Abstract
House dust mites are a major source of allergens in house dust and, thus, the main trigger of perennial allergic respiratory diseases [1,2,3,4,5]. Scientific research on the life cycle, diet, and reproductive behavior of dust mites and on the biology of mite allergens has uncovered mechanisms leading to the development of respiratory allergies and suggests measures that can minimize exposure to dust mite allergens. Here, we discuss the evidence linking house dust mite exposure and respiratory allergies and present the efficacy of avoidance measures and their scientific evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Historical development of mite avoidance measures
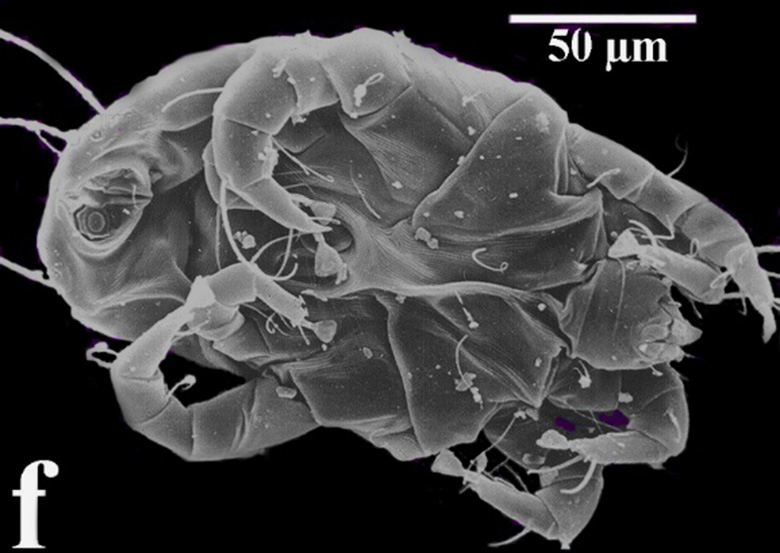
Although the importance of house dust as a source of allergens was recognized as early as the 1920s, mites were not identified as the major source of house dust allergens until 1967 [6, 7]. Microscopic detection of house dust mites rapidly led to the development of techniques for culturing them, allowing the preparation of house dust mite extracts for skin testing and for the detection of specific IgE antibodies [8,9,10]. This has demonstrated that sensitization to house dust mites is strongly associated with asthma development in many temperate zones worldwide [11]. The impact of these findings was dramatic, as this was the first well-defined year-round allergen [12]. Anti-dust mite measures have played and continue to play an important role in scientific discussions [13].
The first purification of a house dust mite allergen was achieved from a house dust mite culture medium and was initially designated F4Pl and later Der p1. This was used to develop a radioimmunoassay to measure the presence of Der p1 in dust samples [14]. Detailed studies on the source of the allergen initially focused on mite feces [15]. Evidence that particles from this become airborne provided important information about the form of exposure and the size of the particles [15,16,17]. This also showed that the percentage of particles entering the peripheral lung during resting breathing decreases with increasing size [18, 19]. Conversely, house dust mite allergens in larger particles (median 9.7 µm) elicit bronchial hyperreactivity at a lower concentration than smaller particles (median 1.1 µm) [20]. The allergens in these particles contribute to progressive inflammation of the airway mucosa in sensitized individuals [21]. The notion that allergen size and sensitization pattern may lead to differences in upper and lower airway involvement is an interesting but insufficiently studied hypothesis [22]. Very little mite allergen remains airborne for more than 10–20 min when stirred up indoors [17]. Thus, probably only a small number of mite fecal particles enter the respiratory tract, usually causing no noticeable symptoms or changes in lung function at the time of exposure [15, 21]. Thus, airway inflammation and symptoms in mite allergic individuals are essentially due to chronic exposure to a small number of relatively large particles, in contrast to pollen inhalation, where sufficient allergens can be inhaled to cause massive immediate phase reactions [15, 21]. Thus, nasal or bronchial provocation testing also represents an artificial special situation [13, 15].
Thus, in inhalation allergies to house dust mites, late-phase allergic responses by effector cells such as eosinophils, T cells, and other inflammatory mechanisms apparently play a greater role than immediate IgE- and mast cell-mediated immediate-phase responses [23,24,25] and rarely lead to immediate respiratory symptoms at the time of exposure [26]. This could also explain the marked allergen-induced nasal and bronchial hyperreactivity [27] which is often more pronounced in mite-allergic patients than in pollen-allergic patients, but which can also be reversed, but only with sufficiently long mite abstinence after several months [28,29,30]. Therefore, mite abstinence must always be a long-term therapeutic measure.
Avoiding allergen contact
An intervention to prevent allergen exposure in an already allergic and symptomatic patient is called tertiary prevention, and some intervention studies have been successful in reducing clinical symptoms [31, 32]. However, tertiary prevention for mite allergic patients is also quite critically viewed [33, 34].
Overall, however, the general principle of “no allergen exposure, no allergic reaction” also seems to make a reduction in mite exposure reasonable [35, 36]. In principle, this also applies to primary care—i.e., avoiding the development of sensitization [37, 38].
However, since exposure periods of only one week and even with relatively low allergen concentrations are sufficient to trigger primary sensitization, measures with this goal seem almost hopeless in regions where house dust mites are generally present [39, 40] especially since exposure can occur anywhere, including the home, school, public buildings, transportation, or the workplace [41]. Consequently, inhalant mite allergy reduction measures serve to control or minimize symptoms of allergic diseases, but they cannot prevent the initiation of sensitization.
General information about mite allergy control measures
The aim of the measures is to avoid contact with the allergens to a large extent, to minimize the number of mites to a large extent, and to create unfavorable living conditions for the remaining mite population [42].
For this purpose, allergy-proof bed and mattress covers (encasing), regular washing of the comforters and bed linen at 60 °C, can be a useful measure for tertiary prevention, if according to international recommendations a mite allergen concentration < 10 micrograms per gram of dust is achieved.
The following procedure is recommended:
-
Prevention of contact with mite allergen (“encasing”),
-
Killing existing mites,
-
Creation of unfavorable living conditions for the remaining mites, and
-
Removal of mite allergen.
Several Cochrane meta-analyses have highlighted some clinical efficacy of individual of the above-mentioned reduction measures [43, 44]. Mite allergen-proof covers (so-called “encasings”) lead to a reduced exposure of the sensitized patient to mite allergens during sleep. The clinical efficacy of this measure has been extensively demonstrated for patients with mite allergic asthma.
Embedded in an overall concept to reduce house dust mite allergens, these individual measures, such as the use of encasing, have a significantly better effect. Measures to reduce mite exposure in the context of secondary and tertiary prevention are also recommended in the 2022 revised guideline on allergy prevention by the German allergological societies [42].
Detection of mite load
In addition to elaborate laboratory chemical detection methods, the detection of significant mite allergen exposure by the guanine method is possible for home use [45, 46]. Here, the guanine, which is present in the mites’ feces, is detected. However, the tests for home use have been withdrawn from the German market in recent years. If required, test kits from foreign companies can be purchased (e.g., Ventia™ Rapid Allergen Test [RT-DM‑1] [Ventia, New South Wales, Australia]).
Prevention of contact with mite allergen
Mite allergen-proof covers are semi-permeable membranes made of polyester, polyamide or natural fibers (cotton), more rarely polyurethane, polytetrafluoroethylene or polyethylene, which completely enclose the mattress, blanket and pillow and can thus significantly reduce allergen exposure in the “bed ecosystem”. These membranes are usually made of nonwoven or woven textile and provide a physical barrier to mite allergen-containing particles. They are offered by various companies. An excerpt is shown in Table 1.
For house dust mite allergic children with asthma, clinical studies have demonstrated that such “encasings” can highly significantly reduce allergen exposure and thus reduce asthmatic symptoms [47]. In a recent study, 46 mite-allergic children with asthma were included and the efficacy of impermeable covers for mattresses and pillows versus mite-permeable placebo covers was investigated over the period of one year [48]. Use of the mite-impermeable covers resulted in significant mite allergen reduction in the mattresses as well as significantly reduced need for inhaled steroids compared to children in the placebo group. Also in a study of 52 adolescent and adult patients with allergic asthma, van den Bemt and coworkers demonstrated that “encasing” resulted in a significant reduction of Der p1 on the mattresses as well as a significant improvement in the morning peak flow of the patients [49].
In the case of allergic rhinitis, inconsistent study results were found [44], which may be due to the different quality of the encasings used. For example, in a study of 279 dust mite allergic patients with allergic rhinitis, there was a significant reduction in mite allergen concentration in the mattresses of the patients who received an encasement, but no improvement in the clinical parameters studied compared to the patients who received a mite-permeable placebo cover [50].
Properties, processing and quality criteria of encasings
Mite allergen impermeable covers should meet the following quality criteria:
Allergen tightness—pore size
The encasing must be able to retain live mites, parts of dead mites, mite excrement and smaller particles to which mite allergens adhere. The pore size should be smaller than 0.5 µm.
-
Quality criterion: TÜV Nord tested (validated and certified test method with real dust mite allergens).
Allergen tightness—complete equipment
All bed components (mattress, blanket, pillow) must be completely enclosed by encasings. A fitted cover for mattresses or toppers is not sufficient. Partner or sibling beds in the same room must also be completely enclosed with encasings.
Processing—textile
In principle, two types of textile are available as suitable encasing material: woven textile and nonwoven (Fig. 1).
-
a.
Nonwoven fabric is formed from fibers or filaments by mechanical, aero- or hydrodynamic processes. The resulting textile has good filtration properties, but may have varying layer thicknesses and irregularities across the surface.
-
b.
Woven textile must be woven particularly tightly, creating a uniformly dense fabric. Postprocessing of the woven textile (“finishing”) further reduces the pore size. The polyurethane coating of encasings, which was common in the past, is no longer necessary due to the use of modern fibers and techniques.
Processing—seams and closures
Particularly in the area of seams and zippers, there are small openings which must be covered by special processing (seam/zipper cuffs, Fig. 2) so that no allergens can penetrate.
Water vapor permeability
A breathable textile (high air and water vapor permeability) has significant therapeutic benefits, especially for neurodermatitis sufferers and people who perspire heavily, as eczema and itching can be prevented.
Woven, uncoated textile is generally more breathable than fleece.
-
Quality criterion: TÜV Nord tested (validated and certified test method)
Qualitative production
All raw materials needed for production must be tested for harmful substances according to OEKO-TEX standards. The manufacturer itself must be ISO certified to ensure the quality standards. There are encasings with OEKO-TEX Standard 100 Class I, which are also suitable for babies.
-
Quality criterion: Hohenstein Institute, OEKO-TEX Standard 100 Class I
Medical device class I according to MDR (Medical device regulation)
Encasings are fundamentally different from so-called “allergy bedding”. Encaisings have a proven safety and effectiveness. In comparison “allergy bedding” is a commodity of everyday life and therefore does not fall within the scope of the health insurers’ obligation to provide benefits (no reimbursement, but personal responsibility of the insured).
Rescribable and reimbursable encasings have:
-
Class I (low risk) registration for non-invasive medical devices, with claims for the treatment and prevention of dust mite allergy,
-
Proven safety: the allergen-tightness within the scope of the perennial application as well as the pollutant-free nature of the raw materials was tested, and
-
Clinically proven efficacy: the recommendation for encasings is found in all dermatological and allergological guidelines (including the current 2022 EDF Guideline, European Dermatology Forum).
Furthermore, a quality management system is required in the manufacturing plants, at least according to ISO 9001, and possibly also ISO 13485.
Encasings are eligible for prescription and reimbursement if they have been approved as a medical device (Class I according to MDR). Manufacturers must be able to prove this by means of a declaration of conformity (CE). This is the qualitative prerequisite for reimbursement by statutory health insurers as a medical device.
Other
Synthetic fibers release moisture more quickly, thus drying faster and providing a poorer breeding ground for bacteria than natural fibers such as cotton. Since encasings should be washed as rarely as possible so as not to impair the impermeability of the material, this hygiene aspect plays an important role.
It is important to distinguish between the different types of encasings [51]. All other materials placed on the mattress should be suitable for regular washing [52]. The washing temperature here should be 60 °C or higher, and the use of a tumble dryer is helpful for killing live mites [52,53,54]. Furthermore, special mite detergents can be used, with allergen eliminating effect.
The mite-allergen-proof covers (“encasings”) awarded the “Material test—suitable for allergy sufferers” test mark by TÜV-Nord is available in German at www.tuev-nord.de, search term “Raumlufthygiene”. There are differences in the reimbursement of mite-allergen-proof covers on the part of the cost bearers. Table 2 shows an excerpt regarding the reimbursement by the statutory health insurance.
In private health insurance, there is no general stipulation on the reimbursement of encasings. Here, insured persons can take out individual insurance coverage tailored to their personal needs. The contractually agreed benefits are generally provided if the treatment is medically necessary. Therefore, it is checked whether a mite allergy is present and whether a treatment to reduce the allergen exposure is necessary. The amount of the insurance benefits depends on the selected insurance coverage and will be checked individually.
We consider the use of encasings to be particularly useful in combination with allergen immunotherapy, especially in the initial phase of allergen immunotherapy. A template from the Ärzteverband deutscher Allergologen (AeDA) can be used for the prescription of encasings.
Acaricides
Acaricides are pesticides or biocides used to control mites. Generally, one can distinguish between mite sprays and mite washes. The mite sprays are mostly based on neem oil, eucalyptus, geraniol and many more. The formerly contained benzyl benzoate is now only allowed in washing additives (excerpt of acaricides on the market in Table 3).
Use as a mite reduction measure may be considered, although no controlled studies of efficacy and absolute population size reduction of individual acaricides are known.
Humidity control
House dust mites depend on relatively high ambient humidity for growth and reproduction, but can survive for extended periods in low-humidity environments [55]. This helps to explain why both dust mite exposure and mite-related respiratory symptoms can vary seasonally and argues for a possible role for humidity reduction measures in mite scarcity [56, 57].
Here, a relative humidity of 45–50% is given as a threshold value to achieve a relevant effect [56, 57]. However, the results from controlled studies on the effect of dehumidification measures on mite abundance have been markedly inconsistent [58,59,60]. This is probably related to the fact that even short periods of increased humidity are sufficient for the survival and reproduction of dust mites. In addition, house dust mites can be found in large numbers even in desert areas if they find high humidity locally, e.g., in apartments where evaporative coolers are used [61,62,63].
Air purifier
Technical options for cleaning indoor air of particulate solids include electrostatic cleaners, in which the charged particles adhere to plates in the device [64]. Alternatively, filters are used in which the particles are physically trapped in the filter. HEPA (high efficiency particulate air) filters consist of a large area of folded paper that allows air to pass through and filter out 99.7% of particles down to 0.1 microns in size. The criticism here is that the exhaust air can swirl out dust and thus possibly swirl up more allergens than the filter removes from the air [65]. The complexity of these various issues underscores the importance of patient education and involvement. There is evidence that HEPA filters can reduce respiratory symptoms in mite allergic patients, suggesting that they may be helpful as part of a multifaceted avoidance strategy [66, 67].
Carpets, furniture, curtains
Several studies have shown that in addition to mattresses, carpets and upholstery materials are important sources of dust mite allergens [68, 69]. Shifting furniture, fluffing or moving pillows, curtains or bedding can release significant amounts of mite allergens into the air [15].
Vacuum cleaners can remove particulate matter such as mite allergens from carpets and upholstered furniture, but cannot reduce live mites to any significant extent because mites can cling to almost any surface with gripping tools on their feet [70, 71]. Even with modern vacuum cleaners, it is therefore impossible to remove all dust mite allergens from a carpet or upholstered furniture. Therefore, humidity control should be emphasized at this point as part of the strategy. Placing carpets in the sun to clean and dry, as has traditionally been done, seems to be most effective. It should be remembered that vacuum cleaners can also stir up dust [72] which should be investigated in industry standard tests [73]. Suitable high-quality filters or extractors can filter out most of the allergen containing particles [74]. Steam cleaners provide little additional benefit in reducing mite allergens [75, 76].
Effects of controlled studies on mite allergen avoidance
The design of a controlled study of mite allergen avoidance is complex and captures many parameters of daily life that are difficult to control (including ventilation behavior, length of stay in rooms, cleaning behavior of mattresses, blankets, sheets, etc.) [77]. In addition, behavioral changes may occur simply due to participation in the study and improved access to information in both the control and intervention groups, which may, for example, render the (additional) effect of an encasing undetectable [50].
Also, in polysensitized patients, symptomatology may be maintained by allergens other than house dust mites, so that the effect of the tested exemption measure is not detectable [78], or patients with relatively well-controlled disease or minimal dust exposure are included [79]. Therefore, it is important to know the mite allergen exposure precisely before starting the intervention over a longer period of time and under different living conditions [31, 32, 35, 74, 80].
Despite all these difficulties, successful studies have been conducted, with the main intervention usually related to beds.
The studies presented below focused on controlled study designs, in addition to the use of physical barriers (encasings), heat treatment to kill mites, additional use of tannic acid to denature mite allergens, and a complex design with measures to control exposure to animal dander, cockroaches, and dust mites [81, 82].
Murray et al. included children with mite asthma and preceding asthma exacerbations with need for hospitalization in a controlled, effectively blinded study of mite abstinence [82]. The result was a significant decrease in exacerbations over the next year.
Discussion
The important role of mite sensitization in the manifestation of perennial allergic rhinoconjunctivitis and/or allergic asthma in industrialized countries is unquestionable [83, 84]. Improved drug therapy options [85] and the modern allergen immunotherapy [36, 86] contribute significantly to an improved morbidity and mortality of these diseases.
Studies on the correlation of early exposure to house dust mites and later development of asthma and/or allergic sensitization show partly contradictory results. Only actual complete allergen exposure avoidance can prevent sensitization. For the development of tolerance, the exposure of the immune system to allergens is necessary. It can be assumed today that small allergen amounts tend to lead to sensitization, whereas higher allergen concentrations tend to induce tolerance. In the U.S. birth cohort study URECA, exposure to house dust mite allergen in the first year of life was not associated with an increased risk of recurrent wheeze at 3 years of age [87]. In a subsample, the microbial content of house dust was additionally examined [87]. A combined analysis of this embedded case–control study showed the lowest rate of allergic sensitization and “wheezing” at 3 years of age in the group of children who had high exposure to both indoor allergens and bacterial endotoxins in the first year of life, suggesting a synergistic effect. In a Finnish birth cohort study, a subanalysis captured associations between quantity and diversity of microbial markers in house dust samples collected at 2 months of age and children’s later respiratory symptoms and allergies [88, 89]. Here, microbial diversity correlated negatively with asthma risk at 6 years of age [88] and at 10.5 years [89]. Other studies found differences in the qualitative and quantitative allergen composition and microbial diversity of house dust from homes where children with and without asthma symptoms grew up [90,91,92]. In particular, the indoor microbiota in urban, poorer neighborhoods appeared to be associated with a risk of developing respiratory symptoms. Further studies are needed to clarify whether the childhood microbiome is altered by this and to better characterize protective and risk factors.
Interventions to reduce the exposure to dust mite allergens in the household are therefore currently not proven useful with the aim of primary prevention, but can be recommended for tertiary prevention of allergic diseases, as evidence of efficacy exists here. We therefore recommend a therapy trial of at least 6 weeks with mite control measures in the case of mild symptoms and additional allergen-specific immunotherapy if there is no improvement. In the case of moderate to severe symptoms, allergen-specific immunotherapy should be administered at the same time as the above-mentioned control measures.
Abbreviations
- AeDA:
-
Ärzteverband deutscher Allergologen
- CE:
-
declaration of conformity
- EDF:
-
European Dermatology Forum
- HEPA-filter:
-
high efficiency particulate air-filter
- MDR:
-
medical device regulation
References
Bergmann K‑C. Frequency of sensitizations and allergies to house dust mites. Allergo J Int. 2022;31:279–83.
Bergmann K‑C. Biology of house dust mites and storage mites. Allergo J Int. 2022;31:272–8.
Brehler R. Clinic and diagnostics of house dust mite allergy. Allergo J Int. 2022; https://doi.org/10.1007/s40629-022-00232-7.
Mülleneisen N, Springob M, Salge S, Völkel A, Magnet F, Callegari J. Der lange Weg von den ersten Symptomen einer Milbenallergie zur Milben-AIT. Allergo J Int. 2022;31:284–7.
Vrtala S. Allergene von Hausstaub- und Vorratsmilben. Allergo J Int. 2022;31:267–71.
Spieksma FTM, Dieges PH. The history of the finding of the house dust mite. J Allergy Clin Immunol. 2004;113:573–6.
Vannier WE, Campbell DH. A starch block electrophoresis study of aqueous house dust extracts. J Allergy. 2003;32:36–54.
Miyamoto T, Oshima S, Ishizaki T, Sato SH. Allergenic identity between the common floor mite (Dermatophagoides farinae Hughes, 1961) and house dust as a causative antigen in bronchial asthma. J Allergy. 1968;42:14–28.
Smith JM, Disney ME, Williams JD, Goels ZA. Clinical significance of skin reactions to mite extracts in children with asthma. Br Med J. 1969;2:723–6.
Wide L, Bennich H, Johansson SG. Diagnosis of allergy by an in-vitro test for allergen antibodies. Lancet. 1967;2:1105–7.
International Workshop report. Dust mite allergens and asthma: a worldwide problem. Bull World Health Organ. 1988;66:769–80.
Platts-Mills TAE. Weck ALd. Dust mite allergens and asthma—A worldwide problem. J Allergy Clin Immunol. 1989;83:416–27.
Platts-Mills TA, Chapman MD. Dust mites: immunology, allergic disease, and environmental control. J Allergy Clin Immunol. 1987;80:755–75.
Chapman MD, Platts-Mills TA. Purification and characterization of the major allergen from Dermatophagoides pteronyssinus-antigen P1. J Immunol. 1980;125:587–92.
Tovey ER, Chapman MD, Wells CW, Platts-Mills TA. The distribution of dust mite allergen in the houses of patients with asthma. Am Rev Respir Dis. 1981;124:630–5.
Busse WW, Reed CE, Hoehne JH. Where is the allergic reaction in ragweed asthma? J Allergy Clin Immunol. 1972;50:289–93.
Platts-Mills TA, Heymann PW, Longbottom JL, Wilkins SR. Airborne allergens associated with asthma: particle sizes carrying dust mite and rat allergens measured with a cascade impactor. J Allergy Clin Immunol. 1986;77:850–7.
Bates DV, Fish BR, Hatch TF, Mercer TT, Morrow PE. Deposition and retention models for internal dosimetry of the human respiratory tract. Task group on lung dynamics. Health Phys. 1966;12:173–207.
Svartengren M, Falk R, Linnman L, Philipson K, Camner P. Deposition of large particles in human lung. Exp Lung Res. 1987;12:75–88.
Casset A, Purohit A, Birba E, Chenard MP, Uring Lambert B, Bahram S, et al. Bronchial challenge test in asthmatics sensitized to mites: role of particle size in bronchial response. J Aerosol Med. 2007;20:509–18.
Platts-Mills TAE, Mitchell EB, Tovey ER, Chapman MD, Wilkins SR. Airborne allergen exposure, allergen avoidance and bronchial hyperreactivity In. In: Kay AB, Austen KF, Lichtenstein LM, editors. Asthma physiology, immunopharmacology, and treatment: Third International Symposium London. Orlando: Academic Press; 1984. pp. 297–314.
Schiphof-Godart L, van der Wiel E, Ten Hacken NH, van den Berge M, Postma DS, van der Molen T. Development of a tool to recognize small airways dysfunction in asthma (SADT). Health Qual Life Outcomes. 2014;12:155.
Dullaers M, Schuijs MJ, Willart M, Fierens K, Van Moorleghem J, Hammad H, et al. House dust mite-driven asthma and allergen-specific T cells depend on B cells when the amount of inhaled allergen is limiting. J Allergy Clin Immunol. 2017;140:76–88.e7.
Nathan AT, Peterson EA, Chakir J, Wills-Karp M. Innate immune responses of airway epithelium to house dust mite are mediated through beta-glucan-dependent pathways. J Allergy Clin Immunol. 2009;123:612–8.
Rawle FC, Mitchell EB, Platts-Mills TA. T cell responses to the major allergen from the house dust mite Dermatophagoides pteronyssinus, Antigen P1: comparison of patients with asthma, atopic dermatitis, and perennial rhinitis. J Immunol. 1984;133:195–201.
Woodfolk JA, Commins SP, Schuyler AJ, Erwin EA, Platts-Mills TAE. Allergens, sources, particles, and molecules: Why do we make IgE responses? Allergol Int. 2015;64:295–303.
Richards IM, Jackson DM, Altounyan RE. Airway hyperreactivity and its relationship to sodium cromoglycate. Agents Actions Suppl. 1983;13:51–3.
Charpin D, Birnbaum J, Haddi E, Genard G, Lanteaume A, Toumi M, et al. Altitude and allergy to house-dust mites. A paradigm of the influence of environmental exposure on allergic sensitization. Am Rev Respir Dis. 1991;143:983–6.
Kerrebijn K. Endogenous factors in childhood CNSLD: methodological aspects in population studies. Bronchitis. 1970;III:38–48.
Piacentini GL, Martinati L, Mingoni S, Boner AL. Influence of allergen avoidance on the eosinophil phase of airway inflammation in children with allergic asthma. J Allergy Clin Immunol. 1996;97:1079–84.
Custovic A, Simpson A, Chapman MD, Woodcock A. Allergen avoidance in the treatment of asthma and atopic disorders. Thorax. 1998;53:63–72.
Marks GB. House dust mite exposure as a risk factor for asthma: benefits of avoidance. Allergy. 1998;53:108–14.
Gøtzsche PC, Johansen HK. House dust mite control measures for asthma: systematic review. Allergy. 2008;63:646–59.
Gøtzsche PC, Johansen HK, Schmidt LM, Burr ML. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2004;4:CD1187.
Platts-Mills TAE. Allergen avoidance in the treatment of asthma: problems with the meta-analyses. J Allergy Clin Immunol. 2008;122:694–6.
Portnoy J, Miller JD, Williams PB, Chew GL, Miller JD, Zaitoun F, et al. Environmental assessment and exposure control of dust mites: a practice parameter. Ann Allergy Asthma Immunol. 2013;111:465–507.
Perzanowski MS, Ronmark E, James HR, Hedman L, Schuyler AJ, Bjerg A, et al. Relevance of specific IgE antibody titer to the prevalence, severity, and persistence of asthma among 19-year-olds in northern Sweden. J Allergy Clin Immunol. 2016;138:1582–90.
Sporik R, Ingram JM, Price W, Sussman JH, Honsinger RW, Platts-Mills TA. Association of asthma with serum IgE and skin test reactivity to allergens among children living at high altitude. Tickling the dragon’s breath. Am J Respir Crit Care Med. 1995;151:1388–92.
Warner AM, Bjorksten B, Munir AK, Moller C, Schou C, Kjellman NI. Childhood asthma and exposure to indoor allergens: low mite levels are associated with sensitivity. Pediatr Allergy Immunol. 1996;7:61–7.
Woodcock A, Lowe LA, Murray CS, Simpson BM, Pipis SD, Kissen P, et al. Early life environmental control: effect on symptoms, sensitization, and lung function at age 3 years. Am J Respir Crit Care Med. 2004;170:433–9.
Custovic A, Taggart SC, Woodcock A. House dust mite and cat allergen in different indoor environments. Clin Exp Allergy. 1994;24:1164–8.
Kopp MV, Muche-Borowski C, Abou-Dakn M, Ahrens B, Beyer K, Blümchen K, et al. S3 guideline allergy prevention. Allergol Sel. 2022;6:61–97.
Nurmatov U, van Schayck CP, Hurwitz B, Sheikh A. House dust mite avoidance measures for perennial allergic rhinitis: an updated Cochrane systematic review. Allergy. 2012;67:158–65.
Sheikh A, Hurwitz B, Nurmatov U, van Schayck CP. House dust mite avoidance measures for perennial allergic rhinitis. Cochrane Database Syst Rev. 2010;2010:CD1563.
Bischoff E, Schirmacher W. Farbnachweis für allergenhaltigen Hausstaub. 2. Mitteilung: Weitere Gesichtspunkte. Allergologie. 1985;8:36–8.
Hill MR. Quantification of house-dust-mite populations. Allergy. 1998;53:18–23.
Ehnert B, Lau-Schadendorf S, Weber A, Buettner P, Schou C, Wahn U. Reducing domestic exposure to dust mite allergen reduces bronchial hyperreactivity in sensitive children with asthma. J Allergy Clin Immunol. 1992;90:135–8.
Halken S, Høst A, Niklassen U, Hansen LG, Nielsen F, Pedersen S, et al. Effect of mattress and pillow encasings on children with asthma and house dust mite allergy. J Allergy Clin Immunol. 2003;111:169–76.
van den Bemt L, van Knapen L, de Vries MP, Jansen M, Cloosterman S, van Schayck CP. Clinical effectiveness of a mite allergen-impermeable bed-covering system in asthmatic mite-sensitive patients. J Allergy Clin Immunol. 2004;114:858–62.
Terreehorst I, Hak E, Oosting AJ, Tempels-Pavlica Z, de Monchy JG, Bruijnzeel-Koomen CA, et al. Evaluation of impermeable covers for bedding in patients with allergic rhinitis. N Engl J Med. 2003;349:237–46.
Miller JD, Naccara L, Satinover S, Platts-Mills TA. Nonwoven in contrast to woven mattress encasings accumulate mite and cat allergen. J Allergy Clin Immunol. 2007;120:977–9.
Choi SY, Lee IY, Sohn JH, Lee YW, Shin YS, Yong TS, et al. Optimal conditions for the removal of house dust mite, dog dander, and pollen allergens using mechanical laundry. Ann Allergy Asthma Immunol. 2008;100:583–8.
Miller JD. Difference in mite survival in blankets washed in top-loading vs. Front-loading washing machines. J Allergy Clin Immunol. 2017;139:AB119.
Mason K, Riley G, Siebers R, Crane J, Fitzharris P. Hot tumble drying and mite survival in duvets. J Allergy Clin Immunol. 1999;104:499–500.
Arlian LG. Water balance and humidity requirements of house dust mites. Exp Appl Acarol. 1992;16:15–35.
Hervas D, Pons J, Mila J, Matamoros N, Hervas JA, Garcia-Marcos L. Specific IgE levels to dermatophagoides pteronyssinus are associated with meteorological factors. Int Arch Allergy Immunol. 2013;160:383–6.
Platts-Mills TA, Hayden ML, Chapman MD, Wilkins SR. Seasonal variation in dust mite and grass-pollen allergens in dust from the houses of patients with asthma. J Allergy Clin Immunol. 1987;79:781–91.
Arlian LG, Neal JS, Morgan MS, Vyszenski-Moher DL, Rapp CM, Alexander AK. Reducing relative humidity is a practical way to control dust mites and their allergens in homes in temperate climates. J Allergy Clin Immunol. 2001;107:99–104.
Arlian LG, Neal JS, Vyszenski-Moher DL. Reducing relative humidity to control the house dust mite dermatophagoides farinae. J Allergy Clin Immunol. 1999;104:852–6.
Singh M, Jaiswal N. Dehumidifiers for chronic asthma. Cochrane Database Syst Rev. 2013;2013:CD3563.
Ellingson AR, LeDoux RA, Vedanthan PK, Weber RW. The prevalence of Dermatophagoides mite allergen in Colorado homes utilizing central evaporative coolers. J Allergy Clin Immunol. 1995;96:473–9.
Johnston JD, Barney TP, Crandall JH, Brown MA, Westover TR, Paulson SM, et al. Prevalence of house dust mite allergens in low-income homes with evaporative coolers in a semiarid climate. Arch Environ Occup Health. 2018;73:38–41.
Prasad C, Hogan MB, Peele K, Wilson NW. Effect of evaporative coolers on skin test reactivity to dust mites and molds in a desert environment. Allergy Asthma Proc. 2009;30:624–7.
Custis NJ, Woodfolk JA, Vaughan JW, Platts-Mills TA. Quantitative measurement of airborne allergens from dust mites, dogs, and cats using an ion-charging device. Clin Exp Allergy. 2003;33:986–91.
Luczynska CM, Li Y, Chapman MD, Platts-Mills TA. Airborne concentrations and particle size distribution of allergen derived from domestic cats (Felis domesticus). Measurements using cascade impactor, liquid impinger, and a two-site monoclonal antibody assay for Fel d I. Am Rev Respir Dis. 1990;141:361–7.
Antonicelli L, Bilo MB, Pucci S, Schou C, Bonifazi F. Efficacy of an air-cleaning device equipped with a high efficiency particulate air filter in house dust mite respiratory allergy. Allergy. 1991;46:594–600.
Reisman RE, Mauriello PM, Davis GB, Georgitis JW, DeMasi JM. A double-blind study of the effectiveness of a high-efficiency particulate air (HEPA) filter in the treatment of patients with perennial allergic rhinitis and asthma. J Allergy Clin Immunol. 1990;85:1050–7.
Sidenius KE, Hallas TE, Brygge T, Poulsen LK, Mosbech H. House dust mites and their allergens at selected locations in the homes of house dust mite-allergic patients. Clin Exp Allergy. 2002;32:1299–304.
Van Strien RT, Verhoeff AP, Brunekreef B, Van Wijnen JH. Mite antigen in house dust: relationship with different housing characteristics in the Netherlands. Clin Exp Allergy. 1994;24:843–53.
de Boer R. The control of house dust mite allergens in rugs. J Allergy Clin Immunol. 1990;86:808–14.
Wickman M, Paues S, Emenius G. Reduction of the mite-allergen reservoir within mattresses by vacuum-cleaning. A comparison of three vacuum-cleaning systems. Allergy. 1997;52:1123–7.
Gore RB, Durrell B, Bishop S, Curbishley L, Woodcock A, Custovic A. High-efficiency vacuum cleaners increase personal mite allergen exposure, but only slightly. Allergy. 2006;61:119–23.
Vaughan JW, Woodfolk JA, Platts-Mills TA. Assessment of vacuum cleaners and vacuum cleaner bags recommended for allergic subjects. J Allergy Clin Immunol. 1999;104:1079–83.
Platts-Mills TA, Vaughan JW, Carter MC, Woodfolk JA. The role of intervention in established allergy: avoidance of indoor allergens in the treatment of chronic allergic disease. J Allergy Clin Immunol. 2000;106:787–804.
Vojta PJ, Randels SP, Stout J, Muilenberg M, Burge HA, Lynn H, et al. Effects of physical interventions on house dust mite allergen levels in carpet, bed, and upholstery dust in low-income, urban homes. Environ Health Perspect. 2001;109:815–9.
Yu CH, Yiin LM, Tina Fan ZH, Rhoads GG. Evaluation of HEPA vacuum cleaning and dry steam cleaning in reducing levels of polycyclic aromatic hydrocarbons and house dust mite allergens in carpets. J Environ Monit. 2009;11:205–11.
Woodcock A, Forster L, Matthews E, Martin J, Letley L, Vickers M, et al. Control of exposure to mite allergen and allergen-impermeable bed covers for adults with asthma. N Engl J Med. 2003;349:225–36.
Rijssenbeek-Nouwens LH, Oosting AJ, de Bruin-Weller MS, Bregman I, de Monchy JG, Postma DS. Clinical evaluation of the effect of anti-allergic mattress covers in patients with moderate to severe asthma and house dust mite allergy: a randomised double blind placebo controlled study. Thorax. 2002;57:784–90.
de Vries MP, van den Bemt L, Aretz K, Thoonen BP, Muris JW, Kester AD, et al. House dust mite allergen avoidance and self-management in allergic patients with asthma: randomised controlled trial. Br J Gen Pract. 2007;57:184–90.
Colloff M. Dust mites. Vol. xvi. Collingwood: CSIRO; 2009. p. 583.
Morgan WJ, Crain EF, Gruchalla RS, O’Connor GT, Kattan M, Evans R 3rd, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351:1068–80.
Murray CS, Foden P, Sumner H, Shepley E, Custovic A, Simpson A. Preventing severe asthma exacerbations in children. A randomized trial of mite-impermeable bedcovers. Am J Respir Crit Care Med. 2017;196:150–8.
Erwin EA, Wickens K, Custis NJ, Siebers R, Woodfolk J, Barry D, et al. Cat and dust mite sensitivity and tolerance in relation to wheezing among children raised with high exposure to both allergens. J Allergy Clin Immunol. 2005;115:74–9.
Soto-Quiros M, Avila L, Platts-Mills TA, Hunt JF, Erdman DD, Carper H, et al. High titers of IgE antibody to dust mite allergen and risk for wheezing among asthmatic children infected with rhinovirus. J Allergy Clin Immunol. 2012;129:1499–1505 e5.
Busse WW, Morgan WJ, Gergen PJ, Mitchell HE, Gern JE, Liu AH, et al. Randomized trial of omalizumab (anti-IgE) for asthma in inner-city children. N Engl J Med. 2011;364:1005–15.
Klimek L, Brehler R, Casper I, Klimek F, Hagemann J, Cuevas M, et al. Allergen-Immuntherapie bei HSM-AR: Wirksamkeit der 300 IR Milbentablette. Allergo J Int. 2023;32:10–7. https://doi.org/10.1007/s40629-022-00241-6.
Lynch SV, Wood RA, Boushey H, Bacharier LB, Bloomberg GR, Kattan M, et al. Effects of early-life exposure to allergens and bacteria on recurrent wheeze and atopy in urban children. J Allergy Clin Immunol. 2014;134:593–601.e12.
Karvonen AM, Hyvärinen A, Rintala H, Korppi M, Täubel M, Doekes G, et al. Quantity and diversity of environmental microbial exposure and development of asthma: a birth cohort study. Allergy. 2014;69:1092–101.
Karvonen AM, Kirjavainen PV, Täubel M, Jayaprakash B, Adams RI, Sordillo JE, et al. Indoor bacterial microbiota and development of asthma by 10.5 years of age. J Allergy Clin Immunol. 2019;144:1402–10.
Ciaccio CE, Barnes C, Kennedy K, Chan M, Portnoy J, Rosenwasser L. Home dust microbiota is disordered in homes of low-income asthmatic children. J Asthma. 2015;52:873–80.
Loo EXL, Chew LJM, Zulkifli AB, Ta LDH, Kuo IC, Goh A, et al. Comparison of microbiota and allergen profile in house dust from homes of allergic and non-allergic subjects-results from the GUSTO study. World Allergy Organ J. 2018;11:37.
Thorne PS, Kulhánková K, Yin M, Cohn R, Arbes SJ, Zeldin DC. Endotoxin exposure is a risk factor for asthma: the national survey of endotoxin in United States housing. Am J Respir Crit Care Med. 2005;172:1371–7.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
L. Klimek reports grants and/or honoraria from Allergopharma, MEDA/Mylan, HAL Allergie, ALK Abelló, ALLERGIKA, LETI Pharma, Stallergenes, Quintiles, Sanofi, grants from ASIT Biotech, Lofarma, Allergy Therapeutics, AstraZeneca, GSK, Inmunotek, Cassella med, outside the submitted work; and memberships with: AeDA, DGHNO, German Academy of Allergology and Clinical Immunology, ENT-BV, GPA and EAACI. L. Klimek is editor in chief of Allergo Journal International. R. Brehler reports honoraria from ALK, Allergopharma, Bencard, HAL, Leti, Stallergenes, Astra Zeneca, GSK, MedUpdate, Novertis, BiotechTools, Genentech and Circassia, outside the submitted work. K.‑C. Bergmann received honoraria from Allergopharma, HAL Allergie, ALK Abelló, LETI Pharma, Stallergenes, Sanofi, Lofarma, Novartis, Bencard Allergy Therapeutics, AstraZeneca and GSK, outside the submitted work. I. Casper, F. Klimek, J. Hagemann, M.-L. Polk and M. Cuevas declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Klimek, L., Brehler, R., Bergmann, KC. et al. Avoidance measures for mite allergy—an update. Allergo J Int 32, 18–27 (2023). https://doi.org/10.1007/s40629-022-00242-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40629-022-00242-5