Abstract
Background
Echocardiography is commonly used to assess hydratation status and cardiac function in kidney failure patients, but the impact of structural or functional abnormalities on the prognosis of kidney failure patients was yet to be investigated. This study aimed to investigate the prevalence and clinical significance of echocardiographic abnormalities in kidney failure patients.
Methods
This study included 857 kidney failure patients who underwent echocardiography at dialysis initiation. Patients were followed up for a median of 4.2 years for the occurrence of major adverse cardiovascular events (MACE) and all-cause mortality.
Results
Among the 857 patients studied, 77% exhibited at least one echocardiographic abnormality. The most common abnormalities were left ventricular hypertrophy and left atrial enlargement, but they were not significantly correlated with poor outcomes. Instead, the primary predictors of both major adverse cardiovascular events and mortality in kidney failure patients were left ventricular systolic function, right ventricular systolic function, left ventricular volume index, and valvular abnormalities. Although diastolic dysfunction was linked to major adverse cardiovascular events, it was not associated with mortality. Furthermore, the study revealed that increased left ventricular volume index and left ventricular systolic dysfunction had a more significant impact on peritoneal dialysis (PD) patients than on hemodialysis (HD) patients.
Conclusion
This study provides insights into the echocardiographic abnormalities and their association with adverse outcomes in kidney failure patients, which can help clinicians optimize the management of patients and closely monitor possible high-risk populations.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kidney failure patients have a high mortality rate, with cardiovascular disease being the leading cause [1]. The kidneys have an essential role in maintaining blood pressure and eliminating waste products and surplus fluids from the body. However, when the kidneys fail to function properly, waste products and fluids can accumulate in the body, leading to type 4 cardiorenal syndrome and cardiac remodeling [2]. This process involves structural and functional changes in the heart, primarily left ventricular dilatation, hypertrophy, and diastolic dysfunction, which significantly increase the risk of cardiovascular events [3]. In addition, accelerated atherosclerosis, dialysis-related hemodynamic instability, and acute electrolyte changes, all contribute to the high cardiovascular mortality in kidney failure patients [4, 5]. The current heart failure classification systems, such as the AHA and NYHA systems, are largely based on symptoms and functional capacity. However, these systems may not be suitable for patients with kidney failure due to the complex interactions between fluid overload, left ventricular (LV) preload, and structural changes in the heart. Additionally, kidney failure patients may have different symptoms and functional limitations compared to patients with heart failure alone.
Echocardiography is commonly used as the primary method for evaluating cardiac function and structure. As a result, it is also considered one of the most accessible and robust examinations for evaluating heart failure in patients with kidney failure [6,7,8]. According to the Kidney Disease Outcomes Quality Initiative (KDOQI) guideline recommendation, all new dialysis patients should undergo an echocardiographic exam in the initial phase of dialysis once the patient has achieved dry weight to access the fluid status, and every 3 years thereafter [9]. However, not all dialysis centers have access to echocardiography or trained personnel to perform and interpret the exams. There is also a lack of standardized protocols for echocardiography in kidney failure patients, in addition, the cost of echocardiography can be a barrier for some patients or healthcare systems.
When using echocardiography to evaluate kidney failure patients, several parameters are examined to assess cardiac function. Although left ventricular ejection fraction (LVEF) is commonly considered a crucial parameter, other factors such as left atrial size, left ventricular mass, and diastolic function may also hold significance. However, the impact of these echocardiographic abnormalities on the predictive value of adverse cardiovascular outcomes in kidney failure patients is yet to be investigated. The present study aims at investigating the potential clinical implications of baseline echocardiography and evaluating the predictive value of echocardiographic parameters on the outcomes.
Methods
Study design and patient selection
We included patients who started long-term outpatient peritoneal dialysis (PD) (n = 383) or chronic hemodialysis (HD) (n = 664) between 2006 and 2020 at Taipei Veterans General Hospital and excluded those who did not undergo echocardiogram examination within 3 months of starting dialysis (n = 190). The primary outcomes of this study were major adverse cardiovascular events (MACE) and all-cause mortality; patients were followed up for 5 years or until the end of the study (July 31, 2021). The baseline characteristics of the patients, such as age, gender, height, body weight, dialysis modality, comorbidities, cause of kidney failure, and medication history were collected from electronic medical records. The investigation adhered to the Declaration of Helsinki with the approval of the Institutional review board of Taipei Veteran General Hospital.
Echocardiography parameters and definition of abnormality
Left ventricular ejection fraction was obtained manually at end-diastole and end-systole in four-chamber and two-chamber views using the modified biplane Simpson’s method [10]. Left ventricular systolic dysfunction was defined as a left ventricular ejection fraction of 45% or lower. Cardiac abnormality was defined according to the American Society of Echocardiography (ASE) and European Society of Cardiology guidelines with minor modifications to account for kidney failure patients [11,12,13]. For the purpose of this study, seven parameters were utilized to assess cardiac function. Left ventricular hypertrophy (LVH) was defined as left ventricular mass index (LVMi) greater than 100 g/m2 for women and greater than 130 g/m2 for men. Increased left ventricular volume index (LVVi) was defined as greater than 86 ml/m2 end-diastolic volume or greater than 37 ml/m2 end-systolic volume. Right ventricular systolic dysfunction was defined as tricuspid annular plane systolic excursion (TAPSE) < 1.6 cm or right ventricular pulsed doppler peak systolic velocity at the annulus (RVS’) < 10 cm/s [14]. Pulmonary hypertension was defined as pulmonary artery systolic pressure more than 35 mmHg. Left atrial enlargement (LAE) was defined as left atrial (LA) size greater than 40 mm. Diastolic dysfunction was defined according to the 2016 ASE guideline recommendation but using left atrial size as a surrogate of the left atrial volume index [15]. Valvular diseases with moderate to severe stenosis or regurgitation were also considered as a distinct parameter of cardiac abnormality.
Outcomes of interest
Patients were followed up for all-cause mortality and major adverse cardiovascular events including non-fatal stroke, non-fatal myocardial infarction, and hospitalization for heart failure.
Statistical analysis
Baseline characteristics were presented as means with standard deviation for continuous variables, and percentages for categorical variables. Comparisons of proportions between groups were made using the Chi-square test. Continuous variables were compared using independent t test. Event rates were presented with Kaplan–Meier methods and compared by log-rank test. Cox proportional hazard model was utilized to access the risk of each echocardiographic abnormality on major adverse cardiovascular events and mortality. Multivariate model was based on the factors with p < 0.1 in the univariate analysis. All analyses were performed using IBM SPSS Statistics 25.0 software (Armonk, NY: IBM Corp.). All the tests performed were 2 sided, and p value < 0.05 was considered statistically significant.
Results
Study cohort
Between January 2006 and December 2020, a total of 1047 patients began long-term dialysis treatment in Taipei Veterans General Hospital, with 383 receiving PD and 664 receiving HD. After excluding 190 patients who did not receive an echocardiogram within 3 months of dialysis initiation, 857 patients met the study inclusion criteria. The mean age of the study population was 62 ± 12 years, with 445 (52%) patients being male, 275 (32%) receiving PD, and 131 (15%) having a history of heart failure. The most common causes of kidney failure were diabetes mellitus (39%), hypertension (20%), and glomerulonephritis (14%).
Among the study population, 659 patients (77%) had one or more echocardiographic abnormalities. Patients with diabetes, a history of heart failure, and higher body weight were more likely to have abnormal echocardiograms (Table 1).
Echocardiographic findings in kidney failure patients
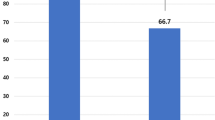
Most patients with an abnormal echocardiogram have more than one abnormal parameter. The most frequently observed abnormalities were left ventricular hypertrophy (56%), diastolic dysfunction (49%), and left atrial enlargement (45%). Mitral regurgitation was the most common valvular abnormality, present in 9% of patients. Right ventricular systolic dysfunction was observed in 5% of patients (Table 2). The average age was higher among the HD patients compared to PD patients (65.68 ± 16.07 vs 53.42 ± 14.67, p < 0.001). In addition, a greater prevalence of left atrial enlargement, diastolic dysfunction, and pulmonary hypertension among HD patients was also identified in the present study (Fig. 1). The echocardiographic findings relative to the type of dialysis vascular access are presented in Supplementary Table 1. Notably, left atrial size was significantly larger in subjects with arteriovenous fistulas (AVFs) compared to those using central venous catheters (CVCs). Apart from this distinction, other parameters including left ventricular mass index, left ventricular volume index, left ventricular ejection fraction, diastolic function, pulmonary artery systolic pressure (PASP), and right ventricular function showed no significant differences between the two groups.
Echocardiographic abnormalities and patient outcomes
During a mean follow-up period of 4.28 ± 2.61 years, a total of 183 patients developed major adverse cardiovascular events while 185 patients died. The cumulative survival rate at 1 year, 3 years, and 5 years was 93%, 84%, and 79%, respectively, which is consistent with the mortality rate of dialysis patients in Taiwan [16].
Patients who exhibited abnormalities on echocardiography had significantly higher rates of both major adverse cardiovascular events (log-rank p = 0.002) and total mortality (log-rank p = 0.011) compared to those without abnormalities. The Kaplan–Meier figures demonstrated that all echocardiographic abnormalities, except for left ventricular hypertrophy and left atrial enlargement, were associated with an increased risk of 5-year all-cause mortality (Fig. 2). Additionally, most echocardiographic abnormalities, except for left ventricular hypertrophy, were found to be associated with an increased risk of major adverse cardiovascular events (Fig. 3). To assess the association between echocardiographic abnormalities and outcomes, we performed a Cox proportional hazard model analysis, adjusting for age, sex, comorbidities, and medications. Our findings showed that left ventricular systolic dysfunction (HR, 95% CI 2.31, 1.56–3.41, p < 0.001), left ventricular volume index (HR, 95% CI 1.93, 1.30–2.90, p = 0.001), right ventricular dysfunction (HR, 95% CI 1.86, 1.09–3.19, p = 0.024), valvular heart disease (HR, 95% CI 1.75, 1.22–2.51, p = 0.002), and pulmonary hypertension (HR, 95% CI 1.72, 1.25–2.34, p < 0.001) were significantly associated with a higher mortality rate (Table 3). Similarly, right ventricular systolic dysfunction (HR, 95% CI 2.36, 1.44–3.86, p = 0.001), left ventricular systolic dysfunction (HR, 95% CI 2.20, 1.47–3.30, p < 0.001), left ventricular volume index (HR, 95% CI 1.98, 1.34–2.94, p < 0.001), and valvular heart disease (HR, 95% CI 1.81, 1.25–2.61, p = 0.002) were identified as the independent risk factors for major adverse cardiovascular events. (Table 4).
Survival analysis of abnormal echocardiographic parameters in the dialysis population. Kaplan–Meier survival curve analysis of mortality over a 5-year follow-up period in relation to specific echocardiographic abnormalities including right ventricular systolic dysfunction, left ventricular systolic dysfunction, left ventricular volume index, and moderate to severe valvular heart disease
Impact of specific echocardiographic abnormalities on major adverse cardiovascular events (MACE) in dialysis patients. Kaplan–Meier survival curve analysis of mortality over a 5-year follow-up period in relation to specific echocardiographic abnormalities including right ventricular systolic dysfunction, left ventricular systolic dysfunction, left ventricular volume index, and moderate to severe valvular heart disease
Subgroup analysis of the interaction between dialysis modalities and specific echocardiographic abnormalities
The 5-year survival rate was 76.5% and 82.5% in HD and PD subjects, respectively. Hemodialysis can cause fluctuations in blood pressure and volume, as well as changes in electrolyte levels. In contrast, PD does not cause as many rapid shifts in fluid, but both HD and PD can have negative effects on the heart over time [17, 18]. To evaluate the interaction between dialysis modality and each echocardiographic abnormality on mortality and major adverse cardiovascular events, we performed subgroup analysis of interaction between dialysis modality and echocardiogram abnormalities on patient outcomes. The findings demonstrated that in PD patients, left ventricular systolic dysfunction (p for interaction = 0.019) and elevated left ventricular volume index (p for interaction < 0.001) were more strongly associated with increased mortality risk compared to HD patients (Fig. 4A). Conversely, there was no notable interaction between dialysis modality and echocardiographic abnormalities in predicting major adverse cardiovascular events (Fig. 4B).
Discussion
The present study investigated the potential clinical implications of baseline echocardiography beyond its conventional use for assessing fluid status in kidney failure patients. Our findings demonstrated that a high percentage of patients exhibited at least one echocardiographic abnormality, with left ventricular hypertrophy and left atrial enlargement being the most common. However, these abnormalities were not found to be associated with adverse outcomes. On the other hand, left ventricular systolic dysfunction, diastolic dysfunction and valvular heart disease were found to be significant risk factors for major adverse cardiovascular events in kidney failure patients, consistent with their established association in the general population. In addition, right ventricular dysfunction and increased left ventricular volume index were also identified as predictors of poor outcome in this patient population. Furthermore, left ventricular systolic dysfunction and left ventricular volume index had a higher predictive value for mortality in patients on PD compared with patients on HD.
Although almost all echocardiographic parameters were associated with patient outcomes, left ventricular systolic function, right ventricular systolic function, and left ventricular volume index were the most important parameters associated with both major adverse cardiovascular events and mortality in our study. It is important to note that right ventricular systolic dysfunction was rare, occurring in only 5% of patients, but had the strongest association with major adverse cardiovascular events. In kidney failure patients, it is especially important to monitor right ventricular dysfunction due to the preload-dependent characteristic of the right ventricle and the vulnerability of fluid overload in this population [19]. In a study with 654 patients under chronic dialysis, Hickson et al., demonstrated that reduced left ventricular ejection fraction and right ventricular systolic dysfunction were independent risk factors for mortality [11]. However, our study, which had a larger sample size and longer follow-up period, revealed that abnormal left ventricular volume index and valvular heart disease were also independent risk factors for both major adverse cardiovascular events and death in this population.
Left ventricular hypertrophy and high left ventricular volume index represent distinct forms of left ventricular remodeling, each characterized by unique pathophysiological mechanisms. Left ventricular hypertrophy refers to an increase in mass of the left ventricle, which is commonly caused by chronic pressure overload. On the other hand, high left ventricular volume index refers to an enlargement of the left ventricular cavity, which is typically caused by chronic volume overload [20]. In the present study, left ventricular hypertrophy is the most prevalent echocardiographic abnormality in kidney failure patients. Left ventricular hypertrophy is a frequently encountered cardiac abnormality in kidney failure patients due to chronic hypertension; however, data from our study and other groups suggest left ventricular hypertrophy is not an independent factor of poor outcomes in dialysis patients [21,22,23]. In the present study, left atrial enlargement is also a prevalent echocardiography abnormality in kidney failure patients. Atrial fibrillation (Af), mitral valve disease, and left ventricular diastolic dysfunction are common etiologies for left atrial enlargement. Kidney failure patients have a higher prevalence of atrial fibrillation compared to the general population. Several studies have reported that the prevalence of atrial fibrillation in dialysis patients ranges from 8 to 27% [24, 25], which is significantly higher than the 1~2% prevalence of atrial fibrillation in the general population [26]. In the current study, 10% of the participants had mitral valve disease, and 49% had diastolic dysfunction. These findings were in line with the high occurrence of left atrial enlargement that reaches up to 45%. However, left atrial enlargement was not an independent predictor for either mortality or major adverse cardiovascular events.
Fluid overload is a common and important complication encountered in the care of kidney failure patients. Interestingly, we observed that the prognostic value of the baseline left ventricular systolic dysfunction and left ventricular volume index differed depending on the dialysis modality. Although left ventricular systolic dysfunction is a negative predictor of mortality in both PD and HD patients, its effect is more pronounced in PD patients than in HD patients (p for interaction = 0.019). Furthermore, higher left ventricular volume index is a significant risk factor for mortality in PD patients but not in HD patients (p for interaction < 0.001). A similar trend was also found in the prediction of major adverse cardiovascular events. Although there was no significant difference in the predictive value of pulmonary hypertension between PD and HD patients, there was a noticeable trend towards a higher predictive value in PD patients (with interaction p values of 0.079 for mortality and 0.055 for major adverse cardiovascular events. (Table 4) This lack of significance could be attributed to the broad standard deviation among PD patients, who were represented by a smaller sample size compared to HD patients (247 vs. 583, respectively). These observations highlight the challenge of fluid control in PD. Continuous and slower ultrafiltration rates during PD may increase the risk of fluid overload without causing any clinical symptoms [27, 28]. In a study of 311 patients, it was found that asymptomatic fluid overload is a frequent occurrence among incident PD patients and is strongly associated with both major adverse cardiovascular events and survival [29]. In contrast, HD patients require ultrafiltration to their preset dry weight thrice weekly and may face intradialytic hypotension due to excessive interdialytic weight gain, which imposes strict fluid intake restrictions [30, 31]. Furthermore, left ventricular systolic dysfunction and left ventricular dilatation may also contribute to fluid overload, which was previously mentioned as more common in PD patients and associated with poor outcomes. There is concern that removing too much fluid may result in residual renal function loss in PD [32]. However, it is worth mentioning that with cautious ultrafiltration, or by using objective measurements like bioimpedance, PD patients can reach their desired dry weight and blood pressure without compromising residual kidney function [33, 34].
There are several limitations to acknowledge in our study. Firstly, the study was conducted at a single center, which may limit the generalizability of the findings to other patient populations. Additionally, the study was retrospective in nature, which may introduce biases and confounding factors. Secondly, the echocardiographic measurements were performed by different operators, which may have resulted in some degree of variability in the results. Thirdly, echocardiography sessions were not uniformly timed with hemodialysis treatments. Nonetheless, echocardiography was conducted within three months of enrolling the participants. In our hospital, establishing a new patient’s dry weight generally takes about one month, encompassing 10–13 dialysis sessions. This process, while specific to our institution, acknowledges the diversity in clinical protocols across various healthcare environments. Consequently, the participants were predominantly stable and not experiencing decompensated states, with most achieving their dry weight by the time of the echocardiography. This approach likely reduced the impact of fluid status on our findings, helping to mitigate potential bias. Fourthly, left atrial size, but not left atrial volume index, was used as an indicator of diastolic dysfunction. This is because the study population was recruited before the publication of the latest left ventricular diastolic dysfunction guideline and the limitation of the echocardiographic machine [15]. Lastly, although the study identified left ventricular systolic function, right ventricular systolic function, and left ventricular volume index as important predictors of major adverse cardiovascular events and mortality, further investigation is needed to understand the complex interplay between these three cardiac abnormalities as predictors of major adverse cardiovascular events and mortality.
In conclusion, this study provides insights into echocardiographic abnormalities and their association with adverse outcomes in kidney failure patients, which can help clinicians optimize the management of patients and improve their overall health. The present study describes a high prevalence of echocardiographic abnormalities in kidney failure patients, with left ventricular systolic function, right ventricular systolic function, and left ventricular volume index being the most important predictors of both major adverse cardiovascular events and mortality. Although left ventricular hypertrophy and left atrial enlargement were the most common abnormalities, they were not associated with adverse outcomes. The prognostic value of the baseline left ventricular volume index and left ventricular systolic dysfunction differed depending on the dialysis modality, being less critical in HD compared to PD.
Data availability
The data supporting the findings of this study are available within the article and its supplementary materials.
References
Collins AJ, Foley RN, Gilbertson DT, Chen SC (2011) United States Renal Data System public health surveillance of chronic kidney disease and end-stage renal disease. Kidney Int Suppl 2015(5):2–7. https://doi.org/10.1038/kisup.2015.2
Ronco C, Haapio M, House AA, Anavekar N, Bellomo R (2008) Cardiorenal syndrome. J Am Coll Cardiol 52:1527–1539. https://doi.org/10.1016/j.jacc.2008.07.051
Herzog CA, Mangrum JM, Passman R (2008) Sudden cardiac death and dialysis patients. Semin Dial 21:300–307. https://doi.org/10.1111/j.1525-139X.2008.00455.x
Lindner A, Charra B, Sherrard DJ, Scribner BH (1974) Accelerated atherosclerosis in prolonged maintenance hemodialysis. N Engl J Med 290:697–701. https://doi.org/10.1056/NEJM197403282901301
Schwarz U, Buzello M, Ritz E, Stein G, Raabe G, Wiest G et al (2000) Morphology of coronary atherosclerotic lesions in patients with end-stage renal failure. Nephrol Dial Transplant 15:218–223. https://doi.org/10.1093/ndt/15.2.218
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463. https://doi.org/10.1016/j.echo.2005.10.005
Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP et al (2009) Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr 22:1–23. https://doi.org/10.1016/j.echo.2008.11.029. (quiz 101–102)
Barbieri A, Bursi F, Mantovani F, Valenti C, Quaglia M, Berti E et al (2012) Left ventricular hypertrophy reclassification and death: application of the recommendation of the American Society of Echocardiography/European Association of Echocardiography. Eur Heart J Cardiovasc Imaging 13:109–117. https://doi.org/10.1093/ejechocard/jer176
Workgroup KD (2005) K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis 45:S1-153
Kan G, Visser CA, Lie KI, Durrer D (1984) Early two-dimensional echocardiographic measurement of left ventricular ejection fraction in acute myocardial infarction. Eur Heart J 5:210–217. https://doi.org/10.1093/oxfordjournals.eurheartj.a061638
Hickson LJ, Negrotto SM, Onuigbo M, Scott CG, Rule AD, Norby SM et al (2016) Echocardiography criteria for structural heart disease in patients with end-stage renal disease initiating hemodialysis. J Am Coll Cardiol 67:1173–1182. https://doi.org/10.1016/j.jacc.2015.12.052
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1–39):e14. https://doi.org/10.1016/j.echo.2014.10.003
Mitchell C, Rahko PS, Blauwet LA, Canaday B, Finstuen JA, Foster MC et al (2019) Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr 32:1–64. https://doi.org/10.1016/j.echo.2018.06.004
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K et al (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713. https://doi.org/10.1016/j.echo.2010.05.010
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29:277–314. https://doi.org/10.1016/j.echo.2016.01.011
Wu BS, Wei CH, Yang CY, Lin MH, Hsu CC, Hsu YJ et al (2022) Mortality rate of end-stage kidney disease patients in Taiwan. J Formos Med Assoc 121(Suppl 1):S12–S19. https://doi.org/10.1016/j.jfma.2021.12.015
Canaud B, Kooman JP, Selby NM, Taal MW, Francis S, Maierhofer A et al (2020) Dialysis-induced cardiovascular and multiorgan morbidity. Kidney Int Rep 5:1856–1869. https://doi.org/10.1016/j.ekir.2020.08.031
Wang AY, Wang M, Lam CW, Chan IH, Lui SF, Sanderson JE (2011) Heart failure in long-term peritoneal dialysis patients: a 4-year prospective analysis. Clin J Am Soc Nephrol 6:805–812. https://doi.org/10.2215/CJN.07130810
Konstam MA, Kiernan MS, Bernstein D, Bozkurt B, Jacob M, Kapur NK et al (2018) Evaluation and management of right-sided heart failure: a scientific statement from the American Heart Association. Circulation 137:e578–e622. https://doi.org/10.1161/CIR.0000000000000560
Pitoulis FG, Terracciano CM (2020) Heart plasticity in response to pressure- and volume-overload: a review of findings in compensated and decompensated phenotypes. Front Physiol 11:92. https://doi.org/10.3389/fphys.2020.00092
Foley RN, Curtis BM, Randell EW, Parfrey PS (2010) Left ventricular hypertrophy in new hemodialysis patients without symptomatic cardiac disease. Clin J Am Soc Nephrol 5:805–813. https://doi.org/10.2215/CJN.07761109
Stack AG, Saran R (2002) Clinical correlates and mortality impact of left ventricular hypertrophy among new ESRD patients in the United States. Am J Kidney Dis 40:1202–1210. https://doi.org/10.1053/ajkd.2002.36881
Niu CY, Yang SF, Ou SM, Wu CH, Huang PH, Hung CL et al (2022) Sacubitril/valsartan in patients with heart failure and concomitant end-stage kidney disease. J Am Heart Assoc 11:e026407. https://doi.org/10.1161/JAHA.122.026407
Genovesi S, Pogliani D, Faini A, Valsecchi MG, Riva A, Stefani F et al (2005) Prevalence of atrial fibrillation and associated factors in a population of long-term hemodialysis patients. Am J Kidney Dis 46:897–902. https://doi.org/10.1053/j.ajkd.2005.07.044
Winkelmayer WC, Patrick AR, Liu J, Brookhart MA, Setoguchi S (2011) The increasing prevalence of atrial fibrillation among hemodialysis patients. J Am Soc Nephrol 22:349–357. https://doi.org/10.1681/ASN.2010050459
Dewland TA, Olgin JE, Vittinghoff E, Marcus GM (2013) Incident atrial fibrillation among Asians, Hispanics, blacks, and whites. Circulation 128:2470–2477. https://doi.org/10.1161/CIRCULATIONAHA.113.002449
Kim YL, Biesen WV (2017) Fluid overload in peritoneal dialysis patients. Semin Nephrol 37:43–53. https://doi.org/10.1016/j.semnephrol.2016.10.006
Papakrivopoulou E, Booth J, Pinney J, Davenport A (2012) Comparison of volume status in asymptomatic haemodialysis and peritoneal dialysis outpatients. Nephron Extra 2:48–54. https://doi.org/10.1159/000337338
Ng JK, Kwan BC, Chow KM, Pang WF, Cheng PM, Leung CB et al (2018) Asymptomatic fluid overload predicts survival and cardiovascular event in incident Chinese peritoneal dialysis patients. PLoS ONE 13:e0202203. https://doi.org/10.1371/journal.pone.0202203
McCullough PA, Chan CT, Weinhandl ED, Burkart JM, Bakris GL (2016) Intensive hemodialysis, left ventricular hypertrophy, and cardiovascular disease. Am J Kidney Dis 68:S5–S14. https://doi.org/10.1053/j.ajkd.2016.05.025
Ohashi Y, Sakai K, Hase H, Joki N (2018) Dry weight targeting: the art and science of conventional hemodialysis. Semin Dial 31:551–556. https://doi.org/10.1111/sdi.12721
Nongnuch A, Assanatham M, Panorchan K, Davenport A (2015) Strategies for preserving residual renal function in peritoneal dialysis patients. Clin Kidney J 8:202–211. https://doi.org/10.1093/ckj/sfu140
Tian N, Yang X, Guo Q, Zhou Q, Yi C, Lin J et al (2020) Bioimpedance guided fluid management in peritoneal dialysis: a randomized controlled trial. Clin J Am Soc Nephrol 15:685–694. https://doi.org/10.2215/CJN.06480619
Li SY, Chuang CL, Lin CC, Tsai SH, Chen JY (2021) Peritoneal-membrane characteristics and hypervolemia management in peritoneal dialysis: a randomized control trial. Membranes (Basel). https://doi.org/10.3390/membranes11100768
Acknowledgements
We express our sincere gratitude to the diligent nurses of the dialysis center and the staff of the echocardiogram team at Taipei Veterans General Hospital for their invaluable efforts and contributions to this project.
Funding
Open Access funding enabled and organized by National Yang Ming Chiao Tung University. This work was supported by the Ministry of Science and Technology R.O.C MOST 110-2314-B-075 -028 -MY3.
Author information
Authors and Affiliations
Contributions
Y.A.H and S.Y.L designed the study and applied for the initial IRB approval. S.Y.L, C.Y.T and C.C.L participated in patient enrollment and data interpretation. C.H.T, and W.C.Y reviewed and interpreted the echocardiograms. C.H.T, Y.A.H and S.Y.L wrote the initial draft of the manuscript. W.C.Y and C.C. L reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no competing interests. Relationship with industry: There is no relationships with industry.
Ethical approval
This work received ethical approval from the Institutional Review Board of Taipei Veterans General Hospital. After review by the Human Research Protection Center, the implementation of the protocol is approved. (TPEVGH IRB No.: 2021-12-007C).
Informed consent to participate
Patient consent was waived due to it being a retrospective study across 10 years and de-identification before data analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tseng, CH., Hu, YA., Chen, YT. et al. Beyond prevalence: significance and differential impact of echocardiographic abnormalities in dialysis patients. J Nephrol (2024). https://doi.org/10.1007/s40620-024-01963-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40620-024-01963-2