Abstract
Purpose
Vitamin D deficiency has been associated with multiple chronic diseases, including metabolic disorders such as insulin resistance and type 2 diabetes (T2D). The aim of the study was to analyze the association between validated predicted serum vitamin D status and the risk of developing T2D in a large prospective cohort based on a Mediterranean population.
Methods
The SUN project is a prospective and dynamic Spanish cohort that gathers university graduates who have answered lifestyle questionnaires, including a validated Food Frequency Questionnaire. The association between predicted serum vitamin D and the risk of T2D was assessed through Cox regression models according to quartiles (Q) of predicted vitamin D at baseline. The models were adjusted for potential confounders and sensitivity analyses were performed to ensure the robustness of our findings.
Results
Our study included a total of 18,594 participants and after a total follow-up of 238,078 person-years (median follow-up of 13.5 years), 209 individuals were diagnosed with incident T2D. We found a significant inverse association between predicted levels of serum vitamin D and the risk of developing T2D, after adjusting for potential confounders and performing different sensitivity analyses (hazard ratio Q4 vs. Q1: 0.48, 95% CI 0.26–0.88; p for trend = 0.032).
Conclusion
The outcomes suggest that higher levels of vitamin D at baseline may be associated with a reduced risk of developing T2D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes (T2D) is the most common type of diabetes and a highly prevalent chronic disease, which leads to an increased morbidity affecting life quality and functional capacities of many patients, along with higher rates of mortality [1]. The last report published in 2021 by the International Diabetes Federation (IDF) stated that approximately 537 million adults between 20 and 79 years old had already been diagnosed with diabetes worldwide and 541 million adults were at high risk of developing type 2 diabetes [1, 2]. In addition, such reports have predicted that cases of diabetes are expected to rise to 643 million by 2030 and 783 million by 2045 [2]. Furthermore, the continuous growing trend in the number of cases has generated a significant increase in health care costs, which has turned T2D into a relevant public health issue [2].
Vitamin D deficiency has also become a worldwide health problem. In fact, published scientific evidence highlights that near 40% of Europeans and 24% of North Americans show deficient values of serum vitamin D, although data may vary depending on age or ethnicity in different regions [3,4,5,6]. Vitamin D is a fat-soluble vitamin, which is naturally found in different dietary sources (such as fatty fish or egg yolks), and it is also synthesized endogenously after sun exposure [7, 8]. Vitamin D has been involved in many different physiological processes. Apart from its well-known role in calcium and bone metabolism, it seems to be associated with the regulation of inflammatory processes as well as the modulation of different mechanisms such as cell growth, immune function, and glucose metabolism [9, 10]. In fact, there is current evidence that vitamin D deficiency plays a role in the development of metabolic disorders including insulin resistance and T2D [11]. Several observational studies have shown a possible association between vitamin D deficiency and diabetes onset as well as progression toward complications [12,13,14]. In fact, various mechanisms have been described such as the modulation of immune responses and depletion of systemic inflammation, the reduction of peripheral insulin resistance through vitamin D receptors located in muscles and liver or the increase or calcium influx into pancreatic beta cells, which influences insulin secretion, among others [15, 16]. However, it remains unclear the protective role of vitamin D supplementation in the prevention of T2D [17,18,19,20,21]. Two recent trials showed that the risk of a new onset of T2DM was lower in the supplemented group, although the differences were not statistically significant [17, 18]. The most important randomized trial (the D2d study) observed a 12% relative reduction in the risk of T2D [17], whereas The Diabetes Prevention with Active Vitamin D study found a 13% lower risk of T2D among adults with prediabetes after supplementation with eldecalcitol [18].
This study aims to give some light over the possible association between levels of predicted serum vitamin D and the risk of developing type 2 diabetes in a large Mediterranean cohort with a long follow-up period.
Materials and methods
Study population
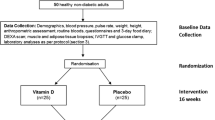
The SUN project (Seguimiento Universidad de Navarra) is a prospective, multipurpose, and dynamic cohort conducted in Spain that started to recruit participants in 1999 [22].
Information was collected from participants through validated questionnaires, which were mailed at baseline and every 2 years. They included information about socio-demographic, lifestyle and dietary variables, as well as the prevalence or incidence of different diseases at baseline and during the follow-up. All participants are university graduates and over the half are health professionals who live throughout Spain, which provides a wide range of different lifestyles and dietary patterns. Up to May 31, 2022, a total of 23,133 participants completed their baseline questionnaire. For the current analysis, the sample was selected according to the following exclusion criteria: 421 individuals with a previous diagnosis of diabetes at the time of the enrollment were excluded; we also excluded 232 participants who completed the baseline questionnaire after August 31, 2019 to ensure a minimum follow-up of 2 years and 9 months. We further excluded 2103 participants with energy intake outside the predefined limits by Willett (a daily energy intake below 500 kcal or above 3500 kcal for women and below 800 kcal or above 4000 kcal for men) [23] and also 1783 subjects who were lost to follow-up. Finally, a total of 18,594 participants and 209 incident cases of type 2 diabetes were included (Fig. 1). The overall long-term retention rate in the cohort was 91%. The institutional review committee of the University of Navarra approved the study. Voluntary completion of the first questionnaire was considered to imply informed consent.
Exposure assessment
Predicted vitamin D serum levels were forecasted through a previously validated predictive model obtained after multiple linear regression analysis [24]. The prediction model included the following variables: dietary intake of vitamin D; age and sex; body mass index (BMI), which was calculated from self-reported weight and height (kg/m2); skin reaction after sun exposure (mild or severe reaction); time spent on daily walks (minutes per day); and summer sun exposure (hours per day) (Supplementary Table 1). This last variable was estimated after performing a weighted average of the weekly sun exposure during summer. Dietary information was obtained from a validated semiquantitative 136-item Food Frequency Questionnaire (FFQ) [25,26,27]. In this way, values of vitamin D ingested from diet and vitamin supplements were included in the same variable and it was adjusted for total energy intake (kcal) using the residual method. Physical activity was also assessed through a validated questionnaire [28]. Each practice of physical activity was weighted using its proportional number of metabolic equivalents (METs) and time spent on each activity was also taken into account to obtain a global value of METs-h/week for each volunteer. The whole process of the abovementioned predictive model has been previously described [24].
Outcome assessment
Ascertainment of type 2 diabetes mellitus (T2D) in the SUN cohort has been well described before [29]. Prevalent cases of T2D were initially classified only as probable cases when the participant reported a confirmed medical diagnosis at baseline. Adjudication of incident cases of T2D were all those participants who were medically diagnosed of diabetes in one of the follow-up questionnaires but did not report the disease at baseline. In addition, these volunteers were asked to fill in an additional confirmation questionnaire and their medical records were also requested. Subsequently, an independent expert endocrinologist who was blinded to the exposure definitively confirmed the incident cases of T2D, based on all this information collected. The incident cases of T2D were adjudicated following all these steps and using the American Diabetes Association’s criteria [30]. These criteria include: fasting plasma glucose ≥ 126 mg/dL (7.0 mmol/L) or 2-h plasma glucose ≥ 200 mg/dL (11.1 mmol/L) during oral glucose tolerance test or glycated hemoglobin ≥ 6.5% or a random plasma glucose ≥ 200 mg/dL (11.1 mmol/L) in a patient with classic symptoms of hyperglycemia or hyperglycemic crisis [30].
Covariates assessment
The baseline questionnaire gathered information about socio-demographics (marital status, educational level), validated anthropometric measures [31], lifestyle habits (smoking status, physical activity or time spent watching television), and medical variables (prevalence of cancer, hypertension, hypertriglyceridemia and hypercholesterolemia, among others). Information about the total amount of energy intake (kcal/day) was also collected. Adherence to Mediterranean diet (MedDiet) was evaluated using the well-known score proposed by Trichopoulou et al. [32]. This score ranged from 0 to 9 points; where higher score implies higher adherence to the Mediterranean diet.
Statistical analysis
Description of baseline characteristics was performed, computing means and standard deviations for continuous variables and proportions for categorical variables, and comparison between quartiles of predicted serum vitamin D was conducted using ANOVA test for continuous variables and Chi-squared test for categorical variables. Afterward, p values were adjusted performing Bonferroni’s method. The association between quartiles of predicted serum vitamin D levels and the risk of developing T2D was assessed using Cox regression models, with the lowest quartile as the reference category. Hazard ratios (HR) and their 95% confidence intervals (95% CI) were estimated. Moreover, we calculated the continuous association of incident T2D for each 10 ng/mL increase of predicted serum levels of vitamin D.
A first model was adjusted for age and sex. A second model, included additionally, marital status (married/others), smoking status (current, former or never smoker), cumulative exposure to tobacco (smoking pack-years), weight change (yes/no), years of university education attained, TV hours/day, family history of T2D (yes/no), physical activity (MET-h/week), adherence to Mediterranean dietary pattern (low (0–3), moderate (4–6), high (7–9)), energy intake (kcal/day), sugar-sweetened beverage consumption (servings/day), snacking between meals (yes/no), following a special diet (yes/no), prevalent hypertension, prevalent cancer, prevalent hypercholesterolemia, prevalent hypertriglyceridemia. A third model was fitted additionally adjusting for obesity (≥ 30 kg/m2 yes/no). Missing values were imputed (simple imputation) using the Stata command impute, based on multivariable linear regression models for continuous variables and multivariable logistic or multinomial regression models for categorical variables. The imputed variables were time spent watching TV (18.0% of missing values), following a special diet (2.4%), skin reaction after sun exposure (1.6%), and summer sun exposure (20.7%). We performed an analysis to assess potential effect modification by sex, age (under or above 50 years old), and obesity (yes/no). We used the likelihood ratio test comparing the fully adjusted Cox regression model and the same model with the interaction cross product terms with quartiles of estimated vitamin D (3 d.f,) to estimate the p value for interaction. Several sensitivity analyses were conducted under different assumptions: excluding extreme values of total energy intake (< p1 and > p99), excluding participants with outliers’ values of predicted serum vitamin D (± 1.5 IQR). Additional analyses were performed excluding those participants who had prevalent cancer, hypertension, hypertriglyceridemia, and hypercholesterolemia to reduce the chance of reverse causality. We also conducted analyses including only participants with family history of T2D, overweight (BMI ≥ 25 kg/m2) or sedentary lifestyle, which was defined as physical activity below the median (MET-h/week < p50).
Restricted cubic splines with three knots, considering 10 (ng/mL) as the reference, were applied to the flexible model to graphically represent the dose–response association between type 2 diabetes and the predicted serum vitamin D level (as a continuous variables), as well as to evaluate non-linearity. All p values were two-tailed and statistical significance was set at the cut-off point of p < 0.05. All analyses were performed using STATA 15.0 (StataCorp, College Station, TX).
Results
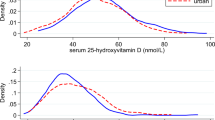
For the analysis, we included 18,594 participants, with a 60.5% of female participation; the mean age was 38.0 ± 12.2 years. Table 1 describes baseline characteristics of the sample according to quartiles of predicted serum vitamin D. Mean predicted serum vitamin D was 19.9 ± 2.32 ng/mL. Participants in the highest quartile of predicted vitamin D tended to be younger, mostly not married and they showed lower prevalence of cardiovascular risk factors as well as cancer. They also tended to smoke less, to show lower body mass index, to be more physically active (3.7 times more sportive as compared to those in the first quartile), and to have greater summer sunlight exposure. In terms of nutrition, they also showed greater daily intake of vitamin D and slightly higher adherence to Mediterranean diet compared to the first quartile. Other characteristics such as time spent watching TV or sleeping, as well as the intake of the different nutrients (carbohydrates, proteins and fat) and alcohol were very similar across quartiles. After a total of 238,078 person-years with a median follow-up of 13.5 years, 209 individuals were diagnosed with incident type 2 diabetes. Most of the T2D cases (n = 118) were found in the first quartile of predicted serum vitamin D, showing an incident rate of 2 × 10–3 vs. 0.3 × 10–3 in the last quartile. When comparing quartiles of predicted serum vitamin D, considering the lowest quartile as the reference, we found an inverse significant association between predicted levels of serum vitamin D and the risk of developing diabetes, after adjusting for potential cofounders (Table 2). Compared to the reference category, the hazard ratios shown were HRQ2vsQ1 of 0.65 (95% CI 0.44–0.95), HRQ3vsQ1 of 0.71 (95% CI 0.45–1.10), HRQ4vsQ1 of 0.48 (95% CI 0.26–0.88) p for trend = 0.032. In addition, each increase of 10 ng/mL (25 nmol/L) in 25(OH)D concentration was associated with a HR of 0.31 (95% CI 0.14–0.68) Fig. 2 represents the dose–response relationship between the predicted serum levels of vitamin D and the risk of developing T2D. The graph shows that serum vitamin D levels under 10 ng/mL (25 nmol/L) seemed to be significantly associated with an increased risk of developing T2D up to 40%. However, as serum vitamin D increases, the curve suggested a statistically significant protective effect.
Restricted cubic splines dose–response pattern: adjusted hazard ratios (HR)* and 95% confidence intervals (CI) for the development of T2D according to predicted serum vitamin D. *Adjusted for sex, age, marital status, smoking status (current, former or never smoker), smoking pack-years, weight change, years of university, TV hours/day, family history of T2D, physical activity (MET-h/week), Trichopoulou’s 9-point score/Mediterranean dietary pattern, energy intake (kcal/day), sugar-sweetened beverage consumption (servings/day), snacking, following a special diet, prevalent hypertension, prevalent cancer, prevalent hypercholesterolemia, prevalent hypertriglyceridemia and obesity (>= 30 kg/m2 yes, no)
We carried out several sensitivity analyses to determine the robustness of our findings. After excluding patients with prevalent cancer, hypertension, hypertriglyceridemia, extreme daily energy intake and the outliers of predicted vitamin D and including only participants with sedentary lifestyle and overweight, the results did not suffer any substantial change compared to the main analyses (see Table 3). The inverse association between predicted 25(OH)D (highest vs. lowest quartile) and the risk of incident T2D was stronger after excluding participants diagnosed with hypertension at baseline (HRQ4vsQ1 0.28; 95% CI 0.11–0.72) and including only individuals with sedentary habits (HRQ4vsQ1 0.28; 95% CI 0.09–0.93) and overweight (HRQ4vsQ1 0.19; 95% CI 0.07–0.56). However, when we excluded participants with prevalent hypercholesterolemia and took into account only individuals with family history of T2D, we did not find any statistically significant association (HRQ4vsQ1 0.50; 95% CI 0.22–1.17 and HRQ4vsQ1 0.34; 95% CI 0.10–1.10, respectively).
The stratified analysis for the effect modification (Table 4) showed a stronger association between predicted serum vitamin D levels and T2D in participants younger than 50 years, in men and in non-obese subjects when comparing the highest vs. the lowest quartile. However, we found no evidence of significant interaction between age (p for interaction 0.120), sex (p for interaction 0.961) or obesity (p for interaction 0.806).
Discussion
In this prospective cohort of Spanish adults, the risk of developing T2D decreases in the highest quartiles of predicted serum vitamin D levels compared to the lowest quartile, independently of obesity and other potential confounders. After adjusting for obesity, the association was slightly attenuated remaining statistically significant, which may act as an intermediate factor in the risk of new-onset T2D. We did not adjust for BMI as a continuous variable because we assumed that it could be an intermediate link in the causal chain. Results showed a 52% reduction in the risk of developing T2D in the top vs. the bottom quartile of predicted vitamin D (HR 0.48; 95% CI 0.26–0.88, p = 0.032). Moreover, a relatively 69% lower incidence rate of type 2 diabetes after each increase of 10 ng/mL was observed. Our results are in agreement with previous large observational studies [12, 13]. Some meta-analyses based on observational studies mainly conducted in Nordic (Denmark, Norway and Sweden) or Anglo-Saxon countries have also reported an inverse association between directly measured serum 25(OH)D levels and the risk of incident diabetes [11,12,13,14, 33]. Afzal et al. conducted a meta-analysis of 16 studies and showed a 50% higher risk for incident diabetes in the lowest category compared to the highest one (OR 1.5; 95% CI 1.33–1.70) [12]. Another study also reported an increased risk in incident T2D of 22% after each decrease of 10 ng/mL (25 nmol/L) in serum 25(OH)D [34]. Song et al. included 21 studies and estimated a reduction of 4% in the risk of diabetes after each 10 nmol/L increment in serum 25(OH)D levels (p for linear trend = 0.0001), and when comparing the highest vs. the lowest category of 25(OH)D levels, they found a 38% risk reduction in T2D development (RR 0.62; 95% CI 0.54–0.70) [13]. However, the association between the two variables was also slightly decreased after adjustment for BMI [13]. In the same line, Rafiq et al. described an inverse correlation between levels of vitamin D and insulin resistance, stronger in the diabetic sample (r = −0.26; 95% CI −0.39 to −0.11, p = 0.001), independent of age and sex but enhanced after BMI’s increase [14]. These findings highlight obesity as part of the causal chain in the risk of new-onset T2D. In fact, the relationship between vitamin D and adiposity may be complex and bidirectional as obese patients tend to show an increased storage of 25(OH)D in adipose tissue and less sunlight exposure due to a reduced mobility, which contribute to low circulating 25(OH)D levels [13]. When we explored the non-linear association between predicted serum 25(OH)D and T2D, our results showed that values above 12 ng/mL (30 nmol/L) seemed to have a protective effect over the risk of developing T2D. This association remained statistically significant up to 30 ng/mL (75 nmol/L). It remains unclear what levels of 25(OH)D are necessary to influence glucose and insulin homeostasis, and therefore the risk of incident diabetes. Song et al. proposed that reaching levels of serum 25(OH)D of at least 50 nmol/L contributed to reduce the risk of T2D [13]. Moreover, Avila-Rubio et al. conducted their research in women with postmenopausal osteoporosis and found that levels of 25(OH)D above 45 ng/mL were necessary to balance glucose metabolism [35]. In this line, another research including 903 non-diabetic participants established the threshold of serum vitamin D at 30 ng/mL to reduce the incident rate of T2D [36]. There are different hypothesis that try to explain the mechanisms that lie beneath the association between vitamin-D-deficient status and a higher risk of diabetes. A large meta-analysis based on published small trials from 1980 to 2019 showed that sufficient levels of serum vitamin D diminish the risk of developing cellular pathological processes related to insulin resistance [15]. Such processes include the maintenance of low concentration of radicals, a low expression of pro-inflammatory cytokines but a higher production of anti-inflammatory ones [14, 15, 37]. Vitamin D is also involved in epigenetic processes affecting pancreatic β-cells and other insulin-sensitive peripheral tissues [15, 38]. Furthermore, vitamin has a modulation effect on insulin synthesis and secretion, given the presence of vitamin D receptors, 1α-hydroxylase, and vitamin D-binding protein in pancreatic islet cells [14, 33, 39]. Vitamin D has additional receptors in adipocytes, muscle, and hepatocytes reducing insulin resistance by enhancing insulin receptor expression and insulin responsiveness for glucose transport, and regulating calcium metabolism [14, 33, 37, 39, 40]. In this line, cholecalciferol (the active form of vitamin D) has the ability to increase calcium influx across β-cells’ membrane into their intracellular space, influencing insulin secretion [14, 33, 37,38,39,40].
The potential role of vitamin D supplementation in diabetes prevention has been also studied; however, inconclusive outcomes have been obtained [17, 19, 20, 33, 41]. The most important randomized trial (the D2d study) included 2,423 obese participants with prediabetes [17]. After 2.5 years of median follow-up, a new diagnosis of T2D was observed in 293 participants allocated to 4000 IU/d of vitamin D and in 323 participants of the placebo group, with hazard ratio of 0.88 (95% CI 0.75–1.04; p = 0.12). In subgroup analysis, participants showing insufficient levels of vitamin D seemed to have a lower risk of developing T2D after supplementation. The initial levels of vitamin D were 28 ng/ml and the trial’s duration probably was not very long [17]. Despite the lack of conventional statistical significance, this trial observed a 12% relative reduction in risk [17]. Given this finding, it can be speculated that a longer duration and a larger sample size would probably have found a greater benefit. In fact, this interpretation was favored by a secondary per protocol analysis, which found that among participants adherent to the trial protocol, vitamin D lowered the risk of developing T2D at the end of the study [42]. Another meta-analysis reported a 27% reduction in the risk of progression from prediabetes status to diabetes after supplementation in non-obese subjects (RR 0.73; 95% CI 0.57–0.92) [33]. In addition, Li X et al. evinced a partial reduction of insulin resistance compared with placebo in patients diagnosed with T2D [20]. However, this outcome was shown after large doses and short-term supplementation in vitamin-D-deficient non-obese participants from Middle East Asia [20]. In the same line, another randomized controlled clinical trial conducted among pre-diabetic Iranian individuals found a slightly but statistically significant improvement on insulin sensitivity and a lower risk of progression toward diabetes in the vitamin D group compared to placebo, after high dose supplementation [43]. Published literature highlights the significant association between serum vitamin D deficiency and diabetic peripheral and cardiac neuropathy, erectile dysfunction and diabetic retinopathy, as it has been suggested that vitamin D has a protective effect over the optic nerves [14, 37, 44, 45]. In addition, low serum 25(OH)D status has been related to an increased risk of developing diabetic nephropathy, after finding that vitamin D analogs strengthen the protective effects of the renin–angiotensin–aldosterone system inhibitors over the renal function through suppression of renin expression [37, 44].
In addition, other authors have studied the association between predicted serum vitamin D and other clinical outcomes, such as different types of tumors (breast or colorectal cancers) [46, 47] or the risk of fractures [48], among others.
Our study has some limitations. The use of self-reported, validated FFQ to evaluate nutritional intake provides subjective details and may fall into an information bias. This is particularly important when reporting vitamin D intake, since the data collected reflect a consumption below the recommended limits (15 mcg/day) [7]. In addition, our serum vitamin D predictive model is a subjective tool, which may be more useful in the epidemiological and research fields, rather than the daily clinical setting, as it may not be suitable for particular groups such as pregnant women, children or patients with severe kidney disease, in which specific prediction models should be used to reach adequate outcomes. In this line, considering that serum vitamin D concentrations show diurnal [49] and annual fluctuations (higher levels in summer and lower during winter), weakly but significantly correlate with other hormones such as testosterone and cortisol [50], assessing predicted serum levels of vitamin D at the same hour of the day and during the same season in a sufficiently large sample of participants with and without T2D, could strengthen the significance of our findings. Moreover, the sample is not representative of the general population as it includes mostly young adults with a high educational level. Therefore, the extrapolation of our results to general population should not be based on representativeness of the study sample. Proper generalization should be grounded on the knowledge of specific conditions and the clear understanding of involved biological mechanisms [51]. However, this feature of our design also has the advantage of increasing the internal validity of our results due to the high educational level and homogeneity of the participants, which reduces potential confounding related to educational and socioeconomic status. The strengths of the current study include its prospective design and dynamic participation. To our knowledge, this is one of the few studies to assess the association between estimated circulating vitamin D and incidental T2D in Spanish population and the first one based on a validated predictive model. The SUN project also includes a large sample with a considerable long-term follow-up and a good retention rate, which are relevant to ensure an adequate temporal sequence between exposure and outcome. Self-reported cases of incident T2D were confirmed by an expert endocrinologist who was blinded to the exposure, which provides data reliability and a high specificity. What is more, we adjusted the models for a wide range of potential confounders and several sensitivity analyses were performed to guarantee the robustness of our outcomes and minimize the likelihood of residual confounding.
Conclusion
Our study based on validated predicted serum 25(OH)D in a Mediterranean cohort conclude that vitamin D has a role in the modulation of diabetes risk, suggesting that higher levels of predicted vitamin D at baseline may have a protective effect in the prevention of incident T2D. However, the baseline 25(OH)D threshold considered to be preventive from developing type 2 diabetes remains unclear.
Data availability
The data from the SUN project that support our findings are available upon request to the Department of Preventive Medicine and Public Health, School of Medicine, University of Navarra (Spain) at sun@unav.es.
Abbreviations
- T2D:
-
Type 2 diabetes
- SUN project:
-
Seguimiento Universidad de Navarra
- BMI:
-
Body mass index
- FFQ:
-
Food Frequency Questionnaire
- MET:
-
Metabolic equivalent of task
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- d.f.:
-
Degrees of freedom
- IQR:
-
Interquartile range
References
Stumvoll M, Goldstein BJ, van Haeften T (2005) Type 2 diabetes: principles of pathogenesis and therapy. Lancet 365:1333–1346
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB et al (2022) IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract 183:109–119
Cashman KD, Dowling KG, Škrabáková Z, Gonzalez-Gross M, Valtueña J, De Henauw S et al (2016) Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr 103(4):1033–1044
Schleicher RL, Sternberg MR, Looker AC, Yetley EA, Lacher DA, Sempos CT et al (2016) National estimates of serum total 25-hydroxyvitamin D and metabolite concentrations measured by liquid chromatography-tandem mass spectrometry in the US population during 2007–2010. J Nutr 146(5):1051–1061
Amrein K, Scherkl M, Hoffmann M, Neuwersch-Sommeregger S, Köstenberger M, Tmava Berisha A et al (2020) Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr 74:1498–1513
Holick MF (2017) The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord 18(2):153–165
Institute of Medicine (US) (2011) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. In: Ross AC, Taylor CL, Yaktine AL, et al. (eds.) Dietary Reference Intakes for Calcium and Vitamin D. Washington (DC), National Academies Press (US). https://doi.org/10.17226/13050https://www.ncbi.nlm.nih.gov/books/NBK56070/
Roseland JM, Phillips KM, Patterson KY, Pehrsson PR, Taylor CL (2018) Vitamin D in Foods: An Evolution of Knowledge. Vitamin D Health, Disease and Therapeutics, vol 2, 4th edn. Elsevier, Amsterdam The Netherlands, pp 41–78
Charoenngam N, Holick MF (2020) Immunologic effects of vitamin d on human health and disease. Nutrients 12(7):1–28
Giovinazzo S, Alibrandi A, Campennì A et al (2017) Correlation of cardio-metabolic parameters with vitamin D status in healthy premenopausal women. J Endocrinol Invest 40:1337–1343
Pittas AG, Jorde R, Kawahara T, Dawson-Hughes B (2020) Vitamin D supplementation for prevention of type 2 diabetes mellitus: to D or Not to D? J Clin Endocrinol Metab 105(12):3721–3733
Afzal S, Bojesen SE, Nordestgaard BG (2013) Low 25-hydroxyvitamin D and risk of type 2 diabetes: a prospective cohort study and metaanalysis. Clin Chem 59(2):381–391
Song Y, Wang L, Pittas AG, Del Gobbo LC, Zhang C, Manson JE et al (2013) Blood 25-hydroxyvitamin D levels and incident type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care 36(5):1422–1428
Rafiq S, Jeppesen PB (2021) Insulin resistance is inversely associated with the status of vitamin d in both diabetic and non-diabetic populations. Nutrients. https://doi.org/10.3390/nu13061742
Szymczak-Pajor I, Śliwińska A (2019) Analysis of association between vitamin D deficiency and insulin resistance. Nutrients 11(4):794
Muñoz-Garach A, García-Fontana B, Muñoz-Torres M (2019) Vitamin D status, calcium intake and risk of developing type 2 diabetes: an unresolved issue. Nutrients 11(3):1–17
Pittas AG, Dawson-Hughes B, Sheehan P, Ware JH, Knowler WC, Aroda VR et al (2019) Vitamin D Supplementation and prevention of Type 2 Diabetes. N Engl J Med 381(6):520–530
Kawahara T, Suzuki G, Mizuno S, Inazu T, Kasagi F, Kawahara C et al (2022) Effect of active vitamin D treatment on development of type 2 diabetes: DPVD randomised controlled trial in Japanese population. BMJ 377:e066222
Jorde R, Sollid ST, Svartberg J, Schirmer H, Joakimsen RM, Njølstad I et al (2016) Vitamin D 20 000 IU per week for five years does not prevent progression from prediabetes to diabetes. J Clin Endocrinol Metab 101(4):1647–1655
Li X, Liu Y, Zheng Y, Wang P, Zhang Y (2018) The effect of vitamin D supplementation on glycemic control in type 2 diabetes patients: a systematic review and meta-analysis. Nutrients 10(3):375
Saponaro F, Marcocci C, Zucchi R (2019) Vitamin D status and cardiovascular outcome. J Endocrinol Invest 42:1285–1290
Carlos S, De La Fuente-Arrillaga C, Bes-Rastrollo M, Razquin C, Rico-Campà A, Martínez-González MA et al (2018) Mediterranean diet and health outcomes in the SUN cohort. Nutrients 10(4):1–24
Willett W, Stampfer MJ (1986) Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 24(1):17–27
Valer-Martinez A, Sayon-Orea C, Alfredo J, Hernandez M, De La Fuente-Arrillaga C, Rojas JP et al (2023) Forecasting levels of serum 25-hydroxyvitamin D based on dietary intake, lifestyle and personal determinants in a sample of Southern Europeans. Br J Nutr. https://doi.org/10.1017/S0007114523000946
Martin-Moreno JM, Boyle P, Gorgojo L, Maisonneuve P, Fernandez-Rodriguez JC, Salvini S et al (1993) Development and validation of a food frequency questionnaire in Spain. Int J Epidemiol 22(3):512–519
De La Fuente-Arrillaga C, Vazquez Ruiz Z, Bes-Rastrollo M, Sampson L, Martinez-González MA (2010) Reproducibility of an FFQ validated in Spain. Public Health Nutr 13(9):1364–1372
Fernández-Ballart JD, Lluís Piñol J, Zazpe I, Corella D, Carrasco P, Toledo E et al (2010) Relative validity of a semi-quantitative food-frequency questionnaire in an elderly mediterranean population of Spain. Br J Nutr 103(12):1808–1816
Martínez-González MA, López-Fontana C, Varo JJ, Sánchez-Villegas A, Martinez JA (2005) Validation of the Spanish version of the physical activity questionnaire used in the nurses’ health study and the health professionals’ follow-up study. Public Health Nutr 8(7):920–927
Martínez-González MA, De La Fuente-Arrillaga C, Nunez-Cordoba JM, Basterra-Gortari FJ, Beunza JJ, Vazquez Z et al (2008) Adherence to mediterranean diet and risk of developing diabetes: prospective cohort study. BMJ 336(7657):1348–1351
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D et al (2023) Classification and diagnosis of diabetes: standards of care in diabetes—2023. Diabetes Care 46:S19–S40
Bes-Rastrollo M, Valdivieso-Pérez J, Sánchez-Villegas A, Alonso A, Martínez-González MA (2005) Validación del peso e índice de masa corporal auto-declarados de los participantes de una cohorte de graduados universitarios [validation of self-reported weight and body mass index of participants from a cohort of college graduates]. Rev Esp Obes 3:352–358
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D (2003) Adherence to a mediterranean diet and survival in a Greek population. N Engl J Med 26:2599–2608
Zhang Y, Tan H, Tang J, Li J, Chong W, Hai Y et al (2020) Effects of vitamin D supplementation on prevention of type 2 diabetes in patients with prediabetes: a systematic review and meta-analysis. Diabetes Care 43(7):1650–1658
Ye Z, Sharp SJ, Burgess S, Scott RA, Imamura F, Langenberg C et al (2015) Association between circulating 25-hydroxyvitamin D and incident type 2 diabetes: a mendelian randomisation study. Lancet Diabetes Endocrinol 3(1):35–42
Ávila-Rubio V, García-Fontana B, Novo-Rodríguez C, Cantero-Hinojosa J, Reyes-García R, Muñoz-Torres M (2018) Higher levels of serum 25-hydroxyvitamin D are related to improved glucose homeostasis in women with postmenopausal osteoporosis. J Womens Health 27(8):1007–1015
Park SK, Garland CF, Gorham ED, BuDoff L, Barrett-Connor E (2018) Plasma 25-hydroxyvitamin D concentration and risk of type 2 diabetes and pre-diabetes: 12-year cohort study. PLoS ONE 13(4):1–17
Issa CM (2017) Vitamin D and type 2 diabetes mellitus. Adv Exp Med Biol 996:193–205
Vondra K, Hampl R (2021) Vitamin D and new insights into pathophysiology of type 2 diabetes. Horm Mol Biol Clin Investig 42(2):203–208
Mitri J, Pittas AG (2014) Vitamin D and diabetes. Endocrinol Metab Clin North Am 43(1):205–232
Maddaloni E, Cavallari I, Napoli N, Conte C (2018) Vitamin D and diabetes mellitus. Front Horm Res 50:161–176
Pittas AG, Kawahara T, Jorde R, Dawson-Hughes B, Vickery EM, Angellotti E et al (2023) Vitamin D and risk for type 2 diabetes in people with prediabetes. Ann Intern Med 176(3):355–364
Hsia DS, Nelson J, Vickery EM, Rasouli N, LeBlanc ES, Kim S et al (2023) Effect of vitamin D on regression to normal glucose regulation and individual glycemic measures: a secondary analysis among participants adherent to the trial protocol in the randomized clinical trial vitamin D and type 2 diabetes (D2d) study. Diabetes Res Clin Pract 202:110792
Niroomand M, Fotouhi A, Irannejad N, Hosseinpanah F (2019) Does high-dose vitamin D supplementation impact insulin resistance and risk of development of diabetes in patients with pre-diabetes? A double-blind randomized clinical trial. Diabetes Res Clin Pract 148(2):1–9
Sacerdote A, Dave P, Lokshin V, Bahtiyar G (2019) Type 2 Diabetes Mellitus, insulin resistance, and vitamin d. Curr Diab Rep. https://doi.org/10.1007/s11892-019-1201-y
Ahmed LHM, Butler AE, Dargham SR, Latif A, Robay A, Chidiac OM et al (2020) Association of vitamin D2 and D3 with type 2 diabetes complications. BMC Endocr Disord 20(1):65
Palmer JR, Gerlovin H, Bethea TN, Bertrand KA, Holick MF, Ruiz-Narvaez EN et al (2016) Predicted 25-hydroxyvitamin D in relation to incidence of breast cancer in a large cohort of African American women. Breast Cancer Res 18(1):86
Fuchs MA, Yuan C, Sato K, Niedzwiecki D, Ye X, Saltz LB et al (2017) Predicted vitamin D status and colon cancer recurrence and mortality in CALGB 89803 (Alliance). Ann Oncol 28(6):1359–1367
Petersen SB, Strøm M, Maslova E, Granström C, Vestergaard P, Mølgaard C et al (2015) Predicted vitamin D status during pregnancy in relation to offspring forearm fractures in childhood: a study from the Danish National Birth Cohort. Br J Nutr 114(11):1900–1908
Jones KS, Redmond J, Fulford AJ, Jarjou L, Zhou B, Prentice A et al (2017) Diurnal rhythms of vitamin D binding protein and total and free vitamin D metabolites. J Steroid Biochem Mol Biol 172:130–135
Lombardi G, Vitale JA, Logoluso S, Logoluso G, Cocco N, Cocco G et al (2017) Circannual rhythm of plasmatic vitamin D levels and the association with markers of psychophysical stress in a cohort of Italian professional soccer players. Chronobiol Int 34(4):471–479
Rothman KJ, Gallacher JEJ, Hatch EE (2013) Why representativeness should be avoided. Int J Epidemiol 42(4):1012–1021
Acknowledgements
We thank other members of the SUN Group: Alonso A, Álvarez-Álvarez I, Balaguer A, Barbagallo M, Barrientos I, Barbería-Latasa M, Barrio-López MT, Battezzati A, Bazal P, Benito S, Bertoli S, Beulen Y, Beunza JJ, Buil-Cosiales P, Canales M, Carlos S, Carmona L, Cervantes S, Cristobo C, de Irala J, de la Fuente-Arrillaga C, de la O V, de la Rosa PA, Delgado-Rodríguez M, Díaz-Gutiérrez J, Díez Espino J, Domínguez L, Donat-Vargas C, Donazar M, Eguaras S, Fernández-Montero A, Fresán U, Galbete C, García-Arellano A, García López M, Gutiérrez Bedmar M, Gomes-Domingos AL, Gómez-Donoso C, Gómez-Gracia E, Goñi E, Goñi L, Guillén F, Henríquez P, Hernández A, Hershey MS, Hidalgo-Santamaría M, Hu E, Lahortiga F, Leone A, Llorca J, López del Burgo C, Marí A, Marques I, Martí A, Martín Calvo N, Martín-Moreno JM, Martínez-Lapiscina EH, Mendonça R, Menéndez C, Molendijk M, Molero P, Murphy K, Muñoz M, NúñezCórdoba JM, Pajares R, Papadaki A, Parletta N, Pérez de Ciriza P, Pérez Cornago A, Pérez de Rojas J, Pimenta AM, Pons J, Ramallal R, Razquin C, Rico-Campà A, Ruano C, Ruiz L, Ruiz-Canela M, Ruiz Zambrana A, Salgado E, San Julián B, Sánchez D, Sánchez-Tainta A, Sánchez- Villegas A, Santiago S, Schlatter J, Serrano-Martinez M, Toledo J, Tortosa A, Valencia F, Vázquez Z, Zarnowiecki D, Zazpe I. We especially thank all participants in the SUN cohort for their long-standing and enthusiastic collaboration and our advisors from Harvard TH Chan School of Public Health Walter Willett, Alberto Ascherio, Frank B. Hu and Meir J. Stampfer who helped to design the SUN project.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. The SUN project has received funding from the Spanish Government—Instituto de Salud Carlos III, the European Regional Development Fund (FEDER) (RD 06/0045, CIBER-OBN, Grants PI10/02658, PI10/02293, PI13/00615, PI14/01668, PI14/01798, PI14/01764, PI17/01795, PI20/00564, PI23/01332, and G03/140), the Navarra Regional Government (27/2011, 45/2011, 122/2014), the National Plan on Drugs (2020/021), and the University of Navarra.
Author information
Authors and Affiliations
Contributions
Ana Valer-Martinez: conceptualization, data curation, formal analysis, writing—original draft preparation; Carmen Sayon-Orea: conceptualization, data curation, formal analysis, supervision, writing—reviewing and editing; Alfredo Martinez: supervision, writing—reviewing and editing; Javier Basterra-Gortari: data curation, writing—reviewing and editing; Miguel Angel Martinez-Gonzalez: conceptualization, project administration, writing—reviewing and editing; Maira Bes-Rastrollo: conceptualization, project administration, formal analysis, supervision, validation, writing—reviewing and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest. The funders had no role in the design of the study, collection, analysis and interpretation of the data; they did not intervene either in the writing process nor the decision to publish the outcomes.
Research involving human participants and/or animals
The present study was approved by the Research Ethics Committee of the University of Navarra and complies with the guidelines for studies involving human participation. The SUN cohort is registered at https://clinicaltrials.gov/ with number of registry NCT02669602.
Institutional review board
The present study was conducted according the Declaration of Helsinki’s guidelines and approved by the Institutional Review Board of the University of Navarra.
Informed consent
All participants gave informed consent through voluntary fulfillment of the baseline questionnaire.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Valer-Martinez, A., Sayon-Orea, C., Martinez, J.A. et al. Vitamin D and risk of developing type 2 diabetes in the SUN project: a prospective cohort study. J Endocrinol Invest (2024). https://doi.org/10.1007/s40618-024-02324-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40618-024-02324-3