Abstract
Purpose
Evidence showed that benign thyroid disease was one of the risk factors for thyroid cancer. However, the results of some studies were inconsistent and were previously meta-analyses of case–control studies. Therefore, we performed a meta-analysis of prospective studies to investigate the relationship between benign thyroid diseases and thyroid cancer risk.
Methods
All eligible studies were identified via systematic searches of multiple literature databases. The combined RR (relative risk)/HR (hazard ratio) or SIR (standardized incidence ratio) with 95% confidence interval was calculated. Heterogeneity was assessed with the I2 test. Publication bias and subgroup analyses were also performed.
Results
Twelve studies were eligible for inclusion in the meta-analysis. The pooled RR/HR of thyroid carcinoma in benign thyroid diseases was 4.39 (95% CI 3.22–5.55). The pooled SIR of thyroid carcinoma in benign thyroid diseases was 5.98 (95% CI 4.09–7.86). Subgroup analysis was performed using the type of benign thyroid diseases. Effect value was RR/HR: hyperthyroidism (RR/HR = 3.89, 95% CI = 1.69–6.08), hypothyroidism (RR/HR = 2.72, 95% CI = 1.04–4.41), and goiter (RR/HR = 22.18, 95% CI = 12.09–32.28). Effect value was SIR: hyperthyroidism (RR/HR = 5.96, 95% CI = 1.88–10.03), goiter (RR/HR = 7.65, 95% CI = 6.94–8.37), and thyroiditis (RR/HR = 3.25, 95% CI = 1.62–4.89).
Conclusions
Our study has shown that benign thyroid diseases might be associated with increased risk of thyroid cancer, especially in hyperthyroidism, hypothyroidism, and goiter. However, further investigation is needed to better understand the underlying biological mechanisms.







Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics. CA Cancer J Clin 68(1):7–30. https://doi.org/10.3322/caac.21442
Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R (2013) Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol 2013:965212. https://doi.org/10.1155/2013/965212
Albi E, Cataldi S, Lazzarini A, Codini M, Beccari T, Ambesi-Impiombato FS, Curcio F (2017) Radiation and thyroid cancer. Int J Mol Sci 18(5):E911. https://doi.org/10.3390/ijms18050911
Ron E, Kleinerman RA, Boice JD Jr, LiVolsi VA, Flannery JT, Fraumeni JF Jr (1987) A population-based case-control study of thyroid cancer. J Natl Cancer Inst 79(1):1–12
Franceschi S, Fassina A, Talamini R, Mazzolini A, Vianello S, Bidoli E, Serraino D, La Vecchia C (1989) Risk factors for thyroid cancer in northern Italy. Int J Epidemiol 18(3):578–584
Ren PY, Liu J, Xue S, Chen G (2017) Pediatric differentiated thyroid carcinoma: The clinicopathological features and the coexistence of Hashimoto’s thyroiditis. Asian J Surg. https://doi.org/10.1016/j.asjsur.2017.10.006
Tam AA, Ozdemir D, Aydın C, Bestepe N, Ulusoy S, Sungu N, Ersoy R, Cakir B (2018) Association between preoperative thyrotrophin and clinicopathological and aggressive features of papillary thyroid cancer. Endocrine 59(3):565–572. https://doi.org/10.1007/s12020-018-1523-6
Hung SH, Chung SD, Lin HC (2018) Thyroxin use is associated with increased risk of thyroid cancer in patients with hypothyroidism. J Clin Pharmacol 58(1):29–33. https://doi.org/10.1002/jcph.972
Kitahara CM, Farkas DK, Jørgensen JOL, Cronin-Fenton D, Sørensen HT (2018) Benign thyroid diseases and risk of thyroid cancer: a nationwide cohort study. J Clin Endocrinol Metab 103(6):2216–2224. https://doi.org/10.1210/jc.2017-02599
Anil C, Goksel S, Gursoy A (2010) Hashimoto’s thyroiditis is not associated with increased risk of thyroid cancer in patients with thyroid nodules: a single-center prospective study. Thyroid 20(6):601–606. https://doi.org/10.1089/thy.2009.0450
Gabalec F, Srbova L, Nova M, Hovorkova E, Hornychova H, Jakubikova I, Ryska A, Cap J (2016) Impact of Hashimoto’s thyroiditis, TSH levels, and anti-thyroid antibody positivity on differentiated thyroid carcinoma incidence. Endokrynol Polska 67(1):48–53. https://doi.org/10.5603/EP.a2016.0022
Selek A, Cetinarslan B, Tarkun I, Canturk Z, Ustuner B, Akyay Z (2017) Thyroid autoimmunity: is really associated with papillary thyroid carcinoma? Eur Arch Otorhinolaryngol 274(3):1677–1681. https://doi.org/10.1007/s00405-016-4414-6
Franceschi S, Preston-Martin S, Dal Maso L, Negri E, La Vecchia C, Mack WJ, McTiernan A, Kolonel L, Mark SD, Mabuchi K, Jin F, Wingren G, Galanti R, Hallquist A, Glattre E, Lund E, Levi F, Linos D, Ron E (1999) A pooled analysis of case-control studies of thyroid cancer. IV. Benign thyroid diseases. Cancer Causes Control 10(6):583–595
Staniforth JU, Erdirimanne S, Eslick GD (2016) Thyroid carcinoma in Graves’ disease: a meta-analysis. Int J Surg 27:118–125. https://doi.org/10.1016/j.ijsu.2015.11.027
Lai X, Xia Y, Zhang B, Li J, Jiang Y (2017) A meta-analysis of Hashimoto’s thyroiditis and papillary thyroid carcinoma risk. Oncotarget 8(37):62414–62424. https://doi.org/10.18632/oncotarget.18620
Resende de Paiva C, Grønhøj C, Feldt-Rasmussen U, von Buchwald C (2017) Association between Hashimoto’s thyroiditis and thyroid cancer in 64,628 patients. Front Oncol 7:53. https://doi.org/10.3389/fonc.2017.00053
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283(15):2008–2012
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Balasubramaniam S, Ron E, Gridley G, Schneider AB, Brenner AV (2012) Association between benign thyroid and endocrine disorders and subsequent risk of thyroid cancer among 4.5 million US male veterans. J Clin Endocrinol Metab 97(8):2661–2669. https://doi.org/10.1210/jc.2011-2996
Iribarren C, Haselkorn T, Tekawa IS, Friedman GD (2001) Cohort study of thyroid cancer in a San Francisco Bay area population. Int J Cancer 93(5):745–750
Meinhold CL, Ron E, Schonfeld SJ, Alexander BH, Freedman DM, Linet MS, Berrington de González A (2010) Nonradiation risk factors for thyroid cancer in the US radiologic technologists study. Am J Epidemiol 171(2):242–252. https://doi.org/10.1093/aje/kwp354
Adams MJ, Shore RE, Dozier A, Lipshultz SE, Schwartz RG, Constine LS, Pearson TA, Stovall M, Thevenet-Morrison K, Fisher SG (2010) Thyroid cancer risk 40+ years after irradiation for an enlarged thymus: an update of the Hempelmann cohort. Radiat Res 174(6):753–762. https://doi.org/10.1667/RR2181.1
Yeh NC, Chou CW, Weng SF, Yang CY, Yen FC, Lee SY, Wang JJ, Tien KJ (2013) Hyperthyroidism and thyroid cancer risk: a population-based cohort study. Exp Clin Endocrinol Diabetes 121(7):402–406. https://doi.org/10.1055/s-0033-1341474
Chen YK, Lin CL, Chang YJ, Cheng FT, Peng CL, Sung FC, Cheng YH, Kao CH (2013) Cancer risk in patients with Graves’ disease: a nationwide cohort study. Thyroid 23(7):879–884. https://doi.org/10.1089/thy.2012.0568
Liu CL, Cheng SP, Lin HW, Lai YL (2014) Risk of thyroid cancer in patients with thyroiditis: a population-based cohort study. Ann Surg Oncol 21(3):843–849. https://doi.org/10.1245/s10434-013-3363-1
Holm LE, Blomgren H, Löwhagen T (1985) Cancer risks in patients with chronic lymphocytic thyroiditis. N Engl J Med 312(10):601–604
Mellemgaard A, From G, Jørgensen T, Johansen C, Olsen JH, Perrild H (1998) Cancer risk in individuals with benign thyroid disorders. Thyroid 8(9):751–754
Shu X, Ji J, Li X, Sundquist J, Sundquist K, Hemminki K (2010) Cancer risk in patients hospitalised for Graves’ disease: a population-based cohort study in Sweden. Br J Cancer 102(9):1397–1399. https://doi.org/10.1038/sj.bjc.6605624
Divani SN, Kalodimos GP, Lioupis MA, Syrmos NC (2016) Hashimoto’s thyroiditis and papillary thyroid carcinoma. Are cytokeratin 19 and P63 proteins of any diagnostic value? Hell J Nucl Med 19(3):250–253. https://doi.org/10.1967/s002449910408
Yu Y, Zhang J, Lu G, Li T, Zhang Y, Yu N, Gao Y, Gao Y, Guo X (2016) Clinical relationship between IgG4-positive Hashimoto’s thyroiditis and papillary thyroid carcinoma. J Clin Endocrinol Metab 101(4):1516–1524. https://doi.org/10.1210/jc.2015-3783
Moazezi Z, Mahmoudi M, Yahyahpour Y, Alaleh A (2011) Risk factors of thyroid cancer in Babol, Northern Iran. Casp J Intern Med 2(1):171–177
Negro R, Valcavi R, Toulis KA (2013) Incidental thyroid cancer in toxic and nontoxic goiter: is TSH associated with malignanCy rate? Results of a meta-analysis. Endocr Pract 19(2):212–218. https://doi.org/10.4158/EP12234.OR
Rees Smith B, McLachlan SM, Furmaniak J (1988) Autoantibodies to the thyrotropin receptor. Endocr Rev 9(1):106–121
Valenti TM, Macchia E, Pisa R, Bucalo ML, Russo V, Colletti I, Compagno V, Abbadi V, Donatelli M (1999) Toxic adenoma and papillary thyroid carcinoma in a patient with Graves’ disease. J Endocrinol Investig 22(9):701–704
Belfiore A, Garofalo MR, Guiffrida D, Runello F, Filetti S, Fiumara A, Ippolito O, Vigneri R (1990) Increased aggressiveness of thyroid cancer in patients with Graves’ disease. J Clin Endocrinol Metab 70(4):830–835
Krassas GE, Poppe K, Glinoer D (2010) Thyroid function and human reproductive health. Endocr Rev 31(5):702–755. https://doi.org/10.1210/er.2009-0041
Kumar A, Klinge CM, Goldstein RE (2010) Estradiol-induced proliferation of papillary and follicular thyroid cancer cells is mediated by estrogen receptors α and β. Int J Oncol 36(5):1067–1080
Ron E, Doody MM, Becker DV, Brill AB, Curtis RE, Goldman MB, Harris BS 3rd, Hoffman DA, McConahey WM, Maxon HR, Preston-Martin S, Warschauer ME, Wong FL, Boice JD Jr (1998) Cancer mortality following treatment for adult hyperthyroidism. Cooperative Thyrotoxicosis Therapy Follow-up Study Group. JAMA 280(4):347–355
Franklyn JA, Maisonneuve P, Sheppard M, Betteridge J, Boyle P (1999) Cancer incidence and mortality after radioiodine treatment for hyperthyroidism: a population-based cohort study. Lancet 353(9170):2111–2115
Jonklaas J, Nsouli-Maktabi H, Soldin SJ (2008) Endogenous thyrotropin and triiodothyronine concentrations in individuals with thyroid cancer. Thyroid 18(9):943–952. https://doi.org/10.1089/thy.2008.0061
Haymart MR, Repplinger DJ, Leverson GE, Elson DF, Sippel RS, Jaume JC, Chen H (2008) Higher serum thyroid stimulating hormone level in thyroid nodule patients is associated with greater risks of differentiated thyroid cancer and advanced tumor stage. J Clin Endocrinol Metab 93(3):809–814
Rinaldi S, Plummer M, Biessy C, Tsilidis KK, Østergaard JN, Overvad K, Tjønneland A, Halkjaer J, Boutron-Ruault MC, Clavel-Chapelon F, Dossus L, Kaaks R, Lukanova A, Boeing H, Trichopoulou A, Lagiou P, Trichopoulos D, Palli D, Agnoli C, Tumino R, Vineis P, Panico S, Bueno-de-Mesquita HB, Peeters PH, Weiderpass E, Lund E, Quirós JR, Agudo A, Molina E, Larrañaga N, Navarro C, Ardanaz E, Manjer J, Almquist M, Sandström M, Hennings J, Khaw KT, Schmidt J, Travis RC, Byrnes G, Scalbert A, Romieu I, Gunter M, Riboli E, Franceschi S (2014) Thyroid-stimulating hormone, thyroglobulin, and thyroid hormones and risk of differentiated thyroid carcinoma: the EPIC study. J Natl Cancer Inst 106(6):dju097
Bozec A, Lassalle S, Hofman V, Ilie M, Santini J, Hofman P (2010) The thyroid gland: a crossroad in inflammation-induced carcinoma? An ongoing debate with new therapeutic potential. Curr Med Chem 17(30):3449–3461
Muzza M, Degl’Innocenti D, Colombo C, Perrino M, Ravasi E, Rossi S, Cirello V, Beck-Peccoz P, Borrello MG, Fugazzola L (2010) The tight relationship between papillary thyroid cancer, autoimmunity and inflammation: clinical and molecular studies. Clin Endocrinol (Oxf) 72(5):702–708. https://doi.org/10.1111/j.1365-2265.2009.03699.x
Arora N, Scognamiglio T, Zhu B, Fahey TJ 3rd (2008) Do benign thyroid nodules have malignant potential? An evidence-based review. World J Surg 32(7):1237–1246. https://doi.org/10.1007/s00268-008-9484-1
Funding
This work was supported by National Natural Science Foundation of China (No. 81373071) and the Project for Anhui Province Academic Technology Leader Reserve Candidates’ Academic Research Activities (2017H108).
Author information
Authors and Affiliations
Contributions
LL acquisition of data, analysis and interpretation of data, drafted the manuscript; MH completed the database searches and selected, reviewed the articles and extracted the data; XZ and QZ collection and assembly of data, and performed the data analyses; SW and FH conception and design of the study, discussed the idea of the meta-analysis, critical revision of the article for important intellectual content, submitted the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Since this is a meta-analysis, informed consent is not applicable.
Electronic supplementary material
Below is the link to the electronic supplementary material.
40618_2018_968_MOESM1_ESM.eps
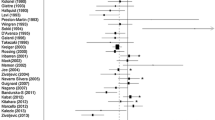
Supplementary material 1 Forest plot for subgroup analysis based on the NOS quality score. Error bars indicate 95% CI. Solid diamonds represent each record in the meta-analysis. Hollow diamonds represent pooled RR/HR (EPS 58132 kb)
40618_2018_968_MOESM2_ESM.eps
Supplementary material 2 Forest plot for subgroup analysis based on whether adjusted for multivariate. Error bars indicate 95% CI. Solid diamonds represent each record in the meta-analysis. Hollow diamonds represent pooled RR/HR (EPS 75312 kb)
40618_2018_968_MOESM5_ESM.eps
Supplementary material 5 Sensitivity analysis plot: investigated the influence of a single record on the overall SIR estimate by removing each record in each turn (EPS 38201 kb)
Rights and permissions
About this article
Cite this article
Liang, L., Zheng, XC., Hu, MJ. et al. Association of benign thyroid diseases with thyroid cancer risk: a meta-analysis of prospective observational studies. J Endocrinol Invest 42, 673–685 (2019). https://doi.org/10.1007/s40618-018-0968-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-018-0968-z