Abstract
Aims
Opportunities and needs for starting insulin therapy in Type 2 diabetes (T2D) have changed overtime. We evaluated clinical characteristics of T2D subjects undergoing the first insulin prescription during a 15-year-observation period in the large cohort of the AMD Annals Initiative in Italy.
Methods
Data on clinical and laboratory variables, complications and concomitant therapies and the effects on glucose control after 12 months were evaluated in T2D patients starting basal insulin as add-on to oral/non-insulin injectable agents, and in those starting fast-acting in add-on to basal insulin therapy in three 5-year periods (2005–2019).
Results
We evaluated data from 171.688 T2D subjects who intensified therapy with basal insulin and 137.225 T2D patients who started fast-acting insulin. Overall, intensification with insulin occurred progressively earlier over time in subjects with shorter disease duration. Moreover, the percentage of subjects with HbA1c levels > 8% at the time of basal insulin initiation progressively decreased. The same trend was observed for fast-acting formulations. Clinical characteristics of subjects starting insulin did not change in the three study-periods, although all major risk factors improved overtime. After 12 months from the starting of basal or fast-acting insulin therapy, mean HbA1c levels decreased in all the three investigated time-periods, although mean HbA1c levels remained above the recommended target.
Conclusions
In this large cohort of T2D subjects, a progressively earlier start of insulin treatment was observed during a long observation period, suggesting a more proactive prescriptive approach. However, after 12 months from insulin prescription, in many patients, HbA1c levels were still out-of-target.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of type 2 diabetes (T2D) is rising in many places in the world, including Italy, where it increased from 4.1 to 5.9% in the latest 20 years [1, 2]. This figure places an enormous burden on healthcare systems, payers, and providers as well as at individual and social level.
To contain this dangerous wave, national and international guidelines are regularly updated to include better therapeutic options to cope with the evolving evidence, with the major aim of preventing T2D chronic complications while maintaining an adequate quality of life [3].
Metformin is recommended as the first-line pharmacological treatment, while innovative drugs are indicated for cardio-renal protection [3,4,5]. Injectable therapies including insulin are well-established agents for T2D, although the indication on the appropriate timing for starting insulin treatment in the therapeutic algorithm varied overtime [4,5,6]. Moreover, the advantages and the cost-benefits of insulin analogs and their combination with new glucose-lowering drugs are still a matter of debate [7].
In spite of the availability of new, highly effective treatments for T2D care, there is still a large gap between the guidelines recommendations and the outcomes achieved in clinical practice. Thus, HbA1c levels are higher than those recommended in many T2D patients: in 2022, in Italy about 40% of all T2DM subjects in care at diabetes clinics had HbA1c levels > 7%, and about 20% of them had HbA1c levels > 8% [8] and this is commonly observed also in other cohorts [9,10,11,12].
Reasons behind the lack of glucose control achievement in about half of T2D patients worldwide is a complex issue involving several aspects. The first of them is related to the progressive nature of the disease, characterized by a continuous decline of beta-cell function [13, 14]. Consequently, insulin supplementation is often needed to attain good glucose control in T2D [15].
Notably, a substantial proportion of patients with suboptimal control often experience delays in treatment intensification, a phenomenon that has been termed clinical inertia, with profound negative impact on the onset and the progression of both micro- and macrovascular complications [16, 17].
It has been calculated that a 1-year delay in intensification of glucose-lowering treatment is associated with a 62% increased risk of cardiovascular events [17].
At this regard, a recent systematic review showed that clinical inertia involves over 50% of T2D patients, ranging from 35.4 to 85.8% in the USA, to over 60% in Canada, Brazil, and Thailand [18]. Consequently, a significant number of T2D patients would suffer poor glycemic control for quite a long time before treatment intensification with oral glucose-lowering drugs (OHA) or insulin.
On the other hand, clinical inertia is a complex and multifaceted phenomenon, not only concerning glycemic control. Notably, the objectives of T2D management also include the timely treatment of all cardiovascular risk factors and body weight management. Weight loss, in overweight or obese subjects with T2D, represents a fundamental and achievable goal with various therapeutic options, including drugs and a personalized approach [19]. Despite this, the burden of obesity is increasing among individuals with both T2D and T1D [20].
In Italy, a continuous initiative to monitoring diabetes care has been in place since 2006 by a network of diabetes clinics operating within the national healthcare system as a key strategy to overcome clinical inertia [21,22,23].
This initiative, promoted by the Italian Association of Medical Diabetologists (AMD), which allows the yearly evaluation and critical revision of patterns of diabetes care, has documented a clear improvement in T2D care overtime [8], with a tangible impact on clinical outcomes and related healthcare costs [24].
As part of this initiative, the aim of our study was to evaluate temporal trends in insulin prescription and patterns of use over time in the large population of T2D outpatients participating to the AMD Annals Initiative. In particular, in three quinquennia spanning a 15-year observation period, we evaluated potential changes in the clinical characteristics of subjects receiving the first prescription of basal and/or fast-acting insulin therapy, and its consequences on 12-month glucose control.
Materials and methods
The AMD annals initiative
This observational, longitudinal, retrospective study was conducted in a network of Italian diabetes clinics participating in the continuous quality improvement initiative called AMD Annals, promoted since 2006, by the Italian Association of Clinical Diabetologists (Associazione Medici Diabetologi, AMD) [8, 24]. A total of 258 centres, accounting for approximately one-third of all the clinics operating within the Italian National Healthcare System, share the same software for data extraction from electronic medical records. Data from participating centres are annually collected in a standardized format (AMD Data File) and centrally analysed. Notably, both patients and centers are anonymously extracted and analyzed. The database is anonymous and each patient is assigned a unique numerical code, allowing the longitudinal analysis of the same patient in different years. As requested by the Regulatory authority in Italy, due to the nature of the study, the AMD Initiative received an ethics approval. The project is conducted without allocation of extra resources or financial incentives.
For the purposes of the present study, data on all patients with T2D attending the participating diabetes clinics between 2005 and 2019 were used. Two different groups were identified: patients starting basal insulin and patients starting fast acting insulin as add on to ongoing basal insulin treatment, with or without oral agents.
Statistical analyses
The index date for each patient was represented by the date of basal insulin or fast acting insulin start. Baseline characteristics at index date are reported separately for three 5-year periods (2005–2009; 2010–2014; 2015–2019) and treatment (start of basal insulin or fast acting insulin).
Baseline descriptive variables included age, sex, body weight, BMI, HbA1c, blood pressure, lipid profile, estimated glomerular filtration rate (eGFR; Chronic Kidney Disease Epidemiology Collaboration, CKD-EPI formula), and diabetes treatment.
In each cohort, HbA1c values were analysed at the index date and after 12 months.
Patients’ characteristics overall and by cohort were summarized as mean and standard deviation (continuous variables) or frequencies and percentages (categorical variables).
All statistical analyses were performed with SAS software, version 9.4 (SAS Institute Inc., Cary, NC).
Results
Clinical characteristics of T2D subjects intensifying therapy with basal insulin, overall and by study period
A total of 171,688 T2D subjects intensifying therapy with basal insulin were included in the analysis. They all received a first prescription for basal insulin and had not previously used either rapid insulin or mix-insulin. Clinical and biochemical characteristics of study subjects at the time of intensification of therapy, overall and in each 5-year period under consideration are shown in Table 1.
Among subjects intensifying therapy with basal insulin for the first time, from the first to the last quinquennium, we registered a progressive mild increase in the percentage of men (from 52.8 to 56.1% to 57.2%) and of mean age (from 66.9 ± 11.1 to 67.4 ± 12.2 to 68.1 ± 12.5 years). Conversely, the duration of diabetes at the time of prescribing basal insulin decreased progressively (from 11.4 ± 8.4 to 8.8 ± 7.8 and to 7.7 ± 7.2 years), suggesting a timely and more accurate prescribing attitude of Italian diabetologists.
Consistently, although mean HbA1c levels at the time of insulin prescription only modestly decreased over time, the percentage of subjects with HbA1c ≤ 7% at the time of insulin initiation increased from 10.4 to 14.1%, to 18.3%, and specularly, the percentage of subjects with HbA1c levels > 8% progressively decreased overtime (from 71 to 68 to 60%).
Overall, T2D subjects starting basal insulin presented out-of-target mean BP and lipid values. Clinical characteristics did not change in the three study periods, although major cardiovascular risk factors, such as BP, total cholesterol and LDL-Cholesterol levels, improved overtime.
On the contrary, mean values of body weight (79.1 ± 16.5 kg) and BMI (29.4 ± 5.5 kg/m2) which were diagnostics for an overweight condition in the first examined 5-year period, remained almost constant in the following two 5-year periods (body weight 80.9 ± 17.7 and 81.6 ± 18.4, respectively; BMI 29.8 ± 6.5 and 29.8 ± 7.1 kg/m2, respectively).
As for renal function, among those starting basal insulin, 36% had an impaired eGFR (< 60 ml/min/1.73 m2); in particular, 9.8% had eGFR < 30 ml/min/1.73 m2, 26% had eGFR 30–60 ml/min/1.72 m2, 37.4% had eGFR values 60–90 ml/min/1.73 m2 and 26.8% had eGFR > 90 ml/min/1.73 m2. Among new basal insulin users, there was a progressive increase overtime of those with moderate renal impairment (eGFR values 30–60 ml/min/1.73 m2) and a concomitant decrease of those with a mild eGFR decrease (eGFR 60–90 ml/min/1.73 m2) (Table 1).
Glucose-lowering agents prescribed in combination with basal insulin, overall and by study period, are shown in Table 2.
Metformin was the most prescribed oral agent (over 66%) in this population of T2D subjects, and its use remained constant over the three 5-year periods, while the use of glinides (from 21 to 7.6%) and sulfonylureas (from 50 to 24%) significantly decreased overtime. Acarbose and pioglitazone were overall infrequently prescribed (about 3% both) in the three 5-year period, while innovative drugs prescription rates progressively increased across the three 5-year periods. Notably, in the last quinquennium, basal insulin was prescribed in association with DPP4i in 23.5% of T2D subjects, with GLP1-RA in 6.8%, and SGLT2i in 9.9% (Table 2).
Clinical characteristics of T2D subjects intensifying therapy with fast-acting insulin, overall and by study period
Clinical characteristics of T2D subjects on basal insulin intensifying therapy by adding fast-acting insulin, overall and by study period are shown in Table 3. All T2D subjects analyzed in this group were on basal insulin (± OHA) and intensified therapy with fast-acting insulin; Table 3 shows clinical and biochemical characteristics of study subjects at the time of intensification of therapy, in each 5-year period.
From 2005 to 2019, a total of 137,225 T2D subjects on basal insulin intensified therapy with fast-acting insulin and were included in this analysis.
Both the percentage of men (from 51.2 to 56.3%) and mean age (from 66.1 ± 11.0 to 67.9 ± 13.1 years) progressively increased, from the first to the last quinquennium, while T2D duration at the time of starting fast-acting insulin progressively decreased overtime (from 14.5 ± 9.3 to 10.4 ± 8.5 years).
Overall, mean HbA1c levels at the time of starting fast-acting insulin were similar to that of T2D subjects starting basal insulin (9.1 ± 2.1% vs 8.9 ± 1.8%, respectively). Notably, among those first prescribed with fast-acting insulin, the percentage of subjects with at-target values (HbA1c ≤ 7%) increased from 13.2 to 17.1% and, vice-versa, the percentage of subjects with HbA1c > 8% slightly decreased (from 64.8 to 60.8%).
In the group of T2D subjects starting fast-acting insulin in add on to basal insulin, there was an overall improvement overtime of major risk factors; however, mean body weight (80.4 ± 17.5 kg) and BMI (29.9 ± 9.1 kg/m2) values, close to the cut-off for the diagnosis of obesity, remained almost constant in the three 5-year periods under examination (Table 3).
About renal function, among subjects starting fast-acting insulin, 41% had an impaired eGFR; in particular, 12% had eGFR < 30 ml/min/1.73 m2, 29.1% had eGFR 30–60 ml/min/1.73 m2, 35.3% had eGFR 60–90 ml/min/1.73m2 and 23.6% had eGFR > 90 ml/min/1.73 m2. Mean eGFR values were 65.7 ± 29.2 ml/min/1.73 m2.
The percentage of subjects with eGFR between 60 and 90 ml/min was 39.4% in the first examined quinquennium and 34.4% in the most recent one, while the distribution of subjects with the other eGFR classes did not change substantially overtime.
Glucose-lowering agents prescribed in combination with the start of multiple insulin regimens (fast-acting insulin in add-on to basal insulin), overall and by study period are shown in Table 4.
The use of metformin was 24.2% in this population, and it did not change over the three 5-year periods, while the use of glinides and sulfonylureas progressively decreased. Acarbose, pioglitazone, GLP-1 RAs and DPP4i were infrequently prescribed in combination with basal + fast acting insulins (< 1%), while the prescription of SGLT2i increased from 0 to 4.4% from the first to the last quinquennium.
HbA1c levels at therapy intensification and after 12 months, by study period
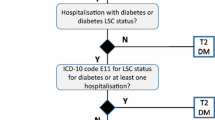
Mean HbA1c levels at the time of therapy intensification and after 12 months, by study period are shown in Fig. 1.
Overall, mean HbA1c levels decreased by 0.7–0.9% after 12 months from basal insulin prescription to a similar extent in the three examined periods. However, mean HbA1c levels remained above the recommended target in subjects with T2D (Fig. 1A).
Similarly, after 12 months from the starting of fast-acting insulin prescription, mean HbA1c levels fell by about 1 percentage point: in particular, in the 5-year period 2015–2019, mean HbA1c levels decreased from 9.1 ± 2.3% to 7.7 ± 1.4%. Even after initiating fast-acting insulin, mean HbA1c levels remained above recommended targets in the study population (Fig. 1B).
Discussion
The appropriate positioning and timing of initiation of insulin therapy have changed over time. In this analysis from the large AMD Annals Initiative, we investigated the clinical characteristics of subjects with T2D starting either basal and/or fast-acting insulin therapy over a 15-year period span.
Our study demonstrated a modest anticipation in the prescription of basal insulin and no profound changes in that of fast-acting formulations. Despite these observations, insulin therapy is still started at high HbA1c values and, after 12 months, mean HbA1c levels are still out-of-target, thus documenting the persistence of therapeutic inertia. A consistent body of literature tried to elucidate the underlying causes of this intricate and multifaceted phenomenon, involving a complex interaction among patients’, physicians’ and health systems’ barriers [18, 25]. At this regard, a recent sophisticated analysis of the AMD Annals dataset, with the support of artificial intelligence (logic learning machine), showed that patient's dynamic glycaemic profile, instead of repeated out-of-target HbA1c values, and specifically, a meaningful difference in HbA1c values between two consecutive visits (“HbA1c gap”) is the driver for the choice of starting insulin therapy [26].
In the current analysis, the variation of clinical characteristics of subjects starting insulin therapy documented a more proactive attitude of clinicians in the first prescription of insulin therapy overtime. Thus, our data showed a progressive decrease of diabetes duration, a higher rate of subjects with HbA1c < 7% and a reduction of those with HbA1c > 8%, among T2D subjects starting insulin therapy, when comparing the last vs. the first quinquennium. In particular, about 40% of our patients started basal insulin when HbA1c values were still < 8%. Notably, a recent analysis on the AMD Annals dataset showed a similar trend since, in more recent years, a second or third non-insulin agents after metformin was prescribed in T2D subjects with a shorter duration of the disease and an overall better CVD profile [15]. Collectively, these findings suggest an improved approach to clinical inertia of Italian diabetologists.
On the other hand, insulin was first prescribed to subjects with far off target mean HbA1c levels (approximately of 9%) and constantly high in the explored quinquennia, with no meaningful differences between those starting basal or fast-acting formulations. This means that our patients are exposed to the risk of uncontrolled hyperglycemia for a long time. Prolonged hyperglycemia is the first and more obvious consequence of the delay in initiating basal insulin, with an increased risk for micro- and macrovascular outcomes and all-cause mortality, likely independently from other conventional risk factors [27,28,29]. In accordance with our findings, a study on 37.053 T2D patients from different cohorts showed that basal insulin was usually prescribed when mean HbA1c values were > 9% and after up to 24 months of uncontrolled hyperglycemia [30].
Delaying the start of insulin therapy has negative effects even in the long-term, hindering the subsequent achievement of target values, and real-world data from electronic health records have shown that baseline HbA1c levels influence the likelihood of achieving glycemic goals with various therapeutic interventions [31].
On that point, a retrospective cohort study of adults with T2D from the US and UK, confirmed that when initiation of the first injectable therapy (either basal insulin or GLP-1RA) only occurred with HbA1c considerably above target, this impeded the achievement of glucose targets [32]. Clinical inertia also resulted in worse glycemic outcomes over a 12-month period in a large medical and pharmacy claim dataset, also contributing to the increased health care utilization and costs, due to poor clinical outcomes [33].
In line with these previous observations, also in our dataset, after 12 months from the start of insulin therapy, mean HbA1c levels decreased in all the three investigated time-periods, without reaching target values for mean HbA1c, both in subjects who started basal insulin therapy and in those who started fast-acting insulin, thus confirming how the delay of intensification has important consequences on the possibility of reaching therapeutic targets subsequently. A rather discouraging result that should also be considered in the light of the general finding that overall only about half of T2D subjects reach HbA1c levels < 7%, irrespective of the treatment [8]. Specifically, for insulin-treated patients, failure to achieve therapeutic targets may also be due to insufficient insulin titration, which does not allow to adapt the therapy to individual needs. Personalization of glucose targets toward less stringent goals is another crucial issue, since elderly, frail and multimorbid patients, are those who usually starts insulin therapy. Accordingly, it should be noticed that in our study, T2D patients starting basal insulin therapy had a mean age of 68 years and a mean disease duration of 9 years, with an overall preserved renal function, whereas those starting fast-acting insulin overall showed the same mean age, with a longer diabetes duration (12 vs 9 years) and a slightly worse renal function (41% vs 36% of patients with eGFR < 60 ml/min/1.73m2).
When addressing the topic of inertia in diabetes, the importance of the management of all cardiovascular risk factors, including body weight, must also be underlined as a fundamental target of T2D care. Thus, overweight/obesity is a clinical and social problem with a growing impact in T2D patients because of its prevalence, costs and associated cardiovascular risk.
Actually, clinicians have several available therapeutic options, that must include nutritional, education and lifestyle intervention, together with the use of innovative medications. These options should be personalized, also because of the different safety profiles and degrees of effectiveness of innovative drugs [19]. Importantly, even modest weight loss can improve glucose control and cardiometabolic profile, and a 5% body weight loss through a balanced hypocaloric diet was associated with an improvement in lipid profile and markers of systemic inflammation in subjects with metabolic syndrome [34].
It is well known that the efficacy of insulin therapy is counterbalanced by the risk of hypoglycemia and undesired weight gain, and our study clearly documents that, in subjects with T2D who intensified hypoglycemic therapy with insulin therapy over three 5 years (2005–2019), the average BMI value remained high (overweight) and almost unchanged over time. This observation strongly suggests the need for a more incisive commitment of clinicians in managing body weight also in T2D starting insulin therapy.
Our study also investigated changes in the background hypoglycemic therapy in patients starting insulin. A progressive decrease in the prescription of sulphonylureas and concomitant increase of innovative drugs was registered in the third quinquennium among those starting basal insulin, although with rates still far from those recommended by diabetes guidelines. As for those starting fast-acting formulation, as expected, the rate of use of other non-insulin drugs was overall lower, and only the increase of SGLT2i (allowed in combination with basal-bolus or basal-plus insulin regimens) should be noticed. Of course, these results may reflect timely guidelines and reimbursement procedures valid at the time of insulin prescription. On the other hand, the overall stable rate of prescription of insulin therapy in T2D subjects overtime (~ 30% of T2D subjects) [8], despite the variety of currently available therapeutic options, should be related to the progressive nature of the disease, and the occurrence of beta cell dysfunction and deterioration of glucose control, especially in those with longer diabetes duration, higher baseline HbA1c and glucose levels, as well as with increased lipid, inflammatory and beta-cell dysfunction markers or those on a combination of metformin plus secretagogues [13, 14].
As for renal function, the recent availability of non-insulin drugs that can be prescribed in cases of mild–moderate renal insufficiency did not significantly change the prescribing attitude over time in patients with severe CKD in the AMD Annals. Similarly, the overall clinical characteristics of subjects starting either basal and/or fast-acting insulin, did not significantly change in the three study periods, although all major cardiovascular risk factors improved overtime. The amelioration in the control of major CVD risk factors overtime further corroborates the progressive alignment of T2D management with guidelines, although the gap remains difficult to bridge due to therapeutic inertia and the increasingly stringent recommendations [3,4,5,6], as documented by the latest analysis of the AMD Annals dataset [8].
Limitations
Our analysis has some limitations that should be considered. First, no information on basal and fast-acting insulin titration is available, and consequently we could not explore the phenomenon of over-basalization or under-titration [35]. Moreover, a subgroup analysis of the combination of insulin with the innovative drugs, i.e., SGLT2i and GLP-1RAs, is also lacking, due to the limited number of subjects on those drugs in the considered timeframes.
Conclusions
The choice of glucose-lowering treatment is today focused on cardiovascular and renal protection, but uncontrolled hyperglycemia often requires a targeted approach to prevent adverse outcomes, often including insulin treatment. In this large cohort of T2D subjects during a long observation period, a progressively earlier start of insulin treatment was observed, suggesting a more proactive prescriptive approach. However, the off-targets HbA1c values achieved after 1 year of insulin therapy, suggest the need for greater clinical effort in T2D management.
Data availability
The datasets generated during and/or analyzed in the current study are available from the corresponding author upon reasonable request.
References
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R, IDF Diabetes Atlas Committee (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract 157:107843
14th Italian Barometer Diabetes Report 2021. IBDO Foundation 2021. https://viewer.ipaper.io/sp-servizi-pubblicitari-srl/report2021. Accessed 31 Jul 2023
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Das SR, Hilliard ME, Isaacs D, Johnson EL, Kahan S, Khunti K, Kosiborod M, Leon J, Lyons SK, Perry ML, Prahalad P, Pratley RE, Seley JJ, Stanton RC, Gabbay RA, on behalf of the American Diabetes Association (2023) 10. Cardiovascular Disease and Risk Management: Standards of Care in Diabetes-2023. Diabetes Care 46(Suppl 1):S158–S190. https://doi.org/10.2337/dc23-S010. (Erratum in: Diabetes Care. 2023 Jan 26;: PMID: 36507632; PMCID: PMC981047)
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Hilliard ME, Isaacs D, Johnson EL, Kahan S, Khunti K, Leon J, Lyons SK, Perry ML, Prahalad P, Pratley RE, Seley JJ, Stanton RC, Gabbay RA, on behalf of the American Diabetes Association (2023) 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2023. Diabetes Care 46(Suppl 1):S140–S157. https://doi.org/10.2337/dc23-S009
Standard italiani per la cura del diabete mellito 2018. Associazione Medici Diabetologi (AMD)-Società Italiana di Diabetologia (SID). https://www.siditalia.it/clinica/standarddi-cura-amd-sid. Accessed 23 Aug 2023
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, ESC Scientific Document Group et al (2020) 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Erratum in: Eur Heart J 41(2):255–323
Aschner P (2020) Insulin therapy in type 2 diabetes. Am J Ther 27(1):e79–e90. https://doi.org/10.1097/MJT.0000000000001088
Russo G, Di Bartolo P, Candido R, Lucisano G, Manicardi V, Giandalia A, Nicolucci A, Rocca A, Rossi MC, Di Cianni G (2023) The AMD ANNALS: a continuous initiative for the improvement of type 2 diabetes care. Diabetes Res Clin Pract 199:110672. https://doi.org/10.1016/j.diabres.2023.110672. (Epub 2023 Apr 19. PMID: 37084893)
Leite EB, Pedrosa HC, Casulari LA (2015) Results of glycated hemoglobin during treatment with insulin analogues dispensed in the public health system of Federal District in Brazil. Diabetol Metab Syndr 18(7):66. https://doi.org/10.1186/s13098-015-0061-0.PMID:26288660;PMCID:PMC4539715
Ramachandran A, Jain SM, Mukherjee S, Phatak S, Pitale S, Singh SK, Agrawal N, Majumdar A, Deshpande N, Jhulka S, Minakshisundaram S, Chawla M, Lodha S, Maheshwari A, Makkar BM, Rao S, Shah P, Ghosh R, Mohanasundaram S, Menon S, Chodankar D, Kanade V, Trivedi C (2020) Suboptimal glycemic control among subjects with diabetes mellitus in India: a subset analysis of cross-sectional wave-7 (2016) data from the International Diabetes Management Practices Study (IDMPS). Ther Adv Endocrinol Metab 27(11):2042018820937217
Tong YT, Gao GJ, Chang H, Wu XW, Li MT (2023) Development and economic assessment of machine learning models to predict glycosylated hemoglobin in type 2 diabetes. Front Pharmacol 30(14):1216182
Aschner P, Gagliardino JJ, Ilkova H, Lavalle F, Ramachandran A, Mbanya JC, Shestakova M, Chantelot JM, Chan JCN (2020) Persistent poor glycaemic control in individuals with type 2 diabetes in developing countries: 12 years of real-world evidence of the International Diabetes Management Practices Study (IDMPS). Diabetologia 63(4):711–721. https://doi.org/10.1007/s00125-019-05078-3. (Epub 2020 Jan 4. Erratum in: Diabetologia. 2020 May;63(5):1088-1089)
Russo GT, Giorda CB, Cercone S, De Cosmo S, Nicolucci A, Cucinotta D (2018) Beta cell stress in a 4-year follow-up of patients with type 2 diabetes: a longitudinal analysis of the BetaDecline Study. Diabetes Metab Res Rev 34(6):e3016. https://doi.org/10.1002/dmrr.3016. (Epub 2018 May 21. PMID: 29669179)
Giorda CB, Russo GT, Cercone S, De Cosmo S, Nicolucci A, Cucinotta D (2016) Incidence and correlated factors of beta cell failure in a 4-year follow-up of patients with type 2 diabetes: a longitudinal analysis of the BETADECLINE study. Acta Diabetol 53(5):761–767. https://doi.org/10.1007/s00592-016-0868-7. (Epub 2016 May 18 PMID: 27193886)
Cucinotta D, Nicolucci A, Giandalia A, Lucisano G, Manicardi V, Mannino D, Rossi MC, Russo GT, Di Bartolo P (2021) Temporal trends in intensification of glucose-lowering therapy for type 2 diabetes in Italy: data from the AMD Annals initiative and their impact on clinical inertia. Diabetes Res Clin Pract 181:109096. https://doi.org/10.1016/j.diabres.2021.109096. (Epub 2021 Oct 18 PMID: 34673085)
Okemah J, Peng J, Quiñones M (2018) Addressing clinical inertia in type 2 diabetes mellitus: a review. Adv Ther 35(11):1735–1745. https://doi.org/10.1007/s12325-018-0819-5. (Epub 2018 Oct 29. PMID: 30374807; PMCID: PMC6223992)
Paul SK, Klein K, Thorsted BL, Wolden ML, Khunti K (2015) Delay in treatment intensification increases the risks of cardiovascular events in patients with type 2 diabetes. Cardiovasc Diabetol 7(14):100
Almigbal TH, Alzarah SA, Aljanoubi FA, Alhafez NA, Aldawsari MR, Alghadeer ZY, Alrasheed AA (2023) Clinical inertia in the management of type 2 diabetes mellitus: a systematic review. Medicina (Kaunas) 59(1):182. https://doi.org/10.3390/medicina59010182
Lazzaroni E, Ben Nasr M, Loretelli C, Pastore I, Plebani L, Lunati ME, Vallone L, Bolla AM, Rossi A, Montefusco L, Ippolito E, Berra C, D’Addio F, Zuccotti GV, Fiorina P (2021) Anti-diabetic drugs and weight loss in patients with type 2 diabetes. Pharmacol Res 171:105782
Giandalia A, Russo GT, Ruggeri P, Giancaterini A, Brun E, Cristofaro M, Bogazzi A, Rossi MC, Lucisano G, Rocca A, Manicardi V, Bartolo PD, Cianni GD, Giuliani C, Napoli A (2023) The burden of obesity in type 1 diabetic subjects: a sex-specific analysis from the AMD annals initiative. J Clin Endocrinol Metab 108(11):e1224–e1235. https://doi.org/10.1210/clinem/dgad302
Rossi MC, Nicolucci A, Arcangeli A, Cimino A, De Bigontina G, Giorda C, For the Associazione Medici Diabetologi Annals Study Group et al (2008) Baseline quality-of-care data from a quality-improvement program implemented by a network of diabetes outpatient clinics. Diabetes Care 31:2166–2168
Nicolucci A, Rossi MC, Arcangeli A, Cimino A, de Bigontina G, Fava D, For AMD-Annals Study Group et al (2010) Four-year impact of a continuous quality improvement effort implemented by a network of diabetes outpatient clinics: the AMD-Annals initiative. Diabet Med 27:1041–1048
Rossi MC, Candido R, Ceriello A, Cimino A, Di Bartolo P, Giorda C, Esposito K, Lucisano G, Maggini M, Mannucci E, Meloncelli I, Nicolucci A, Pellegrini F, Scardapane M, Vespasiani G (2015) Trends over 8 years in quality of diabetes care: results of the AMD Annals continuous quality improvement initiative. Acta Diabetol 52:557–571
Ceriello A, Rossi MC, De Cosmo S, Lucisano G, Pontremoli R, Fioretto P, Giorda C, Pacilli A, Viazzi F, Russo G, Nicolucci A, AMD-Annals Study Group (2019) Overall quality of care predicts the variability of key risk factors for complications in type 2 diabetes: an observational, longitudinal retrospective study. Diabetes Care 42(4):514–519. https://doi.org/10.2337/dc20-er02
Ruiz-Negrón N, Wander C, McAdam-Marx C, Pesa J, Bailey RA, Bellows BK (2019) Factors associated with diabetes-related clinical inertia in a managed care population and its effect on hemoglobin A1c goal attainment: a claims-based analysis. J Manag Care Spec Pharm 25(3):304–313. https://doi.org/10.18553/jmcp.2019.25.3.304
Musacchio N, Zilich R, Ponzani P, Guaita G, Giorda C, Heidbreder R, Santin P, Di Cianni G (2023) Transparent machine learning suggests a key driver in the decision to start insulin therapy in individuals with type 2 diabetes. J Diabetes 15(3):224–236. https://doi.org/10.1111/1753-0407.13361. (Epub 2023 Mar 8. PMID: 36889912; PMCID: PMC10036260)
Laiteerapong N, Ham SA, Gao Y, Moffet HH, Liu JY, Huang ES, Karter AJ (2019) The legacy effect in type 2 diabetes: impact of early glycemic control on future complications (The Diabetes & Aging Study). Diabetes Care 42(3):416–426. https://doi.org/10.2337/dc17-1144++
Zhang Y, Hu G, Yuan Z, Chen L (2012) Glycosylated hemoglobin in relationship to cardiovascular outcomes and death in patients with type 2 diabetes: a systematic review and meta-analysis. PLoS ONE 7(8):e42551. https://doi.org/10.1371/journal.pone.0042551
Fralick M, Colacci M, Odutayo A, Siemieniuk R, Glynn RJ (2020) Lowering of hemoglobin A1C and risk of cardiovascular outcomes and all-cause mortality, a meta-regression analysis. J Diabetes Complic 34(11):107704. https://doi.org/10.1016/j.jdiacomp.2020.107704]
Raccah D, Guerci B, Ajmera M, Davis K, Meyers J, Lew E, Shaunik A, Blonde L (2019) Clinical implications of prolonged hyperglycaemia before basal insulin initiation in type 2 diabetes patients: An electronic medical record database analysis. Endocrinol Diabetes Metab 2(3):e00061. https://doi.org/10.1002/edm2.61
Pantalone KM, Misra-Hebert AD, Hobbs TM, Ji X, Kong SX, Milinovich A, Weng W, Bauman JM, Ganguly R, Burguera B, Kattan MW, Zimmerman RS (2020) Intensification patterns and the probability of HbA1c goal attainment in Type 2 diabetes mellitus: real-world evidence for the concept of “intensification inertia.” Diabet Med 37(7):1114–1124. https://doi.org/10.1111/dme.13900
Peng XV, McCrimmon RJ, Shepherd L, Boss A, Lubwama R, Dex T, Skolnik N, Ji L, Avogaro A, Blonde L (2020) Glycemic control following GLP-1 RA or basal insulin initiation in real-world practice: a retrospective, observational, longitudinal cohort study. Diabetes Ther 11(11):2629–2645. https://doi.org/10.1007/s13300-020-00905-y
Kallenbach L, Shui AM, Cheng WY, Fan T, Hu W, Zichlin ML, Duh MS, Ye F, Levin PA (2018) Predictors and clinical outcomes of treatment intensification in patients with type 2 diabetes uncontrolled on basal insulin in a real-world setting. Endocr Pract 24(9):805–814. https://doi.org/10.4158/EP-2017-0261
Montefusco L, D’Addio F, Loretelli C, Ben Nasr M, Garziano M, Rossi A, Pastore I, Plebani L, Lunati ME, Bolla AM, Porta MD, Piuri G, Rocchio F, Abdelsalam A, Assi E, Barichella M, Maestroni A, Usuelli V, Loreggian L, Muzio F, Zuccotti GV, Cazzola R, Fiorina P (2021) Anti-inflammatory effects of diet and caloric restriction in metabolic syndrome. J Endocrinol Invest 44(11):2407–2415. https://doi.org/10.1007/s40618-021-01547-y
Mehta R, Goldenberg R, Katselnik D, Kuritzky L (2021) Practical guidance on the initiation, titration, and switching of basal insulins: a narrative review for primary care. Ann Med 53(1):998–1009. https://doi.org/10.1080/07853890.2021.1925148
Funding
This research received external funding from the Association of Medical Diabetologists (Associazione Medici Diabetologi, AMD).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Data for this analysis comes from the database of the Annals Initiative of the Italian Association of Medical Diabetologists (AMD, Associazione Medici Diabetologi). The database includes clinical information on all patients with diabetes receiving care at 295 diabetes centers in Italy. Patients and centers are identified by numeric codes, and analysis is centralized. Participating centers share a software developed to extract information from electronic medical records. Data are centrally collected and analyzed anonymously. Due to the methodology of data extraction, the center, patients and all data are anonymous and there is no possibility of tracing the patient's name. Local ethics committees of each participating center approved the study protocol. The project is conducted without allocation of extra resources or financial incentives.
Informed consent
The AMD Annals Initiative database is anonymous by study-design and the analysis is retrospective. Given the nature of the study, based on the Italian regulations, the signature of the informed consent was not requested.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Giandalia, A., Nicolucci, A., Modugno, M. et al. Temporal trends in the starting of insulin therapy in type 2 diabetes in Italy: data from the AMD Annals initiative. J Endocrinol Invest 47, 2087–2096 (2024). https://doi.org/10.1007/s40618-024-02306-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-024-02306-5