Abstract
Purpose
I. R. Iran has been considered iodine replete since 2000, but iodine nutrition of vulnerable subjects is not clear. The main goal of this study was assessment of iodine nutrition and thyroid function in pregnant Iranian women.
Methods
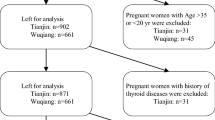
A total of 1072 pregnant women from ten provinces in the different parts of the country were recruited from November to March 2014. Median urinary iodine concentration (UIC) as the measure of iodine status and serum free T4 (FT4), thyrotropin (TSH), thyroglobulin (Tg), anti-thyroglobulin and anti-thyroid peroxidase antibodies (TgAb and TPOAb) were measured.
Results
Mean ± SD age of the cohort was 27.0 ± 7.2 years and gestational age was 20.7 ± 10.0 weeks. The median UIC for pregnant women was 87.3 μg/L, being 92.1, 86.0 and 76.8 μg/L, in three trimesters of pregnancy, respectively. Median UIC of <100, 100–149, 150–249, 250–499 and ≥500 μg/L was found in 58.4, 19.8, 16.2, 5.13 and 0.46 % of subjects, respectively. Median (IQR) values in the first, second, and third trimesters were 1.7 (0.9–2.8), 2.1 (1.5–2.9), and 2.1 (1.4–2.8) mIU/L for TSH, and 16.4 (12.21–21.13), 14.34 (12.16–19.69), and 14/07 (12.02–18.64) pmol/L for FT4, respectively. The frequency of elevated serum TSH was 9.0 % (6.6 % subclinical, 2.4 % overt hypothyroidism). The frequency of low serum TSH was 0.6 %. The frequency of positive TPOAb was 7.6 %.
Conclusions
Results of this study have clarified that despite iodine sufficiency of school children in Iran, pregnant women have moderate iodine deficiency and need iodine supplementation.

Similar content being viewed by others
References
Delange F (2000) The role of iodine in brain development. Proc Nutr Soc 59:75–79
Zimmermann MB (2009) Iodine deficiency. Endocr Rev 30:376–408
Krassas GE, Popoe K, Glinor D (2010) Thyroid function and human reproductive health. Endocr Rev 31:702–755
de Escobar GM, Ares S, Berbel P et al (2008) The changing role of maternal thyroid hormone in fetal brain development. Semin Perinatol 32:380–386
Bath SC, Walter A, Taylor A et al (2014) Iodine deficiency in pregnant women living in the South-East of the UK: the influence of diet and nutritional supplements on iodine status. Br J Nutr 111(9):1622–1631
Haddow JE, Palomaki GE, Allan WC et al (1999) Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Engl J Med 341:549–555
Teng W, Shan Z, Patil-Sisodia K, Cooper DS (2013) Hypothyroidism in pregnancy. Lancet Diabetes Endocrinol. 1:228–237
Bath SC, Steer CD, Golding J et al (2013) Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Lancet 382:331–337
Smyth PPA (1999) Variation in iodine handling during normal pregnancy. Thyroid 9:637–642
Caldwell K, Pan Y, Mortensen ME et al (2013) Iodine status in pregnant women in the United States: National Children’s Study and National Health and Nutrition Examination Survey. Thyroid. doi:10.1089/thy.2013.0012
Becker DV, Braverman LE, Delange F et al (2006) Iodine supplementation for pregnancy and lactation—United States and Canada: recommendations of the American Thyroid Association. Thyroid 16:949–951
WHO Secretariat, Andersson M, de Benoist B, Delange F, Zupan J (2007) Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation. Public Health Nutr 10:1606–1611
WHO/UNICEF (2007) Reaching optimal iodine nutrition in pregnant and lactating women and young children. Joint Statement by the WHO and the UNICEF. World Health Organization, Geneva
International Council for Control of Iodine Deficiency Disorders (2007) Iodine requirements in pregnancy and infancy. IDD Newslett 23(1):1–2
Stagnaro-Green A, Abalovich M, Alexander E et al (2012) Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid 21:1081–1125
De Groot L, Abalovich M, Alexander EK et al (2012) Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 97:2543–2565
Azizi F, Sheikholeslam R, Hedayati M et al (2002) Sustainable control of iodine deficiency in Iran: beneficial results of the implementation of the mandatory law on salt iodization. J Endocrinol Invest 25(5):409–413
Azizi F, Mehran L, Sheikholeslam R et al (2008) Sustainability of a well-monitord salt iodization program in Iran: marked reduction in goiter prevalence and eventual normalization of urinary iodine concentrations without alteration in iodine content of salt. J Endocrinol Invest 32(5):422–431
Delshad H, Amouzegar A, Mirmiran P et al (2012) Eighteen years of continuously sustained elimination of iodine deficiency in the Islamic Republic of Iran: the vitality of periodic monitoring. Thyroid 22:415–421
Dunn JT, Crutchfield HE, Gutekunst R, Dunn AD (1993) Methods for measuring iodine in urine. ICCIDD/UNICEF/WHO Publications, The Netherlands
Baloch Z, Carayon P, Conte-Devolx B et al (2003) Laboratory medicine practice guidelines. Laboratory support for the diagnosis and monitoring of thyroid disease. Thyroid 13:3–126
Mehran L, Amouzegar A, Delshad H et al (2013) Trimester-specific reference ranges for thyroid hormones in Iranian pregnant women. J Thyroid Res 65:15–17
Kut A, Kalli H, Anil C, Mousa U, Gursoy A (2015) Knowledge, attitudes and behaviors of physicians towards thyroid disorders and iodine requirements in pregnancy. J Endocrinol Invest 38(10):1057–1064
Lise Brantsæter A, Hope Abel M, Haugen M, Meltzer HM (2013) Risk of suboptimal iodine intake in pregnant Norwegian women. Nutrients 5(2):424–440
Michael Hambidge K, Krebs NF, Westcott JE et al (2014) Preconception maternal nutrition: a multi-site randomized controlled trial. BMC Pregnancy Childbirth 14:111
Bath SC, Furmidge-Owen VL, Redman CWG, Rayman MP (2015) Gestational changes in iodine status in a cohort study of pregnant women from the United Kingdom: season as an effect modifier. Am J Clin Nutr 101(6):1180–1187
Bath SC, Walter A, Taylor A et al (2014) Iodine deficiency in pregnant women living in the South-East of the UK: the influence of diet and nutritional supplements on iodine status. Br J Nutr 111(9):1622–1631
Kibirige M, Hutchison S, Owen C, Delves H (2004) Prevalence of maternal dietary iodine insufficiency in the north east of England: implications for the fetus. Arch Dis Child Fetal Neonatal Ed 89(5):436–439
Yozen F, Yoshimasa S, Minoru I (2013) Gestational changes of thyroid function and urinary iodine in thyroid antibody-negative Japanese women. Endocr J 60(9):1095–1106
Amouzegar A, Azizi F (2013) Variations of urinary iodine during the first trimester of pregnancy in an iodine-replete area. Comparison with non-pregnant women. Hormones 12(1):111-11
Smyth PPA, Hetherton AMT, Smith DF et al (1997) Maternal iodine status and thyroid volume during pregnancy: correlation with neonatal iodine intake. J Clin Endocrinol Metab 82:2840–2843
Brander L, Als C, Buess H et al (2003) Urinary iodine concentration during pregnancy in an area of unstable dietary iodine intake in Switzerland. J Endocrinol Invest 26:389–396
Stilwell G, Reynolds PJ, Parameswaran V et al (2008) The influence of gestational stage on urinary iodine excretion in pregnancy. J Clin Endocrinol Metab 93:1737–1742
Fuse Y, Ohashi T, Yamaguchi S et al (2011) Iodine status of pregnant and postpartum Japanese women: effect of iodine intake on maternal and neonatal thyroid function in an iodine-sufficient area. J Clin Endocrinol Metab 96:3846–3854
Alvarez-Pedrerol M, Guxens M, Mendez M et al (2009) Iodine levels and thyroid hormones in healthy pregnant women and birth weight of their offspring. Eur J Endocrinol 160:423–429
Luton D, Alberti C, Vuillard E et al (2011) Iodine deficiency in Northern Paris area: impact on fetal thyroid mensuration. PLoS One 6(2):e14707
Kung AWC, Lao TT, Chau MT et al (2000) Goitrogenesis during pregnancy and neonatal hypothyroxinaemia in a borderline iodine sufficient area. Clin Endocrinol (Oxf) 53:725–731
Negro R, Formoso G, Mangieri T et al (2006) Levothyroxine treatment in euthyroid pregnant women with autoimmune thyroid disease: effects on obstetrical complications. J Clin Endocrinol Metab 91:2587–2591
Moleti M, Trimarchi F, Tortorella G, Candia Longo A, Giorgianni G, Sturniolo G, Alibrandi A, Vermiglio F (2016) Effects of maternal iodine nutrition and thyroid status on cognitive development in offspring: a pilot study. Thyroid 26(2):296–305
Andersen S, Karmisholt J, Pedersen KM, Laurberg P (2008) Reliability of studies of iodine intake and recommendations for number of samples in groups and individuals. Br J Nutr 99:813–818
Korenek A, Prochazka M (2008) Iodine in early pregnancy—is there enough? Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 152(1):97–99
Raverot V, Bournaud C, Sassolas G et al (2012) Pregnant French women living in the Lyon area are iodine deficient and have elevated serum thyroglobulin concentrations. Thyroid 22:522–528
Zimmermann MB (2009) Iodine deficiency in pregnancy and the effects of maternal iodine supplementation on the offspring: a review. Am J Clin Nutr 89:668S–672S
Qian M, Wang D, Watkins WE et al (2005) The effects of iodine on intelligence in children: a meta-analysis of studies conducted in China. Asia Pac J Clin Nutr 14:32–42
Caldwell KL, Makhmudov A, Ely E, Jones RL, Wang RY (2011) Iodine Status of the U.S Population, National Health and Nutrition Examination Survey, 2005–2006 and 2007–2008. Thyroid 21:419–427
Acknowledgments
The authors wish to thank the participants for their cooperation in this study. The authors also wish to acknowledge Ms. Niloofar Shiva for critical editing of English grammar and syntax of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have any commercial associations which might create a conflict of interest in connection with this manuscript.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
No informed consent.
Rights and permissions
About this article
Cite this article
Delshad, H., Touhidi, M., Abdollahi, Z. et al. Inadequate iodine nutrition of pregnant women in an area of iodine sufficiency. J Endocrinol Invest 39, 755–762 (2016). https://doi.org/10.1007/s40618-016-0438-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-016-0438-4