Abstract
Background
Primary membranous nephropathy (PMN) is a rare pathological finding in paediatric patients. Data on PMN in children have been restricted to studies with small samples and fairly short follow-up periods. Therefore, we conducted this single-centre study to evaluate the long-term renal survival and related risk factors for PMN in children, and the clinical and histological characteristics were also described.
Method
Two hundred and seventeen children with PMN were enrolled from July 2008 to September 2017. Patients with follow-up durations < 12 months were excluded, except for patients who progressed to end-stage kidney disease (ESKD) or experienced a related death within 12 months. Long-term renal survival and related risk factors were analysed.
Result
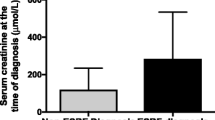
The sex ratio was 1.33:1 (male vs female), and the median age was 15.0 (14.0—17.0) years old. The most prominent clinical manifestation was nephrotic syndrome (130 59.9%), which was accompanied by various degrees of oedema (142 65.4%), hyperlipidaemia (151 69.6%), hypoalbuminemia (130 59.9%), and nephrotic proteinuria (135 62.2%). Hypertension occurred in 36.4% of children with PMN. After a median follow-up of 45.0 (23.5–74.0) months, 11 patients (5.1%) developed ESKD, and the cumulative kidney survival rates of ESKD at 5 and 10 years after renal biopsy were 95.3% and 67.8%, respectively. The cumulative kidney survival rates of the combined event of ESKD and/or 30% decline in estimated glomerular filtration rate (eGFR) at 5 and 10 years after renal biopsy were 92.6% and 59.5%, respectively. Cox multivariate regression and Kaplan–Meier analysis demonstrated that hypertension and proteinuria ≥ 50 mg/kg/day were associated with renal outcome.
Conclusion
In this study, the 5-year and 10-year cumulative renal survival rates of ESKD in children with PMN were reported for the first time as 95.3% and 67.8%, respectively. In addition, this is the first report to find that hypertension and proteinuria ≥ 50 mg/kg/day are associated with renal outcome in children with PMN.



Similar content being viewed by others
Code availability
Not applicable.
References
Zhou FD, Shen HY, Chen M et al (2011) The renal histopathological spectrum of patients with nephrotic syndrome: an analysis of 1523 patients in a single Chinese centre. Nephrol Dial Transplant 26(12):3993–3997. https://doi.org/10.1093/ndt/gfr166
Ng JK, Ma TK, Lai FM et al (2018) Causes of nephrotic syndrome and nephrotic-range proteinuria are different in adult Chinese patients: a single centre study over 33 years. Nephrology (Carlton) 23(6):565–572. https://doi.org/10.1111/nep.13061
Zhu P, Zhou FD, Wang SX et al (2015) Increasing frequency of idiopathic membranous nephropathy in primary glomerular disease: a 10-year renal biopsy study from a single Chinese nephrology centre. Nephrology (Carlton) 20(8):560–566. https://doi.org/10.1111/nep.12542
Couser WG (2017) Primary membranous nephropathy. Clin J Am Soc Nephrol 12(6):983–997. https://doi.org/10.2215/CJN.11761116
Maifata SM, Hod R, Zakaria F et al (2019) Primary membranous glomerulonephritis: the role of serum and urine biomarkers in patient management. Biomedicines. https://doi.org/10.3390/biomedicines7040086
Dionne JM (2017) Updated guideline may improve the recognition and diagnosis of hypertension in children and adolescents; review of the 2017 AAP blood pressure clinical practice guideline. Curr Hypertens Rep 19(10):84. https://doi.org/10.1007/s11906-017-0780-8
Radice A, Trezzi B, Maggiore U et al (2016) Clinical usefulness of autoantibodies to M-type phospholipase A2 receptor (PLA2R) for monitoring disease activity in idiopathic membranous nephropathy (IMN). Autoimmun Rev 15(2):146–154. https://doi.org/10.1016/j.autrev.2015.10.004
Bally S, Debiec H, Ponard D et al (2016) Phospholipase A2 receptor-related membranous nephropathy and mannan-binding lectin deficiency. J Am Soc Nephrol 27(12):3539–3544. https://doi.org/10.1681/ASN.2015101155
Ronco P, Debiec H (2015) Pathophysiological advances in membranous nephropathy: time for a shift in patient's care. Lancet 385(9981):1983–1992. https://doi.org/10.1016/S0140-6736(15)60731-0
Liu A, Wu H, Su Y et al (2015) Idiopathic membranous nephropathy in children in China. Fetal Pediatr Pathol 34(3):185–189. https://doi.org/10.3109/15513815.2015.1016589
Ayalon R, Beck LJ (2015) Membranous nephropathy: not just a disease for adults. Pediatr Nephrol 30(1):31–39. https://doi.org/10.1007/s00467-013-2717-z
Cattran DC, Brenchley PE (2017) Membranous nephropathy: integrating basic science into improved clinical management. Kidney Int 91(3):566–574. https://doi.org/10.1016/j.kint.2016.09.048
Chen A, Frank R, Vento S et al (2007) Idiopathic membranous nephropathy in pediatric patients: presentation, response to therapy, and long-term outcome. BMC Nephrol 8:11. https://doi.org/10.1186/1471-2369-8-11
Kumar V, Varma AK, Nada R et al (2017) Primary membranous nephropathy in adolescence: a prospective study. Nephrology (Carlton) 22(9):678–683. https://doi.org/10.1111/nep.12835
Wasserstein AG (1997) Membranous glomerulonephritis. J Am Soc Nephrol 8(4):664–674
Ponticelli C, Passerini P (2010) Can prognostic factors assist therapeutic decisions in idiopathic membranous nephropathy? J Nephrol 23(2):156–163
Kumar V, Ramachandran R, Kumar A et al (2015) Antibodies to m-type phospholipase A2 receptor in children with idiopathic membranous nephropathy. Nephrology (Carlton) 20(8):572–575. https://doi.org/10.1111/nep.12478
Zhang Q, Huang B, Liu X et al (2017) Ultrasensitive quantitation of anti-phospholipase A2 receptor antibody as a diagnostic and prognostic indicator of idiopathic membranous nephropathy. Sci Rep 7(1):12049. https://doi.org/10.1038/s41598-017-12014-1
Huh H, Lee H, Lee JP et al (2017) Factors affecting the long-term outcomes of idiopathic membranous nephropathy. BMC Nephrol 18(1):104. https://doi.org/10.1186/s12882-017-0525-6
Sprangers B, Bomback AS, Cohen SD et al (2012) Idiopathic membranous nephropathy: clinical and histologic prognostic features and treatment patterns over time at a tertiary referral center. Am J Nephrol 36(1):78–89. https://doi.org/10.1159/000339628
Xiaofan H, Jing X, Chenni G et al (2019) New risk score for predicting progression of membranous nephropathy. J Transl Med 17(1):41. https://doi.org/10.1186/s12967-019-1792-8
Kanigicherla DA, Short CD, Roberts SA et al (2016) Long-term outcomes of persistent disease and relapse in primary membranous nephropathy. Nephrol Dial Transplant 31(12):2108–2114. https://doi.org/10.1093/ndt/gfv435
Tsai SF, Wu MJ, Chen CH (2019) Low serum C3 level, high neutrophil-lymphocyte-ratio, and high platelet-lymphocyte-ratio all predicted poor long-term renal survivals in biopsy-confirmed idiopathic membranous nephropathy. Sci Rep 9(1):6209. https://doi.org/10.1038/s41598-019-42689-7
Zhang MF, Cui Z, Zhang YM et al (2018) Clinical and prognostic significance of glomerular C1q deposits in primary MN. Clin Chim Acta 485:152–157. https://doi.org/10.1016/j.cca.2018.06.050
Navaratnarajah A, Sambasivan K, Cook TH et al (2019) Predicting long-term renal and patient survival by clinicopathological features in elderly patients undergoing a renal biopsy in a UK cohort. Clin Kidney J 12(4):512–520. https://doi.org/10.1093/ckj/sfz006
Stangou MJ, Marinaki S, Papachristou E et al (2019) Histological grading in primary membranous nephropathy is essential for clinical management and predicts outcome of patients. Histopathology 75(5):660–671. https://doi.org/10.1111/his.13955
Acknowledgements
The authors acknowledge support from the Clinical Advanced Techniques, Primary Research & Development Plan of Jiangsu Province (BE2017719), and the Pediatric Medical Innovation Team of Jiangsu Province (CXTDA2017022).
Funding
This work was supported by the project of Clinical Advanced Techniques, Primary Research & Development Plan of Jiangsu Province (BE2017719), and the Pediatric Medical Innovation Team of Jiangsu Province (CXTDA2017022).
Author information
Authors and Affiliations
Contributions
R.W., M.Q.W. both are principal co-investigators, contributed equally to study design, data analysis, and draft the manuscript. Z.K.X., C.L.G., and Z.S. are co-investigators who reviewed the data for this study and participated in discussions around the observed outcomes. X.F., H.Y.W., and Y.C.P. are independent members who collected the data. All authors were involved in the writing of the manuscript and the decision to submit the manuscript for publication.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests;
Ethical statement
All data were obtained via electronic medical records and a database review and were de-identified (the patient's name was replaced with an identification code, and the patient's private information was deleted before the analysis) to protect patient privacy. This study was approved by the Institutional Ethics Committee.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, R., Wang, M., Xia, Z. et al. Long-term renal survival and related risk factors for primary membranous nephropathy in Chinese children: a retrospective analysis of 217 cases. J Nephrol 34, 589–596 (2021). https://doi.org/10.1007/s40620-020-00816-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-020-00816-y