.
Pascual JL, Georgoff P, Maloney-Wilensky E, et al. Reduced brain tissue oxygen in traumatic brain injury: are most commonly used interventions successful? J Trauma. 2011;70:535–46.
Hemphill JC, Andrews P, De Georgia M. Multimodal monitoring and neurocritical care bioinformatics. Nat Rev Neurol. 2011;7:451–60.
Marin-Caballos AJ, Murillo-Cabezas F, Cayuela-Dominguez A, et al. Cerebral perfusion pressure and risk of brain hypoxia in severe head injury: a prospective observational study. Crit Care. 2005;9:R670–6.
Kramer DR, Winer JL, Pease BA, et al. Cerebral vasospasm in traumatic brain injury. Neurol Res Int. 2013;2013:415813.
Sharma V. Role of transcranial Doppler in traumatic brain injury. Turkish Neurosurg. 2012;22:525–6.
Rosenthal ES. The utility of EEG, SSEP, and other neurophysiologic tools to guide neurocritical care. Neurother: J Am Soc Exp Neurother. 2012;9:24–36.
Rosenthal G, Furmanov A, Itshayek E, et al. Assessment of a noninvasive cerebral oxygenation monitor in patients with severe traumatic brain injury. J Neurosurg. 2014;120:901–7.
Chesnut RM, Temkin N, Carney N, et al. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012;367:2471–81.
Armonda RA, Bell RS, Vo AH, et al. Wartime traumatic cerebral vasospasm: recent review of combat casualties. Neurosurgery. 2006;59:1215–25. discussion 25.
Cairns CJ, Finfer SR, Harrington TJ, et al. Papaverine angioplasty to treat cerebral vasospasm following traumatic subarachnoid haemorrhage. Anaesth Intensive Care. 2003;31:87–91.
Kordestani RK, Counelis GJ, McBride DQ, et al. Cerebral arterial spasm after penetrating craniocerebral gunshot wounds: transcranial Doppler and cerebral blood flow findings. Neurosurgery. 1997;41:351–9. discussion 9-60.
Soustiel JF, Shik V, Feinsod M. Basilar vasospasm following spontaneous and traumatic subarachnoid haemorrhage: clinical implications. Acta Neurochir. 2002;144:137–44. discussion 44.
Vajramani GV, Chandramouli BA, Jayakumar PN, et al. Evaluation of posttraumatic vasospasm, hyperaemia, and autoregulation by transcranial colour-coded duplex sonography. Br J Neurosurg. 1999;13:468–73.
Yamada K, Harada M, Hasegawa S, et al. Delayed posttraumatic middle cerebral artery vasospasm demonstrated by magnetic resonance angiography: case report. Neurosurgery. 1998;43:153–6.
Zubkov AY, Lewis AI, Raila FA, et al. Risk factors for the development of post-traumatic cerebral vasospasm. Surg Neurol. 2000;53:126–30.
Hald ES, Alford PW. Smooth muscle phenotype switching in blast traumatic brain injury-induced cerebral vasospasm. Transl Stroke Res. 2014;5:385–93.
Firsching R, Woischneck D, Diedrich M, et al. Early magnetic resonance imaging of brainstem lesions after severe head injury. J Neurosurg. 1998;89:707–12.
Paterakis K, Karantanas AH, Komnos A, et al. Outcome of patients with diffuse axonal injury: the significance and prognostic value of MRI in the acute phase. J Trauma. 2000;49:1071–5.
Gentry LR, Godersky JC, Thompson B, et al. Prospective comparative study of intermediate-field MR and CT in the evaluation of closed head trauma. AJR Am J Roentgenol. 1988;150:673–82.
Lee H, Wintermark M, Gean AD, et al. Focal lesions in acute mild traumatic brain injury and neurocognitive outcome: CT versus 3T MRI. J Neurotrauma. 2008;25:1049–56.
Adams JH, Doyle D, Ford I, et al. Diffuse axonal injury in head injury: definition, diagnosis and grading. Histopathology. 1989;15:49–59.
Skandsen T, Kvistad KA, Solheim O, et al. Prognostic value of magnetic resonance imaging in moderate and severe head injury: a prospective study of early MRI findings and one-year outcome. J Neurotrauma. 2011;28:691–9.
Lagares A, Ramos A, Perez-Nunez A, et al. The role of MR imaging in assessing prognosis after severe and moderate head injury. Acta Neurochir. 2009;151:341–56.
Moen KG, Brezova V, Skandsen T, et al. Traumatic axonal injury: the prognostic value of lesion load in corpus callosum, brain stem, and thalamus in different magnetic resonance imaging sequences. J Neurotrauma. 2014;31:1486–96.
Betz J, Zhuo J, Roy A, et al. Prognostic value of diffusion tensor imaging parameters in severe traumatic brain injury. J Neurotrauma. 2012;29:1292–305.
Muccio CF, De Simone M, Esposito G, et al. Reversible post-traumatic bilateral extensive restricted diffusion of the brain. A case study and review of the literature. Brain Inj. 2009;23:466–72.
Edlow BL, Giacino JT, Hirschberg RE, et al. Unexpected recovery of function after severe traumatic brain injury: the limits of early neuroimaging-based outcome prediction. Neurocritical care. 2013.
Maxwell WL, Povlishock JT, Graham DL. A mechanistic analysis of nondisruptive axonal injury: a review. J Neurotrauma. 1997;14:419–40.
Ommaya AK. Head injury mechanisms and the concept of preventive management: a review and critical synthesis. J Neurotrauma. 1995;12:527–46.
Gentry LR. Imaging of closed head injury. Radiology. 1994;191:1–17.
Scheid R, Preul C, Gruber O, et al. Diffuse axonal injury associated with chronic traumatic brain injury: evidence from T2*-weighted gradient-echo imaging at 3 T. AJNR Am J Neuroradiol. 2003;24:1049–56.
Tong KA, Ashwal S, Holshouser BA, et al. Diffuse axonal injury in children: clinical correlation with hemorrhagic lesions. Ann Neurol. 2004;56:36–50.
Geurts BH, Andriessen TM, Goraj BM, et al. The reliability of magnetic resonance imaging in traumatic brain injury lesion detection. Brain Inj. 2012.
Yanagawa Y, Tsushima Y, Tokumaru A, et al. A quantitative analysis of head injury using T2*-weighted gradient-echo imaging. J Trauma. 2000;49:272–7.
Scheid R, Walther K, Guthke T, et al. Cognitive sequelae of diffuse axonal injury. Arch Neurol. 2006;63:418–24.
Niogi SN, Mukherjee P, Ghajar J, et al. Extent of microstructural white matter injury in postconcussive syndrome correlates with impaired cognitive reaction time: a 3T diffusion tensor imaging study of mild traumatic brain injury. AJNR Am J Neuroradiol. 2008;29:967–73.
Gennarelli TA, Spielman GM, Langfitt TW, et al. Influence of the type of intracranial lesion on outcome from severe head injury. J Neurosurg. 1982;56:26–32.
Nakase-Richardson R, Whyte J, Giacino JT, et al. Longitudinal outcome of patients with disordered consciousness in the NIDRR TBI Model Systems Programs. J Neurotrauma. 2012;29:59–65.
McNab JA, Edlow BL, Witzel T, et al. The Human Connectome Project and beyond: initial applications of 300mT/m gradients. Neuroimage. 2013;80:234–45.
Bell RS, Vo AH, Neal CJ, et al. Military traumatic brain and spinal column injury: a 5-year study of the impact blast and other military grade weaponry on the central nervous system. J Trauma. 2009;66:S104–11.
Zoroya G. For troops with brain trauma, a long journey back. Tampa: USA Today; 2010.
McNamee S, Howe L, Nakase-Richardson R, et al. Treatment of disorders of consciousness in the Veterans Health Administration polytrauma centers. J Head Trauma Rehabil. 2012;27:244–52.
Andrews K, Murphy L, Munday R, et al. Misdiagnosis of the vegetative state: retrospective study in a rehabilitation unit. BMJ. 1996;313:13–6.
Childs NL, Mercer WN, Childs HW. Accuracy of diagnosis of persistent vegetative state. Neurology. 1993;43:1465–7.
Schnakers C, Vanhaudenhuyse A, Giacino J, et al. Diagnostic accuracy of the vegetative and minimally conscious state: clinical consensus versus standardized neurobehavioral assessment. BMC Neurol. 2009;9:35.
Giacino JT, Kalmar K, Whyte J. The JFK Coma Recovery Scale-Revised: measurement characteristics and diagnostic utility. Arch Phys Med Rehabil. 2004;85:2020–9.
Giacino JT, Kalmar K. The vegetative and minimally conscious states: a comparison of clinical features and functional outcome. J Head Trauma Rehabil. 1997;12:36–51.
Luaute J, Maucort-Boulch D, Tell L, et al. Long-term outcomes of chronic minimally conscious and vegetative states. Neurology. 2010;75:246–52.
Edlow BL, Wu O. Advanced neuroimaging in traumatic brain injury. Semin Neurol. 2012;32:372–98.
Edlow BL, Giacino JT, Wu O. Functional MRI and outcome in traumatic coma. Curr Neurol Neurosci Rep. 2013;13:375.
Haacke EM, Xu Y, Cheng YC, et al. Susceptibility weighted imaging (SWI). Magn Reson Med. 2004;52:612–8.
Tong KA, Ashwal S, Holshouser BA, et al. Hemorrhagic shearing lesions in children and adolescents with posttraumatic diffuse axonal injury: improved detection and initial results. Radiology. 2003;227:332–9.
Scheid R, Ott DV, Roth H, et al. Comparative magnetic resonance imaging at 1.5 and 3 Tesla for the evaluation of traumatic microbleeds. J Neurotrauma. 2007;24:1811–6.
Nandigam RN, Viswanathan A, Delgado P, et al. MR imaging detection of cerebral microbleeds: effect of susceptibility-weighted imaging, section thickness, and field strength. AJNR Am J Neuroradiol. 2009;30:338–43.
Pierpaoli C, Jezzard P, Basser PJ, et al. Diffusion tensor MR imaging of the human brain. Radiology. 1996;201:637–48.
Mac Donald CL, Dikranian K, Song SK, et al. Detection of traumatic axonal injury with diffusion tensor imaging in a mouse model of traumatic brain injury. Exp Neurol. 2007;205:116–31.
Li J, Li XY, Feng DF, et al. Quantitative evaluation of microscopic injury with diffusion tensor imaging in a rat model of diffuse axonal injury. Eur J Neurosci. 2011;33:933–45.
Huisman TA, Schwamm LH, Schaefer PW, et al. Diffusion tensor imaging as potential biomarker of white matter injury in diffuse axonal injury. AJNR Am J Neuroradiol. 2004;25:370–6.
Newcombe V, Chatfield D, Outtrim J, et al. Mapping traumatic axonal injury using diffusion tensor imaging: correlations with functional outcome. PLoS One. 2011;6, e19214.
Xu J, Rasmussen IA, Lagopoulos J, et al. Diffuse axonal injury in severe traumatic brain injury visualized using high-resolution diffusion tensor imaging. J Neurotrauma. 2007;24:753–65.
Sidaros A, Engberg AW, Sidaros K, et al. Diffusion tensor imaging during recovery from severe traumatic brain injury and relation to clinical outcome: a longitudinal study. Brain. 2008;131:559–72.
Tollard E, Galanaud D, Perlbarg V, et al. Experience of diffusion tensor imaging and 1H spectroscopy for outcome prediction in severe traumatic brain injury: preliminary results. Crit Care Med. 2009;37:1448–55.
Perlbarg V, Puybasset L, Tollard E, et al. Relation between brain lesion location and clinical outcome in patients with severe traumatic brain injury: a diffusion tensor imaging study using voxel-based approaches. Hum Brain Mapp. 2009;30:3924–33.
Palacios EM, Fernandez-Espejo D, Junque C, et al. Diffusion tensor imaging differences relate to memory deficits in diffuse traumatic brain injury. BMC Neurol. 2011;11:24.
Kinnunen KM, Greenwood R, Powell JH, et al. White matter damage and cognitive impairment after traumatic brain injury. Brain. 2011;134:449–63.
Palacios EM, Sala-Llonch R, Junque C, et al. White matter integrity related to functional working memory networks in traumatic brain injury. Neurology. 2012;78:852–60.
Palacios EM, Sala-Llonch R, Junque C, et al. Long-term declarative memory deficits in diffuse TBI: correlations with cortical thickness, white matter integrity and hippocampal volume. Cortex. 2012.
Mori S, Crain BJ, Chacko VP, et al. Three-dimensional tracking of axonal projections in the brain by magnetic resonance imaging. Ann Neurol. 1999;45:265–9.
Behrens TE, Woolrich MW, Jenkinson M, et al. Characterization and propagation of uncertainty in diffusion-weighted MR imaging. Magn Reson Med. 2003;50:1077–88.
Hansen B, Flint JJ, Heon-Lee C, et al. Diffusion tensor microscopy in human nervous tissue with quantitative correlation based on direct histological comparison. Neuroimage. 2011;57:1458–65.
Edlow BL, Haynes RL, Takahashi E, et al. Disconnection of the ascending arousal system in traumatic coma. J Neuropathol Exp Neurol. 2013;72:505–23.
Jones DK, Knosche TR, Turner R. White matter integrity, fiber count, and other fallacies: the do’s and don’ts of diffusion MRI. Neuroimage. 2013;73:239–54.
Thomas C, Ye FQ, Irfanoglu MO, et al. Anatomical accuracy of brain connections derived from diffusion MRI tractography is inherently limited. Proc Natl Acad Sci U S A. 2014;111:16574–9.
Wang JY, Bakhadirov K, Devous Sr MD, et al. Diffusion tensor tractography of traumatic diffuse axonal injury. Arch Neurol. 2008;65:619–26.
Wang JY, Bakhadirov K, Abdi H, et al. Longitudinal changes of structural connectivity in traumatic axonal injury. Neurology. 2011;77:818–26.
Newcombe VF, Williams GB, Scoffings D, et al. Aetiological differences in neuroanatomy of the vegetative state: insights from diffusion tensor imaging and functional implications. J Neurol Neurosurg Psychiatry. 2010;81:552–61.
Ommaya AK, Gennarelli TA. Cerebral concussion and traumatic unconsciousness. Correlation of experimental and clinical observations of blunt head injuries. Brain. 1974;97:633–54.
Gennarelli TA, Thibault LE, Adams JH, et al. Diffuse axonal injury and traumatic coma in the primate. Ann Neurol. 1982;12:564–74.
Smith DH, Nonaka M, Miller R, et al. Immediate coma following inertial brain injury dependent on axonal damage in the brainstem. J Neurosurg. 2000;93:315–22.
Rutgers DR, Fillard P, Paradot G, et al. Diffusion tensor imaging characteristics of the corpus callosum in mild, moderate, and severe traumatic brain injury. AJNR Am J Neuroradiol. 2008;29:1730–5.
Singh M, Jeong J, Hwang D, et al. Novel diffusion tensor imaging methodology to detect and quantify injured regions and affected brain pathways in traumatic brain injury. Magn Reson Imaging. 2010;28:22–40.
Fernandez-Espejo D, Soddu A, Cruse D, et al. A role for the default mode network in the bases of disorders of consciousness. Ann Neurol. 2012;72:335–43. This study demonstrated that DTT-based measurements of connectivity within the DMN, a brain network believed to be involved in self-awareness, correlated with the level of consciousness on behavioral testing in patients with traumatic DOC.
Donaldson DI, Buckner RL. Effective paradigm design. In: Jezzard P, Matthews PM, Smith SM, editors. Functional MRI: an introduction to methods. Oxford: Oxford University Press; 2001.
Forgacs PB, Conte MM, Fridman EA, et al. Preservation of electroencephalographic organization in patients with impaired consciousness and imaging-based evidence of command-following. Ann Neurol. 2014;76:869–79. This study demonstrated that patients with traumatic DOC who are capable of “covert” command-following during an fMRI motor imagery task also have evidence of normal or near-normal EEG findings during wake and sleep, as well as partial preservation of brain metabolism on FDG PET.
Kasahara M, Menon DK, Salmond CH, et al. Traumatic brain injury alters the functional brain network mediating working memory. Brain Inj. 2011;25:1170–87.
Kasahara M, Menon DK, Salmond CH, et al. Altered functional connectivity in the motor network after traumatic brain injury. Neurology. 2010;75:168–76.
Owen AM, Coleman MR, Boly M, et al. Detecting awareness in the vegetative state. Science. 2006;313:1402.
Coleman MR, Davis MH, Rodd JM, et al. Towards the routine use of brain imaging to aid the clinical diagnosis of disorders of consciousness. Brain. 2009;132:2541–52.
Coleman MR, Rodd JM, Davis MH, et al. Do vegetative patients retain aspects of language comprehension? Evidence from fMRI. Brain. 2007;130:2494–507.
Monti MM, Pickard JD, Owen AM. Visual cognition in disorders of consciousness: from V1 to top-down attention. Hum Brain Mapp. 2013;34:1245–53.
Rodriguez Moreno D, Schiff ND, Giacino J, et al. A network approach to assessing cognition in disorders of consciousness. Neurology. 2010;75:1871–8.
Schiff ND, Rodriguez-Moreno D, Kamal A, et al. fMRI reveals large-scale network activation in minimally conscious patients. Neurology. 2005;64:514–23.
Fernandez-Espejo D, Junque C, Vendrell P, et al. Cerebral response to speech in vegetative and minimally conscious states after traumatic brain injury. Brain Inj. 2008;22:882–90.
Bekinschtein T, Leiguarda R, Armony J, et al. Emotion processing in the minimally conscious state. J Neurol Neurosurg Psychiatry. 2004;75:788.
Bekinschtein T, Tiberti C, Niklison J, et al. Assessing level of consciousness and cognitive changes from vegetative state to full recovery. Neuropsychol Rehabil. 2005;15:307–22.
Di HB, Yu SM, Weng XC, et al. Cerebral response to patient’s own name in the vegetative and minimally conscious states. Neurology. 2007;68:895–9.
Zhu J, Wu X, Gao L, et al. Cortical activity after emotional visual stimulation in minimally conscious state patients. J Neurotrauma. 2009;26:677–88.
Qin P, Di H, Liu Y, et al. Anterior cingulate activity and the self in disorders of consciousness. Hum Brain Mapp. 2010;31:1993–2002.
Fernandez-Espejo D, Junque C, Cruse D, et al. Combination of diffusion tensor and functional magnetic resonance imaging during recovery from the vegetative state. BMC Neurol. 2010;10:77.
Heelmann V, Lippert-Gruner M, Rommel T, et al. Abnormal functional MRI BOLD contrast in the vegetative state after severe traumatic brain injury. Int J Rehabil Res Int Z Rehab Forschung Revue Int Rech Readaptation. 2010;33:151–7.
Monti MM, Vanhaudenhuyse A, Coleman MR, et al. Willful modulation of brain activity in disorders of consciousness. N Engl J Med. 2010;362:579–89. This study includes a large cohort of patients with DOC studied with spatial and motor imagery fMRI paradigms (n = 54). Not only did 5 of 54 patients (all with TBI) have patterns of brain activation during these command-following paradigms that were similar to controls, but one patient could link the two imagery tasks to “yes” and “no” answers.
Bekinschtein TA, Manes FF, Villarreal M, et al. Functional imaging reveals movement preparatory activity in the vegetative state. Front Hum Neurosci. 2011;5:5.
Bardin JC, Fins JJ, Katz DI, et al. Dissociations between behavioural and functional magnetic resonance imaging-based evaluations of cognitive function after brain injury. Brain. 2011;134:769–82.
Jilka SR, Scott G, Ham T, et al. Damage to the Salience Network and interactions with the Default Mode Network. J Neurosci. 2014;34:10798–807.
Laureys S, Schiff ND. Coma and consciousness: paradigms (re)framed by neuroimaging. Neuroimage. 2012;61:478–91.
Raichle ME, MacLeod AM, Snyder AZ, et al. A default mode of brain function. Proc Natl Acad Sci U S A. 2001;98:676–82.
Raichle ME, Snyder AZ. A default mode of brain function: a brief history of an evolving idea. Neuroimage. 2007;37:1083–90. discussion 97-9.
Shulman GL, Fiez JA, Corbetta M, et al. Common blood flow changes across visual tasks: II. Decreases in cerebral cortex. J Cogn Neurosci. 1997;9:648–63.
Binder JR, Frost JA, Hammeke TA, et al. Conceptual processing during the conscious resting state. A functional MRI study. J Cogn Neurosci. 1999;11:80–95.
Sharp DJ, Beckmann CF, Greenwood R, et al. Default mode network functional and structural connectivity after traumatic brain injury. Brain. 2011;134:2233–47.
Hillary FG, Slocomb J, Hills EC, et al. Changes in resting connectivity during recovery from severe traumatic brain injury. Int J Psychophysiol: Off J Int Organ Psychophysiol. 2011;82:115–23.
Bonnelle V, Leech R, Kinnunen KM, et al. Default mode network connectivity predicts sustained attention deficits after traumatic brain injury. J Neurosci. 2011;31:13442–51.
Bonnelle V, Ham TE, Leech R, et al. Salience network integrity predicts default mode network function after traumatic brain injury. Proc Natl Acad Sci U S A. 2012;109:4690–5.
Cauda F, Micon BM, Sacco K, et al. Disrupted intrinsic functional connectivity in the vegetative state. J Neurol Neurosurg Psychiatry. 2009;80:429–31.
Vanhaudenhuyse A, Noirhomme Q, Tshibanda LJ, et al. Default network connectivity reflects the level of consciousness in non-communicative brain-damaged patients. Brain. 2010;133:161–71.
Soddu A, Vanhaudenhuyse A, Bahri MA, et al. Identifying the default-mode component in spatial IC analyses of patients with disorders of consciousness. Hum Brain Mapp. 2012;33:778–96.
Ovadia-Caro S, Nir Y, Soddu A, et al. Reduction in inter-hemispheric connectivity in disorders of consciousness. PLoS One. 2012;7, e37238.
Ham TE, Bonnelle V, Hellyer P, et al. The neural basis of impaired self-awareness after traumatic brain injury. Brain. 2014;137:586–97.
Teipel SJ, Bokde AL, Meindl T, et al. White matter microstructure underlying default mode network connectivity in the human brain. Neuroimage. 2010;49:2021–32.
Greicius MD, Supekar K, Menon V, et al. Resting-state functional connectivity reflects structural connectivity in the default mode network. Cereb Cortex. 2009;19:72–8.
Detre JA, Wang J. Technical aspects and utility of fMRI using BOLD and ASL. Clin Neurophysiol. 2002;113:621–34.
Kim J, Whyte J, Patel S, et al. Resting cerebral blood flow alterations in chronic traumatic brain injury: an arterial spin labeling perfusion FMRI study. J Neurotrauma. 2010;27:1399–411.
Kim J, Whyte J, Patel S, et al. A perfusion fMRI study of the neural correlates of sustained-attention and working-memory deficits in chronic traumatic brain injury. Neurorehabil Neural Repair. 2012;26:870–80.
Bergsneider M, Hovda DA, Shalmon E, et al. Cerebral hyperglycolysis following severe traumatic brain injury in humans: a positron emission tomography study. J Neurosurg. 1997;86:241–51.
Stender J, Gosseries O, Bruno MA, et al. Diagnostic precision of PET imaging and functional MRI in disorders of consciousness: a clinical validation study. Lancet. 2014;384:514–22. This study demonstrated that the prognostic utility of FDG PET for predicting outcomes in patients with traumatic DOC may be superior to that of stimulus-based fMRI.
Bruno MA, Majerus S, Boly M, et al. Functional neuroanatomy underlying the clinical subcategorization of minimally conscious state patients. J Neurol. 2012;259:1087–98.
Stender J, Kupers R, Rodell A, et al. Quantitative rates of brain glucose metabolism distinguish minimally conscious from vegetative state patients. Journal of cerebral blood flow and metabolism: official journal of the International Society of Cerebral Blood Flow and Metabolism. 2014.
Milligan TA, Zamani A, Bromfield E. Frequency and patterns of MRI abnormalities due to status epilepticus. Seizure. 2009;18:104–8.
Hartings JA, Watanabe T, Bullock MR, et al. Spreading depolarizations have prolonged direct current shifts and are associated with poor outcome in brain trauma. Brain. 2011;134:1529–40.
Baxter D, Sharp DJ, Feeney C, et al. Pituitary dysfunction after blast traumatic brain injury: the UK BIOSAP study. Ann Neurol. 2013;74:527–36.
Autio JA, Shatillo A, Giniatullin R, et al. Parenchymal spin-lock fMRI signals associated with cortical spreading depression. J Cereb Blood Flow Metab: Off J Int Soc Cereb Blood Flow Metab. 2014;34:768–75.
Sala N, Suys T, Zerlauth JB, et al. Cerebral extracellular lactate increase is predominantly nonischemic in patients with severe traumatic brain injury. J Cereb Blood Flow Metab: Off J Int Soc Cereb Blood Flow Metab. 2013;33:1815–22.
Carpentier A, Galanaud D, Puybasset L, et al. Early morphologic and spectroscopic magnetic resonance in severe traumatic brain injuries can detect “invisible brain stem damage” and predict “vegetative states”. J Neurotrauma. 2006;23:674–85.
Brown EN, Lydic R, Schiff ND. General anesthesia, sleep, and coma. N Engl J Med. 2010;363:2638–50.
Boly M, Phillips C, Tshibanda L, et al. Intrinsic brain activity in altered states of consciousness: how conscious is the default mode of brain function? Ann N Y Acad Sci. 2008;1129:119–29.
Greicius MD, Kiviniemi V, Tervonen O, et al. Persistent default-mode network connectivity during light sedation. Hum Brain Mapp. 2008;29:839–47.
Fukunaga M, Horovitz SG, van Gelderen P, et al. Large-amplitude, spatially correlated fluctuations in BOLD fMRI signals during extended rest and early sleep stages. Magn Reson Imaging. 2006;24:979–92.
Kim J, Whyte J, Patel S, et al. Methylphenidate modulates sustained attention and cortical activation in survivors of traumatic brain injury: a perfusion fMRI study. Psychopharmacology. 2012;222:47–57.
Niogi SN, Mukherjee P, Ghajar J, et al. Structural dissociation of attentional control and memory in adults with and without mild traumatic brain injury. Brain. 2008;131:3209–21.
Kraus MF, Susmaras T, Caughlin BP, et al. White matter integrity and cognition in chronic traumatic brain injury: a diffusion tensor imaging study. Brain. 2007;130:2508–19.
Edlow BL, Takahashi E, Wu O, et al. Neuroanatomic connectivity of the human ascending arousal system critical to consciousness and its disorders. J Neuropathol Exp Neurol. 2012;71:531–46.
Edlow BL, Haynes RL, Takahashi E, et al. Disconnection of the ascending arousal system in traumatic coma. J Neuropathol Exp Neurol. 2013; in press.
Beissner F, Schumann A, Brunn F, et al. Advances in functional magnetic resonance imaging of the human brainstem. Neuroimage. 2014;86:91–8.
Parvizi J, Damasio AR. Neuroanatomical correlates of brainstem coma. Brain. 2003;126:1524–36.
Acknowledgments
The contents of this manuscript were developed with support from the American Academy of Neurology and American Brain Foundation.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Brian L. Edlow declares no conflict of interest. Eric S. Rosenthal has a patent “System and method employing the stochastic Gabor function and dual energy pulses for electrical impedance spectroscopy” pending.
Human and Animal Rights and Informed Consent
The data presented in Fig. 1 were acquired with informed consent from the patient’s surrogate decision-maker.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Blunt Head Trauma
Rights and permissions
About this article
Cite this article
Edlow, B.L., Rosenthal, E.S. Diagnostic, Prognostic, and Advanced Imaging in Severe Traumatic Brain Injury. Curr Trauma Rep 1, 133–146 (2015). https://doi.org/10.1007/s40719-015-0018-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40719-015-0018-7
Keywords
- Traumatic brain injury (TBI)
- Traumatic axonal injury (TAI)
- Coma
- Diffusion tensor imaging (DTI)
- Diffusion tensor tractography (DTT)
- Susceptibility-weighted imaging (SWI)
- Functional MRI (fMRI)
- Resting-state functional MRI (rs-fMRI)
- Arterial spin-labeled (ASL) perfusion MRI
- Positron emission tomography (PET)
- Magnetic resonance spectroscopy (MRS)