Abstract
Purpose
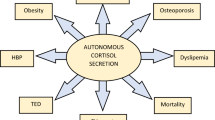
To evaluate differences between patients with unilateral and bilateral adrenal incidentalomas (AIs) in the prevalence of autonomous cortisol secretion (ACS) and related comorbidities.
Methods
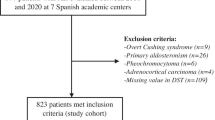
In this multicentre retrospective study, AIs ≥ 1 cm without overt hormonal excess were included in the study. ACS was defined by a post-dexamethasone suppression test (DST) serum cortisol ≥ 5.0 µg/dl, in the absence of signs of hypercortisolism. For the association of ACS with the prevalence of comorbidities, post-DST serum cortisol was also analysed as a continuous variable.
Results
Inclusion criteria were met by 823 patients, 66.3% had unilateral and 33.7% bilateral AIs. ACS was demonstrated in 5.7% of patients. No differences in the prevalence of ACS and related comorbidities were found between bilateral and unilateral AIs (P > 0.05). However, we found that tumour size was a good predictor of ACS (OR = 1.1 for each mm, P < 0.001), and the cut-off of 25 mm presented a good diagnostic accuracy to predict ACS (sensitivity of 69.4%, specificity of 74.1%).
During a median follow-up time of 31.2 (IQR = 14.4–56.5) months, the risk of developing dyslipidaemia was increased in bilateral compared with unilateral AIs (HR = 1.8, 95% CI = 1.1–3.0 but, this association depended on the tumour size observed at the end of follow-up (HR adjusted by last visit-tumour size = 0.9, 95% CI = 0.1–16.2).
Conclusions
Tumour size, not bilaterality, is associated with a higher prevalence of ACS. During follow-up, neither tumour size nor bilaterality were associated with the development of new comorbidities, yet a larger tumour size after follow-up explained the association of bilateral AIs with the risk of dyslipidaemia.


Similar content being viewed by others
References
Wagner J, Aron DC (2012) Incidentalomas—a “disease” of modern imaging technology. Best Pract Res Clin Endocrinol Metab 26(1):3–8. https://doi.org/10.1016/j.beem.2011.08.006
Araujo-Castro M, Sampedro Núñez MA, Marazuela M (2019) Autonomous cortisol secretion in adrenal incidentalomas. Endocrine 64(1):1–13. https://doi.org/10.1007/s12020-019-01888-y
Terzolo M, Stigliano A, Chiodini I, Loli P, Furlani L, Arnaldi G et al (2011) AME position statement on adrenal incidentaloma. Eur J Endocrinol 164(6):851–870. https://doi.org/10.1530/EJE-10-1147
Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A et al (2016) Management of adrenal incidentalomas: European society of endocrinology clinical practice guideline in collaboration with the European network for the study of adrenal tumours. Eur J Endocrinol 175(2):G1–G34. https://doi.org/10.1530/EJE-16-0467
Chiodini I (2011) Diagnosis and treatment of subclinical hypercortisolism. J Clin Endocrinol Metab 96(5):1223–1236
Araujo-Castro M, Robles Lázaro C, Parra Ramírez P, Cuesta Hernández M, Sampedro Núñez MA, Marazuela M (2019) Cardiometabolic profile of non-functioning and autonomous cortisol-secreting adrenal incidentalomas. Is the cardiometabolic risk similar or are there differences? Endocrine 66(3):650–659. https://doi.org/10.1007/s12020-019-02066-w
Rossi R, Tauchmanova L, Luciano A, Di Martino M, Battista C, Del Viscovo L et al (2000) Subclinical cushing’s syndrome in patients with adrenal incidentaloma: clinical and biochemical features. J Clin Endocrinol Metab 85(4):1440–1448
Terzolo M, Pia A, Ali A, Osella G, Reimondo G, Bovio S et al (2002) Adrenal incidentaloma: a new cause of the metabolic syndrome? J Clin Endocrinol Metab 87(3):998–1003
Vassiliadi DA, Ntali G, Vicha E, Tsagarakis S (2011) High prevalence of subclinical hypercortisolism in patients with bilateral adrenal incidentalomas: a challenge to management. Clin Endocrinol (Oxf) 74(4):438–444. https://doi.org/10.1111/j.1365-2265.2010.03963.x
Ognjanović S, Macut D, Petakov M, Elezović Kovačević V, Isailović T, Bozić Antić I, Ilić DS et al (2016) The occurrence of subclinical hypercortisolism and osteoporosis in patients with incidentally discovered unilateral and bilateral adrenal tumours. J Med Biochem 35(4):401–409. https://doi.org/10.1515/jomb-2016-0020.0020
Yener S, Ertilav S, Secil M, Akinci B, Demir T, Kebapcilar L et al (2012) Increased risk of unfavorable metabolic outcome during short-term follow-up in subjects with nonfunctioning adrenal adenomas. Med Princ Pract 21(5):429–434. https://doi.org/10.1159/000336589
Masserini B, Morelli V, Bergamaschi S, Ermetici F, Eller-Vainicher C, Barbieri AM et al (2009) The limited role of midnight salivary cortisol levels in the diagnosis of subclinical hypercortisolism in patients with adrenal incidentaloma. Eur J Endocrinol 160(1):87–92. https://doi.org/10.1530/EJE-08-0485
Androulakis A II, Kaltsas GA, Markou A, Tseniklidi E, Kafritsa P, Pappa T et al (2011) The functional status of incidentally discovered bilateral adrenal lesions. Clin Endocrinol (Oxf) 75(1):44–49. https://doi.org/10.1111/j.1365-2265.2011.04013.x
Vassilatou E, Vryonidou A, Ioannidis D, Paschou SA, Panagou M, Tzavara I (2014) Bilateral adrenal incidentalomas differ from unilateral adrenal incidentalomas in subclinical cortisol hypersecretion but not in potential clinical implications. Eur J Endocrinol 171(1):37–45. https://doi.org/10.1530/EJE-13-0848
Favia G, Lumachi F, Basso S, D’Amico DF, D’Amico DF (2000) Management of incidentally discovered adrenal masses and risk of malignancy. Surgery 128(6):918–924
Barzon L, Sonino N, Fallo F, Palù G, Boscaro M (2003) Prevalence and natural history of adrenal incidentalomas. Eur J Endocrinol 149(4):273–285
Grumbach MM, Biller BMK, Braunstein GD, Campbell KK, Aidan Carney J, Godley PA et al (2003) Management of the clinically inapparent adrenal mass (“incidentaloma”). Ann Intern Med 138(5):424–429
Anagnostis P, Karagiannis A, Tziomalos K, Kakafika AI, Athyros VG, Mikhailidis DP (2009) Adrenal incidentaloma: a diagnostic challenge. Hormones 8:163–184
Association American Diabetes group (2018) Updates to the Standards of Medical Care in Diabetes-2018. Diabetes Care 41(9):2045–2047. https://doi.org/10.2337/dc18-su09
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002) Third report of the national cholesterol education program (NCEP) Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation 106(25):3143–3421
Morelli V, Masserini B, Salcuni AS et al (2010) Subclinical hypercortisolism: correlation between biochemical diagnostic criteria and clinical aspects. Clin Endocrinol (Oxf) 73(2):161–166. https://doi.org/10.1111/j.1365-2265.2010.03794.x
Olsen H, Nordenström E, Bergenfelz A, Nyman U, Valdemarsson S, Palmqvist E (2012) Subclinical hypercortisolism and CT appearance in adrenal incidentalomas: a multicenter study from Southern Sweden. Endocrine 42(1):164–173. https://doi.org/10.1007/s12020-012-9622-2
Ilias I, Sahdev A, Reznek RH, Grossman AB, Pacak K (2007) The optimal imaging of adrenal tumours: a comparison of different methods. Endocr Relat Cancer 14(3):587–599
Vassilatou E, Vryonidou A, Michalopoulou S, Manolis J, Caratzas J, Phenekos C et al (2009) Hormonal activity of adrenal incidentalomas: results from a long-term follow-up study. Clin Endocrinol (Oxf) 70(5):674–679. https://doi.org/10.1111/j.1365-2265.2008.03492.x
Falcetta P, Orsolini F, Benelli E, Agretti P, Vitti P, Di Cosmo C et al (2020) Clinical features, risk of mass enlargement, and development of endocrine hyperfunction in patients with adrenal incidentalomas: a long-term follow-up study. Endocrine. https://doi.org/10.1007/s12020-020-02476-1
Huayllas MKP, Sirineni GK, Smith LM, Christopher Gallagher J, Singh RJ, Netzel BC et al (2020) Correlation between size and function of unilateral and bilateral adrenocortical nodules: an observational study. Am J Roentgenol 214(4):800–807. https://doi.org/10.2214/AJR.19.21753
Mosconi C, Vicennati V, Papadopoulos D, Di Dalmazi G, Morselli-Labate AM, Golfieri R, Pasquali R (2017) Can imaging predict subclinical cortisol secretion in patients with adrenal adenomas? A CT predictive score. Am J Roentgenol 209(1):122–129. https://doi.org/10.2214/AJR.16.16965
Elhassan YS, Alahdab F, Prete A, Delivanis DA, Khanna A, Prokop L et al (2019) Natural history of adrenal incidentalomas with and without mild autonomous cortisol excess. Ann Intern Med 171(2):107–116. https://doi.org/10.7326/m18-3630
Morelli V, Palmieri S, Salcuni AS, Eller-Vainicher C, Cairoli E, Zhukouskaya V et al (2013) Bilateral and unilateral adrenal incidentalomas: biochemical and clinical characteristics. Eur J Endocrinol 168(2):235–241. https://doi.org/10.1530/EJE-12-0777
Majnik J, Patocs A, Balogh K, Toth M, Gergics P, Szappanos A et al (2013) Brief report: overrepresentation of the N363S variant of the glucocorticoid receptor gene in patients with bilateral adrenal incidentalomas. Eur J Endocrinol 168(2):235–241. https://doi.org/10.1530/EJE-12-0777
Di Blasio AM, Van Rossum EFC, Maestrini S, Berselli ME, Tagliaferri M, Podestà F et al (2003) The relation between two polymorphisms in the glucocorticoid receptor gene and body mass index, blood pressure and cholesterol in obese patients. Clin Endocrinol (Oxf) 59(1):68–74
Morelli V, Donadio F, Eller-Vainicher C, Cirello V, Olgiati L, Savoca C et al (2010) Role of glucocorticoid receptor polymorphism in adrenal incidentalomas. Eur J Clin Invest 40(9):803–811. https://doi.org/10.1111/j.1365-2362.2010.02330.x
Yener S, Ertilav S, Secil M, Demir T, Akinci B, Kebapcilar L et al (2010) Prospective evaluation of tumour size and hormonal status in adrenal incidentalomas. J Endocrinol Invest 33(1):32–36. https://doi.org/10.3275/6377
Giordano R, Marinazzo E, Berardelli R, Picu A, Maccario M, Ghigo E et al (2010) Long-term morphological, hormonal, and clinical follow-up in a single unit on 118 patients with adrenal incidentalomas. Eur J Endocrinol 162(4):779–785. https://doi.org/10.1530/EJE-09-0957
Brossaud J, Ducint D, Corcuff JB (2016) Urinary glucocorticoid metabolites: biomarkers to classify adrenal incidentalomas. Clin Endocrinol (Oxf) 84(2):236–243. https://doi.org/10.1111/cen.12717
Acknowledgements
SENDIMAD: BECA SENDIMAD de Ayuda a la Investigación en Endocrinología, Nutrición y Diabetes 2019. IRYCIS: Convocatoria intramural de ayudas a proyectos de investigación de investigadores noveles, investigadores clínicos asociados y/o grupos emergentes del Hospital Universitario Ramón y Cajal.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Ethical approval
All procedures performed in the participants of the study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, no informed consent is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Araujo-Castro, M., Robles Lázaro, C., Parra Ramírez, P. et al. Maximum adenoma diameter, regardless of uni- or bilaterality, is a risk factor for autonomous cortisol secretion in adrenal incidentalomas. J Endocrinol Invest 44, 2349–2357 (2021). https://doi.org/10.1007/s40618-021-01539-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-021-01539-y