Abstract
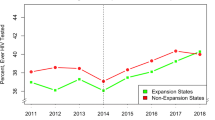
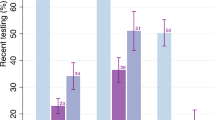
The Centers for Disease Control and Prevention recommends that individuals aged 13–64 test for HIV at least once during their lifetime. However, screening has been disproportionate among racial/ethnic populations. Using the National Health Interview Survey data (2006–2018), we examined HIV screening prevalence within racial/ethnic groups in the United States (US), and factors associated with testing among 301,191 individuals. This consisted of 195,696 White, 42,409 Black, 47,705 Hispanic and 15,381 Asian individuals. Logistic regression was used to calculate odds ratios (OR) and 95% confidence intervals (CI) to estimate the association between ever testing for HIV and demographic, socioeconomic and health-related factors. Approximately 36% of White, 61% of Black, 47% of Hispanic and 36% of Asian individuals reported ever testing for HIV. Hispanic (OR = 1.28, 95% CI [1.25–1.32]) and Black individuals (OR = 2.44, 95% CI [2.38–2.50]) had higher odds of HIV testing, whereas Asian individuals (OR = 0.74, 95% CI [0.71–0.77]) had lower odds of HIV testing compared to White individuals. Individuals who identified as males, married, between the ages of 18–26 years or greater than or equal to 50 years were less likely to ever test for HIV compared to their counterparts. Similarly, those with lower education, lower income, better self-reported health, no health professional visits or living in the midwestern US were less likely to ever test for HIV compared to their counterparts (OR range: 0.14–0.92). Understanding the factors associated with HIV testing opens opportunities to increase testing rates for all and reduce health disparities in HIV detection.

Similar content being viewed by others
Data Availability
NHIS data are publicly available.
References
U.S. Statistics. HIV.gov. https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics. Accessed 13 Nov 2022.
Status of HIV in the U.S. | Mobilizing to End the Epidemic | Strategic Priorities | Policy and Law | HIV/AIDS | CDC. Published August 6, 2021. https://www.cdc.gov/hiv/policies/strategicpriorities/mobilizing/status-of-hiv.html. Accessed 25 Jul 2023.
HIV Undetectable=Untransmittable (U=U), or Treatment as Prevention | NIH: National Institute of Allergy and Infectious Diseases. https://www.niaid.nih.gov/diseases-conditions/treatment-prevention. Accessed 14 May 2023.
Patel D, Johnson CH, Krueger A, et al. Trends in HIV Testing Among US Adults, Aged 18–64 Years, 2011–2017. Aids Behav. 2020;24(2):532–9. https://doi.org/10.1007/s10461-019-02689-0.
Lo CC, Runnels RC, Cheng TC. Racial/ethnic differences in HIV testing: An application of the health services utilization model. SAGE Open Med. 2018;6:2050312118783414. https://doi.org/10.1177/2050312118783414.
Hill MJ, Cardenas-Turanzas M, Prater S, Campbell JW, McNeese M. Racial and sex disparities in HIV screening outcomes within emergency departments of Harris County, Texas. J Am Coll Emerg Phys Open. 2020;1(4):476–83. https://doi.org/10.1002/emp2.12046.
Volume 33 | HIV Surveillance | Reports | Resource Library | HIV/AIDS | CDC. Published May 24, 2022. https://www.cdc.gov/hiv/library/reports/hiv-surveillance/vol-33/index.html. Accessed 13 Nov 2022.
Lee JJ, Zhou Y. Facilitators and barriers to HIV testing among Asian individuals in the United States: a systematic review. AIDS Care. 2019;31(2):141–52. https://doi.org/10.1080/09540121.2018.1533231.
Ebrahim SH, Anderson JE, Weidle P, Purcell DW. Race/ethnic disparities in HIV testing and knowledge about treatment for HIV/AIDS: United States, 2001. AIDS Patient Care STDS. 2004;18(1):27–33. https://doi.org/10.1089/108729104322740893.
Benbow ND, Aaby DA, Rosenberg ES, Brown CH. County-level factors affecting Latino HIV disparities in the United States. PLoS One. 2020;15(8):e0237269. https://doi.org/10.1371/journal.pone.0237269.
Murdock CJ, Laurencin L, Christensen DM, Laurencin CT. HIV/AIDS and the African-American Community 2018: A Decade Call To Action. J Racial Ethn Health Disparities. 2018;5(3):449–58. https://doi.org/10.1007/s40615-018-0491-0.
Ostermann J, Kumar V, Pence BW, Whetten K. Trends in HIV Testing and Differences Between Planned and Actual Testing in the United States, 2000–2005. Arch Intern Med. 2007;167(19):2128–35. https://doi.org/10.1001/archinte.167.19.2128.
HIV Incidence | HIV in the United States by Region | Statistics Overview | Statistics Center | HIV/AIDS | CDC. https://www.cdc.gov/hiv/statistics/overview/incidence.html. Accessed 14 May 2023.
HIV Screening Coverage. https://www.medicare.gov/coverage/hiv-screenings Accessed 14 May 2023.
State Medicaid Coverage of Routine HIV Screening. KFF. Published February 25, 2014. https://www.kff.org/hivaids/fact-sheet/state-medicaid-coverage-of-routine-hiv-screening/. Accessed 14 May 2023.
Dovel K, Balakasi K, Gupta S, et al. Frequency of visits to health facilities and HIV services offered to men. Malawi Bull World Health Organ. 2021;99(9):618–26. https://doi.org/10.2471/BLT.20.278994.
NHIS - National Health Interview Survey. https://www.cdc.gov/nchs/nhis/index.htm. Accessed 13 Nov 2022.
NHIS - 2018 Data Release. Published June 14, 2021. https://www.cdc.gov/nchs/nhis/nhis_2018_data_release.htm. Accessed 13 Nov 2022.
Ruggles, Steven, Flood, Sarah, Goeken, Ronald, Schouweiler, Megan, Sobek, Matthew. IPUMS USA: Version 12.0. Published online 2022. https://doi.org/10.18128/D010.V12.0
IPUMS NHIS. https://nhis.ipums.org/nhis/userNotes_weights.shtml. Accessed 13 Nov 2022.
Final Rule: Removal of HIV Entry Ban. Published March 22, 2021. https://www.cdc.gov/immigrantrefugeehealth/laws-regs/hiv-ban-removal/final-rule.html. Accessed 15 May 2023.
R Studio Team. RStudio: Integrated Development Environment for R. RStudio, PBC, Boston, MA: R Studio. http://www.rstudio.com/. Published 2022. Accessed 13 Nov 2022.
HIV Statistics Impact on Racial and Ethnic Minorities. HIV.gov. https://www.hiv.gov/hiv-basics/overview/data-and-trends/impact-on-racial-and-ethnic-minorities. Accessed 15 Jul 2023.
National HIV/AIDS Strategy. HIV gov. 2022-2025. https://www.hiv.gov/federal-response/national-hiv-aids-strategy/national-hiv-aids-strategy-2022-2025. Accessed 26 Jul 2023.
French RS, Bonell C, Wellings K, Weatherburn P. An exploratory review of HIV prevention mass media campaigns targeting men who have sex with men. BMC Public Health. 2014;14:616.
Maulsby C, Millett G, Lindsey K, et al. A systematic review of HIV interventions for Black men who have sex with men (MSM). BMC Public Health. 2013;13:625.
Solorio R, Norton-Shelpuk P, Forehand M, et al. Tu Amigo Pepe: Evaluation of a multi-media marketing campaign that targets young Latino immigrant MSM with HIV testing messages. AIDS Behav. 2016;20:1973–88.
Adults Who Report Ever Receiving an HIV Test by Race/Ethnicity. KFF. Published October 31, 2022. https://www.kff.org/other/state-indicator/adults-who-report-ever-receiving-an-hiv-test-by-race-ethnicity/. Accessed 15 Jul 2023.
Kim B, Aronowitz T. Invisible Minority: HIV Prevention Health Policy for the Asian American Population. Policy Polit Nurs Pract. 2019;20(1):41–9. https://doi.org/10.1177/1527154419828843.
Opt-Out| Pregnant Women, Infants, and Children | Gender | HIV by Group | HIV/AIDS | CDC. Published February 25, 2021. Accessed May 15, 2023. https://www.cdc.gov/hiv/group/gender/pregnantwomen/opt-out.html
Hsu KK, Rakhmanina NY. Adolescents and Young Adults: The Pediatrician’s Role in HIV Testing and Pre- and Postexposure HIV Prophylaxis. Pediatrics. 2022;149(1):e2021055207. https://doi.org/10.1542/peds.2021-055207.
PrEP privacy on the ACA: Young adults are forgoing the HIV-prevention drug to keep their sex lives private from their parents. https://slate.com/human-interest/2019/04/prep-privacy-parent-insurance-aca-hiv-prevention.html. Accessed 15 May 2023.
Youssef E, Wright J, Delpech V, et al. Factors associated with testing for HIV in people aged ≥50 years: a qualitative study. BMC Public Health. 2018;18(1):1204. https://doi.org/10.1186/s12889-018-6118-x.
2021 | Annual HIV Testing Report | Reports | Resource Library | HIV/AIDS | CDC. Published March 31, 2023. https://www.cdc.gov/hiv/library/reports/testing/2021/index.html. Accessed 15 May 2023.
Lo CC, Cheng TC. The role of social structural factors in treatment of mental health disorder. J Ment Health. 2012;21(5):430–8. https://doi.org/10.3109/09638237.2012.664303.
Song L, Wang Y, Chen B, Yang T, Zhang W, Wang Y. The Association between Health Insurance and All-Cause, Cardiovascular Disease, Cancer and Cause-Specific Mortality: A Prospective Cohort Study. Int J Environ Res Public Health. 2020;17(5):1525. https://doi.org/10.3390/ijerph17051525.
Corwin T, Ozieh MN, Garacci E, Walker RJ, Egede LE. Association of Social Risk Domains With Poor Cardiovascular Risk Factor Control in US Adults With Diabetes, From 2006 to 2016. JAMA Network Open. 2022;5(9):e2230853. https://doi.org/10.1001/jamanetworkopen.2022.30853.
Schmier JK, Halpern MT. Patient recall and recall bias of health state and health status. Expert Rev Pharmacoecon Outcomes Res. 2004;4(2):159–63. https://doi.org/10.1586/14737167.4.2.159.
Muyunda B, Musonda P, Mee P, Todd J, Michelo C. Educational Attainment as a Predictor of HIV Testing Uptake Among Women of Child-Bearing Age: Analysis of 2014 Demographic and Health Survey in Zambia. Front Public Health. 2018;6:192. https://doi.org/10.3389/fpubh.2018.00192.
Peytremann A, Senn N, Mueller Y. Are healthcare workers more likely than the general population to consult in primary care for an influenza-like illness? Results from a case-control study. Influenza Other Respir Viruses. 2020;14(5):524–9. https://doi.org/10.1111/irv.12750.
Obiebi IP, Moeteke NS, Eze GU, Umuago IJ. How mindful of their own health are healthcare professionals? perception and practice of personnel in a tertiary hospital in Nigeria. Ghana Med J. 2020;54(4):215–24. https://doi.org/10.4314/gmj.v54i4.3.
Baumann KE, Hemmige V, Kallen MA, Street RL, Giordano TP, Arya M. Whether Patients Want It or Not, Physician Recommendations Will Convince Them to Accept HIV Testing. J Int Assoc Provid AIDS Care. 2018;17:2325957417752258. https://doi.org/10.1177/2325957417752258.
Hossain SJ, MtJ Ferdousi, Siddique MdAB, Tipu SMMU, Qayyum MA, Laskar MS. Self-reported health problems, health care seeking behaviour and cost coping mechanism of older people: Implication for primary health care delivery in rural Bangladesh. J Family Med Prim Care. 2019;8(3):1209–15. https://doi.org/10.4103/jfmpc.jfmpc_162_18.
Ng’ambi W, Mangal T, Phillips A, et al. Factors associated with healthcare seeking behaviour for children in Malawi: 2016. Trop Med Int Health. 2020;25(12):1486–95. https://doi.org/10.1111/tmi.13499.
Trepka MJ, Fennie KP, Sheehan DM, Lutfi K, Maddox L, Lieb S. Late HIV Diagnosis: Differences by Rural/Urban Residence, Florida, 2007–2011. AIDS Patient Care STDS. 2014;28(4):188–97. https://doi.org/10.1089/apc.2013.0362.
Ward BW, Schiller JS, Freeman G, Clarke TC. Early release of selected estimates based on data from the January– March 2014 National Health Interview Survey. National Center for Health Statistics. September 2014. Available from: https://www.cdc.gov/nchs/nhis.htm.
Acknowledgements
The authors would like to thank the Stanford Center for Asian Health Research and Education and the Chi-Li Pao Foundation for project and conference support.
Author information
Authors and Affiliations
Contributions
Armaan Jamal: Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing—original draft, Writing— -review & editing. Malathi Srinivasan: Conceptualization, Methodology, Resources, Supervision, Writing—review & editing. Gloria Kim: Conceptualization, Methodology, Resources, Supervision, Writing—review & editing. Andrew Nevins: Conceptualization, Methodology, Supervision, Writing—review & editing. Sanah Vohra: Conceptualization, Methodology, Visualization, Resources, Supervision, Writing—original draft, Writing—review & editing.
Corresponding author
Ethics declarations
Conflicts of Interest
All authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jamal, A., Srinivasan, M., Kim, G. et al. Factors associated with HIV Testing within the National Health Interview Survey (2006–2018). J. Racial and Ethnic Health Disparities (2023). https://doi.org/10.1007/s40615-023-01728-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-023-01728-w