Abstract
Purpose
Previous studies have not fully described the relationship between high-density lipoprotein cholesterol (HDL-C) and death risks from all cause and cardiovascular disease (CVD). This study quantitatively evaluates HDL-C–mortality associations.
Methods
Embase and PubMed databases were searched for relevant articles published up to 1 June 2019. Random-effects models were used to pool relative risks (RRs) and 95% confidence intervals (CIs). We used restricted cubic splines to model the dose–response association.
Results
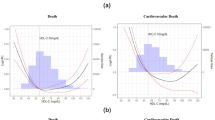
We identified 32 prospective cohort studies including 369,904 participants and 33,473 total deaths (9426 CVD deaths). Compared to the lowest HDL-C levels, all cause and CVD mortality risks were reduced by 18% (RR 0.82; 95% CI, 0.73–0.93) and 36% (0.64, 0.46–0.89), respectively, for the highest HDL-C levels. All cause and CVD mortality risks were reduced by 15% (0.85, 0.79–0.92) and 23% (0.77, 0.69–0.87), respectively, with each 1 mmol/L increment of HDL-C. We found evidence of nonlinear and negative dose–response associations of HDL-C with all cause and CVD mortality (Pnonlinearity < 0.001), and the lowest death risks from all cause and CVD were observed at approximately 1.34 and 1.55 mmol/L, respectively.
Conclusion
HDL-C is inversely associated with all cause and CVD mortality risks under approximately 2.05 and 2.33 mmol/L, respectively. Optimal doses require investigation via clinical practice or high-quality research.



Similar content being viewed by others
Availability of data and materials
The data and materials of this study are available from the corresponding author upon reasonable request.
Code availability
The code of software application is available from the corresponding author upon reasonable request.
References
World Health Organization. Projections of mortality and causes of death, 2016 to 2060. https://www.who.int/healthinfo/global_burden_disease/projections/en/. Accessed 21 July 2020
Zhou M, Wang H, Zeng X et al (2019) Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 394(10204):1145–1158
World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013–2020. http://www.who.int/cardiovascular_diseases/15March2013UpdatedRevisedDraftActionPlanAPPROVEDBYADG.pdf. Accessed 27 July 2020
World Health Organization. Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. http://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf. Accessed 21 July 2020
Committee for the Promotion Healthy China Initiative. Healthy China Initiative (2019–2030). http://www.gov.cn/xinwen/2019-07/15/content_5409694.htm. Accessed 18 July 2020
Xiang AS, Kingwell BA (2019) Rethinking good cholesterol: a clinicians’ guide to understanding HDL. Lancet Diabetes Endo 7(7):575–582
Cui Y, Blumenthal RS, Flaws JA et al (2001) Non-high-density lipoprotein cholesterol level as a predictor of cardiovascular disease mortality. JAMA Intern Med 161(11):1413–1419
Linna M, Ahotupa M, Lopponen MK et al (2012) Circulating oxidised LDL lipids, when proportioned to HDL-c, emerged as a risk factor of all-cause mortality in a population-based survival study. Age Ageing 42(1):110–113
Oksala N, Seppälä I, Hernesniemi J et al (2012) Complementary prediction of cardiovascular events by estimated apo- and lipoprotein concentrations in the working age population. The Health 2000 Study. Ann Med 45(2):141–148
McGarrah RW, Craig DM, Haynes C et al (2016) High-density lipoprotein subclass measurements improve mortality risk prediction, discrimination and reclassification in a cardiac catheterization cohort. Atherosclerosis 246:229–235
Ou S, Chen Y, Shih C, et al (2017) Impact of physical activity on the association between lipid profiles and mortality among older people. Sci Rep-UK 7(1)
Bae J, Yang Y, Li Z et al (2012) Low cholesterol is associated with mortality from cardiovascular diseases: a dynamic cohort study in Korean adults. J Korean Med Sci 27(1):58
Madsen CM, Varbo A, Nordestgaard BG (2017) Extreme high high-density lipoprotein cholesterol is paradoxically associated with high mortality in men and women: two prospective cohort studies. Eur Heart J 38(32):2478–2486
Psaty BM, Anderson M, Kronmal RA et al (2004) The association between lipid levels and the risks of incident myocardial infarction, stroke, and total mortality: the Cardiovascular Health Study. J Am Geriatr Soc 52(10):1639–1647
Okamura T, Hayakawa T, Kadowaki T et al (2006) The inverse relationship between serum high-density lipoprotein cholesterol level and all-cause mortality in a 9.6-year follow-up study in the Japanese general population. Atherosclerosis 184(1):143–150
Wells GA, Shea B, O’Connell D, et al The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 21 July 2020
Orsini N, Li R, Wolk A et al (2012) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175(1):66–73
Higgins JPT, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Paunio M, Heinonen OP, Virtamo J et al (1994) HDL cholesterol and mortality in Finnish men with special reference to alcohol intake. Circulation 90(6):2909–2918
Perova NV, Oganov RG, Williams DH et al (1995) Association of high-density-lipoprotein cholesterol with mortality and other risk factors for major chronic noncommunicable diseases in samples of US and Russian men. Ann Epidemiol 5(3):179–185
Tervahauta M, Pekkanen J, Nissinen A (1995) Risk factors of coronary heart disease and total mortality among elderly men with and without preexisting coronary heart disease. J Am Coll Cardiol 26(7):1623–1629
Norrish A, North D, Yee RL et al (1995) Do cardiovascular disease risk factors predict all-cause mortality. Int J Epidemiol 24(5):908–914
von Mühlen D, Langer RD, Barrett-Connor E (2003) Sex and time differences in the associations of non-high-density lipoprotein cholesterol versus other lipid and lipoprotein factors in the prediction of cardiovascular death (The Rancho Bernardo Study). Am J Cardiol 91(11):1311–1315
Akerblom JL, Costa R, Luchsinger JA et al (2008) Relation of plasma lipids to all-cause mortality in Caucasian, African-American and Hispanic elders. Age Ageing 37(2):207–213
Landi F, Russo A, Pahor M et al (2008) Serum High-density lipoprotein cholesterol levels and mortality in Frail. Community-Living Elderly Gerontol 54(2):71–78
Nilsson G, Öhrvik J, Lönnberg I et al (2009) Ten-year survival in 75-year-old men and women: predictive ability of total cholesterol, HDL-C, and LDL-C. Curr Gerontol Geriatr Res 2009:1–7
Upmeier E, Lavonius S, Lehtonen A et al (2009) Serum lipids and their association with mortality in the elderly: a prospective cohort study. Aging Clin Exp Res 21(6):424–430
Werle MH, Moriguchi E, Fuchs SC et al (2011) Risk factors for cardiovascular disease in the very elderly: results of a cohort study in a city in southern Brazil. Eur J Cardiov Prev R 18(3):369–377
Newson RS, Felix JF, Heeringa J et al (2011) Association between serum cholesterol and noncardiovascular mortality in older age. J Am Geriatr Soc 59(10):1779–1785
Skretteberg PT, Grundvold I, Kjeldsen SE et al (2012) HDL-cholesterol and prediction of coronary heart disease: modified by physical fitness? Atherosclerosis 220(1):250–256
Venskutonyte L, Rydén L, Nilsson G et al (2012) Mortality prediction in the elderly by an easily measured metabolic index. Diabetes Vasc Dis Re 9(3):226–233
Piotrowski W, Waśkiewicz A, Cicha-Mikołajczyk A (2016) Global cardiovascular mortality risk in the adult Polish population: prospective assessment of the cohorts studied in multicentre national WOBASZ and WOBASZ Senior studies. Kardiol Pol 74(3):262–273
Nomikos T, Panagiotakos D, Georgousopoulou E, et al (2015) Hierarchical modelling of blood lipids’ profile and 10-year (2002–2012) all cause mortality and incidence of cardiovascular disease: the ATTICA study. Lipids Health Dis 14(1)
Liu Z, Zhong G, Li S, et al (2015) Use of serum albumin and activities of daily living to predict mortality in long-lived individuals over 95 years of age: a population-based study. Age 37(4)
Umeki Y, Adachi H, Enomoto M et al (2016) Serum albumin and cerebro-cardiovascular mortality during a 15-year study in a community-based Cohort in Tanushimaru, a cohort of the seven countries study. Internal Med 55:2917–2925
Hirata A, Okamura T, Sugiyama D et al (2016) The relationship between very high levels of serum high-density lipoprotein cholesterol and cause-specific mortality in a 20-year follow-up study of Japanese general population. J Atheroscler Thromb 23(7):800–809
Ghasemzadeh Z, Abdi H, Asgari S, et al (2016) Divergent pathway of lipid profile components for cardiovascular disease and mortality events: results of over a decade follow-up among Iranian population. Nutr Metab 13(1)
Hamer M, O’Donovan G, Stamatakis E (2018) High-density lipoprotein cholesterol and mortality. Arterioscl Throm Vas Biol 38(3):669–672
Li Z, Lv Y, Zhong W et al (2019) High-density lipoprotein cholesterol and all-cause and cause-specific mortality among the elderly. J Clin Endocr Metab 104(8):3370–3378
Penson P, Long L, Howard G et al (2019) Associations between cardiovascular disease, cancer and very low HDL cholesterol in the Reasons for Geographical And Racial Differences in Stroke (REGARDS) study. Cardiovasc Res 115(1):204–212
Bowe B, Xie Y, Xian H et al (2016) High density lipoprotein cholesterol and the risk of all-cause mortality among U.S. Veterans Clin J Am Soc Nephrol 11:1784–1793
Hirata A, Sugiyama D, Watanabe M et al (2018) Association of extremely high levels of high-density lipoprotein cholesterol with cardiovascular mortality in a pooled analysis of nine cohort studies including 43,407 individuals: the EPOCH-JAPAN study. J Clin Lipidol 12(3):674–684
Wilkins JT, Ning H, Stone NJ et al (2014) Coronary heart disease risks associated with high levels of HDL cholesterol. J Am Heart Assoc 3(2):e519
Ju S, Lee J, Kim D (2017) Association of metabolic syndrome and its components with all-cause and cardiovascular mortality in the elderly: a meta-analysis of prospective cohort studies. Medicine 96(45):e8491
Barzi F, Patel A, Woodward M et al (2005) A comparison of lipid variables as predictors of cardiovascular disease in the Asia Pacific region. Ann Epidemiol 15(5):405–413
Toth PP (2009) Should we target HDL cholesterol level in lowering cardiovascular risk? Pol Arch Intern Med 119(10):667
Mineo C, Shaul PW (2012) Novel biological functions of high-density lipoprotein cholesterol. Circ Res 111(8):1079–1090
Lüscher TF, Landmesser U, von Eckardstein A et al (2014) High-density lipoprotein: vascular protective effects, dysfunction, and potential as therapeutic target. Circ Res 114(1):171–182
Rye KA, Barter PJ (2014) Cardioprotective functions of HDLs. J Lipid Res 55(2):168–179
Barter PJ, Rye KA (1996) Molecular mechanisms of reverse cholesterol transport. Curr Opin Lipidol 7(2):82–87
Cheng E, Burrows R, Correa P et al (2019) Light smoking is associated with metabolic syndrome risk factors in Chilean young adults. Acta Diabetol 56(4):473–479
Fu S, Luo L, Ye P et al (2013) Overall and abdominal obesity indicators had different association with central arterial stiffness and hemodynamics independent of age, sex, blood pressure, glucose, and lipids in Chinese community-dwelling adults. Clin Interv Aging 3:1579–1584
Varbo A, Nordestgaard BG (2019) Commentary: triglycerides or HDL cholesterol in cardiovascular disease-which is the true culprit? Int J Epidemiol. https://doi.org/10.1093/ije/dyy292
Agerholm-Larsen B, Nordestgaard BG, Steffensen R et al (2000) Elevated HDL cholesterol is a risk factor for ischemic heart disease in white women when caused by a common mutation in the cholesteryl ester transfer protein gene. Circulation 101(16):1907–1912
Zanoni P, Khetarpal SA, Larach DB et al (2016) Rare variant in scavenger receptor BI raises HDL cholesterol and increases risk of coronary heart disease. Science 351(6278):1166–1171
Marz W, Kleber ME, Scharnagl H et al (2017) HDL cholesterol: reappraisal of its clinical relevance. Clin Res Cardiol 106(9):663–675
Funding
This study was supported by the National Key R&D Program of China (NO. 2017YFC0907301) and the Science and Technology Plan Project of Guizhou Province, China (NO. QKHPTRC[2018]5403).
Author information
Authors and Affiliations
Contributions
LL conceived, designed and performed the work; LL and MH screened and evaluated studies; LL and MH extracted the data; LL, MH, RQ, QL, and XZ analyzed the data; LL wrote the manuscript; JZ, SZ, LZ, ZX, CZ, and FH revised the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy. As the corresponding author, FH takes responsibility for the contents of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval
As this meta-analysis is performed based on the published studies, no ethical approval was required.
Consent to participate
Not applicable.
Consent for publication
As this meta-analysis is performed based on the published studies, no patient safety consideration was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, L., Han, M., Qie, R. et al. A dose–response meta-analysis to evaluate the relationship between high-density lipoprotein cholesterol and all-cause and cardiovascular disease mortality. J Endocrinol Invest 45, 551–562 (2022). https://doi.org/10.1007/s40618-021-01690-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-021-01690-6