Abstract
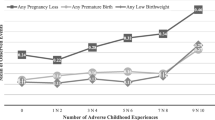
Racial and ethnic disparities in birth outcomes have persisted in the United States for decades, though the causes remain poorly understood. The life course perspective posits that poorer outcomes of Black birthing people stem from heightened exposure to stressors early in life and cumulative exposure to stressors over time. Despite its prominence, this perspective has seldom been investigated empirically. We analyzed longitudinal data gathered from 1319 women in low-income households in Wisconsin who received perinatal home visiting services. Variable- and person-centered analyses were performed to assess whether 15 adverse childhood experiences (ACEs) and 10 adverse adult experiences (AAEs) were associated, alone and in combination, with pregnancy loss, preterm birth, and low birth weight among Hispanic (i.e., Latinx) and non-Hispanic Black and White participants. As expected, there were disparities in preterm birth and low birth weight, and both ACEs and AAEs were linked to poorer pregnancy and birth outcomes. Unexpectedly, bivariate and multivariate analyses showed that the associated effects of ACEs and AAEs were most robust for non-Hispanic White women. A latent class analysis produced four patterns of life course adversity, and multigroup latent class analyses confirmed that, compared to White women, higher-adversity class assignments were associated with less robust effects for Hispanic women, and even less robust effects for Black women. We discuss interpretations of the paradoxical findings, including the possibility that alternative sources of stress such as interpersonal and structural racism may better account for the reproductive disparities that disproportionately affect Black birthing people.

Similar content being viewed by others
Data Availability
The authors do not have permission to share the source data.
Code Availability
The authors may provide syntax upon request.
References
Alhusen JL, Bower KM, Epstein E, Sharps P. Racial discrimination and adverse birth outcomes: an integrative review. Journal of Midwifery & Women’s Health. 2016;61(6):707–20.
Almeida J, Bécares L, Erbetta K, Bettegowda VR, Ahluwalia IB. Racial/ethnic inequities in low birth weight and PTB: the role of multiple forms of stress. Matern Child Health J. 2018;22(8):1154–63.
Alvidrez J, Castille D, Laude-Sharp M, Rosario A, Tabor D. The national institute on minority health and health disparities research framework. Am J Public Health. 2019;109(S1):S16–20.
Beam AL, Fried I, Palmer N, Agniel D, Brat G, Fox K, … & Armstrong J. Estimates of healthcare spending for preterm and low-birthweight infants in a commercially insured population: 2008–2016. J Perinatol. 2020;40(7), 1091–1099
Bellerose M, Rodriguez M, Vivier PM. A systematic review of the qualitative literature on barriers to high-quality prenatal and postpartum care among low-income women. Health Serv Res. 2022;57(4):775–85.
Bernard DL, Calhoun CD, Banks DE, Halliday CA, Hughes-Halbert C, Danielson CK. Making the “C-ACE” for a culturally-informed adverse childhood experiences framework to understand the pervasive mental health impact of racism on Black youth. J Child Adolesc Trauma. 2021;14:233–47.
Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med. 2010;39(3):263–72.
Braveman P, Dominguez TP, Burke W, Dolan SM, Stevenson DK, Jackson FM, Collins JW, Driscoll DA, Haley T, Acker J, Shaw GM, McCabe ERB, Hay WW, Thornburg K, Acevedo-Garcia D, Cordero JF, Wise PH, Legaz G, Rashied-Henry K, … Waddell L. Explaining the Black-White disparity in PTB: a consensus statement from a multi-disciplinary scientific work group convened by the March of Dimes. Front Reprod Health. 2021;3
Brown CC, Moore JE, Tilford JM. Rates of preterm birth and low birthweight: an analysis of racial and ethnic populations: Study examines preterm birth and low birthweight rates among racial and ethnic populations. Health Aff. 2023;42(2):261–7.
Burris HH, Hacker MR. Birth outcome racial disparities: a result of intersecting social and environmental factors. In Seminars Perinatol. 2017; (Vol. 41, No. 6, pp. 360–366). WB Saunders
Buultjens M, Farouque A, Karimi L, Whitby L, Milgrom J, Erbas B. The contribution of group prenatal care to maternal psychological health outcomes: a systematic review. Women and Birth. 2021;34(6):e631–42.
Chambers BD, Baer RJ, McLemore MR, Jelliffe-Pawlowski LL. Using index of concentration at the extremes as indicators of structural racism to evaluate the association with PTB and infant mortality—California, 2011–2012. J Urban Health. 2019;96(2):159–70.
Choi C, Mersky JP, Janczewski CE, Lee CTP, Davies WH, Lang AC. Validity of an expanded assessment of adverse childhood experiences: a replication study. Child Youth Serv Rev. 2020;117:105216.
Christiaens I, Hegadoren K, Olson DM. Adverse childhood experiences are associated with spontaneous PTB: a case–control study. BMC Med. 2015;13(1):1–9.
Christian LM. Psychoneuroimmunology in pregnancy: immune pathways linking stress with maternal health, adverse birth outcomes, and fetal development. Neurosci Biobehav Rev. 2012;36(1):350–61.
Coomarasamy, A., Dhillon-Smith, R. K., Papadopoulou, A., Al-Memar, M., Brewin, J., Abrahams, V. M., … & Quenby, S. Recurrent miscarriage: evidence to accelerate action. Lancet. 2021;397(10285), 1675–1682.
Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, … & Fein JA. Adverse childhood experiences: expanding the concept of adversity. Am J Prevent Med. 2015;49(3), 354–361.
Culhane JF, Goldenberg RL. Racial disparities in preterm birth. In Seminars Perinatol. 2011;(Vol. 35, No. 4, pp. 234–239). WB Saunders.
Cutts DB, Coleman S, Black MM, Chilton MM, Cook JT, de Cuba SE, … & Frank DA. Homelessness during pregnancy: a unique, time-dependent risk factor of birth outcomes. Maternal Child Health J. 2015;19(6), 1276–1283.
Deichen Hansen ME. Predictors of preterm birth and low birth weight: a person-centered approach. SSM-Population Health. 2021;15:100897.
Dubay L, Hill I, Garrett B, Blavin F, Johnston E, Howell E, … & Cross-Barnet C. Improving birth outcomes and lowering costs for women on Medicaid: impacts of ‘Strong Start For Mothers And Newborns’. Health Affairs. 2020;39(6), 1042–1050.
Ely DM, Driscoll AK. Infant mortality in the United States, 2019: data from the period linked birth/infant death file. Natl Vital Stat Rep: From Centers Dis Control Prevent, Natl Center Health Stat, Natl Vital Stat Syst. 2021;70(14):1–18.
Emanuel EJ, Gudbranson E, Van Parys J, Gørtz M, Helgeland J, Skinner J. Comparing health outcomes of privileged US citizens with those of average residents of other developed countries. JAMA Intern Med. 2021;181(3):339–44.
Evans CR, Williams DR, Onnela JP, Subramanian SV. A multilevel approach to modeling health inequalities at the intersection of multiple social identities. Soc Sci Med. 2018;203:64–73.
Fernandes-Alcantara AL. Maternal, infant, and early childhood home visiting (MIECHV) program: background and funding. Congression Res Service. 2018;18:1–51.
Fine A, Kotelchuck M Rethinking MCH: the life course model as an organizing framework. US Department of Health and Human Services, Health Resources and Services Administration. Maternal Child Health Bureau. 2010;1–20.
Finkelhor D, Shattuck A, Turner H, Hamby S. A revised inventory of adverse childhood experiences. Child Abuse Negl. 2015;48:13–21.
Foney DM, DiBari J, Li R, Kogan M. Life course investments at the Maternal and Child Health Bureau. Pediatrics. 2022;149(Supplement 5):e2021053509B.
Goin DE, Gomez AM, Farkas K, Zimmerman S, Matthay EC, Ahern J. Exposure to community homicide during pregnancy and adverse birth outcomes: a within-community matched design. Epidemiology (Cambridge, Mass). 2019;30(5):713–22.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of PTB. The Lancet. 2008;371(9606):75–84.
Groos M, Wallace M, Hardeman R, Theall KP. Measuring inequity: a systematic review of methods used to quantify structural racism. J Health Disparities Res Pract. 2018;11(2):13.
Hailu EM, Maddali SR, Snowden JM, Carmichael SL, Mujahid MS. Structural racism and adverse maternal health outcomes: a systematic review. Health Place. 2022;78:102923.
Hardeman RR, Murphy KA, Karbeah JM, Kozhimannil KB. Naming institutionalized racism in public health literature: a systematic literature review. Public Health Rep. 2018;133(3):240–9.
Hawes DJ, Lechowicz M, Roach A, Fisher C, Doyle FL, Noble S, Dadds MR. Capturing the developmental timing of adverse childhood experiences: the Adverse Life Experiences Scale. Am Psychol. 2021;76(2):253–67.
Hill A, Pallitto C, McCleary-Sills J, Garcia-Moreno C. A systematic review and meta-analysis of intimate partner violence during pregnancy and selected birth outcomes. Int J Gynecol Obstet. 2016;133(3):269–76.
Hodnett ED, Gates S, Hofmeyr GJ, & Sakala C. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2013;7.
Issel LM, Forrestal SG, Slaughter J, Wiencrot A, Handler A. A review of prenatal home-visiting effectiveness for improving birth outcomes. J Obstet Gynecol Neonatal Nurs. 2011;40(2):157–65.
Jacobsson B, Simpson JL, FIGO Working Group for Preterm Birth, Jacobsson B, Simpson JL, Norman J, ... & Shennan A. FIGO good practice recommendations for reducing preterm birth and improving child outcomes. Int J Gynecol Obstet. 2021; 155(1), 1-4.
Janevic T, Zeitlin J, Egorova NN, Hebert P, Balbierz A, Stroustrup AM, Howell EA. Racial and economic neighborhood segregation, site of delivery, and morbidity and mortality in neonates born very preterm. J Pediatr. 2021;235:116–23.
Jeffers NK, Berger BO, Marea CX, Gemmill A. Investigating the impact of structural racism on black birthing people-associations between racialized economic segregation, incarceration inequality, and severe maternal morbidity. Soc Sci Med. 2023;317:115622.
Jones NL, Gilman SE, Cheng TL, Drury SS, Hill CV, Geronimus AT. Life course approaches to the causes of health disparities. Am J Public Health. 2019;109(S1):S48–55.
Kennedy-Moulton K, Miller S, Persson P, Rossin-Slater M, Wherry L, & Aldana G Maternal and infant health inequality: new evidence from linked administrative data (No. w30693). National Bureau of Economic Research. 2022.
Kozhimannil KB, Hardeman RR, Alarid-Escudero F, Vogelsang CA, Blauer-Peterson C, Howell EA. Modeling the cost-effectiveness of doula care associated with reductions in preterm birth and cesarean delivery. Birth. 2016;43(1):20–7.
Kuzawa CW, Sweet E. Epigenetics and the embodiment of race: developmental origins of US racial disparities in cardiovascular health. Am J Human Biol: Off J Human Biol Assoc. 2009;21(1):2–15.
Larrabee Sonderlund A, Schoenthaler A, Thilsing T. The association between maternal experiences of interpersonal discrimination and adverse birth outcomes: a systematic review of the evidence. Int J Environ Res Public Health. 2021;18(4):1465.
Leeners B, Rath W, Block E, Görres G, Tschudin S. Risk factors for unfavorable pregnancy outcome in women with adverse childhood experiences. J Perinat Med. 2014;42(2):171–8.
Leifheit KM, Schwartz GL, Pollack CE, Edin KJ, Black MM, Jennings JM, Althoff KN. Severe housing insecurity during pregnancy: association with adverse birth and infant outcomes. Int J Environ Res Public Health. 2020;17(22):8659.
Leimert KB, Olson DM. Racial disparities in pregnancy outcomes: genetics, epigenetics, and allostatic load. Curr Opin Physio. 2020;13:155–65.
Liu Y, Wang Y, Wu Y, Chen X, Bai J. Effectiveness of the CenteringPregnancy program on maternal and birth outcomes: a systematic review and meta-analysis. Int J Nurs Stud. 2021;120:103981.
Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7(1):13–30.
Lu MC, Kotelchuck M, Hogan V, Jones L, Wright K, Halfon N. Closing the Black-White gap in birth outcomes: a life-course approach. Ethnicity Dis. 2010;20(1 0 2):S2.
Maguire-Jack K, Lanier P, Lombardi B. Investigating racial differences in clusters of adverse childhood experiences. Am J Orthopsych. 2020;90(1):106–20.
Martin CL, Ghastine L, Lodge EK, Dhingra R, Ward-Caviness CK. Understanding health inequalities Through the lens of social epigenetics. Annu Rev Public Health. 2022;43(1):235–54.
Masho SW, Cha S, Chapman DA, Chelmow D. Understanding the role of violence as a social determinant of PTB. Am J Obstet Gynecol. 2017;216(2):183-e1.
Mehra R, Boyd LM, Ickovics JR. Racial residential segregation and adverse birth outcomes: a systematic review and meta-analysis. Soc Sci Med. 2017;191:237–50.
Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of adverse childhood experiences from the 2011–2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatr. 2018;172(11):1038–44.
Mersky JP, Janczewski CE, Topitzes J. Rethinking the measurement of adversity: Moving toward second-generation research on adverse childhood experiences. Child Maltreat. 2017;22(1):58–68.
Mersky JP, Janczewski CE. Racial and ethnic differences in the prevalence of adverse childhood experiences: Findings from a low-income sample of US women. Child Abuse and Neglect. 2018;76:480–7.
Mersky JP, Janczewski CE, Nitkowski JC. Poor mental health among low-income women in the US: The rolesof adverse childhood and adult experiences. Soc Sci Med. 2018;206:14–21.
Mersky JP, Plummer Lee C. Adverse childhood experiences and poor birth outcomes in a diverse, low-income sample. BMC Preg Child. 2019;19(387):1–7.
Mersky JP, Choi C, Lee CP, Janczewski CE. Disparities in adverse childhood experiences by race/ethnicity, gender, and economic status: Intersectional analysis of a nationally representative sample. Child Abuse & Neglect. 2021;117:105066.
Mersky JP, Plummer Lee C, Janczewski CE. Toward the assessment of adverse adult experiences: An initial validation study of the Adult Experiences Survey. Psychol Trauma: Theory, Res Prac Pol. 2021;13(5):528–36.
Mersky JP, Plummer Lee C, Janczewski CE. Adverse adult experiences and health outcomes: Racial and ethnic differences in a low-income sample. Stress & Health. 2023 (Advance online publication). https://doi.org/10.1002/smi.3212
Moniz MH, Low LK, Stout MJ. Intensive nurse home visiting program and adverse birth outcomes. JAMA. 2022;328(1):23–4.
Mukherjee S, Velez Edwards DR, Baird DD, Savitz DA, Hartmann KE. Risk of miscarriage among black women and white women in a US prospective cohort study. Am J Epidemiol. 2013;177(11):1271–8.
Muthén LK and Muthén BO (1998–2017). Mplus User’s Guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén
Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model. 2007;14(4):535–69.
Osterman MJK, Hamilton BE, Martin JA, Driscoll AK, Valenzuela CP. Births: Final data for 2020. National Vital Statistics Reports. 2022;70(17), 1–50. https://www.cdc.gov/nchs/data/nvsr/nvsr70/nvsr70-17.pdf
Osypuk TL, Slaughter-Acey JC, Kehm RD, Misra DP. Life-course social mobility and reduced risk of adverse birth outcomes. Am J Prev Med. 2016;51(6):975–82.
Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, ... & Gee G. Racism as a determinant of health: a systematic review and meta-analysis. PloS one. 2015;10(9), e0138511
Petrou S, Yiu HH, Kwon J. Economic consequences of PTB: a systematic review of the recent literature (2009–2017). Arch Dis Child. 2019;104(5):456–65.
Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012;98(5):1103–11.
Quenby S, Gallos ID, Dhillon-Smith RK, Podesek M, Stephenson MD, Fisher J, ... & Coomarasamy A. Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet. 2021;397(10285), 1658–1667
Reno R, Hyder A. The evidence base for social determinants of health as risk factors for infant mortality: a systematic scoping review. J Health Care Poor Underserved. 2018;29(4):1188–208.
Rossen LM, Ahrens KA, Branum AM. Trends in risk of pregnancy loss among US women, 1990–2011. Paediatr Perinat Epidemiol. 2018;32(1):19–29.
Schaaf JM, Liem SM, Mol BWJ, Abu-Hanna A, Ravelli AC. Ethnic and racial disparities in the risk of PTB: a systematic review and meta-analysis. Am J Perinatol. 2013;30(06):433–50.
Shah PS, Shah J. Maternal exposure to domestic violence and pregnancy and birth outcomes: a systematic review and meta-analyses. J Womens Health. 2010;19(11):2017–31.
Sheikh J, Allotey J, Kew T, Fernández-Félix BM, Zamora J, Khalil A, ... & van Gelder M. Effects of race and ethnicity on perinatal outcomes in high-income and upper-middle-income countries: an individual participant data meta-analysis of 2 198 655 pregnancies. Lancet. 2022;400(10368), 2049–2062.
Singh GK, Stella MY. Infant mortality in the United States, 1915–2017: large social inequalities have persisted for over a century. Int J Maternal Child Health AIDS. 2019;8(1):19.
Slopen N, Shonkoff JP, Albert MA, Yoshikawa H, Jacobs A, Stoltz R, Williams DR. Racial disparities in child adversity in the US: interactions with family immigration history and income. Am J Prev Med. 2016;50(1):47–56.
Staneva A, Bogossian F, Pritchard M, Wittkowski A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on PTB: a systematic review. Women and Birth. 2015;28(3):179–93.
Strutz KL, Hogan VK, Siega-Riz AM, Suchindran CM, Halpern CT, Hussey JM. Preconception stress, birth weight, and birth weight disparities among US women. Am J Public Health. 2014;104(8):e125–32.
Stumbo SP, Yarborough BJH, Paulson RI, Green CA. The impact of adverse child and adult experiences on recovery from serious mental illness. Psychiatr Rehabil J. 2015;38(4):320.
Su D, Samson K, Hanson C, Berry ALA, Li Y, Shi L, Zhang D. Racial and ethnic disparities in birth outcomes: a decomposition analysis of contributing factors. Prevent Med Rep. 2021;23:101456.
Testa A, Jackson DB. Maternal adverse childhood experiences, paternal involvement, and infant health. J Pediatr. 2021;236:157–63.
van Daalen KR, Kaiser J, Kebede S, Cipriano G, Maimouni H, Olumese E, ... & Oliver-Williams C. Racial discrimination and adverse pregnancy outcomes: a systematic review and meta-analysis. BMJ Glob Health. 2022;7(8), e009227
van der Feltz-Cornelis C, Bakker M, van der Sluijs JVE. Four clinical profiles of adult outpatients with somatic Symptom Disorders and Related Disorders (SSRD) A latent class analysis. J Psychosom Res. 2022;156:110775.
Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40(1):105–25.
Wolke D, Johnson S, Mendonça M. The life course consequences of very PTB. Ann Rev Develop Psychol. 2019;1:69–92.
World Health Organization. WHO recommendations on interventions to improve preterm birth outcomes: highlights and key messages from the World Health Organization's 2015 global recommendations (No. WHO/RHR/15.16). World Health Organization. 2015
Zhang G, Srivastava A, Bacelis J, Juodakis J, Jacobsson B, Muglia LJ. Genetic studies of gestational duration and PTB. Best Pract Res Clin Obstet Gynaecol. 2018;52:33–47.
Zhang L, Mersky JP, Lee CP. Intergenerational pathways linking mothers’ adverse childhood experiences and children’s social-emotional problems. Child Maltreat. 2023;28(1):107–18.
Zuccarello D, Sorrentino U, Brasson V, Marin L, Piccolo C, Capalbo A, ... & Cassina M. Epigenetics of pregnancy: looking beyond the DNA code. J Assist Reprod Gene. 2022;39(4), 801–816
Funding
This work was supported by grants from the U.S. Department of Health and Human Services, Health Resources Services Administration (X10MC43618; X10MC33618).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by JM and CPL. The first draft of the manuscript was written by JM and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board (FWA00006171) of the University of Wisconsin-Milwaukee (14.286; 3/27/14).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent to Publish
Not applicable. Study participants were informed at the time of consent that their data would be deidentified and used for research.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mersky, J.P., Jeffers, N.K., Lee, C.P. et al. Linking Adverse Experiences to Pregnancy and Birth Outcomes: A Life Course Analysis of Racial and Ethnic Disparities Among Low-Income Women. J. Racial and Ethnic Health Disparities (2023). https://doi.org/10.1007/s40615-023-01647-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-023-01647-w