Abstract
Advances in cardiology have led to improved survival among patients with congenital heart disease (CHD). Racial disparities in cardiovascular and maternal outcomes are well known and are likely to be more profound among pregnant women with CHD. Using the 2001 to 2018 National Inpatient Sample, we identified all hospitalizations for delivery among women ≥ 18 years of age with CHD. Unadjusted and adjusted between-race differences in adverse maternal cardiovascular, obstetric, and fetal events were assessed using logistic regression models. During the study period, we identified 52,711 hospitalizations for delivery among women with concomitant CHD. Of these, 66%, 11%, and 16% were White, Black, and Hispanic, respectively. Obstetric complications and fetal adverse events were higher among Blacks compared to Whites and Hispanics (44% vs. 33% vs. 37%, p < .001; 36% vs. 28% vs. 30%, p < .001), respectively. No between-race differences were observed in overall cardiovascular adverse events (27% vs. 24% vs. 23%, p < .21). However, heart failure was significantly higher among Black women (3.6% vs. 1.7% vs. 2.2%, p = 0.001). While a lower income quartile was associated with higher rates of adverse outcomes, adjustment for income did not attenuate the adverse impact of race. Black females with CHD diagnoses were more likely to experience adverse obstetric, fetal events, and heart failure compared to White and Hispanic women irrespective of their income status. Further research is needed to identify causes and devise interventions to mitigate racial disparities in the care of pregnant women with CHD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is estimated that there are around 1.4 million adults living with congenital heart disease (CHD) in the USA [1]. Advances in surgery and care of these patients have resulted in significant improvement in survival, and it is estimated that 95% of babies born with non-critical CHD and 70% born with critical CHD survive to 18 years of age [2]. The number of pregnancies in women with CHD has therefore been increasing in the last few decades and this trend is expected to continue [3]. Inadequate adaption to the hemodynamic stress of pregnancy significantly increases the risk for adverse obstetric, maternal, and fetal outcomes in pregnant women with CHD [4,5,6]. Appropriate prenatal, intranatal, and postnatal care from a multi-disciplinary pregnancy-heart team consisting of obstetricians, cardiologists, and anesthesiologists with experience in caring for mothers with CHD is critical for optimal maternal and fetal outcomes and is endorsed by multiple professional guidelines [7, 8]. Racial, ethnic, and economic disparities in health care access, care, and outcomes have been well documented in a number of cardiovascular disorders [9,10,11,12,13], and similar disparities in the care and outcomes of pregnancy are also well established [14,15,16,17,18,19]. Given the known higher risk of adverse outcomes in pregnant women with CHD, the impact of racial and socioeconomic inequities is likely to be more profound. Therefore, in this study, we explored the association of race and socioeconomic status on the cardiovascular, maternal, and fetal outcomes of pregnant women with CHD using a large nationally representative database.
Methods
All hospitalizations were abstracted from the 2001 to 2018 National (Nationwide) Inpatient Sample (NIS). The NIS is the largest publicly available all-payer inpatient care database in the USA and is part of the Healthcare Cost and Utilization Project (HCUP) family of databases sponsored by the Agency for Healthcare Research and Quality (AHRQ) [20]. When weighted, the NIS contains data on primary and secondary discharge diagnoses and procedures from more than 7 million inpatient hospitalizations annually [20]. This study was acknowledged as Not Human Subjects Research by the Institutional Review Board at Creighton University (InfoEd record number: 2002080).
We identified hospitalizations for childbirth in which the female patient was at least 18 years of age. Hospitalizations for vaginal or cesarean delivery were identified using enhanced childbirth identification methods described previously [4, 21]. Specifically, we used Medicare Severity-Diagnosis Related Groups (MS-DRG) 765, 766, 767, 768, 774, 775; and All Patients Refined-Diagnosis Related Groups (APR-DRG) 540, 541, 542, 560, ICD-9-CM codes V27.x, 650, 669.7x, ICD-10-CM codes Z37.xx, O80, O82, as well as ICD-9-PCS codes 72.xx to 74.xx and ICD-10-PCS codes 10D0- and 10E0-. We excluded any hospitalization resulting from termination of pregnancy (ICD-9-PCS: 74.91; ICD-10-PCS: 10A0-). We identified CHD using relevant ICD-9-CM codes 745.xx to 747.x and ICD-10-CM codes Q20.x to Q28.x. CHD diagnoses were stratified into severe (e.g., Tetralogy of Fallot, hypoplastic heart, and transposition); shunt only (e.g., atrial or ventricular septal defects and patent ductus arteriosus); valve only (e.g., pulmonic, aortic or mitral stenosis); shunt/valve; or other (see Supplemental Table S1 for all ICD-9/10 diagnosis and procedure codes used in this study).
Our outcomes included race-specific differences in cardiovascular events (myocardial infarction, arrhythmia, heart failure, stroke, pulmonary embolism); obstetric events (pregnancy-related hypertension, preeclampsia, eclampsia, preterm delivery, hemorrhage, placental abruption, placenta previa, prolonged pregnancy); and fetal events (malformation, distress, death/stillbirth, growth restriction). In addition, we explored whether socioeconomic status moderated between-race differences by evaluating the two-way interaction between race and median income level. Other outcomes assessed included in-hospital death and length of stay.
For each hospitalization, we extracted patient race (White, Black, Hispanic, other); age, primary payer (medicaid, private, other); income quartile; facility location/teaching status (rural, urban nonteaching, urban teaching); facility bed size (small, medium, large); and the region of the USA in which the facility was located (northeast, midwest, south, west) as well as comorbid conditions that included non-pregnancy related hypertension, heart failure, pulmonary circulation disorder, coronary arterial disease, conduction disorder, diabetes, hyperlipidemia, chronic pulmonary disease, central nervous system disease, obesity, and mental health diagnosis. Further, we calculated the Elixhauser Comorbidity Index from the 29 Elixhauser comorbidities that range from − 32 to 99, in which negative values imply a protective effect and higher positive values imply a harmful effect. The Elixhauser Comorbidity Index is a method of categorizing comorbidities of patients based on the International Classification of Diseases (ICD) diagnosis codes found in administrative data. It is derived based on several comorbid conditions such as congestive heart failure (CHF), hypertension, valvular heart disease, diabetes, obesity, cancer, pulmonary, and renal disorders. categorized dichotomously as either present or absent and has been extensively validated [22, 23].
All descriptive statistics were stratified by race with continuous variables presented as median and interquartile range, and compared using the lognormal regression model. Categorical variables are presented as percent and compared using the Rao-Scott chi-square test; Wilson confidence intervals are presented as appropriate. Unadjusted and adjusted between-race differences in adverse event rates were compared using a logistic regression model; the multivariable models included age, primary payer, income quartile, Elixhauser Comorbidity Index, CHD stratification, congestive heart failure, hypertension, pulmonary circulation disorder, and diabetes. Lognormal regression models were estimated for length of stay given skewed and heteroscedastic residuals. The functional form of continuous covariates was evaluated using restricted cubic splines with knots prespecified at the 5th, 27.5th, 50th, 72.5th, and 95th percentiles; nonlinear effects were retained as dictated by the likelihood ratio test. All analyses were conducted using SAS v. 9.4 and accounted for the NIS sampling design.
Results
From 2001 to 2018, an estimated 69.2 million hospitalizations for vaginal/cesarean delivery occurred in the USA (95% CI, 67.1 million to 71.3 million). An estimated 52,711 of these hospitalizations included a patient with a CHD diagnosis (95% CI, 50,445 to 54,977) with shunt-only lesions (atrial or ventricular septal defects and patent ductus arteriosus) being the most common CHD diagnosis (Fig. 1). The rate of cesarean section was higher with a CHD diagnosis compared to without a CHD diagnosis (37.7% vs. 31.4%, p < 0.001).
For delivery-related hospitalizations that included a patient with a CHD diagnosis, an estimated 65.7% (95% CI, 64.3 to 67.0%) were White patients; 10.5% (95% CI, 9.8 to 11.3%) were Black patients; 15.8% (95% CI, 14.7 to 17.0%) were Hispanic patients; and 8.0% (95% CI, 7.4 to 8.7%) included patients of another race. The estimated rate of cesarean section was statistically similar across races (38.2%, 37.1%, 36.8%, and 36.4% for Whites, Blacks, Hispanics, and other races, respectively; p = 0.625). Further, an estimated 70.9% of Blacks were below the median income quartile compared to 60.3% in Hispanics, 43.1% in Whites, and 38.6% in other races (Table 1) with Black and Hispanic patients tending to be younger, with higher rates of Medicaid, and more often treated in urban teaching hospitals (Table 1). White patients had lower rates of background systemic and pulmonary hypertension, heart failure, diabetes, obesity, respiratory disorders and more often received care in rural or urban non-teaching hospitals. Whites and Blacks had higher rates of mental health and neurologic disorders compared to Hispanic and other races (Table 2).
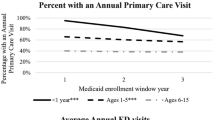
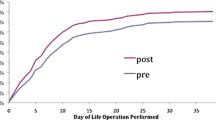
For all races, the unadjusted rates of cardiovascular, obstetric, or fetal adverse events were significantly higher for hospitalizations with CHD diagnosis (all p < 0.001; Fig. 2 and Table 3). Importantly, the pattern of between-race differences in adverse events was similar in hospitalizations with or without CHD with Black patients having the highest rates of adverse events irrespective of CHD. An estimated 24.1% (95% CI, 23.1 to 25.3%) of CHD patients had an adverse cardiovascular event. The most common cardiovascular events were thromboembolism followed by arrhythmias and CHF (Table 3). Black patients had a higher rate of adverse cardiovascular events (27.0%) compared to all other races, though this was not statistically significant (24.0% for Whites and 23.3% for Hispanics and another race, respectively, p = 0.207; Table 3 and Fig. 2). Between-race differences remained consistent in direction and statistically non-significant after adjusting for demographic and clinical characteristics (omnibus p = 0.263; Table 4 and Fig. 3). However, when considering individual adverse cardiovascular events, the rate of heart failure was statistically significant between races (p = 0.001), with the highest rate observed for hospitalizations in which the patient was Black (3.6%) and lowest when the patient was White (1.7%; see Table 3). Notably, between-race differences in adverse cardiovascular event rates were statistically similar across income quartiles (race-by-income quartile interaction p = 0.968; Fig. 4) suggesting that this adverse effect of race persists despite adjustment for income level.
An estimated 35.1% (95% CI, 34.1 to 36.2%) of hospitalizations for delivery among those with CHD had an adverse obstetric event, with statistically higher rates observed for Black patients (44.2%) compared to Whites (33.3%), Hispanics (36.7%), and other races (34.7%; p < 0.001; Table 3 and Fig. 2); these differences were retained after adjusting for demographic and clinical characteristics (Table 4 and Fig. 3). When considering individual adverse obstetric events, between-race differences were driven by pregnancy-related hypertension, pre-eclampsia, and pre-term delivery (all p < 0.001; see Table 3). Race differences in obstetric adverse event rates were statistically similar across income quartiles (race-by-income quartile interaction p = 0.798; Fig. 4) suggesting that these racial differences persist despite adjusting for income differences.
An estimated 29.5% (95% CI, 28.6 to 30.5%) of CHD hospitalizations for delivery included an adverse fetal event, with statistically higher rates observed in Blacks (35.8%) compared to Whites (28.1%; p < 0.001) and Hispanics (29.9%; p = 0.003), but not for hospitalization in which the patient was of other race (32.9%; p = 0.224; Table 3 and Fig. 2); these differences were retained after adjusting for demographic and clinical characteristics (Table 4 and Fig. 3). Between-race differences were primarily driven by fetal growth restriction and malformation (both p < 0.001; see Table 3). Race differences in fetal adverse event rates differed across income quartiles (race-by-income quartile interaction p = 0.003; see supplemental Table S2; Fig. 4), with differences in fetal adverse event rates in Black compared to all other races being larger in the highest income quartile. This suggests that income differences do not completely explain the higher adverse fetal outcomes among Blacks.
The overall in-hospital mortality rate for hospitalizations with CHD was an estimated 0.1% (95% CI, 0.1 to 0.2%), which was statistically higher compared to those without a CHD diagnosis (0.008%, 95% CI, 0.007 to 0.008%, p < 0.001); race-specific mortality rates could not be reported due to the very low observed deaths per the NIS Data Use Agreement. Although statistically significant between-race differences were observed for length of stay (p < 0.001), the median stay for all races was 2 days.
Discussion
The major findings of our study are as follows. (1) In pregnant women with CHD hospitalized for childbirth, Blacks had higher rates of obstetric and fetal adverse events. (2) While overall cardiovascular events were similar across races, Blacks had significantly higher rates of heart failure, and (3) the association between Black race and adverse events persisted even after adjustment for socioeconomic status. Health disparities are complex and the result of numerous social, environmental, biological, genetic, behavioral, healthcare delivery, and system or institutional factors. Our study demonstrated that Black patients with CHD had significantly higher rates of heart failure and adverse obstetric and fetal outcomes compared to Whites and Hispanics. This racial disparity was also noted in pregnancies without CHD, and our study findings are consistent with prior reports on race and pregnancy outcomes [6, 24,25,26,27,28,29]. However, our study highlights the fact that the adverse impact of race is much larger in magnitude in pregnant patients with CHD due to the high rate of adverse outcomes, i.e., the rate of adverse cardiovascular events was 3.0% vs. 2.6% respectively in Black vs. White patients without CHD (absolute difference of 0.4) compared to 27% vs. 24% respectively in Black vs. White pregnant women with CHD (absolute difference of 3.0%). Although the overall difference in cardiovascular events was not statistically different (likely due to the similar rates of thromboembolism which was the most common adverse event), rates of heart failure were notably higher for hospitalizations in which the patient was Black. This is not surprising given the higher rates of background hypertension in Black women. Furthermore, comorbidities like hypertension and diabetes are not just more prevalent but much less likely to be well-controlled in Black women [30, 31].
We also found that obstetric and fetal adverse events were higher in Black patients compared to White and Hispanic patients. In 2019, Schlichting et al. demonstrated the increased rates of maternal morbidity among women with CHD diagnoses [4]. Our study expands on their findings and additionally demonstrates that these adverse outcomes disproportionately affect pregnant Black women with CHD and highlight the disparities in outcomes among different racial/ethnic groups. The higher rates of maternal obstetric and fetal outcomes noted when the patient was Black could be due to a number of biologic (higher background comorbidities); socioeconomic (income, educational attainment); and/or care (healthcare access, systemic bias) factors. In our study, Blacks were younger, had a greater burden of hypertension, diabetes, more often belonged to lower-income quartiles, and carried Medicaid insurance which are concordant with prior observations [32, 33]. These are all known predictors of adverse maternal perinatal outcomes, such as postpartum hemorrhage, eclampsia, and adverse infant outcomes including preterm birth, poor fetal growth, low birth weight, and neonatal mortality [30,31,32,33,34,35,36]. Aside from this, care delivery itself might be different in hospitals that predominantly serve Black patients and this might be contributing to the adverse outcomes [25]. Similarly, the higher rates of adverse fetal outcomes in Black patients may be a direct consequence of the higher maternal obstetric events aside from all of the aforementioned biologic-, socioeconomic-, and care-related factors [29]. Preeclampsia and hypertension in pregnancy increase the risk of preterm delivery, which results in low-birth-weight infants. Higher rates of preterm delivery in Black women are likely related at least in part due to the elevated rates of pre-eclampsia [37, 38]. Our study findings are therefore consistent with prior reports on the impact of race on fetal and maternal outcomes though our study focused exclusively on women with CHD [15,16,17, 29].
A novel aspect that was explored in our study was the interaction between socioeconomic status (income quartile) and race in determining the outcomes of pregnant women with CHD. Although Black patients were more likely to belong to the lower income quartiles, there was no statistically significant interaction between race and income quartile with respect to maternal cardiovascular or obstetric outcomes. This implies that a higher income level does not negate the adverse outcomes of Black women with CHD and that these adverse outcomes may pertain to other factors which may include genetic or physiologic factors, access to healthcare/insurance, care delivery factors such as implicit or explicit bias as has been noted in other disease states such as hypertension [39,40,41,42]. Alternatively, this could be due to the fact that while the income quartile strongly correlates with socioeconomic status, it is not the sole determinant. Other factors like educational attainment, economic stability, employment, neighborhood, family, and community support may play a significant role in determining health care access and quality but are not necessarily captured by administrative databases like the NIS [43,44,45].
A number of limitations should be considered in the interpretation of our findings. First, this is a retrospective study using the NIS database which is an administrative database. Hence, coding inaccuracies can impact our sample identification and findings. Second, details of the exact CHD, lesion complexity, patient functional status, echocardiographic findings, and established predictors such as the World Health Organization (WHO) maternal risk score are unavailable and cannot be accounted for. Third, as previously mentioned, the income quartile may be a poor marker for socioeconomic status and may not capture many of the social determinants of health. Fourth, the outcomes assessed were limited to in-hospital outcomes given the nature of the NIS and we could not assess post-partum events that occur following discharge. Finally, because there are no linkages available between the records of the mother and the infant, fetal complications were only ascertained from those listed on the maternal record. As a result, the data on neonatal complications is likely incomplete. Despite these limitations, the NIS database is a well-validated dataset with stringent data accuracy checks and quality control. Our study is large and has the power to capture outcome differences that are not evident in single-center studies or smaller registries. Finally, data is ethnically and geographically diverse, includes a wide variety of centers and operators, and is likely much more representative of real-world practice and outcomes.
Conclusion
In pregnant females with CHD admitted for delivery, the Black race is associated with a higher rate of obstetric complications and adverse fetal outcomes. While overall cardiovascular event rates did not differ by race, maternal rates of heart failure were higher among Blacks. Although a greater proportion of Black women were in lower income quartiles, the adverse impact of race on these outcomes was not attenuated even in Black women who belonged to the highest income quartile. Future research should focus on the specific mediators of this higher risk among Black women and implement specific strategies to mitigate the racial/ethnic disparities in pregnant women with CHD.
Data Availability
Available for purchase from the HCUP family of databases sponsored by the Agency for Healthcare Research and Quality.
Code Availability
Provided in supplementary Table 1.
References
Gilboa SM, Devine OJ, Kucik JE, Oster ME, Riehle-Colarusso T, Nembhard WN, Xu P, Correa A, Jenkins K, Marelli AJ. Congenital heart defects in the United States. Circulation. 2016;134:101–9.
Centers for Disease Control and Prevention. Data and statistics on congenital heart defects. Available at: https://www.cdc.gov/ncbddd/heartdefects/data.html. Accessed October 15th 2023.
Bottega N, Malhamé I, Guo L, Ionescu-Ittu R, Therrien J, Marelli A. Secular trends in pregnancy rates, delivery outcomes, and related health care utilization among women with congenital heart disease. Congenit Heart Dis. 2019;14:735–44.
Schlichting LE, Insaf TZ, Zaidi AN, Lui GK, Van Zutphen AR. Maternal comorbidities and complications of delivery in pregnant women with congenital heart disease. J Am Coll Cardiol. 2019;73:2181–91.
Thompson JL, Kuklina EV, Bateman BT, Callaghan WM, James AH, Grotegut CA. Medical and obstetric outcomes among pregnant women with congenital heart disease. Obstet Gynecol. 2015;126:346–54.
Hayward RM, Foster E, Tseng ZH. Maternal and fetal outcomes of admission for delivery in women with congenital heart disease. JAMA Cardiol. 2017;2:664–71.
American College of Obstetricians and Gynecologists’ Presidential Task Force on Pregnancy and Heart Disease and Committee on Practice Bulletins - Obstetrics. ACOG Practice Bulletin No. 212: Pregnancy and Heart Disease. Obstet Gynecol 2019;133:e320–56. https://doi.org/10.1097/AOG.0000000000003243
Mehta LS, Warnes CA, Bradley E, Burton T, Economy K, Mehran R, Safdar B, Sharma G, Wood M, Valente AM, Volgman AS; American Heart Association Council on Clinical Cardiology; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; and Stroke Council Cardiovascular Considerations in Caring for Pregnant Patients: A Scientific Statement from the American Heart Association. Circulation 2020; 141:e884–903. https://doi.org/10.1161/CIR.0000000000000772
Golomb M, Redfors B, Crowley A, Smits PC, Serruys PW, von Birgelen C, Madhavan MV, Ben-Yehuda O, Mehran R, Leon MB, Stone GW. Prognostic impact of race in patients undergoing PCI. JACC Cardiovasc Interv. 2020;13:1586–95.
Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, Quyyumi AA, Taylor HA, Gulati M, Harold JG, Mieres JH, Ferdinand KC, Mensah GA, Sperling LS. Socioeconomic status and cardiovascular outcomes. Circulation. 2018;137:2166–78.
Patil S, Shah M, Patel B, Agarwal M, Ram P, Alla VM. Readmissions among patients admitted with acute decompensated heart failure based on income quartiles. Mayo Clin Proc. 2019;94:1939–50.
Breathett K, Liu WG, Allen LA, Daugherty SL, Blair IV, Jones J, Grunwald GK, Moss M, Kiser TH, Burnham E, Vandivier RW, Clark BJ, Lewis EF, Mazimba S, Battaglia C, Ho PM, Peterson PN. African Americans are less likely to receive care by a cardiologist during an intensive care unit admission for heart failure. JACC Heart Fail. 2018;6(5):413–20.
Mahajan S, Caraballo C, Lu Y, Valero-Elizondo J, Massey D, Annapureddy AR, Roy B, Riley C, Murugiah K, Onuma O, Nunez-Smith M, Forman HP, Nasir K, Herrin J, Krumholz HM. Trends in differences in health status and health care access and affordability by race and ethnicity in the United States, 1999–2018. JAMA. 2021;326:637–48.
Hoyert DL. Maternal mortality rates in the United States, 2021. NCHS Health E-Stats. 2023. https://doi.org/10.15620/cdc:124678. Accessed: October 15th 2023
Petersen EE, Davis NL, Goodman D, Cox S, Syverson C, Seed K, Shapiro-Mendoza C, Callaghan WM, Barfield W. Racial/ethnic disparities in pregnancy-related deaths—United States, 2007–2016. MMWR Morb Mortal Wkly Rep 2019;68:762–765. https://doi.org/10.15585/mmwr.mm6835a3. Accessed: October 15th 2023
Creanga AA, Berg CJ, Ko JY, Farr SL, Tong VT, Bruce FC, Callaghan WM. Maternal mortality and morbidity in the United States: where are we now? J Womens Health (Larchmt). 2014;23(1):3–9. https://doi.org/10.1089/jwh.2013.4617.
Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Race, ethnicity, and nativity differentials in pregnancy-related mortality in the United States. Obstet Gynecol. 2012;120:261–8. https://doi.org/10.1097/AOG.0b013e31825cb87a.
Nelson DB, Moniz MH, Davis MM. Population-level factors associated with maternal mortality in the United States, 1997–2012. BMC Public Health. 2018;18:1007. https://doi.org/10.1186/s12889-018-5935-2.
Tucker MJ, Berg CJ, Callaghan WM, Hsia J. The Black-White disparity in pregnancy-related mortality from 5 conditions: differences in prevalence and case-fatality rates. Am J Public Health. 2007;97:247–51. https://doi.org/10.2105/AJPH.2005.072975.
HCUP-US NIS overview. Agency for Healthcare Research and Quality Web site. https://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed February 11th, 2021.
Kuklina EV, Whiteman MK, Hillis SD, Jamieson DJ, Meikle SF, Posner SF, Marchbanks PA. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12(4):469–77.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. https://doi.org/10.1097/00005650-199801000-00004.
Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data. Med Care. 2017;55:698–705. https://doi.org/10.1097/MLR.0000000000000735.
MacDorman MF, Thoma M, Declcerq E, Howell EA. Racial and ethnic disparities in maternal mortality in the United States using enhanced vital records, 2016–2017. Am J Public Health. 2021;111(9):1673–81.
Howell EA, Egorova N, Balbierz A, Zeitlin J, Hebert PL. Black-white differences in severe maternal morbidity and site of care. Am J Obstet Gynecol. 2016;214:122.e1-122.e7. https://doi.org/10.1016/j.ajog.2015.08.019.
Petersen EE, Davis NL, Goodman D, Cox S, Mayes N, Johnston E, Syverson C, Seed K, Shapiro-Mendoza CK, Callaghan WM, Barfield W. Vital signs: pregnancy-related deaths, United States, 2011–2015, and strategies for prevention, 13 States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2019 10;68(18):423–429. https://doi.org/10.15585/mmwr.mm6818e1
Admon LK, Winkelman TNA, Zivin K, Terplan M, Mhyre JM, Dalton VK. Racial and ethnic disparities in the incidence of severe maternal morbidity in the United States, 2012–2015. Obstet Gynecol. 2018;132:1158–66. https://doi.org/10.1097/AOG.0000000000002937.
Tanaka M, Jaamaa G, Kaiser M, Hills E, Soim A, Zhu M, Shcherbatykh IY, Samelson R, Bell E, Zdeb M, McNutt LA. Racial disparity in hypertensive disorders of pregnancy in New York State: a 10-year longitudinal population-based study. Am J Public Health. 2007;97:163–70. https://doi.org/10.2105/AJPH.2005.068577.
Shen JJ, Tymkow C, MacMullen N. Disparities in maternal outcomes among four ethnic populations. Ethn Dis. 2005;15:492–7.
Bower JK, Butler BN, Bose-Brill S, Kue J, Wassel CL. Racial/ethnic differences in diabetes screening and hyperglycemia among US women after gestational diabetes. Prev Chronic Dis. 2019;16: 190144. https://doi.org/10.5888/pcd16.190144.
Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015–2016. NCHS Data Brief. 2017;289:1–8.
Artiga S, Hill L, Damico A. Health coverage by race and ethnicity, 2010–2021. Kaiser Family Foundation. Available at: https://www.kff.org/racial-equity-and-health-policy/issue-brief/health-coverage-by-race-and-ethnicity/. Accessed October 15th 2023
Johnston KJ, Hammond G, Meyers DJ, Joynt Maddox KE. Association of race and ethnicity and medicare program type with ambulatory care access and quality measures. JAMA. 2021;326:628.
Cavazos-Rehg PA, Krauss MJ, Spitznagel EL, Bommarito K, Madden T, Olsen MA, Subramaniam H, Peipert JF, Bierut LJ. Maternal age and risk of labor and delivery complications. Matern Child Health J. 2015;19:1202–11.
Londero AP, Rossetti E, Pittini C, Cagnacci A, Driul L. Maternal age and the risk of adverse pregnancy outcomes: a retrospective cohort study. BMC Pregnancy Childbirth. 2019;19:261.
Cunnington AJ. What’s so bad about teenage pregnancy? J Fam Plan Reprod Heal Care. 2001;27:36–41.
Zhang M, Wan P, Ng K, Singh K, Cheng TH, Velickovic I, Dalloul M, Wlody D. Preeclampsia among African American Pregnant women: an update on prevalence, complications, etiology, and biomarkers. Obstet Gynecol Surv. 2020;75:111–20.
Bryant A, Mhyre JM, Leffert LR, Hoban RA, Yakoob MY, Bateman BT. The association of maternal race and ethnicity and the risk of postpartum hemorrhage. Anesth Analg. 2012;115:1127–36.
Abrahamowicz AA, Ebinger J, Whelton SP, Commodore-Mensah Y, Yang E. Racial and ethnic disparities in hypertension: barriers and opportunities to improve blood pressure control. Curr Cardiol Rep. 2023Jan;25(1):17–27.
Cruz-Flores S, Rabinstein A, Biller J, Elkind MS, Griffith P, Gorelick PB, Howard G, Leira EC, Morgenstern LB, Ovbiagele B, Peterson E, Rosamond W, Trimble B, Valderrama AL; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Epidemiology and Prevention; Council on Quality of Care and Outcomes Research. Racial-ethnic disparities in stroke care: the American experience: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(7):2091–116 https://doi.org/10.1161/STR.0b013e3182213e24
Fontil V, Pacca L, Bellows BK, Khoong E, McCulloch CE, Pletcher M, Bibbins-Domingo K. Association of differences in treatment intensification, missed visits, and scheduled follow-up interval with racial or ethnic disparities in blood pressure control. JAMA Cardiol. 2022;7(2):204–12.
Banerjee S, Aaysha Cader F, Gulati M, Capers Q 4th. Racism and cardiology: a global call to action. CJC Open. 2021;3(12 Suppl):S165–73.
Darin-Mattsson A, Fors S, Kåreholt I. Different indicators of socioeconomic status and their relative importance as determinants of health in old age. Int J Equity Health. 2017;16:173. https://doi.org/10.1186/s12939-017-0670-3.
Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132(9):873–98.
Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion, Division for Heart Disease and Stroke Prevention. Socioeconomic Factors. https://www.cdc.gov/dhdsp/health_equity/socioeconomic.htm. Accessed February 4, 2024.
Acknowledgements
This research was part of the M1 Summer Research Program at Creighton University
Funding
Funding to purchase NIS data was provided by the Creighton University, Department of Medicine.
Author information
Authors and Affiliations
Contributions
John Petersen: conception, study design, interpretation of results and manuscript drafting.
Waiel Abusnina: study design, interpretation of results, manuscript drafting and critical review.
Sandeep Beesabathina: manuscript drafting, critical review and revisions.
Sai Subhakar Desu: manuscript drafting, critical review and revisions.
Ryan Walters: study design, data acquisition, statistical analysis, manuscript critical review.
Venkata Mahesh Alla: study design, data acquisition, analysis plan, manuscript drafting and critical review.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable, Institutional IRB approval.
Consent to Participate
Not applicable (deidentified administrative data).
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Petersen, J., Abusnina, W., Beesabathina, S. et al. Racial Disparities in Outcomes of Delivery and Cardiac Complications Among Pregnant Women with Congenital Heart Disease. J. Racial and Ethnic Health Disparities (2024). https://doi.org/10.1007/s40615-024-01950-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-024-01950-0