Abstract
Background
Previous literature has demonstrated adverse patient outcomes associated with racial/ethnic disparities in health services. Because patients/parents and providers care about the duration of anesthesia, this study focuses on this outcome.
Objectives
To determine the association between race/ethnicity and duration under anesthesia.
Research Design
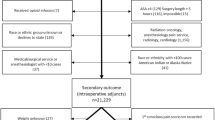
In this retrospective cohort study of data from the Multicenter Perioperative Outcomes Group, White non-Latino was the reference and was compared with Black non-Latino children, Latino, Asian, Native American, Other, and “Unknown” race children.
Subjects
Children aged 3 to 17 years.
Outcomes
Induction duration (primary outcome), procedure-end duration, and total duration under anesthesia (secondary outcomes).
Results
Of 37,596 eligible cases, 9,610 cases with complete data were analyzed. The sample consisted of 6,894 White non-Latino patients, 1,021 Black non-Latino patients, 50 Latino patients, 287 Asian patients, 26 Native American patients, 57 “Other” race patients, and 1,275 patients of “Unknown” race. The mean induction time was 11.9 min (SD 5.6 min). In adjusted analysis, Black non-Latino patients had 5% longer induction and procedure-end durations than White non-Latino children (exponentiated beta coefficient [Exp (β)] 1.05, 95% CI: 1.02–1.08, p < 0.01 and Exp (β) 1.08, 95% CI 1.04–1.13, p < 0.01 respectively).
Conclusions
White non-Latino children had shorter induction and procedure-end durations than Black children. The differences in induction and procedure-end time were small but may be meaningful on a population-health level.

Similar content being viewed by others
Notes
We submitted our research proposal to study three cohorts of patients in August 2018 and received data for one cohort in April 2019.
References
Institute of Medicine (US). unequal treatment: confronting racial and ethnic disparities in health care. (Smedley BD, Stith AY, Nelson AR, eds.). Washington: National Academies Press; 2014.
Rosenbloom JM, Senthil K, Long AS, Robinson WR, Peeples KN, Fiadjoe JE, Litman RS. A limited evaluation of the association of race and anesthetic medication administration: a single-center experience with appendectomies. Paediatr Anaesth. 2017;27:1142–7.
Jette CG, Rosenbloom JM, Wang E, De Souza E, Anderson TA. Association between race and ethnicity with intraoperative analgesic administration and initial recovery room pain scores in pediatric patients: a single-center study of 21,229 surgeries. J Racial Ethn Health Disparities. 2021;8:547–58.
King MR, De Souza E, Rosenbloom JM, Wang E, Anderson TA. Association between race and ethnicity in the delivery of regional anesthesia for pediatric patients: a single-center study of 3189 regional anesthetics in 25,664 surgeries. Anesth Analg. 2020;131:255–62.
Sadhasivam S, Chidambaran V, Ngamprasertwong P, Esslinger HR, Prows C, Zhang X, Martin LJ, McAuliffe J. Race and unequal burden of perioperative pain and opioid related adverse effects in children. Pediatrics. 2012;129:832–8.
Nafiu OO, Chimbira WT, Stewart M, Gibbons K, Porter LK, Reynolds PI. Racial differences in the pain management of children recovering from anesthesia. Paediatr Anaesth. 2017;27:760–7.
Nafiu OO, Thompson A, Chiravuri SD, Cloyd B, Reynolds PI. Factors associated with recovery room intravenous opiate requirement after pediatric outpatient operations. Anesth Analg. 2019;128:1225–33.
Baetzel A, Brown DJ, Koppera P, Rentz A, Thompson A, Christensen R. Adultification of Black children in pediatric anesthesia. Anesth Analg. 2019;129:1118–23.
Jimenez N, Seidel K, Martin LD, Rivara FP, Lynn AM. Perioperative analgesic treatment in Latino and non-Latino pediatric patients. J Health Care Poor Underserved. 2010;21:229–36.
Wallace ER, Birgfeld C, Speltz ML, Starr JR, Collett BR. Surgical approach and periprocedural outcomes by race and ethnicity of children undergoing craniosynostosis surgery. Plast Reconstr Surg. 2019;144:1384–91.
Maher KM, Owusu-Akyaw K, Zhou J, Cooter M, Ross AK, Lark RK, Taicher BM. Analysis of the impact of race on blood transfusion in pediatric scoliosis surgery. Paediatr Anaesth. 2018;28:352–60.
Owusu-Agyemang P, Cata JP, Kapoor R, Van Meter A, Zavala AM, Williams UU, Tsai JY, Feng L, Hayes-Jordan A. A retrospective evaluation of the impact of patient ethnicity on the use of epidural analgesia or blood transfusions in children undergoing major oncologic surgery. Perioper Med. 2019;8:6.
Rosenbloom JM, Mekonnen J, Tron LE, Alvarez K, Alegria M. Racial and ethnic health services disparities in pediatric anesthesia practice: a scoping review. J Racial Ethn Health Disparities. 2021;8:384–93.
Tzong KYS, Han S, Roh A, Ing C. Epidemiology of pediatric surgical admissions in US children: data from the HCUP kids inpatient database. J Neurosurg Anesthesiol. 2012;24:391–5.
Hall MJ, Schwartzman A, Zhang J, Liu X. Ambulatory surgery data from hospitals and ambulatory surgery centers: United States, 2010. Published online 2017.
Sun LS, Li G, Miller TLK, Salorio C, Byrne MW, Bellinger DC, Ing C, Park R, Radcliffe J, Hays SR, DiMaggio CJ, Cooper TJ, Rauh V, Maxwell LG, Youn A, McGowan FX. Association between a single general anesthesia exposure before age 36 months and neurocognitive outcomes in later childhood. JAMA. 2016;315:2312–20.
US Food and Drug Administration. Pediatric Anesthesia. Published April 27, 2017. Accessed May 14, 2018. https://www.fda.gov/Drugs/DrugSafety/InformationbyDrugClass/ucm527779.htm.
Bloche MG. Race and discretion in American medicine. Yale J Health Policy Law Ethics. 2001;1:95–131.
Girvan EJ, Gion C, McIntosh K, Smolkowski K. The relative contribution of subjective office referrals to racial disproportionality in school discipline. Sch Psychol Q. 2017;32:392–404.
Silber JH, Rosenbaum PR, Zhang X, Even-Shoshan O. Influence of patient and hospital characteristics on anesthesia time in medicare patients undergoing general and orthopedic surgery. Anesthesiology. 2007;106:356–64.
Silber JH, Rosenbaum PR, Ross RN, Even-Shoshan O, Kelz RR, Neuman MD, et al. Racial disparities in operative procedure time: the influence of obesity. Anesthesiology. 2013;119:43–51.
Koh JH, Daniel P, Bong CL. Parental perception on the effects of early exposure to anaesthesia on neurodevelopment. Anaesthesia. 2019;74:51–6.
Ayenew NT, Endalew NS, Agegnehu AF, Bizuneh YB. Prevalence and factors associated with preoperative parental anxiety among parents of children undergoing anesthesia and surgery: a cross-sectional study. Int J Surg Open. 2020;24:18–26.
Childers CP, Maggard-Gibbons M. Understanding costs of care in the operating room. JAMA Surg Am Med Assoc. 2018;153:e176233–e176233.
Rinehardt EK, Sivarajan M. Costs and wastes in anesthesia care. Curr Opin Anaesthesiol. 2012;25:221–5.
MPOG. Research. Published 2019, Accessed January 2, 2022. https://mpog.org/research.
Sømme S, Bronsert M, Morrato E, Ziegler M. Frequency and variety of inpatient pediatric surgical procedures in the United States. Pediatrics. 2013;132:e1466–72.
Kramer MR, Black NC, Matthews SA, James SA. The legacy of slavery and contemporary declines in heart disease mortality in the U.S. South. SSM Popul Health. 2017;3:609–17.
Ho AK, Kteily NS, Chen JM. “You’re one of us”: Black Americans’ use of hypodescent and its association with egalitarianism. J Pers Soc Psychol. 2017;113:753–68.
Williams DR, Haile R, González HM, Neighbors H, Baser R, Jackson JS. The mental health of Black Caribbean immigrants: results from the National Survey of American Life. Am J Public Health. 2007;97:52–9.
Rauh-Hain JA, Melamed A, Schaps D, Bregar AJ, Spencer R, Schorge JO, et al. Racial and ethnic disparities over time in the treatment and mortality of women with gynecological malignancies. Gynecol Oncol. 2018;149:4–11.
Pinheiro PS, Callahan KE, Boscoe FP, Balise RR, Cobb TR, Lee DJ, et al. Cancer site-specific disparities in New York, including the 1945–1965 birth cohort’s impact on liver cancer patterns. Cancer Epidemiol Biomarkers Prev. 2018;27:917–27.
Agency for Healthcare Research and Quality. 2019 National Healthcare Quality and Disparities Report Published January 2021. Accessed January 2021. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr19/index.html.
Nafiu OO, Maclean S, Blum J, Kheterpal S, Cowan A, Tremper KK. High BMI in children as a risk factor for intraoperative hypotension. Eur J Anaesthesiol. 2010;27:1065–8.
Ramgolam A, Hall GL, Zhang G, Hegarty M, von Ungern-Sternberg BS. Inhalational versus intravenous induction of anesthesia in children with a high risk of perioperative respiratory adverse events. Anesthesiology. 2018;128:1065–74.
Dewyer NA, Kram YA, Long S, Russell MD. Impact of a pediatric anesthesiologist on operating room efficiency during pediatric tonsillectomies and adenotonsillectomies. Ear Nose Throat J. 2017;96:E24–8.
Keenan RL, Shapiro JH, DAwson K. Frequency of anesthetic cardiac arrest in infants: effect of pediatric anesthesiologists. J Clin Anesthesiol. 1991;3:433–7.
National KIDS COUNT. Child population by race in the United States.” Kids Count Data Center. Published 09/2020. Accessed April 30, 2021. https://datacenter.kidscount.org/data/tables/103-child-population-by-race?loc=1&loct=1#detailed/1/any/false/1729,37,871,870,573,869,36,868,867,133/68,69,67,12,70,66,71,72/423,424.
Robert Wood Johnson, National Public Radio, T. H. Chan Harvard School of Public Health. Discrimination in America. 2018. Accessed January 1, 2021. shttps://www.rwjf.org/en/library/research/2017/10/discrimination-in-america--experiences-and-views.html.
Sox HC. Resolving the tension between population health and individual health care. JAMA. 2013;310:1933–4.
Redhu S, Jalwal GK, Saxena M, Shrivastava OP. A comparative study of induction, maintenance and recovery characteristics of sevoflurane and halothane anaesthesia in pediatric patients (6 months to 6 years). J Anaesthesiol Clin Pharmacol. 2010;26:484–7.
Adachi YU, Satomoto M, Higuchi H, Watanabe K. The determinants of propofol induction time in anesthesia. Korean J Anesthesiol. 2013;65:121–6.
Koenig T, Neumann C, Ocker T, Kramer S, Spies C, Schuster M. Estimating the time needed for induction of anaesthesia and its importance in balancing anaesthetists’ and surgeons’ waiting times around the start of surgery. Anaesthesia. 2011;66:556–62.
Acknowledgements
The authors gratefully acknowledge David A. August, MD PhD, Instructor at Massachusetts General Hospital, 55 Fruit Street Boston, MA, USA, and Erik Shank MD, South Shore Health 55 Fogg Road, South Weymouth, MA, USA. Both Drs. August and Shank are senior pediatric anesthesiologists who provided clinical expertise.
Funding
Dr. Rosenbloom’s work was supported by the National Institutes of Health (T32 GM007592 grant, Research Training for Anesthetists) and by the President and Fellows of Harvard College (Eleanor and Miles Shore 50th Anniversary Fellowship Program for Scholars in Medicine). All other support was provided from institutional and/or departmental sources. Funding for MPOG was provided by departmental and institutional resources at each contributing site. In addition, partial funding to support underlying electronic health record data collection into the Multicenter Perioperative Outcomes Group registry was provided by Blue Cross Blue Shield of Michigan/Blue Care Network as part of the Blue Cross Blue Shield of Michigan/Blue Care Network Value Partnerships program.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception and design. Material preparation, data conditioning, and analysis were performed by Drs. Julia M. Rosenbloom and Hao Deng and supervised by Dr. Timothy Houle. The first draft of the manuscript was written by Dr. Julia M. Rosenbloom and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of Interests
The authors declare no competing interests.
Disclaimer
Although Blue Cross Blue Shield of Michigan/Blue Care Network and Multicenter Perioperative Outcomes Group work collaboratively, the opinions, beliefs, and viewpoints expressed by the authors do not necessarily reflect the opinions, beliefs, and viewpoints of Blue Cross Blue Shield of Michigan/Blue Care Network or any of its employees.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rosenbloom, J.M., Deng, H., Mueller, A.L. et al. Race/Ethnicity and Duration of Anesthesia for Pediatric Patients in the US: a Retrospective Cohort Study. J. Racial and Ethnic Health Disparities 10, 1329–1338 (2023). https://doi.org/10.1007/s40615-022-01318-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-022-01318-2