Abstract
Purpose of the review
This narrative review highlights recent literature pertaining to available intra-articular (IA) therapeutics such as corticosteroids, hyaluronic acid (HA), platelet-rich plasma (PRP), stem cells therapy, and prolotherapy for knee osteoarthritis (OA) by summarizing recently published treatment guidelines and clinical trials, and discusses opinion and future directions.
Recent findings
IA corticosteroid has questionable long-term efficacy in head-to-head comparisons with IA PRP, ketorolac, or normal saline. Combination therapy of IA corticosteroid plus HA may be more effective than a single IA corticosteroid therapy. Significant symptomatic improvement for at least 6 months was detected for combined therapies of IA HA with PRP or diclofenac, compared with single IA HA therapy in small studies. Conflicting results were reported over IA PRP using a variety of comparators such as IA HA, ozone, and normal saline, as well as over IA stem cell therapies, urgently necessitating the standardization of PRP and stem cell products. Prolotherapy may be effective in single or combination regimes in small studies. None of the IA therapies demonstrated serious adverse effects, such as septic arthritis. These findings should be interpreted with caution as the included studies show conflicting results as well as several methodological flaws such as small sample size, short-term follow-ups, a lack of control group and absence of structural evaluations.
Summary
Collectively, these studies have demonstrated the need for further confirmation studies and highlighted the issues of standardization of PRP and stem cell therapies, the placebo effects and cost-effectiveness of IA therapeutics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee osteoarthritis (OA) is the commonest articular disease and usually presents in aging populations with chronic joint pain, brief morning stiffness, impaired knee function, difficulty in activities of daily living, and loss of mobility. Examination may be characterized by audible or palpable coarse crepitus, bony enlargements, joint line tenderness, and deformities of the knee joints [1]. It can be defined radiographically and/or symptomatically, and such definitions can affect epidemiological estimates of knee OA [2]. Its estimated global prevalence in persons over 40 years of age is at 22·9% in 2020 (correspondingly 654·1 million individuals) [3], imposing considerable socioeconomic costs as the direct and indirect costs for OA management being 1 to 2.5% of the gross national product (GNP) in most of developed countries [4].
The current narrative review was aimed at summarizing the efficacy and adverse effects of the currently available IA agents in knee OA such as corticosteroids and hyaluronic acid, platelet-rich plasma, stem cells, and prolotherapy. Moreover, the accuracy rates of available methods of drug injection into knee joint are briefly discussed: blind or landmark-guided method vs ultrasound guidance.
The literature approach was based on the PubMed database over 2 years from 1 January 2021 to 31 December 2023 to reflect current research findings with a search strategy for randomized controlled trials (RCTs) conducted in human beings and written in the English language, focusing on but not limited to the terms “knee osteoarthritis” or “knee arthrosis” in combination with “intra-articular injections” or “injection-based therapy” or “corticosteroid” or “hyaluronic acid” or “platelet-rich plasma” or “stem cells” or “prolotherapy” ( see Online Supplementary Material for the full search strategy). Additional articles were identified by using the bibliographies of each paper. We identified 1515 papers from the search results and tried to focus on articles deemed to provide a purposeful increase in our knowledge base.
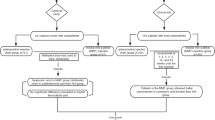
Recommended management of knee osteoarthritis
No drugs are yet available to modify the structural manifestations of the disease course of knee OA [5]. Current OA management focuses on symptomatic improvement only [6] and is largely palliative in approach despite the OA disease course typically being slowly progressive over years/decades [7]. Treatment options include (1) non-pharmacological management such as weight reduction, life-style changes, dieting, and exercises [8], (2) pharmacological options such as paracetamol, nonsteroidal anti-inflammatory drugs (NSAIDs), opioid analgesics, and intra-articular therapies such as steroids and hyaluronic acids, and (3) surgical interventions which are typically reserved only for end-stage OA, as a last resort [9••]. Recently, paracetamol and opioids have been only conditionally or not recommended by several scientific guidelines [6, 9••, 10]. In addition, the existing treatments have shown only modest efficacy at best [2], and long-term use of commonly used analgesics are not recommended due to adverse effects in the gastrointestinal, cardiac, or renal systems as patients with knee OA usually have multiple comorbid diseases [9••].
Intra-articular therapies
The IA administration of drugs possesses the advantage of high efficiency while limiting the systemic exposure and off-target effects as drugs are locally administered into the joints [11]. Most available guidelines for knee OA management would not typically advocate the use of IA medications until the second or third line [6, 12] as it is an invasive procedure and not without uncommon but serious complications such as septic arthritis (10–40 persons per 100,000 injections) [13]. Table 1 summarizes recommendations from NICE [9••], AAOS [14••], ACR [10], OARSI [6], ESCEO [12], and PANLAR [15] guidelines related to available IA therapies for knee OA as part of conservative management. IA therapeutics that possess anti-inflammatory properties might be appropriate, for example, during a flare of knee OA and the presence of a large effusion. The patient should be provided with essential information such as the nature of the IA procedure (blind or imaging guided), the potential benefits and risks of IA therapies, as well as post-injection care such as 24- to 48-h post-injection immobilization [16••, 17•].
On administration of IA therapeutics into the knee joints, either landmark-guided or imaging-guided approach could be used [16••] (Table 2). In the literature, there is strong evidence that ultrasound guidance IA injection provides significantly higher accuracy in administrating the injectates into the knee joints than landmark-guided (blind) injections (96% vs 73%, n=89) [18]; (96% vs 84%, n=99) [19]. Among 3 different approaches, the superolateral portal (100%) and mid-lateral portal (95%) showed significantly higher accuracy than injections in the medial portal (75%) (n=126) [20]. The enhanced injection accuracy achieved with ultrasound needle guidance [21] directly improves patient-reported clinical outcomes, cost-effectiveness [22], and patient satisfaction [23].
Available IA injectates
The commonly used IA injectables in daily practice include corticosteroids, hyaluronic acid (HA), platelet-rich plasma (PRP), stem cell, and prolotherapy.
Corticosteroid
In clinical practice, IA corticosteroid injections are commonly used procedure in knee OA, especially when pain is refractory to physical treatments and oral medications, or to support therapeutic exercise [9••]. The choice of the drug type generally may be triamcinolone, methylprednisolone, or dexamethasone, depending on the clinical experience and preference of the physician. We identified five studies investigating IA corticosteroids in knee OA. In 4 studies, each study used IA normal saline (as a placebo) [24], ketorolac (NSAID) [25], PRP [26], or HA (vs steroid plus HA co-injection) [27] as the comparator group and the remaining study compared the routes of administration (IA vs intramuscular corticosteroid) [28].
Hunter et al. demonstrated significant improvement in WOMAC pain (mean difference = −0.35, p = 0.004) and function (mean difference = −0.26, p = 0.045) in knee OA with radiographic KL grade 2 or 3 when IA injection of 12 mg of liposome formulation (to prolong the local joint residence time) of dexamethasone sodium phosphate (TLC599) was compared to IA normal saline injection at 24-week follow-up (n=76). The percentage of clinically durable responders (defined as > 30% pain reduction as measured by the WOMAC-Pain scale) at 24 weeks was greater in TLC599 group (52% vs 22%; p = 0.0143); however, there was no significant improvement in quality of life on EQ-5D questionnaires. No major or unexpected safety issues were detected [24]. A larger and well-designed pivotal study (ClinicalTrials.gov identifier: NCT04123561) is currently ongoing to confirm this efficacy profile. In a 3-month study comparing the IA administration of 80 mg of triamcinolone with 30 mg of ketorolac under ultrasound guidance in patients with hip (n=52) or knee OA (n=58), no significant between-group differences in HOOS or KOOS and VAS scores with minimal adverse effects were reported [25]. In a 52-week study comparing the single IA injection among three groups (40 mg of triamcinolone hexacetonide (n=33) vs PRP (n=34) vs the saline solution (n=33)), no significant differences were found in the inter-group comparison over time except for superiority of the triamcinolone hexacetonide group over the other two groups at 4 weeks). The PRP group showed the lowest radiographic progression from KL grade 2 to 3 over 52 weeks among the three groups [triamcinolone from 52 to 73%; saline 52 to 91%; PRP from 59 to 62%] [26]. However, the study has several limitations such as small sample size, multiple comparison with no statistical adjustment and questionable sensitivities of radiographic scores in assessing the structural progression of knee OA.
In a 6-month study in knee OA, weekly IA co-injections of corticosteroids plus hyaluronic acid (HA) for 3 weeks (n=28) provided statistically significant improvement in WOMAC-pain (P = .005) and physical function (P = .005), chair-rising time (P = .032), and KOOS-pain (P = .001) from 1 week to 6 months, compared with HA injections alone (n=29) [27]; however, the outcome longer than 6 months is unknown. In a multicenter, open-label, randomized clinical noninferiority trial comparing the IA vs IM administration routes for steroids in symptomatic knee OA, noninferiority could not be declared with between-group mean difference in the KOOS pain score was −3.4 (95% CI, −10.1 to 3.3; effect size = −0.17) favoring the IA route at the primary time point (4 weeks) [28]. Lack of a placebo-controlled group and being an open-level study are study limitations.
Summary
The IA corticosteroid therapy provided short-term symptomatic benefits in knee OA but long-term benefits seem to be less likely even in combination therapies with other IA therapeutics. Extended release IA steroids which can prolong joint residence time are currently under intense research.
Hyaluronic acid
Viscosupplementation with hyaluronic acid (HA) in knee OA has been extensively researched since 1971 [29] and 2438 papers has been published between 2002 and 2021 [30]; however, its role in knee OA management still generates debate in terms of clinical benefits [9••, 30] as the published data were limited by the high heterogeneity of effect sizes perhaps due to different HA formulations, different periods of follow-up, and differences in injection schedules and IA techniques [17•]. In the recent literature, four papers were identified, comparing HA with placebo (n=2) [31, 32] and PRP (n=2) [33, 34].
A 26-week study in Chinese patients with knee OA (n=440) did not establish superiority of single 6 ml Hylan G-F 20 injection over IA placebo using the WOMAC pain score while walking. Percentages of positive responders over 26 weeks, defined as a ≥ 2-point improvement from baseline, was not significantly different (67% in the treatment arm vs. 68% in the placebo arm) [31]. As a note, the placebo effects were marked in the Chinese clinical compared with the European trial (44% vs 29%), which used a similar trial design and methodology (n=253) [35]. When diclofenac etalhyaluronate (DF-HA), which is diclofenac covalently linked to HA, was administered once every 4 weeks for 20 weeks (a total of 6 injections) in Japanese patients with knee OA, a statistically significant improvement in the WOMAC pain subscale, measured on a 100-mm VAS, in the active treatment group was detected at 12 weeks compared to the placebo group, with a difference of −6.1 mm (95% confidence interval −9.4, −2.8; P < 0.001); however, there was no significant difference at week 24 (n=440). Anaphylactic reactions were observed in 2 subjects receiving DF-HA [32]. The limitations are the need to frequent IA injection, which may lead to an increased risk of joint infections [17•] and the lack of evaluation of chondrotoxicity caused by NSAIDs which have been suggested to be deleterious to joint cartilage [36].
A single IA injection of HA (3 ml, 20 mg/ml) followed by 3 ml PRP (the combined-injection group) showed statistically significant pain reduction on a VAS score (mean difference: 7.9; p = 0.020), compared with a single injection of 3 ml PRP (the one-injection group) at 6-month follow-up (n=78). No serious adverse events occurred following injections. As a note, at 3-month follow-up, the subgroup of patients with baseline VAS pain > 56.4 mm in the one-injection group revealed a significantly greater reduction in VAS pain score than the combined injection group [33]. In another 24-month study, PRP combined with HA (48 knees) is significantly effective compared with PRP alone (40 knees) or HA alone (34 knees) at improving pain and function and acts through inhibiting synovial inflammation detected on ultrasound and reducing inflammatory cytokine content[34]. In a recent systematic review and meta-analysis including 7 studies (n=941), PRP combined with HA provided better clinical improvement (standardized mean difference≥0.30), such as pain and function beyond 6-month follow-up than PRP alone with no significant difference in the incidence of side effects [37], presumably due to their synergistic therapeutic effects on the proliferation of chondrocytes and cartilage repair demonstrated in a rabbit model [38].
Summary
While symptomatic benefits of IA HA therapies may be statistically significant, most clinical outcomes do not reach clinical significance. They are frequently being used in combination with other IA agents, expecting the chances of longer-term benefits compared with single-therapy regime. More research in the cost-effectiveness of such combination therapies is required.
Platelet-rich plasma
Platelet-rich plasma (PRP) definitions vary but one group suggested it be defined by its absolute platelet concentration > 1 ×106/μL or a fivefold increase in platelet concentration from baseline [39]. PRP may have the capacity to reverse pro-inflammatory processes and promote tissue repair via the release of many biologically active factors, such as growth factors and cytokines for restoration of the articular homeostasis [40]. Nine recent papers have been identified for IA PRP in knee OA.
In some studies, PRP has been found to be significantly effective in reducing the symptoms [41,42,43,44] and MRI-detected cartilage loss [45], compared with HA [41,42,43] or ozone [42] or normal saline placebo [44, 45] up to 36 [43] or 60 [45] months. However, in the other studies, it was reported that PRP is not superior to the placebo [46,47,48] or HA [49] in improving pain and function [46,47,48,49] and preventing the structural progression of the disease [46] up to 12 months [46, 48]. Regarding the frequency of single-dose PRP injection, PRP injections could be repeated at 6-month intervals as the effect of a single-dose PRP decreased significantly after 6 months[44]. In a recent meta-analysis of IA PRP versus comparative cohorts retrieved until 1 December 2021 which included 24 PRP clinical trials with HA(n=11), corticosteroid (n=6), normal saline (n=5), exercise therapy (n=3), and clinical relevance of outcome improvements (VAS and WOMAC scores) cannot be determined despite statistical significant findings and examination of structural changes showed no difference between the comparative groups. In addition, a paucity of high-quality studies, substantial heterogeneity of included studies, mostly small sample sizes, relatively short-term follow-up (mostly 6-month follow-ups) were noted [50••]. Recently, the American Academy of Orthopaedic Surgeons downgraded their strength of recommendation of PRP to “limited” due to inconsistent evidence [14••].
Summary
Current evidence is of low quality and is based on clinical trials with high risk of bias, great heterogeneity among clinical trials, and serious methodological flaws. Future high-quality studies using larger sample sizes, longer study durations and good methodologies are required.
Stem cell therapy
Due to multilineage differentiation potential, stem cell injections have been proposed as an innovative regenerative therapy for knee OA. However, a recent systematic review reported a paucity of RCT in this area, high risk of bias in the available studies, and a lack of long-term results [51]. We identify two papers related to stem cell therapies compared with PRP [52] or HA [53] in knee OA.
In a 24-month RCT comparing bone marrow aspiration concentrate (BMAC) and PRP in knee OA (n=84), WOMAC scores at 24 months improved by 14.5 points (41%) from baseline in the BMAC group and 12.4 points (38%) in the PRP group with no significant inter-group differences, disputing the beneficial effects of BMAC, given the added morbidity and expense of a bone marrow aspirate in the general OA population (an average cost of US $714 for PRP and US $3000 for BMAC). The study was limited by a high loss to follow-up (24% and 32% at 24 months for the BMAC and PRP groups) and no placebo group[52]. In another study conducted in 56 patients with bilateral knee OA, single IA BMAC injection was administered into one knee and single IA HA injection into the contralateral knee, each patient thereby acting as their own control and eliminating the need for sham bone marrow aspirations to maintain blindness. Compared to HA, BMAC showed a greater improvement in VAS pain at 12 months (2.2 vs 1.7, p = 0.04) and 24 months (2.2 vs 1.4, p <0.01) with no serious adverse events [53].
Summary
Conflicting results are noted between the comparative groups (BMAC vs PRP or HA) in two recent clinical trials, highlighting inconclusive evidence and the need for future high-quality studies.
Prolotherapy
In prolotherapy, small amounts of an irritant solution such as hyperosmolar dextrose (d-glucose) with concentrations ranging from 12.5 to 25% are injected into painful joints to restore joint stability by promoting the tensile strength of joint stabilizing structures, such as ligaments, tendons, and joint capsules [54]. We identified two recent studies.
In a small study conducted in knee OA (n=47), IA dextrose prolotherapy demonstrated a significant reduction in NRS pain scores over 12 weeks, compared with HA injection (−3 vs −2 for prolotherapy vs HA groups on NRS; p=0.04) [55]. In another 6-month study (n=104), HA plus dextrose co-injections under ultrasound guidance provided more significant improvements in stair climbing time and physical function at 6 months, compared with HA plus normal saline co-injection[56].
Summary
Despite statistically significant results in the recent studies, there is uncertain clinical relevance/significance due to small sample size, short-term follow-ups, a lack of control group, and absence of structural evaluations.
Opinion and future directions
Placebo effects
IA saline is a commonly used placebo in control groups in RCTs of IA therapies, and it can produce remarkable pain relief that may reach the values of minimal clinically important difference (MCID) [57]. In a recent meta-analysis, the placebo effects of IA saline at 6 month follow-up generated a significant improvement on 0–100 VAS pain score [−13.4 (−21.7/−5.1)], in WOMAC function sub-score [−10.1 (−12.2,-8.0)] and the pooled responder rate was 56% by using the OMERACT-OARSI criteria [58]. Therefore, in the clinical trials where pain and function are used as the primary endpoints, the placebo effects of IA saline should be accounted for in planning the trial design [59]. As the IA saline injection may be more than a “mere” placebo due to dilution effects in the joint environment [60], the underlying mechanisms of placebo effects and their predictors as well as the comparative effects of sham vs saline injections should be examined in robust study designs[5].
Trial quality and reasons why many injectates are not recommended in guidelines
In evidence-based medicine, the quality of clinical trials is one of the core factors for translating the research results into clinical practice. Increased risk of bias at the individual study level, inconsistent results among included clinical trials for a particular intervention, potential for small study effects and imprecision of the effect estimates often leads to the downgrading of the evidence in formulating the treatment recommendations[6]. In HA and PRP clinical trials, the use of different formulations, trade names, preparation methods, and frequency of injections leads to conflicting results among the studies, thereby reducing the strength of recommendations for these treatment options. Another core factor is cost-effectiveness or in terms of out-of-pocket costs. As an example, a single PRP injection has an average out-of-pocket cost of $714 and BMAC costs on average $3000. Given the degree and duration of efficacy between the two treatment options are not different, patients could elect to receive 4 PRP injections over the course of treatment for the same cost as a single BMC injection [52]. Similarly, IA HA cost per injection ranges from $300 to $600 USD, while a single steroid injection ranges from $10 to $50 USD [25].
Drug delivery systems for sustained release
As IA therapies directly targets the recognized pathogenetic tissues within the joint, lower doses than oral formulations are required due to higher bioavailability. Despite this advantage, there are several issues for IA administration which include pain and swelling during/after injection, uncommon but serious complication of septic arthritis and a short joint residence time due to rapid clearance of the IA therapeutics by the body. Therefore, a variety of drug delivery systems (DDS) have been developed with the aim of increasing the joint residence time of IA therapeutics. An ideal DDS should have such properties as controlled and/or sustained release of IA therapeutics for long-term effectiveness without a need of frequent injections [61] and adequate disease-modifying capacity, biocompatibility, and biodegradability [62]. New smart drug delivery strategies, which utilized hydrogels methods, nanoparticles and microparticles may enhance the opportunity for detecting the ideal long-lasting IA therapeutics [63].
Concomitant use of local anesthetics and chondrotoxicity
As IA injection may have pain and some discomfort to the patients, local anesthetics such as lidocaine are often added to the injectates in many studies described above. In recent systematic reviews, dose-dependent and time-dependent chondrotoxic effects of local anesthetics, presumably through mitochondrial dysfunction have been reported in vitro experimental and in vivo animal studies [64, 65]. However, it is uncertain whether these data from chondrocyte cultures or animal models might be transferrable to human tissues [64]. In the most recent in vivo study, single intra-articular knee injection of 10 ml of 2% lidocaine did not influence the chondrocyte viability and showed fast post-injection reduction of synovial lidocaine concentration (more than 40 times) [66]. Future studies which determine the chondrotoxicity of local anesthetics should be conducted.
Conclusion
Despite quick improvement in pain and function, IA corticosteroid has questionable efficacy on head-to-head comparisons with other comparators such as IA PRP, ketorolac, or normal saline in the long term. Combination therapy of IA corticosteroid plus HA may be more effective than a single IA corticosteroid therapy but needs further confirmation study in larger sample size. Although IA HA failed to show symptomatic improvement compared with normal saline, significant improvement in pain and function at least over 6 months was detected in providing combined therapies of HA with PRP or diclofenac, compared with single HA therapy in small studies, which similarly require further research. Conflicting results were reported over IA PRP using a variety of comparators such as HA, ozone and normal saline with some studies having follow-up durations of 36 or 60 months. Similarly, divergent results are reported for stem cells therapies. Therefore, standardization of PRP and stem cell products are in urgent need. Prolotherapy may be effective in single or combination regimes in small studies. None of the IA therapies included in the review demonstrated serious adverse effects nor septic arthritis. Joint injection accuracy and clinical outcomes are higher with imaging-guidance. Future studies should address the issues of product standardization, placebo effects, possible adverse effects of IA NSAID or local anesthetics on the cartilage, drug delivery systems, and cost-effectiveness of different IA therapeutics.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Oo WM, Hunter DJ. Repurposed and investigational disease-modifying drugs in osteoarthritis (DMOADs). Ther Adv Musculoskelet Dis. 2022;14:1759720x221090297.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745–59.
Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClin Med. 2020;29-30:100587–7.
Leifer VP, Katz JN, Losina E. The burden of OA-health services and economics. Osteoarthr Cart. 2021.
Oo WM. Prospects of disease-modifying osteoarthritis drugs. Clin Geriatr Med. 2022;38(2):397–432.
Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr Cart. 2019;27(11):1578–89.
Driban JB, Harkey MS, Barbe MF, Ward RJ, MacKay JW, Davis JE, et al. Risk factors and the natural history of accelerated knee osteoarthritis: a narrative review. BMC Musculoskeletal Disord. 2020;21(1):332.
Oo WM, Mobasheri A, Hunter DJ. A narrative review of anti-obesity medications for obese patients with osteoarthritis. Expert Opin Pharmacother. 2022;23(12):1381–95.
•• NICE, Osteoarthritis in over 16s: diagnosis and management. The most recent guideline provided the recommendation for or against the IA corticosteroid and hyaluronic acid therapies. 2022. https://www.nice.org.uk/guidance/ng226. Accessed 1 Dec 2022.
Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care Res (Hoboken). 2020;72(2):149–62.
Oo WM, Yu SP, Daniel MS, Hunter DJ. Disease-modifying drugs in osteoarthritis: current understanding and future therapeutics. Expert Opin Emerg Drugs. 2018;23(4):331–47.
Bruyère O, Honvo G, Veronese N, Arden NK, Branco J, Curtis EM, et al. An updated algorithm recommendation for the management of knee osteoarthritis from the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Semin Arthritis Rheum. 2019;49(3):337–50.
Ross KM, Mehr JS, Carothers BL, Greeley RD, Benowitz I, Henry D, et al. Bacterial septic arthritis infections associated with intra-articular injection practices for osteoarthritis knee pain-New Jersey, 2017. Infect Control Hosp Epidemiol. 2019;40(9):1013–8.
•• Brophy RH, Fillingham YA. AAOS Clinical Practice guideline summary: management of osteoarthritis of the knee (Nonarthroplasty). J Am Acad Ortho Surg. 2022;30(9):e721–9 The most recent guideline provided the level of recommendations (high, moderate or limited) for IA corticosteroid, hyaluronic acid and platelet rich therapies.
Rillo O, Riera H, Acosta C, Liendo V, Bolaños J, Monterola L, et al. PANLAR Consensus Recommendations for the management in osteoarthritis of hand, hip, and knee. J Clin Rheumatol. 2016;22(7):345–54.
•• Oo WM, Hunter DJ. Efficacy, safety, and accuracy of intra-articular therapies for hand osteoarthritis: current evidence. Drugs Aging. 2023;40(1):1–20 The latest update related with efficacy, safety and accuracy of injection methods for currently available and investigational intra-articular therapies in people with hand osteoarthritis.
• Oo WM, Liu X, Hunter DJ. Pharmacodynamics, efficacy, safety and administration of intra-articular therapies for knee osteoarthritis. Expert Opin Drug Metab Toxicol. 2019;15(12):1021–32 The recent article discussed the pharmacodynamics, effectiveness, advere effects and accuracy of different routes of IA drugs and summarized the possible barriers and future research directions.
Im SH, Lee SC, Park YB, Cho SR, Kim JC. Feasibility of sonography for intra-articular injections in the knee through a medial patellar portal. J Ultrasound Med. 2009;28(11):1465–70.
Bum Park Y, Ah Choi W, Kim YK, Chul Lee S, Hae Lee J. Accuracy of blind versus ultrasound-guided suprapatellar bursal injection. J Clin Ultrasound. 2012;40(1):20–5.
Park Y, Lee SC, Nam HS, Lee J, Nam SH. Comparison of sonographically guided intra-articular injections at 3 different sites of the knee. J Ultrasound Med. 2011;30(12):1669–76.
Oo WM, Bo MT. Role of ultrasonography in knee osteoarthritis. J Clin Rheumatol. 2016;22(6):324–9.
Berkoff DJ, Miller LE, Block JE. Clinical utility of ultrasound guidance for intra-articular knee injections: a review. Clin Interv Aging. 2012;7:89–95.
Sheth T, Miranda OM, Johnson B. Assessment of patient satisfaction, functionality, and quality of life after ultrasound-guided knee intervention: a prospective study. Clin Rheumatol. 2021;40(2):735–40.
Hunter DJ, Chang CC, Wei JC, Lin HY, Brown C, Tai TT, et al. TLC599 in patients with osteoarthritis of the knee: a phase IIa, randomized, placebo-controlled, dose-finding study. Arthritis Res Ther. 2022;24(1):52.
Jurgensmeier K, Jurgensmeier D, Kunz DE, Fuerst PG, Warth LC, Daines SB. Intra-articular injections of the hip and knee with triamcinolone vs ketorolac: a randomized controlled trial. J Arthroplasty. 2021;36(2):416–22.
Nunes-Tamashiro JC, Natour J, Ramuth FM, Toffolo SR, Mendes JG, Rosenfeld A, et al. Intra-articular injection with platelet-rich plasma compared to triamcinolone hexacetonide or saline solution in knee osteoarthritis: A double blinded randomized controlled trial with one year follow-up. Clin Rehabil. 2022;36(7):900–15.
Wang CP, Lee WC, Hsieh RL. Effects of repeated co-injections of corticosteroids and hyaluronic acid on knee osteoarthritis: a prospective, double-blind randomized controlled trial. Am J Med. 2022;135(5):641–9.
Wang Q, Mol MF, Bos PK, Dorleijn DMJ, Vis M, Gussekloo J, et al. Effect of Intramuscular vs intra-articular glucocorticoid injection on pain among adults with knee osteoarthritis: the KIS Randomized Clinical Trial. JAMA Netw Open. 2022;5(4):e224852.
Rydell N, Balazs EA. Effect of intra-articular injection of hyaluronic acid on the clinical symptoms of osteoarthritis and on granulation tissue formation. Clin Orthop Relat Res. 1971;80:25–32.
Zhang J, Lin M, Huang Y, Wang Y, Huang T, Wu Z, et al. Harnessing hyaluronic acid for the treatment of osteoarthritis: a bibliometric analysis. Front Bioeng Biotechnol. 2022;10:961459.
Ke Y, Jiang W, Xu Y, Chen Y, Zhang Q, Xue Q, et al. Efficacy and safety of a single intra-articular injection of 6 ml Hylan G-F 20 compared to placebo in Chinese patients with symptomatic knee osteoarthritis : C-SOUND study, a 26-week multicenter double-blind randomized placebo-controlled trial in China. BMC Musculoskelet Disord. 2021;22(1):428.
Nishida Y, Kano K, Nobuoka Y, Seo T. Efficacy and safety of diclofenac-hyaluronate conjugate (diclofenac etalhyaluronate) for knee osteoarthritis: a randomized phase iii trial in Japan. Arthritis Rheumatol. 2021;73(9):1646–55.
Sun SF, Lin GC, Hsu CW, Lin HS, Liou IS, Wu SY. Comparing efficacy of intraarticular single crosslinked hyaluronan (HYAJOINT Plus) and platelet-rich plasma (PRP) versus PRP alone for treating knee osteoarthritis. Sci Rep. 2021;11(1):140.
Xu Z, He Z, Shu L, Li X, Ma M, Ye C. Intra-articular platelet-rich plasma combined with hyaluronic acid injection for knee osteoarthritis is superior to platelet-rich plasma or hyaluronic acid alone in inhibiting inflammation and improving pain and function. Arthroscopy. 2021;37(3):903–15.
Chevalier X, Jerosch J, Goupille P, van Dijk N, Luyten FP, Scott DL, et al. Single, intra-articular treatment with 6 ml hylan G-F 20 in patients with symptomatic primary osteoarthritis of the knee: a randomised, multicentre, double-blind, placebo controlled trial. Ann Rheum Dis. 2010;69(01):113–9.
Brandt KD. The role of analgesics in the management of osteoarthritis pain. Am J Ther. 2000;7(2):75–90.
Zhao J, Huang H, Liang G, Zeng LF, Yang W, Liu J. Effects and safety of the combination of platelet-rich plasma (PRP) and hyaluronic acid (HA) in the treatment of knee osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2020;21(1):224.
Marmotti A, Bruzzone M, Bonasia DE, Castoldi F, Rossi R, Piras L, et al. One-step osteochondral repair with cartilage fragments in a composite scaffold. Knee Surg Sports Traumatol Arthrosc. 2012;20(12):2590–601.
Haunschild ED, Huddleston HP, Chahla J, Gilat R, Cole BJ, Yanke AB. Platelet-rich plasma augmentation in meniscal repair surgery: a systematic review of comparative studies. Arthroscopy. 2020;36(6):1765–74.
Everts P, Onishi K, Jayaram P, Lana JF, Mautner K. Platelet-rich plasma: new performance understandings and therapeutic considerations in 2020. Int J Mol Sci. 2020;21(20).
Park YB, Kim JH, Ha CW, Lee DH. Clinical Efficacy of platelet-rich plasma injection and its association with growth factors in the treatment of mild to moderate knee osteoarthritis: a randomized double-blind controlled clinical trial as compared with hyaluronic acid. Am J Sports Med. 2021;49(2):487–96.
Raeissadat SA, Ghazi Hosseini P, Bahrami MH, Salman Roghani R, Fathi M, Gharooee Ahangar A, et al. The comparison effects of intra-articular injection of platelet rich plasma (PRP), plasma rich in growth factor (PRGF), hyaluronic acid (HA), and ozone in knee osteoarthritis; a one year randomized clinical trial. BMC Musculoskelet Disord. 2021;22(1):134.
Sdeek M, Sabry D, El-Sdeek H, Darweash A. Intra-articular injection of Platelet rich plasma versus Hyaluronic acid for moderate knee osteoarthritis. A prospective, double-blind randomized controlled trial on 189 patients with follow-up for three years. Acta Orthop Belg. 2021;87(4):729–34.
Yurtbay A, Say F, Çinka H, Ersoy A. Multiple platelet-rich plasma injections are superior to single PRP injections or saline in osteoarthritis of the knee: the 2-year results of a randomized, double-blind, placebo-controlled clinical trial. Arch Orthop Trauma Surg. 2022;142(10):2755–68.
Chu J, Duan W, Yu Z, Tao T, Xu J, Ma Q, et al. Intra-articular injections of platelet-rich plasma decrease pain and improve functional outcomes than sham saline in patients with knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2022;30(12):4063–71.
Bennell KL, Paterson KL, Metcalf BR, Duong V, Eyles J, Kasza J, et al. Effect of intra-articular platelet-rich plasma vs placebo injection on pain and medial tibial cartilage volume in patients with knee osteoarthritis: The RESTORE Randomized clinical trial. JAMA. 2021;326(20):2021–30.
Dório M, Pereira RMR, Luz AGB, Deveza LA, de Oliveira RM, Fuller R. Efficacy of platelet-rich plasma and plasma for symptomatic treatment of knee osteoarthritis: a double-blinded placebo-controlled randomized clinical trial. BMC Musculoskelet Disord. 2021;22(1):822.
Lewis E, Merghani K, Robertson I, Mulford J, Prentice B, Mathew R, et al. The effectiveness of leucocyte-poor platelet-rich plasma injections on symptomatic early osteoarthritis of the knee: the PEAK randomized controlled trial. Bone Joint J. 2022;104:663–71.
Wang, Y.C., C.L. Lee, Y.J. Chen, Y.C. Tien, S.Y. Lin, C.H. Chen, et al., Comparing the efficacy of intra-articular single platelet-rich plasma(PRP) versus novel crosslinked hyaluronic acid for early-stage knee osteoarthritis: a prospective, double-blind, randomized controlled trial. Medicina (Kaunas), 2022. 58(8).
•• Sax OC, Chen Z, Mont MA, Delanois RE. The Efficacy of platelet-rich plasma for the treatment of knee osteoarthritis symptoms and structural changes: a systematic review and meta-analysis. J Arthroplast. 2022;37(11):2282–2290.e2 The most recent review addressed the clinical relevance of IA platelet-rich plasma comparing with IA corticosteroid, hyaluronic acid, normal saline placebo, and exercises therapies.
Di Matteo B, Vandenbulcke F, Vitale ND, Iacono F, Ashmore K, Marcacci M, et al. Minimally manipulated mesenchymal stem cells for the treatment of knee osteoarthritis: a systematic review of clinical evidence. Stem Cells Int. 2019;2019:1735242.
Anz AW, Plummer HA, Cohen A, Everts PA, Andrews JR, Hackel JG. Bone marrow aspirate concentrate is equivalent to platelet-rich plasma for the treatment of knee osteoarthritis at 2 years: a prospective randomized trial. Am J Sports Med. 2022;50(3):618–29.
Boffa A, Di Martino A, Andriolo L, De Filippis R, Poggi A, Kon E, et al. Bone marrow aspirate concentrate injections provide similar results versus viscosupplementation up to 24 months of follow-up in patients with symptomatic knee osteoarthritis. A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2022;30(12):3958–67.
Hauser RA, Lackner JB, Steilen-Matias D, Harris DK. A systematic review of dextrose prolotherapy for chronic musculoskeletal pain. Clin Med Insights Arthritis Musculoskelet Disord. 2016;9:139–59.
Waluyo Y, Budu A, Bukhari E, Adnan RD, Haryadi II, et al. Changes in levels of cartilage oligomeric proteinase and urinary C-terminal telopeptide of type II collagen in subjects with knee osteoarthritis after dextrose prolotherapy: A randomized controlled trial. J Rehabil Med. 2021;53(5):jrm00196.
Hsieh RL, Lee WC. Effects of intra-articular coinjections of hyaluronic acid and hypertonic dextrose on knee osteoarthritis: a prospective, randomized, double-blind trial. Arch Phys Med Rehabil. 2022;103(8):1505–14.
Simsek, I., T. Phalen, A. Bedenbaugh, M. Phillips, and J. Tambiah, Adjusting for the intra-articular placebo effect in knee osteoarthritis therapies [Abstract]. 2018. 77(Suppl 2): p. 1135-1136.
Previtali D, Merli G, Di Laura Frattura G, Candrian C, Zaffagnini S, Filardo G. The Long-lasting effects of “placebo injections” in knee osteoarthritis: a meta-analysis. Cartilage. 2020:1947603520906597.
Enck P, Bingel U, Schedlowski M, Rief W. The placebo response in medicine: minimize, maximize or personalize? Nat Rev Drug Discov. 2013;12(3):191–204.
Altman RD, Devji T, Bhandari M, Fierlinger A, Niazi F, Christensen R. Clinical benefit of intra-articular saline as a comparator in clinical trials of knee osteoarthritis treatments: a systematic review and meta-analysis of randomized trials. Sem Arthr Rheum. 2016;46(2):151–9.
Maudens P, Jordan O, Allémann E. Recent advances in intra-articular drug delivery systems for osteoarthritis therapy. Drug Discov Today. 2018;23(10):1761–75.
Lima AC, Ferreira H, Reis RL, Neves NM. Biodegradable polymers: an update on drug delivery in bone and cartilage diseases. Expert Opin Drug Deliv. 2019;16(8):795–813.
Gambaro FM, Ummarino A, Torres Andón F, Ronzoni F, Di Matteo B, Kon E. Drug delivery systems for the treatment of knee osteoarthritis: a systematic review of in vivo studies. Int J Mol Sci. 2021;22(17).
Kreuz PC, Steinwachs M, Angele P. Single-dose local anesthetics exhibit a type-, dose-, and time-dependent chondrotoxic effect on chondrocytes and cartilage: a systematic review of the current literature. Knee Surg , Sports Traumatol , Arthrosc. 2018;26(3):819–30.
Jayaram P, Kennedy DJ, Yeh P, Dragoo J. Chondrotoxic effects of local anesthetics on human knee articular cartilage: a systematic review. PM&R. 2019;11(4):379–400.
Ravnihar K, Marš T, Pirkmajer S, Alibegović A, Koželj G, Stožer A, et al. The Influence of a single intra-articular lidocaine injection on the viability of articular cartilage in the knee. Cartilage. 2021;13(1_suppl):456S–63S.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions DJH is supported by an NHMRC Investigator Grant.
Author information
Authors and Affiliations
Contributions
WMO and DJH contributed to the study concept and design. WMO conducted the data search and drafted the first version of the manuscript. DJH and WMO critically revised the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
WMO has no conflict of interest. DJH provides consulting advice on scientific advisory boards for Pfizer, Lilly, TLCBio, Novartis, Tissuegene, Biobone.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 53 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oo, W.M., Hunter, J. Intra-articular Therapies for Knee Osteoarthritis: Current Update. Curr Treat Options in Rheum 9, 99–119 (2023). https://doi.org/10.1007/s40674-023-00207-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40674-023-00207-x